Abstract
Uterine fibroids (leiomyomas) are the most common benign pelvic tumors in women and are the major indication for hysterectomy. Fibroids are more common and more severe among African American women. Although this disease disproportionately affects the African American population, we understand little about what causes this disparity. Fibroids should be considered a public health issue, given the magnitude of the problem and the costs of health care for this disease. In this review, we examine the burden of disease from fibroids in the African American population and review the natural history, diagnosis, and treatment of uterine fibroids, with emphasis on how these can differ, depending on race. We also focus on the socioeconomic burden caused by the disease and describe the anticipated influence of new health care reforms and funding mechanisms for fibroid research.
Keywords: disparity, hysterectomy, leiomyoma, Patient Protection and Affordable Care Act, uterine fibroids
Introduction
Uterine fibroids, also termed leiomyomas or myomas, are the most common benign gynecologic tumors; ultrasound evidence shows that more than 80% of African American women and approximately 70% of white women will have uterine fibroids by age 50 (1). However, because only 20% to 50% of all women with fibroids experience related symptoms (1,2), and because screening for fibroids is not routinely performed, the true incidence is difficult to ascertain. In fact, the reported incidence of fibroids in most studies likely is underestimated because they include only symptomatic women with clinical diagnoses confirmed ultrasonographically. For women in their 40s and 50s, abnormal uterine bleeding is the most common reason to seek gynecologic consultation, and fibroids are one of the most common causes of this symptom. Pelvic pain, another common reason for gynecologic consultation, is a symptom often associated with fibroids. These symptoms markedly alter the quality of life and reproductive health in affected women (3,4). Treatment options include many alternatives to hysterectomy, including medical therapies, minimally invasive surgery, uterine artery embolization, and magnetic resonance–guided focused ultrasound surgery. Hysterectomy, however, remains the most common intervention, and in the United States, fibroids are the leading indication for hysterectomies.
Disproportionate Impact of Fibroids in African Americans
In addition to a having greater lifetime incidence of fibroids, African American women have a 3-fold increased age-adjusted incidence rate and 3-fold increased relative risk of fibroids when adjusted for other confounding factors (1,5). Some investigators suggest a doubling of risk for Hispanic women, whereas others suggest that only African American women have increased risk (4–6). African ancestry is considered a key risk factor for the development of fibroids. African American women have fibroids diagnosed at earlier ages, are more likely to be symptomatic, and are likely to have different responses to medical treatment than white women (7). The size and growth rates of fibroids are greater in African American women, and they are more likely to undergo surgical intervention than other racial groups (8). Approximately 42 per 1,000 women are hospitalized annually because of fibroids, but African American women have higher rates of hospitalization, myomectomies, and hysterectomies compared with white women (relative risks of 3.5, 6.8, and 2.4, respectively) (9,10).
Taran et al (11) published a systematic review detailing the limited racial diversity in high-quality fibroid studies published from 2000 through 2006 and attempted to determine the factors that encouraged reporting of race and ethnicity. The investigation showed that greater than 75% of fibroid studies did not report the patient race, and most of the studies reporting race were those exclusively of African American women (eg, reports from the Black Women's Health Study). Of the remaining studies that reported race, African American women represented 15% of the studied population (11).
Biologic Studies of Racial Differences
Despite the racial differences in symptoms and incidence, relatively little data have been published regarding the biologic basis of fibroids in African American women. The few existing studies that examined large numbers of black and white women (eg, the Nurses' Health Study) did not show that risk factors that traditionally differed by race accounted for the increased burden of fibroids in African American women (5,7). Some data suggest that fibroid growth differs by race, especially as women approach menopause (12). Although some evidence links environmental factors such as diet and history of abuse to this increased risk, most of this information comes from studies such as the Black Women's Health Study (12–14). A recent study has linked vitamin D insufficiency with increased fibroid risk in black women (15). This study is important not only because of the biologic plausibility of the mechanism (ie, darker skin inhibits production of biologically active vitamin D) but because it opens a potential pathway to prevention.
Information on the genetic basis of fibroids in black women has been sparse for several reasons. First, many of the important genetic studies of fibroids using exome sequencing or genome-wide association studies have come from countries such as Finland and Japan, where there are few women of African descent (16,17). The Finding Genes for Fibroids study, begun in 1999, aimed to recruit both black and white US women for genome-wide association studies (18); however, the published reports have all been limited to the genetics of white women because participation by blacks has been limited (19,20). The historical issues of unethical treatment of African American medical study participants (eg, the Tuskegee syphilis studies) potentially has limited enrollment in these important studies.
Additional studies have demonstrated racial differences in fibroids at the molecular level, with differential gene expression of genes, proteins, and micro-RNAs (6,21,22). Based on these biologic differences, it is reasonable to hypothesize that fibroids in African American women may respond differently to medical therapy. If the pathophysiology of fibroids differs by race, there is a need for trials comparing fibroid therapies in African American vs white women.
Differences in Surgical Procedures and Outcomes
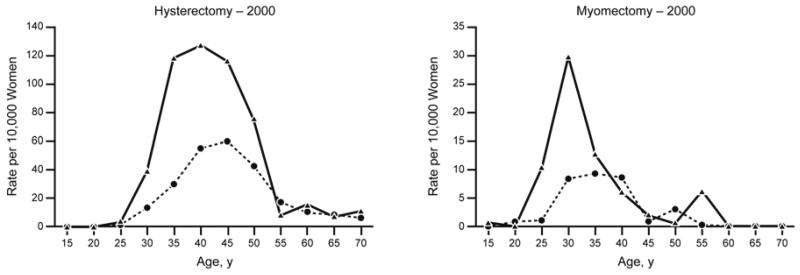
Surgical treatment for fibroids is especially prevalent among African American women because of both an earlier age of onset and more symptomatic disease. African American women are 2 to 3 times more likely to undergo hysterectomy for fibroid tumors than other racial groups (10,23). As reported in the National Hospital Discharge Survey, the total rates of hysterectomy for African American and white women were similar from 1988 through 1990 (61.7 and 56.5 per 10,000 women, respectively). However, fibroids as the primary indication for hysterectomy was muchc higher for African American women (61% vs 29% for white women) (23). This pattern was confirmed in another large cohort of 80,000 women which again showed that African American women had significantly higher rates of fibroid surgery than white women (24). Comparisons of the rates of hysterectomies and myomectomies in African American and white women indicate that African American women are more likely than white women to undergo both myomectomy and hysterectomy (Figure) (25). Myomectomy appears to be even more common in African American women, with almost a 7-fold increased relative risk (10). With the increasing racial diversity in the United States, this means that if surgical rates are stable, fibroid-related surgical procedures and hospitalizations are projected to increase by 20% to 31% by 2050 (10).
Figure.
Resource utilization by age and race (based on data from National Hospital Discharge Survey, National Ambulatory Medical Care Survey, and National Hospital Ambulatory Medical Care Survey only). Solid line denotes black women; dotted line, white women. (Adapted from Flynn et al [25]. Used with permission.)
Fibroids tend to be more numerous and larger among African American patients undergoing hysterectomy (26,27), which increases their risk of blood transfusion and postsurgical complications such as infection and bleeding. However, there are no corresponding data on racial differences in disease burden before other fibroid therapies or at the time of diagnosis.
Postoperative complications after myomectomy were twice as high in African American women compared with white women (odds ratio [OR], 2.5; 95% CI, 1.5–4.8) (28). Also, perioperative blood transfusions were significantly higher among the African American patients (OR, 2.3; 95% CI, 1.1–5.0) (28). The issue of blood transfusions is further complicated by the overrepresentation of African Americans among Jehovah's Witnesses, a group with a religious prohibition against blood transfusion. Published data estimated Jehovah's Witness congregations to be 22% black, whereas the general US population is 12% black (29). Because some gynecologic services and physicians insist that transfusion remain a medical option or decline to provide care for women who refuse transfusion, this can disproportionately affect black women who avoid or delay needed medical care out of fear that their religious beliefs will not be respected.
Fibroids in Pregnancy and Obstetric Outcomes
Uterine fibroids, especially submucosal fibroids, have an adverse impact on fertility and pregnancy (30). Furthermore, many studies have shown that removal of submucosal fibroids and large intramural fibroids (>5 cm) improves pregnancy outcome and live birth rates in patients undergoing in vitro fertilization (IVF) and in those who achieve spontaneous pregnancy (31–34). Pregnancy loss during the first trimester and spontaneous abortion are also twice as common in patients with fibroids (35–38). One meta-analysis evaluated the effect of uterine fibroids on rate of pregnancy loss in women undergoing IVF and found that patients in the leiomyoma group had twice the miscarriage rate as patients without fibroids (15.3% vs 7.7%) (39). Also, uterine fibroids have been associated with various obstetric complications such as preterm labor, fetal malposition, placenta previa, postpartum hemorrhage, and neonatal morbidity. Studies have shown that women with fibroids more commonly have cesarean delivery than women without fibroids (48.8% vs 13.3%), mostly because of fetal malpresentation and abnormal placentation caused by enlarged uterine fibroids (40–42).
A large retrospective cohort study by Lai et al (43) compared neonatal outcomes of women with and without leiomyoma. They found increased risk of preterm birth, low birth rate, and intrauterine fetal death in women with fibroids, regardless of maternal age, ethnicity, or parity.
Fibroids and Assisted Reproductive Technology
A recent review of fibroids and reproductive outcomes compared women with and without fibroids and documented lower cumulative birth rates (36.9% vs 41%), more miscarriages (20.4% vs 12.9%), and an increased rate of preterm delivery (OR, 1.5; 95% CI, 1.3–1.7) in women with fibroids (39). Disparities have been noted in the incidence and outcomes of fibroids when comparing white and African American women undergoing assisted reproductive technology (ART) (incidence of leiomyoma, 30.8% and 10.7% for African American and white women, respectively) (44). The higher prevalence of uterine fibroids among African American women potentially may lead to worse ART outcomes.
Feinberg et al (44) examined minority outcomes and use of ART in the US Department of Defense and compared it with minority utilization of ART in the US population. They compared the implantation rate, clinical pregnancy rate, spontaneous abortion rate, and live birth rate for African American and white women. First, they found that African American women used ART services more often when access to care was improved (eg, for employees of the military and their dependents). Second, they reported a decrease in live birth rate for African Americans (29.6% vs 35.8%; risk ratio [RR] 0.83; 95% CI, 0.67–1.02), and a significant increase in spontaneous abortion rate in African Americans (25% vs 15.9%; RR, 1.57; 95% CI, 1.05–2.36). Third, they determined that fibroids reduced ART success, regardless of race. In their study, fibroids were 3 times more prevalent in African American women (30.8% vs 10.7%; RR, 2.85; 95% CI, 2.06–3.95). For all women, ultrasonographic identification of fibroids at baseline was associated with reduced clinical pregnancy rates (35% vs 43.2%; RR, 0.74; 95% CI, 0.51–0.98), reduced live birth rates (26.2% vs 36.0%; RR, 0.63; 95% CI, 0.44–0.90), and reduced implantation rates (25.6% vs 31.1%; RR, 0.82; 95% CI, 0.69–0.98) (44). This study suggests that differences in ART outcomes by race in an environment offering equal access to care might, to some extent, be explained by the increased incidence of fibroids in African American women.
Fibroids as a Public Health Issue
Many parallels can be drawn between uterine fibroids and obesity, another prevalent public health problem. Greater than 33% of adults in the United States are overweight or obese, and the incidence of obesity is approximately 50% for African American women, whereas it is about 30% for white women (45). In comparison, the cumulative lifetime incidence of fibroids is 70% and 80% in white and African American women, respectively (1). Like obesity, fibroids are associated with a large financial burden; the annual cost of uterine fibroids in the United States (including direct medical costs and lost work-hour costs) is approximately $34.4 billion, and the annual cost of fibroid-related care (eg, surgery, hospital admissions, outpatient visits, and medication) is estimated to be $4.1 to 9.4 billion (46).
Obesity and fibroids each can convey a significant disease burden by affecting many aspects of women's health care and reproductive health, and certain racial and ethnic minorities are more likely to have development of both obesity and fibroids. Furthermore, obesity risk is associated with risk of uterine fibroids. One retrospective cohort study from the United States (47) reported that women with uterine fibroids were heavier than the general population of women (50% of women with fibroids were obese and 16% were morbidly obese; in comparison, 25% and 7.2% of the general population of women are obese and morbidly obese, respectively). The risk of uterine fibroid development is 3 times greater for women who weigh 70 kg or more compared with women who weigh 50 kg or less (9); this suggests that hyperestrogenic states in obesity may enhance fibroid growth.
Socioeconomic Impact and Disparities in Care
Socioeconomic status and race influence access to appropriate health care. This disparity is a significant and controversial problem in the United States health care system, especially because access to some therapies is directly affected by insurance status and cost of the procedure. When hysterectomies are performed, white women and women of other racial groups with private insurance are more likely to undergo laparoscopic procedures, whereas African Americans, Hispanics, and women with Medicare coverage are more likely to undergo abdominal procedures, even for the same indication (48). A large cohort study was conducted that compared the frequency of laparoscopic hysterectomies among different races for the treatment of uterine fibroids and menorrhagia between 1998 and 2002 (49). Even when the median household income was the same, African Americans, Hispanics, and women of other ethnic minorities were less likely to undergo laparoscopic hysterectomies (OR [95% CI] for each group was 0.44 [0.42–0.45], 0.58 [0.55–0.61], and 0.68 [0.64–0.72], respectively, when compared with white women) (49).
The same issues of access may also be present in other minimally invasive alternatives for uterine fibroids, including uterine artery embolization and hysteroscopic and robotically assisted magnetic resonance–guided focused ultrasound surgery. However, again, data are lacking in these key areas.
Among women with equal access to care, there is a race-based difference in the outcome and response to fibroid treatment (49,50). The cause of this difference remains poorly understood. The combination of genetic, physiologic, cultural, and socioeconomic factors likely contribute to these disparities. Patient preference may further influence treatment decisions.
Impact of Health Care Legislation
New legislation on health care reform creates an opportunity to improve women's health. Beginning in 2014, many health care services will make necessary changes that will improve access to affordable health care coverage for women. The Patient Protection and Affordable Care Act (ACA) requires that more health care services in the field of women's health be provided by all health care plans. In their report, the Institute of Medicine set a new national standard by recommending that 8 preventive service measures for women's health be covered in the health plan without cost sharing (51). For example, they recommended at least one “well woman” visit annually, which allows patients to receive reproductive health care during the preconception period, childbearing years, and menopause. These recommendations, along with the ACA, will improve provision of services and coverage to uninsured and underinsured women, ultimately reducing the discriminatory practices of the present health care system.
The new ACA aims to improve health and health care access for women, particularly during childbearing years, and this has specific implications for women with uterine fibroids (51). First, because the ACA gives women direct access to obstetricians and gynecologists without referral or preauthorization, it may decrease the recently reported disparity in the length of time African American women experience symptoms before seeking treatment compared with that of white women (52). Second, access to contraceptive medications without copayments is especially important because some steroid contraceptives, including oral contraceptives and the levonorgestrel intrauterine system, are used for medical treatment of fibroid-related heavy menstrual bleeding. Third, given the high risk of formation of new fibroids (ie, “recurrent disease”), elimination of the insurance companies' ability to deny coverage on the basis of preexisting conditions is a benefit to women with this condition.
Finally, but perhaps most importantly, the ACA provides funds for research through the establishment of the Patient-Centered Outcomes Research Institute (PCORI) (53). Uterine fibroids has recently been designated as a high-priority area for targeted research by PCORI (54).
Summary and Conclusion
Fibroids potentially can adversely affect reproductive health, fertility, success with ART, and birth rates. Fibroids are more common in African Americans compared with women of other races and thus can present major health problems among African American women. Fibroids develop at earlier ages and are more symptomatic; African American women have higher rates of surgery for fibroids and therefore may have more postoperative complications than other racial groups. More studies are needed on medical treatment options for African American women with fibroids because similar treatments have different results in African American and white women.
The ACA is a promising strategy that may improve availability of health care services for African American women. Under the ACA, women with the diagnosis of fibroids cannot be denied insurance coverage. Furthermore, women who undergo surgical treatment for fibroids will no longer be banned from lifetime medical insurance coverage. Women's health care providers will have a vital role in ensuring implementation of the new efforts and delivery of appropriate care.
Acknowledgments
Supported in part by grant R01060503 (to E.A.S.) from the National Institutes of Health.
E.A.S. serves as a clinical trial investigator for InSightec, NIH (HD060503) and as a consultant for Abbott, Bayer, and Gynesonics; she also receives royalties from UpToDate, Johns Hopkins University Press, and Massachusetts Medical Society. H.M.E., M.N.M., M.W., and A.Y.A.
Abbreviations
- ACA
Patient Protection and Affordable Care Act
- ART
assisted reproductive technology
- IVF
in vitro fertilization
- OR
odds ratio
- PCORI
Patient-Centered Outcomes Research Institute
- RR
risk ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: report no conflicts of interest.
References
- 1.Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003 Jan;188(1):100–7. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 2.Dragomir AD, Schroeder JC, Connolly A, Kupper LL, Hill MC, Olshan AF, et al. Potential risk factors associated with subtypes of uterine leiomyomata. Reprod Sci. 2010 Nov;17(11):1029–35. doi: 10.1177/1933719110376979. Epub 2010 Aug 6. [DOI] [PubMed] [Google Scholar]
- 3.Spies JB, Bradley LD, Guido R, Maxwell GL, Levine BA, Coyne K. Outcomes from leiomyoma therapies: comparison with normal controls. Obstet Gynecol. 2010 Sep;116(3):641–52. doi: 10.1097/AOG.0b013e3181ed36b3. [DOI] [PubMed] [Google Scholar]
- 4.Hartmann KE, Birnbaum H, Ben-Hamadi R, Wu EQ, Farrell MH, Spalding J, et al. Annual costs associated with diagnosis of uterine leiomyomata. Obstet Gynecol. 2006 Oct;108(4):930–7. doi: 10.1097/01.AOG.0000234651.41000.58. [DOI] [PubMed] [Google Scholar]
- 5.Marshall LM, Spiegelman D, Barbieri RL, Goldman MB, Manson JE, Colditz GA, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol. 1997 Dec;90(6):967–73. doi: 10.1016/s0029-7844(97)00534-6. [DOI] [PubMed] [Google Scholar]
- 6.Othman EE, Al-Hendy A. Molecular genetics and racial disparities of uterine leiomyomas. Best Pract Res Clin Obstet Gynaecol. 2008 Aug;22(4):589–601. doi: 10.1016/j.bpobgyn.2008.01.014. Epub 2008 Mar 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacoby VL, Fujimoto VY, Giudice LC, Kuppermann M, Washington AE. Racial and ethnic disparities in benign gynecologic conditions and associated surgeries. Am J Obstet Gynecol. 2010 Jun;202(6):514–21. doi: 10.1016/j.ajog.2010.02.039. Epub 2010 Apr 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laughlin SK, Stewart EA. Uterine leiomyomas: individualizing the approach to a heterogeneous condition. Obstet Gynecol. 2011 Feb;117(2 Pt 1):396–403. doi: 10.1097/AOG.0b013e31820780e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007 Nov;110(5):1091–5. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]
- 10.Wechter ME, Stewart EA, Myers ER, Kho RM, Wu JM. Leiomyoma-related hospitalization and surgery: prevalence and predicted growth based on population trends. Am J Obstet Gynecol. 2011 Nov;205(5):492.e1–5. doi: 10.1016/j.ajog.2011.07.008. Epub 2011 Jul 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taran FA, Brown HL, Stewart EA. Racial diversity in uterine leiomyoma clinical studies. Fertil Steril. 2010 Sep;94(4):1500–3. doi: 10.1016/j.fertnstert.2009.08.037. Epub 2009 Dec 6. [DOI] [PubMed] [Google Scholar]
- 12.Wise LA, Radin RG, Palmer JR, Kumanyika SK, Rosenberg L. A prospective study of dairy intake and risk of uterine leiomyomata. Am J Epidemiol. 2010 Jan 15;171(2):221–32. doi: 10.1093/aje/kwp355. Epub 2009 Dec 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baird D, Wise LA. Childhood abuse and fibroids. Epidemiology. 2011 Jan;22(1):15–7. doi: 10.1097/EDE.0b013e3181fe1fbe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wise LA, Radin RG, Palmer JR, Kumanyika SK, Boggs DA, Rosenberg L. Intake of fruit, vegetables, and carotenoids in relation to risk of uterine leiomyomata. Am J Clin Nutr. 2011 Dec;94(6):1620–31. doi: 10.3945/ajcn.111.016600. Epub 2011 Nov 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baird DD, Hill MC, Schectman JM, Hollis BW. Vitamin D and the risk of uterine fibroids. Epidemiology. 2013 May;24(3):447–53. doi: 10.1097/EDE.0b013e31828acca0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makinen N, Mehine M, Tolvanen J, Kaasinen E, Li Y, Lehtonen HJ, et al. MED12, the mediator complex subunit 12 gene, is mutated at high frequency in uterine leiomyomas. Science. 2011 Oct 14;334(6053):252–5. doi: 10.1126/science.1208930. Epub 2011 Aug 25. [DOI] [PubMed] [Google Scholar]
- 17.Cha PC, Takahashi A, Hosono N, Low SK, Kamatani N, Kubo M, et al. A genome-wide association study identifies three loci associated with susceptibility to uterine fibroids. Nat Genet. 2011 May;43(5):447–50. doi: 10.1038/ng.805. Epub 2011 Apr 3. [DOI] [PubMed] [Google Scholar]
- 18.Stewart EA, Morton CC. The genetics of uterine leiomyomata: what clinicians need to know. Obstet Gynecol. 2006 Apr;107(4):917–21. doi: 10.1097/01.AOG.0000206161.84965.0b. [DOI] [PubMed] [Google Scholar]
- 19.Hodge JC, T Cuenco K, Huyck KL, Somasundaram P, Panhuysen CI, Stewart EA, et al. Uterine leiomyomata and decreased height: a common HMGA2 predisposition allele. Hum Genet. 2009 Apr;125(3):257–63. doi: 10.1007/s00439-008-0621-6. Epub 2009 Jan 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eggert SL, Huyck KL, Somasundaram P, Kavalla R, Stewart EA, Lu AT, et al. Genome-wide linkage and association analyses implicate FASN in predisposition to Uterine Leiomyomata. Am J Hum Genet. 2012 Oct 5;91(4):621–8. doi: 10.1016/j.ajhg.2012.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pan Q, Luo X, Chegini N. Genomic and proteomic profiling I: leiomyomas in African Americans and Caucasians. Reprod Biol Endocrinol. 2007 Aug 23;5:34. doi: 10.1186/1477-7827-5-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishikawa H, Reierstad S, Demura M, Rademaker AW, Kasai T, Inoue M, et al. High aromatase expression in uterine leiomyoma tissues of African-American women. J Clin Endocrinol Metab. 2009 May;94(5):1752–6. doi: 10.1210/jc.2008-2327. Epub 2009 Feb 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilcox LS, Koonin LM, Pokras R, Strauss LT, Xia Z, Peterson HB. Hysterectomy in the United States, 1988–1990. Obstet Gynecol. 1994 Apr;83(4):549–55. doi: 10.1097/00006250-199404000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Templeman C, Marshall SF, Clarke CA, Henderson KD, Largent J, Neuhausen S, et al. Risk factors for surgically removed fibroids in a large cohort of teachers. Fertil Steril. 2009 Oct;92(4):1436–46. doi: 10.1016/j.fertnstert.2008.08.074. Epub 2008 Nov 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flynn M, Jamison M, Datta S, Myers E. Health care resource use for uterine fibroid tumors in the United States. Am J Obstet Gynecol. 2006 Oct;195(4):955–64. doi: 10.1016/j.ajog.2006.02.020. Epub 2006 May 24. [DOI] [PubMed] [Google Scholar]
- 26.Kjerulff KH, Langenberg P, Seidman JD, Stolley PD, Guzinski GM. Uterine leiomyomas: racial differences in severity, symptoms and age at diagnosis. J Reprod Med. 1996 Jul;41(7):483–90. [PubMed] [Google Scholar]
- 27.Moorman PG, Leppert P, Myers ER, Wang F. Comparison of characteristics of fibroids in African American and white women undergoing premenopausal hysterectomy. Fertil Steril. 2013 Mar 1;99(3):768–776.e1. doi: 10.1016/j.fertnstert.2012.10.039. Epub 2012 Nov 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roth TM, Gustilo-Ashby T, Barber MD, Myers ER. Effects of race and clinical factors on short-term outcomes of abdominal myomectomy. Obstet Gynecol. 2003 May;101(5 Pt 1):881–4. doi: 10.1016/s0029-7844(03)00015-2. [DOI] [PubMed] [Google Scholar]
- 29.Pew Forum on Religion & Public Life . U.S. Religious Landscape Survey [Internet] The Pew Forum on Religion & Public Life; Washington: c2010. Chapter 3, Religious affiliation and demographic groups; [cited 2012 Dec 27]. Available from: http://religions.pewforum.org/pdf/report-religious-landscape-study-chapter-3.pdf. [Google Scholar]
- 30.Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril. 2009 Apr;91(4):1215–23. doi: 10.1016/j.fertnstert.2008.01.051. Epub 2008 Mar 12. [DOI] [PubMed] [Google Scholar]
- 31.Seracchioli R, Rossi S, Govoni F, Rossi E, Venturoli S, Bulletti C, et al. Fertility and obstetric outcome after laparoscopic myomectomy of large myomata: a randomized comparison with abdominal myomectomy. Hum Reprod. 2000 Dec;15(12):2663–8. doi: 10.1093/humrep/15.12.2663. [DOI] [PubMed] [Google Scholar]
- 32.Abramovici H, Dirnfeld M, Auslander R, Bornstein J, Blumenfeld Z, Sorokin Y. Pregnancies following treatment by GnRH-a (Decapeptyl) and myomectomy in infertile women with uterine leiomyomata. Int J Fertil Menopausal Stud. 1994 May-Jun;39(3):150–5. [PubMed] [Google Scholar]
- 33.Surrey ES, Minjarez DA, Stevens JM, Schoolcraft WB. Effect of myomectomy on the outcome of assisted reproductive technologies. Fertil Steril. 2005 May;83(5):1473–9. doi: 10.1016/j.fertnstert.2004.11.045. [DOI] [PubMed] [Google Scholar]
- 34.Bulletti C, DE Ziegler D, Levi Setti P, Cicinelli E, Polli V, Stefanetti M. Myomas, pregnancy outcome, and in vitro fertilization. Ann N Y Acad Sci. 2004 Dec;1034:84–92. doi: 10.1196/annals.1335.010. [DOI] [PubMed] [Google Scholar]
- 35.Benson CB, Chow JS, Chang-Lee W, Hill JA, 3rd, Doubilet PM. Outcome of pregnancies in women with uterine leiomyomas identified by sonography in the first trimester. J Clin Ultrasound. 2001 Jun;29(5):261–4. doi: 10.1002/jcu.1031. [DOI] [PubMed] [Google Scholar]
- 36.Saravelos SH, Yan J, Rehmani H, Li TC. The prevalence and impact of fibroids and their treatment on the outcome of pregnancy in women with recurrent miscarriage. Hum Reprod. 2011 Dec;26(12):3274–9. doi: 10.1093/humrep/der293. Epub 2011 Sep 27. [DOI] [PubMed] [Google Scholar]
- 37.Lumbiganon P, Rugpao S, Phandhu-fung S, Laopaiboon M, Vudhikamraksa N, Werawatakul Y. Protective effect of depot-medroxyprogesterone acetate on surgically treated uterine leiomyomas: a multicentre case-control study. Br J Obstet Gynaecol. 1996 Sep;103(9):909–14. doi: 10.1111/j.1471-0528.1996.tb09911.x. [DOI] [PubMed] [Google Scholar]
- 38.Sheiner E, Bashiri A, Levy A, Hershkovitz R, Katz M, Mazor M. Obstetric characteristics and perinatal outcome of pregnancies with uterine leiomyomas. J Reprod Med. 2004 Mar;49(3):182–6. [PubMed] [Google Scholar]
- 39.Klatsky PC, Tran ND, Caughey AB, Fujimoto VY. Fibroids and reproductive outcomes: a systematic literature review from conception to delivery. Am J Obstet Gynecol. 2008 Apr;198(4):357–66. doi: 10.1016/j.ajog.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 40.Cook H, Ezzati M, Segars JH, McCarthy K. The impact of uterine leiomyomas on reproductive outcomes. Minerva Ginecol. 2010 Jun;62(3):225–36. [PMC free article] [PubMed] [Google Scholar]
- 41.Vergani P, Ghidini A, Strobelt N, Roncaglia N, Locatelli A, Lapinski RH, et al. Do uterine leiomyomas influence pregnancy outcome? Am J Perinatol. 1994 Sep;11(5):356–8. doi: 10.1055/s-2007-994554. [DOI] [PubMed] [Google Scholar]
- 42.Vergani P, Locatelli A, Ghidini A, Andreani M, Sala F, Pezzullo JC. Large uterine leiomyomata and risk of cesarean delivery. Obstet Gynecol. 2007 Feb;109(2 Pt 1):410–4. doi: 10.1097/01.AOG.0000250470.78700.f0. [DOI] [PubMed] [Google Scholar]
- 43.Lai J, Caughey AB, Qidwai GI, Jacoby AF. Neonatal outcomes in women with sonographically identified uterine leiomyomata. J Matern Fetal Neonatal Med. 2012 Jun;25(6):710–3. doi: 10.3109/14767058.2011.572205. Epub 2012 Mar 13. [DOI] [PubMed] [Google Scholar]
- 44.Feinberg EC, Larsen FW, Catherino WH, Zhang J, Armstrong AY. Comparison of assisted reproductive technology utilization and outcomes between Caucasian and African American patients in an equal-access-to-care setting. Fertil Steril. 2006 Apr;85(4):888–94. doi: 10.1016/j.fertnstert.2005.10.028. Epub 2006 Mar 9. [DOI] [PubMed] [Google Scholar]
- 45.Shaw KA, Caughey AB, Edelman AB. Obesity epidemic: how to make a difference in a busy OB/GYN practice. Obstet Gynecol Surv. 2012 Jun;67(6):365–73. doi: 10.1097/OGX.0b013e318259ee6a. [DOI] [PubMed] [Google Scholar]
- 46.Cardozo ER, Clark AD, Banks NK, Henne MB, Stegmann BJ, Segars JH. The estimated annual cost of uterine leiomyomata in the United States. Am J Obstet Gynecol. 2012 Mar;206(3):211.e1–9. doi: 10.1016/j.ajog.2011.12.002. Epub 2011 Dec 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shikora SA, Niloff JM, Bistrian BR, Forse RA, Blackburn GL. Relationship between obesity and uterine leiomyomata. Nutrition. 1991 Jul-Aug;7(4):251–5. [PubMed] [Google Scholar]
- 48.Armstrong A, Maddox YT. Health disparities and women's reproductive health. Ethn Dis. 2007 Spring;17(2 Suppl 2):S2-4–7. [PubMed] [Google Scholar]
- 49.Abenhaim HA, Azziz R, Hu J, Bartolucci A, Tulandi T. Socioeconomic and racial predictors of undergoing laparoscopic hysterectomy for selected benign diseases: analysis of 341,487 hysterectomies. J Minim Invasive Gynecol. 2008 Jan-Feb;15(1):11–5. doi: 10.1016/j.jmig.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 50.Weiss G, Noorhasan D, Schott LL, Powell L, Randolph JF, Jr, Johnston JM. Racial differences in women who have a hysterectomy for benign conditions. Womens Health Issues. 2009 May-Jun;19(3):202–10. doi: 10.1016/j.whi.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson KA. Women's health and health reform: implications of the Patient Protection and Affordable Care Act. Curr Opin Obstet Gynecol. 2010 Dec;22(6):492–7. doi: 10.1097/GCO.0b013e3283404e31. [DOI] [PubMed] [Google Scholar]
- 52.Stewart EA, Nicholson W, Bradley L, Borah B. The burden of uterine fibroids for African-American women: results of a national survey. J Womens Health. 2013 Oct; doi: 10.1089/jwh.2013.4334. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Patient-Centered Outcomes Research Institute . How we're funded [Internet] Patient-Centered Outcomes Research Institute; Washington (DC): ©2013 [cited 2013]. Available from: http://www.pcori.org/about-us/how-were-funded/ [Google Scholar]
- 54.Fischer E. Patient-Centered Outcomes Research Institute adopts revised methodology standards, okays targeted research topics, at Boston board meeting [Internet] Patient-Centered Outcomes Research Institute; Washington (DC): ©2013 [cited 2013]. Available from: http://www.pcori.org/2012/boston-board-decisions/ [Google Scholar]