Abstract
Quantifying the effects of specific neighborhood features on self-reported health is important to understanding the global health impact of neighborhood context. We investigated associations of neighborhood poverty, sociability and walkability with self-rated physical and mental health in the Multi-Ethnic Study of Atherosclerosis (MESA). In separate models, each neighborhood variable was associated with physical health but associations with sociability and walkability were stronger than those for poverty. Only walkability remained significant after adjusting for the other neighborhood variables. There was no evidence that self-rated mental health as assessed by the SF12 was associated with neighborhood poverty, walkability or sociability. This study provides information on how neighborhood context is associated with global health in diverse midlife and older persons.
Keywords: Neighborhood, self-rated health, income, education, employment
Understanding the determinants of self-reported physical and mental health is important in aging populations because such measures are indicative of quality of life (Alonso et al., 2004), and predict functional decline, other key health indicators, and mortality (Lee, 2000, Benyamini et al., 1999). Unlike objective markers of health, measures of self-rated health provide insight on how satisfied an individual is with his/her health, the way someone feels physically and emotionally, and how well a person is able perform every day activities. This information is valuable because it reflects an individual’s own judgment about how well they function in the world, and because it captures multiple aspects of health. For example, determinants of self-rated health include illness, mental health, lifestyle factors including physical activity and overweight (Molarius et al., 2007), tiredness, depression, pain (Molarius and Janson, 2002), psychosocial stressors, and social supports, some of which may not be captured in a single disease diagnosis (Giordano and Lindstrom, 2010). Self-rated health is therefore an integrated reflection of multiple health indicators, providing a broader picture of health compared to separate evaluations of individual health indicators.
The neighborhood environment may represent a meaningful opportunity to improve self-reported health because it has been shown to shape both health behaviors (such as physical activity, weight control, and smoking) and health outcomes (such as prevalence of chronic conditions and mental health) that are linked to self-rated health (King, 2008, Moore et al., 2009, McNeill et al., 2006, Ding and Gebel, 2012, Karasek et al., 2012, Choi and Schlichting-Ray, 2001, Brennan and Turrell, 2012, Auchincloss et al., 2009, Gidlow et al., 2010, Wilson et al., 2004). Although understanding the causal processes through which neighborhoods may affect health requires the testing of hypotheses about how various features of neighborhoods may affect specific health outcomes, quantifying the associations of neighborhood characteristics with global health measures is useful in understanding the global impact of neighborhood features on health and perceived quality of life generally.
A number of analyses have investigated associations of neighborhood deprivation, poverty or SES with self-reported health, finding that higher neighborhood deprivation is associated with worse self-rated health (van Jaarsveld et al., 2007, Wen et al., 2003, Verhaeghe and Tampubolon, 2012, Poortinga et al., 2008, Becares et al., 2012, Stafford et al., 2004). A growing body of work has also investigated associations of specific neighborhood features (such as facilities and services, green space, safety, and social connections) with self-rated health measures (de Vries et al., 2003, Maas et al., 2006, Collins et al., 2009, Cummins et al., 2005, Weden et al., 2008, Bond et al., 2012, Gidlow et al., 2010). While some studies have investigated both neighborhood deprivation and more specific measures simultaneously many included only selected populations (Wen et al., 2003, Poortinga et al., 2008, Stafford et al., 2004) or focused on a narrow geographic area, such as a single city (Wen et al., 2003). No studies of which we are aware have evaluated neighborhood deprivation and more specific features simultaneously in relation to self-reported health in diverse mid-life and older persons from broad geographic areas. In addition, few neighborhood studies have examined the physical and mental health related aspects of self-rated health separately (Gidlow et al., 2010).
It has been postulated that a number of factors (such as age, individual-level SES, or the extent to which individuals spend time in their neighborhoods) may be important in shaping an individual’s vulnerability to environmental effects (Kim, 2008, Ding and Gebel, 2012, Cummins et al., 2005, Weich et al., 2003). However, research on modifiers has had mixed results (Wong et al., 2009, Fone et al., 2007b, Kavanagh et al., 2006) possibly because of the large number of modifiers that have been explored and the possibility that the effect modification itself is modified by the larger context. A key modifier is likely to be the extent to which individuals spend time in their neighborhood or rely on their neighborhood for resources and social interactions. Learning more about how certain groups respond to their environment remains an important challenge (Ding and Gebel, 2012).
We quantified associations of neighborhood poverty and two specific features of neighborhood social and physical environments neighborhood sociability and walkability) with self-rated physical health and mental health in a large and diverse population-based sample of middle aged and older adults. In addition, we evaluated whether the associations between neighborhood poverty and health were explained by neighborhood sociability and/or neighborhood walkability. Because income, education and employment status may influence the time people spend in their neighborhoods or the degree to which they depend on neighborhood resources, we examined whether the association of health with specific neighborhood features differed depending on these characteristics.
Methods
Study Sample
The Multi-Ethnic Study of Atherosclerosis (MESA) was initiated in 2002 to investigate the prevalence, correlates, and progression of subclinical cardiovascular disease in men and women. Details about the study design are published elsewhere (Bild et al., 2002). Briefly, between July 2000 and August 2002, 6814 individuals who self-identified as white, black, Hispanic, or Chinese, were aged 45 to 84 years and free of clinically apparent cardiovascular disease were recruited from six US communities: Baltimore City and Baltimore County, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; Northern Manhattan and the Bronx, New York; and St. Paul, Minnesota. Individuals were excluded from the MESA sample if they had certain medical histories, were pregnant, spoke other than English, Spanish, Cantonese or Mandarin, resided in a nursing home, or planned to leave the community within five years (Bild et al., 2002).
Of the 6814 individuals in the original cohort, 581 did not provide data for exam 2, 150 did not consent to the neighborhood study, 47 had poor quality or unusable latitude/longitude values, and 77 had missing values for an outcome variable, leading to the final analytic sample of 5959 participants. The 855 excluded participants were significantly older, and were significantly more likely to be female and non-white with a lower education level, but differences were of small magnitude.
Outcome variables: SF12 Health Survey
A slightly modified version of The 12-Item Short Form Health Survey, Version 2.0 (SF12v2) was used as a measure of self-rated health and well-being (Ware et al., 1996). The SF12v2 is a shorter version of the SF36v2. The physical component summary (PCS) and the mental component summary (MCS) were each calculated based on the raw score from the same 12 questionnaire items; however, different weights were applied to each question for the PCS and MCS (Ware et al., 1995). For example, the PCS weighted questions about physical functioning, physical tasks and bodily pain more heavily weighted whereas questions about social functioning, limitations due to emotional problems and mental health were more heavily weighted in the MCS. Each score (range 0–100 points) was standardized according to the U.S. population so that scores above 50 are interpreted as higher than the average in the general U.S. population and those lower than 50 are below the average. Both the PCS and MCS component scores have adequate reliability and validity (Ware et al., 1996, Cheak-Zamora et al., 2009) and are used widely (Gandek et al., 1998). The SF12 was administered at the second MESA examination.
Exposure Measures: Neighborhood Poverty and Neighborhood Scales
Neighborhood poverty quantified the percent of residents in a participant’s census tract that were at or below the poverty level in the year 2000. For example, a four-person family unit with two children and an annual income of less than $17,463 in 2000 would qualify as being in poverty (U.S. Census Bureau, 2009). The data were obtained from the US Census Bureau (Bureau, 2001).
Neighborhood scales were created based on survey responses of residents who rated the aesthetic quality, safety, social cohesiveness and walking environment of their neighborhoods (the mean of each scale item is shown in Table 1). On the survey, “neighborhood” was defined for participants as a one-mile radius around their home. To create these scales, data collected from MESA participants was combined with data from participants in a survey administered to other residents of MESA neighborhoods (referred to as the Community Survey) to create summary measures for each census tract. Census tract level measures were linked to each MESA participant based on their home address. Community Survey participants were recruited using random-digit-dialing (RDD) (Mujahid et al., 2007). The MESA data was supplemented with the Community Survey data in order to have larger sample sizes within each neighborhood (census tract) and improve the reliability and validity of the neighborhood level estimates.
Table 1.
Description of neighborhood characteristic survey scale items (n=5959)
| Measure | Scale items | Crude Mean (SD)a |
|---|---|---|
| Aesthetic Quality Scale | • A lot of trash and litter on street | 3.72 (1.1) |
| • A lot of noise | 3.17 (1.2) | |
| • Neighborhood attractive | 3.93 (0.9) | |
| Safety Scale | • Feel safe walking day or night | 3.61 (1.1) |
| • Violence a problem | 3.70 (1.1) | |
| Social Cohesion Scale | • People willing to help neighbors | 3.72 (0.9) |
| • People generally get along | 3.78 (0.8) | |
| • People can be trusted | 3.50 (0.9) | |
| • People share same values | 3.13 (1.0) | |
| Walking Environment Scale | • Pleasant to walk | 4.00 (0.9) |
| • Easy to walk to places | 3.83 (1.0) | |
| • Often see other people walking | 4.12 (0.8) | |
| • Often see other people exercise | 3.72 (1.1) |
Higher scores represent more favorable neighborhood ratings for all scales; score range = 1–5 for all scales.
Conditional empirical Bayes estimation was used to develop estimates of each neighborhood construct for each census tract (Mujahid et al., 2008). Empirical Bayes estimates are essentially a weighted average of the mean for each neighborhood and the mean across all neighborhoods in the study, where the weights are proportional to the reliability of the neighborhood measure. The empirical Bayes approach improves the estimates for census tracts with small numbers by borrowing information across tracts. The estimates we used were conditional on site and adjusted for age, gender, and survey type (MESA vs. the Community Survey) to account for differences in the characteristics of respondents across census tracts. Each score has a total possible range from 1–5. Mean (SD) empirical Bayes estimates for each scale were: aesthetic quality [3.6 (0.39)], safety [3.6 (0.37)], social cohesion [3.5 (0.22)] and walking environment [3.9 (0.30)]. These scales have been shown to be reliable (Mujahid et al., 2007).
Additional covariates
Age at MESA exam 2 (calculated using date of birth), sex, race/ethnicity (white, Chinese, African American, Hispanic), site (Maryland, Illinois, North Carolina, California, New York, Minnesota), and the highest year of education completed were assessed via questionnaire. Annual personal income was calculated by dividing annual household income (the midpoint of questionnaire-based categories) by the number of people it supported. Measured weight and height values were used to calculate BMI, using the standard formula: weight (kg)/height (m)2. Diabetes mellitus was defined by 2003 American Diabetes Association criteria (Genuth et al., 2003), which includes a fasting glucose level of 126 mg/dL or higher or taking insulin or oral hypoglycemic agents. Hypertension was defined as a blood pressure ≥140/90 mm Hg or a history of hypertension and use of blood pressure medications. Total moderate and vigorous physical activity in a typical week in the past month was used as a measure of physical activity.
Statistical Analysis
Because the four neighborhood characteristic survey scales (aesthetic quality, safety, social cohesion and walking environment) were moderately to highly correlated (Spearman correlation coefficients ranged from 0.09 to 0.8 but most were between 0.6 and 0.7; all p<0.0001), we combined the scales into linear combination variables using principal components analysis with orthogonal rotation. This procedure reduced the number of exposure variables and the number of comparisons made. The two factors that emerged from this analysis are referred to here as “sociability” and “walkability” named for the underlying variables that compose each. Each of these two variables is a standardized estimate of the principal component values. The sociability variable accounted for 62% of the variance in the original 4 variables; the three variables that loaded most highly were included in the final variable: social cohesion (rotated factor loading 0.93), safety (rotated factor loading 0.81) and aesthetic quality (rotated factor loading 0.94). The walkability variable accounted for 25% of the variance in the original variables but only the walking environment loaded highly (rotated factor loading 0.98) onto this variable so it was kept as a separate variable. Correlations among the neighborhood variables (neighborhood poverty with sociability or walkability) were estimated using Spearman rank correlation coefficients.
Unadjusted associations were examined by calculating mean PCS or MCS for low, medium and high categories (based on tertiles of the distribution) of each neighborhood characteristic. Population average linear regression models were fit using generalized estimating equations (Liang and Zeger, 1986) with continuous PCS or MCS score as the outcome variable and neighborhood poverty, sociability, and/or walkability as the exposures of interest. The sample was distributed in 1300 census tracts with a median of 2 participants per tract (SD 10, 25–75th percentiles 1 and 5, respectively); the models accounted for the correlation in outcomes within census tracts and allowed for variable numbers of participants per tract. Since descriptive analyses did not show evidence of a threshold effect, neighborhood variables were included in regression models as continuous variables and were scaled so that a one unit increase was equivalent to the difference between the 90th and 10th percentile (or the 10th and 90th percentile for neighborhood poverty which is inversely associated with health). This approach has been used in prior work (Auchincloss et al., 2009) and has two key advantages: (1) it allows direct comparisons of the strengths of the associations across different neighborhood variables and (2) it facilitates interpretability as it illustrates the strength of the association that would be observed (based on the beta coefficient for the continuous independent variable) across the maximum range of the distribution of the neighborhood variable observed in the data (excluding outliers above the 90th or below the 10th percentile).
We fit two sets of models progressively adjusted for sets of variables. “Model 1” adjusted for known confounders of the association of neighborhood characteristics with health including sex, age, race/ethnicity, education, income and site. “Model 2” added variables that could be either confounders or mediators because prior work has shown them to be potentially influenced by neighborhood characteristics. These variables included BMI, type 2 diabetes, hypertension, history of cardiovascular disease (including cardiac arrest, angina, and stroke) and physical activity.
In order to compare the associations of each neighborhood variable with the outcomes, each neighborhood variable was first examined separately in models 1 and 2. Then in order to address our research question regarding whether the associations between neighborhood poverty and health were explained by neighborhood sociability and/or neighborhood walkability, we fit models that included neighborhood poverty and each of the other two neighborhood variables separately as well as a full model that included all three neighborhood variables. In order to examine our hypothesis regarding effect modification, we added a proposed effect modifier (i.e. employment status, income or education) to the model and interacted that variable with each neighborhood variable in model 2. Effect modification was evaluated in a separate model for each neighborhood variable. For these analyses, persons were defined as employed if they reported being currently employed or self-employed at a job for pay.
Results
MESA participants’ age ranged from 46–86 years, [mean (SD) age 63.5 (10.1) years; Table 2]. Nearly 40% of participants were white, 26.9% were African American, and 21.5% were Hispanic (Table 2). Just over half of participants earned less than $40,000 annually, and about 12% earned less than $12,000 per year. Most had a Bachelor’s degree (37.1%) but roughly a third only had a high school or equivalent or less. The average BMI was in the overweight range [mean (SD) 28.4 (5.5) kg/m2].
Table 2.
Characteristics of participants from Multi-Ethnic Study of Atherosclerosis (MESA) Exam 2, 2002–2004 (n=5959)
| Characteristic | Frequency (%) or Mean (SD) where indicated | PCS score Mean (SD) |
MCS score Mean (SD) |
|---|---|---|---|
| PCS score [Mean (SD)] | 48.8 (9.2) | -- | -- |
| MCS score [Mean (SD)] | 52.1 (8.8) | -- | -- |
| Age, y [mean (SD)] | 63.5 (10.1) | -- | -- |
| 46–56 | 1807 (30.3) | 50.4 (8.4)a | 50.6 (9.3)a |
| 57–66 | 1687 (28.3) | 49.4 (8.8) | 52.6 (8.3) |
| 67–76 | 1749 (29.4) | 47.9 (9.4) | 52.8 (8.6) |
| 77–86 | 716 (12.0) | 45.1 (10.1) | 53.2 (8.7) |
| Sex | |||
| Female | 3119 (52.3) | 47.4 (10.0)b | 51.3 (9.3)b |
| Male | 2840 (47.7) | 50.3 (8.0) | 53.1 (8.1) |
| Race/ethnicity | |||
| White | 2367 (39.7) | 49.9 (8.9) | 52.0 (8.7) |
| Chinese | 712 (12.0) | 48.9 (8.1)c | 52.9 (8.6)c |
| African American | 1600 (26.9) | 47.8 (9.6)c | 52.5 (8.5) |
| Hispanic | 1280 (21.5) | 47.8 (9.5)c | 51.4 (9.6) |
| Annual Income of Participant | |||
| <12000 | 674 (11.7) | 44.4 (10.5)a | 50.4 (10.1)a |
| 12000–24999 | 1019 (17.8) | 47.2 (9.4) | 51.9 (9.4) |
| 25000–39999 | 1182 (21.6) | 48.0 (9.4) | 52.1 (8.7) |
| 40000–74999 | 1498 (26.1) | 49.6 (8.7) | 52.3 (8.7) |
| 75000+ | 1367 (23.8) | 52.1 (7.0) | 52.8 (7.8) |
| Education | |||
| Completed HS/GED or less | 2048 (34.5) | 46.8 (9.6)a | 51.6 (9.3)a |
| Some college, Technical or Associate degree | 1690 (28.4) | 48.4 (9.3) | 52.2 (8.7) |
| Bachelor’s degree or higher | 2204 (37.1) | 50.9 (8.1) | 52.5 (8.4) |
| Currently employed or self-employed at a job for pay | |||
| Yes | 3028 (50.9) | 51.1 (7.2)b | 52.1 (8.3) |
| No | 2925 (49.1) | 46.4 (10.3) | 52.2 (9.3) |
| BMI kg/m2 [Mean (SD)] | 28.4 (5.5) | -- | -- |
| <18.5 kg/m2 (underweight) | 44 (0.7) | 51.6 (7.2)a | 50.2 (9.6) |
| 18.6–25 kg/m2(normal weight) | 1659 (27.9) | 50.3 (8.2) | 52.1 (8.6) |
| 25–29 kg/m2 (overweight) | 2330 (39.2) | 49.6 (8.6) | 52.5 (8.4) |
| 30+ kg/m2 (obese) | 1906 (32.1) | 46.4 (10.1) | 51.7 (9.4) |
Significant trend in mean PCS or MCS score across ordinal categories
Mean PCS or MCS score significantly different between groups; tested with Student’s t-test for independent samples
Mean score significantly different vs. white (referent)
The mean (SD) PCS score was 48.8 (9.2) points (Table 2), just below the average for the US population. As expected, the average score was significantly better in younger persons, males, whites, and those with higher incomes, greater education level and lower BMI (not shown). The average (SD) MCS score was just above the national average [50.6 (9.3) points; Table 2]. In general, the differences in MCS scores were not as great when comparing across these same characteristics, though younger people, males, the more educated, and those with higher income levels tended to have better scores (not shown). The median percent of people living at or below the poverty level in all census tracts was 13% (IQR 16%; 5th percentile 2.5% and 95th percentile 37%). Neighborhood sociability and neighborhood poverty were fairly highly correlated (r=−0.73), whereas neighborhood walkability and neighborhood poverty were much less correlated (r=−0.23).
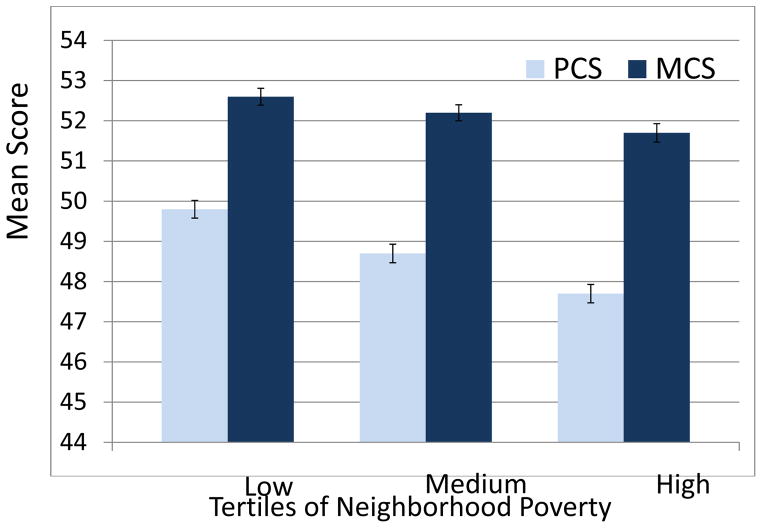
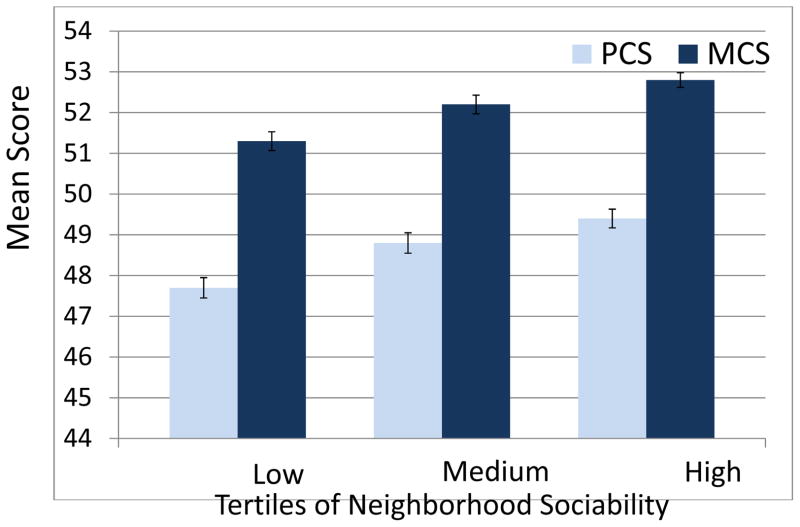
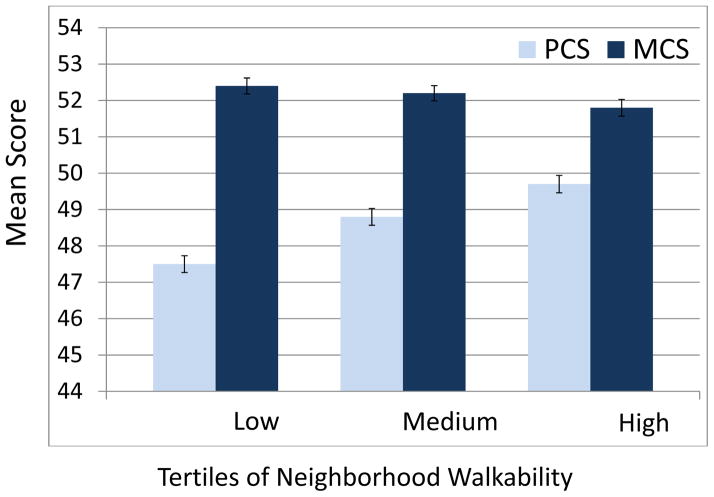
The Figures show mean PCS and MCS scores by tertiles of neighborhood poverty, (Figure 1), neighborhood sociability (Figure 2) and neighborhood walkability (Figure 3), adjusted for age and sex. Both mean PCS and MCS declined as neighborhood poverty increased (p for trend <0.0001 and 0.005, respectively; Figure 1). A similar pattern was observed across sociability tertiles; mean PCS and MCS are higher in neighborhoods of higher sociability in a graded fashion (both p for trend <0.0001; Figure 2). Whereas mean PCS score decreased approximately linearly as neighborhood walkability decreased (p<0.0001), mean MCS score is linear but has a slightly flatter trend across the tertiles (p=0.05; Figure 3).
Figure 1.
Mean physical component score (PCS) and mental component score (MCS) across tertiles of neighborhood poverty, adjusted for age and sex. PCS test for trend: p<0.0001 and MCS test for trend: p=0.005.
Figure 2.
Mean physical component score (PCS) and mental component score (MCS) across tertiles of neighborhood sociability, adjusted for age and sex. PCS test for trend: P<0.0001 and MCS test for trend: p<0.0001.
Figure 3.
Mean physical component score (PCS) and mental component score (MCS) across tertiles of neighborhood walkability, adjusted for age and sex. PCS test for trend: P<0.0001 and MCS for trend: p=0.05.
In separate adjusted models, greater neighborhood poverty, and poorer neighborhood sociability and neighborhood walkability were each significantly associated with lower PCS (Table 3). The mean difference in PCS between the 10th and 90th percentile of neighborhood poverty was 1.0 (95% CI: 0.3, 1.8) after adjusting for sex, age, education, income, race and site (model 1). The association remained similar (mean difference 0.9 (95% CI: 0.2, 1.7) after further adjustment for BMI, type 2 diabetes, hypertension, cardiovascular disease and physical activity (model 2). Associations of neighborhood sociability with PCS were stronger than those observed for poverty: mean difference between the 90th and 10th percentile of neighborhood sociability [1.9 (95% CI: 0.9, 2.9] after adjusting for model 1 variables and [1.7 (95% CI: 0.8, 2.6)] after adjustment for model 2 variables. Walkability was also more strongly associated with PCS than poverty: mean difference comparing the 90th to the 10th percentile was [1.8 (95% CI: 1.0, 2.5)] after adjusting for model 1 variables. This association was reduced by 17% but remained statistically significant after adjustment for model 2 variables [1.5 (95% CI: 0.9, 2.1)]. The model 1 covariates most consistently associated with lower PCS score were female sex, lower income, lower education, higher age, and black race/ethnicity (compared to white race/ethnicity).
Table 3.
Mean differences in PCS or MCS score associated with neighborhood poverty, neighborhood sociability or neighborhood walkability (each neighborhood variable is examined in a separate model)
| PCS score Mean difference (95% CI) |
MCS score Mean difference (95% CI) |
|
|---|---|---|
|
|
||
| Mean difference between 10th (best) vs. 90th (worst) percentile of poverty | ||
| Unadjusted | 2.4 (1.7, 3.0) a | 1.0 (0.4, 1.6) a |
| Adjusted for Model 1 variablesb | 1.0 (0.3, 1.8) a | 0.2 (−0.6, 0.9) |
| Adjusted for Model 2 variablesc | 0.9 (0.2, 1.7) a | 0.2 (−0.6, 0.9) |
| Mean difference between 90th (best) vs. 10th (worst) percentile of sociability | ||
| Unadjusted | 2.3 (1.5, 3.1) a | 1.8 (1.1, 2.4) a |
| Adjusted for Model 1 variablesb | 1.9 (0.9, 2.9) a | 0.6 (−0.4, 1.5) |
| Adjusted for Model 2 variablesc | 1.7 (0.8, 2.6) a | 0.5 (−0.5, 1.5) |
| Mean difference between 90th (best) vs. 10th (worst) percentile of walkability | ||
| Unadjusted | 2.6 (2.0, 3.2) a | −0.8 (−1.5, −0.2) a |
| Adjusted for Model 1 variablesb | 1.8 (1.0, 2.5) a | 0.4 (−0.5, 1.3) |
| Adjusted for Model 2 variablesc | 1.5 (0.9, 2.1) a | 0.4 (−0.5, 1.3) |
P<0.05
Model 1: adjusted for sex, age (centered at 64 years), education (centered at 13 years), income (centered at $22,500 annual income), race, and site.
Model 2: adjusted for sex, age (centered at 64 years), education (centered at 13 years), income (centered at $22,500 annual income), race, site, BMI (centered at 28), type 2 diabetes, hypertension, cardiovascular disease, and total physical activity in a typical week (centered at median value 3570 MET-minutes per week).
None of the associations of neighborhood variables with MCS were statistically significant after adjustment for model 1 or model 2 variables. The model 1 covariates most consistently associated with lower MCS score were female sex, lower income, lower education, lower age, white race/ethnicity, and being a participant at the Chicago study site (compared to the reference group of Los Angeles).
When neighborhood poverty and neighborhood sociability were simultaneously considered in models in which PCS was the dependent variable, neighborhood sociability remained associated with PCS [mean difference (95% CI) in PCS between the 90th and 10th percentile of sociability 1.5 (0.4, 2.6), in the fully adjusted model 2] whereas associations with neighborhood poverty were no longer statistically significant (Table 4). Similarly, when estimates for neighborhood walkability and neighborhood poverty were adjusted for each other, only neighborhood walkability remained significant [mean difference (95% CI) in PCS between the 90th and 10th percentile of walkability 1.3 (0.6, 1.9) in the fully adjusted model 2; Table 4]. When all three neighborhood characteristics were included, only associations of neighborhood walkability with PCS remained statistically significant [mean difference (95% CI) in PCS between the 90th and 10th percentile of walkability 1.0 (0.4, 1.7) in the fully adjusted model 2]. None of the associations of neighborhood variables with MCS were statistically significant.
Table 4.
Mean differences in PCS score or MCS score associated with neighborhood poverty, sociability and walkability, adjusted for other neighborhood characteristics
| Neighborhood Poverty Mean difference (95% CI) in score between the 10th (best) and 90th (worst) percentile of poverty |
Neighborhood Sociability Mean difference (95% CI) in score between the 90th (best) and 10th (worst) percentile of sociability |
Neighborhood Walkability Mean difference (95% CI) in score between the 90th (best) and 10th (worst) percentile of walkability |
|
|---|---|---|---|
|
|
|||
| PCS score
|
|||
| Model 1b | |||
| Neighborhood poverty + sociability | 0.4 (−0.6, 1.3) | 1.6 (0.4, 2.8) a | |
| Neighborhood poverty + walkability | 0.7 (−0.1, 1.5) | 1.5 (0.7, 2.2) a | |
| Neighborhood poverty + sociability + walkability | 0.2 (−0.8, 1.2) | 1.1 (−0.1, 2.3) | 1.3 (0.5, 2.1) a |
| Model 2c | |||
| Neighborhood poverty + sociability | 0.2 (−0.7, 1.2) | 1.5 (0.4, 2.6) a | |
| Neighborhood poverty + walkability | 0.6 (−0.2, 1.3) | 1.3 (0.6, 1.9) a | |
| Neighborhood poverty + sociability + walkability | 0.2 (−0.7, 1.1) | 0.9 (−0.3, 2.1) | 1.0 (0.4, 1.7) a |
| MCS score
|
|||
| Model 1b | |||
| Neighborhood poverty + sociability | −0.3 (−1.3, 0.7) | 0.8 (−0.4, 2.1) | |
| Neighborhood poverty + walkability | 0.001 (−0.8, 0.8) | 0.4 (−0.7, 1.4) | |
| Neighborhood poverty + sociability + walkability | −0.3 (−1.3, 0.7) | 0.8 (−0.5, 2.1) | 0.3 (−0.8, 1.3) |
| Model 2c | |||
| Neighborhood poverty + sociability | −0.3 (−1.3, 0.7) | 0.8 (−0.5, 2.1) | |
| Neighborhood poverty + walkability | −0.05 (−0.9, 0.8) | 0.4 (−0.6, 1.5) | |
| Neighborhood poverty + sociability + walkability | −0.4 (−1.4, 0.6) | 0.7 (−0.6, 2.1) | 0.3 (−0.8, 1.4) |
P<0.05
Model 1: adjusted for sex, age (centered at 64 years), education (centered at 13 years), income (centered at $22,500 annual income), race, and site.
Model 2: adjusted for sex, age (centered at 64 years), education (centered at 13 years), income (centered at $22,500 annual income), race, site, BMI (centered at 28), type 2 diabetes, hypertension, cardiovascular disease, and total physical activity in a typical week (centered at median value 3570 MET-minutes per week).
There were no additive interactions between neighborhood poverty or sociability when PCS was the dependent variable. However, there was evidence of interaction between neighborhood walkability and personal income such that the association between greater walkability and better PCS was stronger in those with lower incomes (p=0.03). In those at the 10th percentile of personal income, the mean difference (95% CI) in PCS between the 90th and 10th percentile of walkability was 1.9 (1.2, 2.6), and in those at the 90th percentile of personal income, the mean difference was still statistically significant but much lower [1.0 (0.3, 1.7)] (model 2). There was also an interaction between neighborhood sociability and employment status for MCS (p=0.002). In persons who were not employed, the mean difference (95% CI) in MCS between the 90th and 10th percentile was 1.4 (0.2, 2.6), and in the employed it was −0.4 (−1.5, 0.6) (model 2).
Discussion
Our results suggest that self-rated physical health is consistently associated with the neighborhood environment. When considered in separate models, each neighborhood variable was associated with physical health but associations with sociability and walkability were stronger than those observed for poverty. In addition, associations with neighborhood poverty were substantially reduced and were no longer statistically significant when walkability or sociability were included in the model. In models including all three neighborhood variables only walkability was significantly associated with the physical health score. In contrast, there was no evidence that self-rated mental health as assessed by the SF12 was associated with neighborhood poverty, walkability or sociability. However, we found that higher neighborhood sociability was associated with better mental health in those who were not employed (but not in those who were employed). We also found evidence that the association between greater neighborhood walkability and better PCS was stronger in those with lower incomes.
To date, most studies of neighborhood deprivation (or poverty) and specific neighborhood features have not focused on mid-life and older persons. In addition, few neighborhood studies have examined the physical and mental health related aspects of self-rated health separately (Gidlow et al., 2010). In our diverse sample of midlife and older participants, we found that neighborhood features were more consistently associated with the physical than with the mental health components of self-reported health. In addition we found that walkability and sociability were more strongly associated with physical health than poverty, and that the associations of neighborhood poverty with physical health disappeared when the more specific measures were in the model. This suggests that poverty may be a limited proxy for the neighborhood features relevant to health.
Neighborhood walkability stood out among the three exposures because it remained significantly associated with general physical health independent of neighborhood poverty, neighborhood sociability and individual characteristics. It is not completely clear why walkability was relatively more important for physical health in our study compared to sociability. The physical health scale taps physical functioning and activity performance that require one to be physically active. It could be that our results reflect that the social environment is somewhat more distal to physical health compared to the walking environment. Differences in the measurement validity of the sociability and walkability scales cannot be ruled out and could also contribute to the more consistent associations of walkability than sociability with physical health after full adjustment. The fairly high correlation between sociability and poverty could also have made it difficult to disentangle the effects of sociability from those of poverty in the model with all three neighborhood measures, although sociability remained statistically significantly associated with self-reported physical health in the model that adjusted only for poverty.
We expected to find associations between specific neighborhood features and self-rated mental health after adjustment for relevant factors but did not. A growing and fairly consistent body of work cites associations between adverse neighborhood conditions and depression (Mair et al., 2008). Associations with self-rated mental health, a separate construct than depression, tend to be in step with the literature on depression though much of this work has been done in the UK (Fone et al., 2007a, Stafford et al., 2008, Gale et al., 2011). For example, in the Whitehall II study, greater neighborhood deprivation and social fragmentation were associated with worse MCS score (Stafford et al., 2008). We have no clear explanation for why neighborhood features were not related to MCS scores in MESA, despite previous work showing associations of neighborhood aesthetic quality, safety, and social cohesion with depressive symptoms in the MESA cohort (Mair et al., 2009). The correlation between the MCS and the Center for Epidemiologic Studies Depression Scale (used to measure depressive symptoms) in MESA is −0.41. It is plausible that the neighborhood measures that we investigated and the summaries that we created are not related to the mental health constructs tapped into by the MCS measures.
A suggestive finding of our analyses is that lower sociability was in fact associated with lower MCS in persons who were not employed. Likewise, the association between higher neighborhood walkability and better PCS was stronger in those with lower personal incomes. It could be that those who were not employed and those with lower incomes were spending more time in their neighborhood and also may have relied more on neighborhood resources. These interactions deserve further exploration.
The MESA sample is diverse ethnically and geographically, but is not a representative sample of all adults 45 and older in the MESA communities because of the exclusion criteria utilized. It is likely that the sample is healthier than the general population. However, unless there is strong effect modification by factors related to participation, our results are likely to be approximately representative of associations observed in the general population. An additional limitation of our study is the cross-sectional nature of the analysis. Reverse causality, i.e. that those with better physical health sought out or were better able to locate in better neighborhoods is also a possibility. The observational nature of the data, and the possibility of residual confounding, also limits causal inferences.
Among the strengths of this study are the large sample size, and the geographic and ethnic diversity of the MESA cohort. Moreover, the MESA population is composed of a relatively stable sample of adults, who on average lived in their respective neighborhoods for 19 years. Another strength is the assessment of neighborhood attributes using sophisticated survey and analytical approaches. We used state of the art statistical approaches (such as conditional empirical Bayes estimation) to aggregate the perceptions of neighborhood characteristics (as reported by MESA participants supplemented by other residents) in order to create more valid and reliable estimates of the underlying objective characteristics of interest. The use of a supplemental community survey increased the sample size per neighborhood resulting in more reliable estimates and the aggregation across multiple respondents eliminated the possibility of same source bias which may affect estimates of associations when individual perception of neighborhood attributes are investigated in relation to self-rated health.
Our results are consistent with a measurable impact of specific features of neighborhood context on global self-reported physical health. This impact is likely the result of the accumulation of the many different pathways through which neighborhood context shapes behaviors, stress and related health outcomes. Longitudinal studies and quasi-experimental studies are necessary to establish causation and identify the most effective interventions and policies.
Highlights.
Neighborhood walkability is more strongly associated with physical health than neighborhood sociability or neighborhood poverty
Physical health was associated with neighborhood walkability more strongly in those with lower income levels
Mental health was associated with neighborhood sociability only in those not employed.
Acknowledgments
This work is supported by R01 HL071759 (Diez-Roux). MESA is supported by Contracts N01-HC-95159 through N01-HC-95165 and N01-HC-95169 from the National Heart, Lung, and Blood Institute. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at/http://www.mesanhlbi.org/. Dr. Tomey was supported by an NIH grant K01 AG039554-02 (Tomey).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ana V. Diez Roux, Email: adiezrou@umich.edu.
Philippa Clarke, Email: pjclarke@umich.edu.
Teresa Seeman, Email: TSeeman@mednet.ucla.edu.
References
- ALONSO J, FERRER M, GANDEK B, WARE JE, JR, AARONSON NK, MOSCONI P, RASMUSSEN NK, BULLINGER M, FUKUHARA S, KAASA S, LEPLEGE A. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Quality of life research: an international journal of quality of life aspects of treatment, care and rehabilitation. 2004;13:283–98. doi: 10.1023/b:qure.0000018472.46236.05. [DOI] [PubMed] [Google Scholar]
- AUCHINCLOSS AH, DIEZ ROUX AV, MUJAHID MS, SHEN M, BERTONI AG, CARNETHON MR. Neighborhood resources for physical activity and healthy foods and incidence of type 2 diabetes mellitus: the Multi-Ethnic study of Atherosclerosis. Archives of internal medicine. 2009;169:1698–704. doi: 10.1001/archinternmed.2009.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BECARES L, NAZROO J, ALBOR C, CHANDOLA T, STAFFORD M. Examining the differential association between self-rated health and area deprivation among white British and ethnic minority people in England. Social science & medicine. 2012;74:616–24. doi: 10.1016/j.socscimed.2011.11.007. [DOI] [PubMed] [Google Scholar]
- BENYAMINI Y, LEVENTHAL EA, LEVENTHAL H. Self-assessments of health - What do people know that predicts their mortality? Research on Aging. 1999;21:477–500. [Google Scholar]
- BILD DE, BLUEMKE DA, BURKE GL, DETRANO R, DIEZ ROUX AV, FOLSOM AR, GREENLAND P, JACOB DR, JR, KRONMAL R, LIU K, NELSON JC, O’LEARY D, SAAD MF, SHEA S, SZKLO M, TRACY RP. Multi-ethnic study of atherosclerosis: objectives and design. American journal of epidemiology. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- BOND L, KEARNS A, MASON P, TANNAHILL C, EGAN M, WHITELY E. Exploring the relationships between housing, neighbourhoods and mental wellbeing for residents of deprived areas. BMC public health. 2012;12:48. doi: 10.1186/1471-2458-12-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BRENNAN SL, TURRELL G. Neighborhood disadvantage, individual-level socioeconomic position, and self-reported chronic arthritis: a cross-sectional multilevel study. Arthritis care & research. 2012;64:721–8. doi: 10.1002/acr.21590. [DOI] [PubMed] [Google Scholar]
- BUREAU, U. C. Census 2000 Summary Summary File 3 – United States/prepared by the U.S. Census Bureau. 2001. [Google Scholar]
- CHEAK-ZAMORA NC, WYRWICH KW, MCBRIDE TD. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Quality of life research: an international journal of quality of life aspects of treatment, care and rehabilitation. 2009;18:727–35. doi: 10.1007/s11136-009-9483-1. [DOI] [PubMed] [Google Scholar]
- CHOI NG, SCHLICHTING-RAY L. Predictors of transitions in disease and disability in pre- and early-retirement populations. Journal of aging and health. 2001;13:379–409. doi: 10.1177/089826430101300304. [DOI] [PubMed] [Google Scholar]
- COLLINS PA, HAYES MV, OLIVER LN. Neighbourhood quality and self-rated health: a survey of eight suburban neighbourhoods in the Vancouver Census Metropolitan Area. Health & place. 2009;15:156–64. doi: 10.1016/j.healthplace.2008.03.008. [DOI] [PubMed] [Google Scholar]
- CUMMINS S, STAFFORD M, MACINTYRE S, MARMOT M, ELLAWAY A. Neighbourhood environment and its association with self rated health: evidence from Scotland and England. Journal of epidemiology and community health. 2005;59:207–13. doi: 10.1136/jech.2003.016147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DE VRIES S, VERHEIJ RA, GROENEWEGEN PP, SPREEUWENBERG P. Natural environments -- healthy environments? An exploratory analysis of the relationship between greenspace and health. Environment and Planning A. 2003;35:1717–1731. [Google Scholar]
- DING D, GEBEL K. Built environment, physical activity, and obesity: what have we learned from reviewing the literature? Health & place. 2012;18:100–5. doi: 10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- FONE D, DUNSTAN F, LLOYD K, WILLIAMS G, WATKINS J, PALMER S. Does social cohesion modify the association between area income deprivation and mental health? A multilevel analysis. International journal of epidemiology. 2007a;36:338–45. doi: 10.1093/ije/dym004. [DOI] [PubMed] [Google Scholar]
- FONE DL, LLOYD K, DUNSTAN FD. Measuring the neighbourhood using UK benefits data: a multilevel analysis of mental health status. BMC public health. 2007b;7:69. doi: 10.1186/1471-2458-7-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GALE CR, DENNISON EM, COOPER C, SAYER AA. Neighbourhood environment and positive mental health in older people: the Hertfordshire Cohort Study. Health & place. 2011;17:867–74. doi: 10.1016/j.healthplace.2011.05.003. [DOI] [PubMed] [Google Scholar]
- GANDEK B, WARE JE, AARONSON NK, APOLONE G, BJORNER JB, BRAZIER JE, BULLINGER M, KAASA S, LEPLEGE A, PRIETO L, SULLIVAN M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. Journal of clinical epidemiology. 1998;51:1171–8. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- GENUTH S, ALBERTI KG, BENNETT P, BUSE J, DEFRONZO R, KAHN R, KITZMILLER J, KNOWLER WC, LEBOVITZ H, LERNMARK A, NATHAN D, PALMER J, RIZZA R, SAUDEK C, SHAW J, STEFFES M, STERN M, TUOMILEHTO J, ZIMMET P. Follow-up report on the diagnosis of diabetes mellitus. Diabetes care. 2003;26:3160–7. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- GIDLOW C, COCHRANE T, DAVEY RC, SMITH G, FAIRBURN J. Relative importance of physical and social aspects of perceived neighbourhood environment for self-reported health. Preventive medicine. 2010;51:157–63. doi: 10.1016/j.ypmed.2010.05.006. [DOI] [PubMed] [Google Scholar]
- GIORDANO GN, LINDSTROM M. The impact of changes in different aspects of social capital and material conditions on self-rated health over time: a longitudinal cohort study. Social science & medicine. 2010;70:700–10. doi: 10.1016/j.socscimed.2009.10.044. [DOI] [PubMed] [Google Scholar]
- KARASEK D, AHERN J, GALEA S. Social norms, collective efficacy, and smoking cessation in urban neighborhoods. American journal of public health. 2012;102:343–51. doi: 10.2105/AJPH.2011.300364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KAVANAGH AM, BENTLEY R, TURRELL G, BROOM DH, SUBRAMANIAN SV. Does gender modify associations between self rated health and the social and economic characteristics of local environments? Journal of epidemiology and community health. 2006;60:490–5. doi: 10.1136/jech.2005.043562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KIM D. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiologic reviews. 2008;30:101–17. doi: 10.1093/epirev/mxn009. [DOI] [PubMed] [Google Scholar]
- KING D. Neighborhood and individual factors in activity in older adults: results from the neighborhood and senior health study. Journal of aging and physical activity. 2008;16:144–70. doi: 10.1123/japa.16.2.144. [DOI] [PubMed] [Google Scholar]
- LEE Y. The predictive value of self assessed general, physical, and mental health on functional decline and mortality in older adults. Journal of epidemiology and community health. 2000;54:123–9. doi: 10.1136/jech.54.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LIANG KY, ZEGER SL. Longitudinal Data-Analysis Using Generalized Linear-Models. Biometrika. 1986;73:13–22. [Google Scholar]
- MAAS J, VERHEIJ RA, GROENEWEGEN PP, DE VRIES S, SPREEUWENBERG P. Green space, urbanity, and health: how strong is the relation? Journal of epidemiology and community health. 2006;60:587–92. doi: 10.1136/jech.2005.043125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAIR C, DIEZ ROUX AV, GALEA S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. Journal of epidemiology and community health. 2008;62:940–6. 8. doi: 10.1136/jech.2007.066605. following 946. [DOI] [PubMed] [Google Scholar]
- MAIR C, DIEZ ROUX AV, SHEN M, SHEA S, SEEMAN T, ECHEVERRIA S, O’MEARA ES. Cross-sectional and longitudinal associations of neighborhood cohesion and stressors with depressive symptoms in the multiethnic study of atherosclerosis. Annals of epidemiology. 2009;19:49–57. doi: 10.1016/j.annepidem.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MCNEILL LH, KREUTER MW, SUBRAMANIAN SV. Social environment and physical activity: a review of concepts and evidence. Social science & medicine. 2006;63:1011–22. doi: 10.1016/j.socscimed.2006.03.012. [DOI] [PubMed] [Google Scholar]
- MOLARIUS A, BERGLUND K, ERIKSSON C, LAMBE M, NORDSTROM E, ERIKSSON HG, FELDMAN I. Socioeconomic conditions, lifestyle factors, and self-rated health among men and women in Sweden. European journal of public health. 2007;17:125–33. doi: 10.1093/eurpub/ckl070. [DOI] [PubMed] [Google Scholar]
- MOLARIUS A, JANSON S. Self-rated health, chronic diseases, and symptoms among middle-aged and elderly men and women. Journal of clinical epidemiology. 2002;55:364–70. doi: 10.1016/s0895-4356(01)00491-7. [DOI] [PubMed] [Google Scholar]
- MOORE LV, DIEZ ROUX AV, NETTLETON JA, JACOBS DR, FRANCO M. Fast-food consumption, diet quality, and neighborhood exposure to fast food: the multi-ethnic study of atherosclerosis. American journal of epidemiology. 2009;170:29–36. doi: 10.1093/aje/kwp090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MUJAHID MS, DIEZ ROUX AV, MORENOFF JD, RAGHUNATHAN T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. American journal of epidemiology. 2007;165:858–67. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- MUJAHID MS, DIEZ ROUX AV, MORENOFF JD, RAGHUNATHAN TE, COOPER RS, NI H, SHEA S. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–8. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- POORTINGA W, DUNSTAN FD, FONE DL. Neighbourhood deprivation and self-rated health: the role of perceptions of the neighbourhood and of housing problems. Health & place. 2008;14:562–75. doi: 10.1016/j.healthplace.2007.10.003. [DOI] [PubMed] [Google Scholar]
- STAFFORD M, GIMENO D, MARMOT MG. Neighbourhood characteristics and trajectories of health functioning: a multilevel prospective analysis. European journal of public health. 2008;18:604–10. doi: 10.1093/eurpub/ckn091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STAFFORD M, MARTIKAINEN P, LAHELMA E, MARMOT M. Neighbourhoods and self rated health: a comparison of public sector employees in London and Helsinki. Journal of epidemiology and community health. 2004;58:772–8. doi: 10.1136/jech.2003.015941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VAN JAARSVELD CH, MILES A, WARDLE J. Pathways from deprivation to health differed between individual and neighborhood-based indices. Journal of clinical epidemiology. 2007;60:712–9. doi: 10.1016/j.jclinepi.2006.10.005. [DOI] [PubMed] [Google Scholar]
- VERHAEGHE PP, TAMPUBOLON G. Individual social capital, neighbourhood deprivation, and self-rated health in England. Social science & medicine. 2012;75:349–57. doi: 10.1016/j.socscimed.2012.02.057. [DOI] [PubMed] [Google Scholar]
- WARE J, JR, KOSINSKI M, KELLER SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- WARE JE, KOSINSKI M, KELLER SD NEW ENGLAND MEDICAL CENTER, H. SF-12: how to score the SF-12 physical and mental health summary scales. Boston, Mass: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- WEDEN MM, CARPIANO RM, ROBERT SA. Subjective and objective neighborhood characteristics and adult health. Social science & medicine. 2008;66:1256–70. doi: 10.1016/j.socscimed.2007.11.041. [DOI] [PubMed] [Google Scholar]
- WEICH S, TWIGG L, HOLT G, LEWIS G, JONES K. Contextual risk factors for the common mental disorders in Britain: a multilevel investigation of the effects of place. Journal of epidemiology and community health. 2003;57:616–21. doi: 10.1136/jech.57.8.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WEN M, BROWNING CR, CAGNEY KA. Poverty, affluence, and income inequality: neighborhood economic structure and its implications for health. Social science & medicine. 2003;57:843–60. doi: 10.1016/s0277-9536(02)00457-4. [DOI] [PubMed] [Google Scholar]
- WILSON K, ELLIOTT S, LAW M, EYLES J, JERRETT M, KELLER-OLAMAN S. Linking perceptions of neighbourhood to health in Hamilton, Canada. Journal of epidemiology and community health. 2004;58:192–8. doi: 10.1136/jech.2003.014308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WONG IO, COWLING BJ, LO SV, LEUNG GM. A multilevel analysis of the effects of neighbourhood income inequality on individual self-rated health in Hong Kong. Social science & medicine. 2009;68:124–32. doi: 10.1016/j.socscimed.2008.09.064. [DOI] [PubMed] [Google Scholar]