Abstract
People who have cardiovascular disease are at increased risk of hospitalization or death associated with influenza infection, and are included among the high-risk groups for whom annual influenza vaccination is recommended. To measure the progress toward the national year 2000 and 2010 objectives of a 60% annual influenza vaccination of adults with high-risk conditions aged 18 to 64 years, we analyzed data from the 1997 to 2001 National Health Interview Surveys (NHIS) regarding persons with cardiovascular disease. The NHIS is an annual, cross-sectional survey representative of the U.S., noninstitutionalized, civilian population. Estimated percentages of persons with heart disease reporting influenza vaccination were relatively stable during the 1996–97 through 2000–2001 influenza seasons, with the highest levels in most groups occurring in 1999–2000: 49.2% (95% confidence interval [CI], 44.1%–54.3%) among persons aged 50 to 64 years; and 22.7% (95% CI, 18.2%–27.2%) among persons aged 18 to 49 years. Influenza vaccine coverage among adults aged 18 to 64 years with cardiovascular disease is substantially below the national objective. Multiple strategies are needed to improve vaccination coverage, such as increasing the awareness of and demand for vaccination by persons with heart disease; increasing implementation by providers of practices that have been shown to increase vaccination levels; and adopting of influenza vaccination by primary care providers and specialists as a standard of care for persons diagnosed with cardiovascular disease.
Key words: Cardiovascular diseases; health services/utilization; influenza/epidemiology/prevention & control; human; influenza vaccine; knowledge, attitudes, practice; National Health Interview Survey; patient acceptance of health care; physician's practice patterns; pneumonia; population surveillance; risk factors; United States; vaccination/utilization
Death resulting from respiratory and circulatory disease increases during annual influenza epidemics. 1,2 Among persons with cardiovascular disease, influenza infection has been associated with increased risk of hospitalization because of pneumonia and influenza 3 and with an increased risk because of a broader combined outcome, including heart failure and myocarditis, in addition to pneumonia and influenza. 4 Influenza vaccination can prevent influenza illness in 70% to 90% of healthy adults below 65 years of age. 5,6 Moreover, influenza vaccination has been associated with reductions in the risk of hospitalization for cardiac disease and respiratory disease (pneumonia or influenza) during the influenza season among persons aged 65 years and older, with or without high-risk medical conditions. 7 One observational study suggested that influenza vaccination may be associated with a reduced risk of recurrent myocardial infarction, 8 and another found no such association. 9
Influenza vaccination is recommended for persons at increased risk for complications from influenza, including all persons aged 65 years and older, and for younger persons with chronic disorders of the pulmonary or cardiovascular systems. 10 Influenza vaccination is also indicated for persons with chronic heart failure 11 and has been proposed as a performance measure for quality of care in persons who have had an acute myocardial infarction. 12
Influenza vaccination coverage is low among persons aged 18 to 64 years with high-risk conditions and has fallen considerably short of the 60% “Healthy People 2010” objective. 13,14 The purpose of this study is to analyze recent data from the National Health Interview Survey (NHIS) in order to evaluate 1) influenza vaccination coverage among adults with heart disease, 2) factors associated with vaccination, and 3) trends in vaccination.
Subjects and Methods
The NHIS, which is an annual, cross-sectional, household survey, was administered by personal interview to a nationally representative sample of the U.S., noninstitutionalized, civilian population aged 18 years and older. A randomly selected adult within each sampled household was asked to answer a detailed questionnaire. The final response rate for adults in 2001 was 74% (n = 33,326 respondents). Respondents were asked, “During the past 12 months, have you had a flu shot?” They were also asked whether they had ever been told by a doctor or other health professional that they had “coronary heart disease,” “angina, also called angina pectoris,” “a heart attack (also called myocardial infarction),” or “any kind of heart condition or heart disease (other than the ones I just asked you about).”
Using 2001 NHIS data, we assessed the prevalence of self-reported heart disease (one or more of the above heart conditions) and the percentage of persons with heart disease reporting influenza vaccination (vaccination coverage) for selected demographic, health status, and health care utilization variables, stratified by age group (18–49 and 50–64 years). We assessed trends in vaccination coverage during the 1996–97 through 2000–2001 influenza seasons by age group (18–49, 50–64, and ≥65 years) and risk group (one or more heart conditions reported vs no reported medical indication for influenza vaccination). We used responses to interviews conducted during January through June of each NHIS survey year from 1997 through 2001 to estimate influenza vaccination coverage for the influenza season beginning the previous fall.
Respondents who refused to answer the influenza vaccination question or did not know their status were excluded from estimation of vaccination coverage (<1.5%). The data were adjusted for nonresponse and weighted to provide national estimates. The SUDAAN software (Research Triangle Institute; Research Triangle Park, NC) was used to calculate point estimates and 95% confidence intervals (95% CI), and to assess the associations of vaccination status with selected variables.
Results
The prevalence of self-reported heart disease in 2001 was 5.3% (95% confidence interval [CI], 4.9%–5.7%) among persons aged 18 to 49 years, 15.3% (95% CI, 14.2%–16.4%) among persons aged 50 to 64 years, and 31.7% (95% CI, 30.4%–33.0%) among those 65 and older.
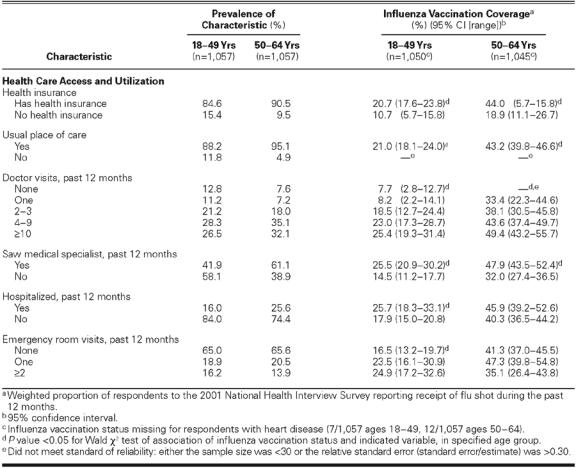
Among persons aged 18 to 64 years with heart disease, more than 80% had health insurance, more than 80% had a usual place of care, more than half reported at least 4 doctor visits during the past 12 months, and 42% to 61% had visited a medical specialist during the past 12 months (Tables IA and IB). Among that same age group, influenza vaccination was positively associated with the following variables: having at least 1 other medical indication for influenza vaccination, having health insurance, having a usual place of care, having visited the doctor at least 4 times during the past year, and having seen a medical specialist during the past 12 months (Table I). Among persons aged 18 to 49 years, hospitalization during the past 12 months and at least 1 emergency room visit during the past 12 months were also positively associated with influenza vaccination. Among persons aged 50 to 64 years, non-Hispanic whites were more likely than non-Hispanic blacks or Hispanics to have been vaccinated, and persons not in the work force were more likely than those employed to have been vaccinated. None of the demographic variables listed in Table I were associated with influenza vaccination in the younger adults (aged 18–49) who had heart disease.
TABLE IA. Reported Demographic and Health Characteristics and Influenza Vaccination Coverage in Persons Aged 18–64 Years with Heart Disease, by Age Group, United States; 2001 National Health Interview Survey
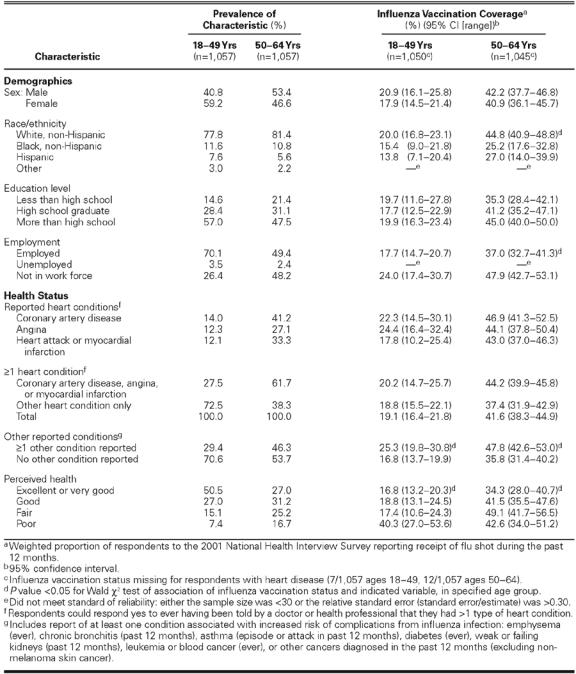
TABLE IB. Reported Health Care Access and Utilization Characteristics and Influenza Vaccination Coverage in Persons Aged 18–64 Years with Heart Disease, by Age Group, United States; 2001 National Health Interview Survey
Estimated influenza vaccination coverage in age-specific subgroups of persons with heart disease or with no reported high-risk condition varied by less than 11% from the 1996–97 through 2000–2001 influenza seasons, with a steady increase observed from 1996–97 through 1999–2000 among persons aged 50 to 64 years, and a drop in coverage of 3 to 7 percentage points from the 1999–2000 to the 2000–2001 season in each subgroup (Fig. 1). Each year, higher coverage was associated with increasing age and with high-risk conditions. The highest coverage occurred during the 1999–2000 season in most subgroups: among persons with heart disease, coverage for this season was 76.7% (95% CI, 73.5%–79.9%) for persons aged 65 years and older, 49.2% (95% CI, 44.1%–54.3%) for per-sons aged 50 to 64 years, and 22.7% (95% CI, 18.2%– 27.2%) for those aged 18 to 49 years.
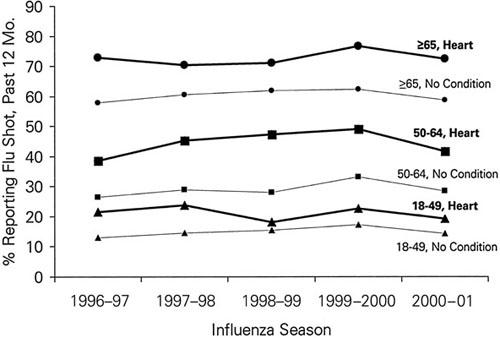
Fig. 1 Percentage of persons reporting receipt of influenza vaccination during the past 12 months, by age group and medical status, 1996–97 through 2000–2001 influenza seasons, United States. Persons with heart disease reported one or more cardiovascular conditions; other persons with no conditions did not report any medical indication for influenza vaccination asked on the survey: emphysema (ever), chronic bronchitis (past 12 months), asthma (episode or attack in past 12 months), diabetes (ever), weak or failing kidneys (past 12 months), leukemia or blood cancer (ever), or other cancers diagnosed in the past 12 months (excluding non-melanoma skin cancer). Vaccination coverages per influenza season were estimated using interviews from January through June of the 1997–2001 National Health Interview Surveys.
Discussion
In this study, persons with heart disease were more likely to be vaccinated than were persons within the same age group without any reported condition associated with increased risk of influenza complications. Moreover, we found that the likelihood of influen-za vaccination among persons with heart disease increased substantially with age. Nevertheless, vaccination coverage for persons with heart disease is below the national target level, particularly for adults aged 18 to 49 years. Vaccine coverage in this age group has remained stable during the past 5 years, with a slight decrease in 2000–2001 in all groups that has been attributed to delays in vaccine manufacturing and distribution. 15 Missed opportunities for vaccination may be frequent, since substantial proportions of persons who visit doctors frequently are unvaccinated.
Low vaccination coverage is attributed to a combination of factors: lack of systematic offering of vaccine to patients by physicians or providers at patient visits during the vaccination season; lack of awareness or interest in vaccination on the part of patients; and concerns and fears of patients regarding the influenza vaccine. Among persons aged 18 to 64 years with high-risk conditions who responded to a mail survey in 2001 (Healthstyles©), the most commonly reported reasons for not being vaccinated were 1) not being offered vaccine by their provider or not knowing it was needed (40%), 2) concern about side effects (22%), and 3) believing that the shot doesn't work (22%).* (Respondents could provide more than 1 reason.)
Systematic offering of vaccine by providers may be more difficult when the indications for vaccine are health conditions rather than age. Influenza vaccination is recommended for all persons aged 50 to 64 years, because 1) about one third of persons in this age group have a high-risk condition, 2) an age-based approach may be more effective in improving coverage in those at higher risk, and 3) 50- to 64-year-olds who are at lower risk can benefit from vaccination. 10 Interventions such as standing orders or provider reminders are necessary to ensure high vaccination rates; however, implementation of such interventions is infrequent. 16 Many persons with cardiac conditions see subspecialists, and subspecialists are less likely to recommend influenza vaccination than are generalists. 16 Recently published standards for the immunization of adults recommend that both primary care healthcare professionals and specialists should include routinely recommended vaccinations as part of their care. 17
We found that influenza vaccination coverage among persons with heart disease was significantly lower for blacks and Hispanics compared with whites, although the differences were not statistically significant for persons aged 18 to 49 years. Racial and ethnic disparities in influenza vaccination have been documented consistently, and these disparities persist after controlling for such factors as demographics, access to care, and utilization of care. 18,19 For Hispanics, English fluency appears to explain much of the difference; 18 however, the reasons for these disparities between blacks and whites are poorly understood. Survey findings suggest that among persons who were not vaccinated, reasons for non-vaccination were similar for blacks and whites. 20 The persistence of this disparity among persons who frequently encounter the healthcare system suggests that access to care is not a central factor explaining the disparity. Overall, we found much lower vaccination coverage for persons without health insurance, without a usual place of care, or with few recent doctor visits, indicating the importance of access to care, particularly among younger persons.
All data used in this analysis were from self-reports without validation. In addition, the specific influenza season during which the vaccination was reportedly received could not be exactly determined. The validity of self-reported influenza vaccination is considered high. 21 The validity of self-reported diabetes and hypertension is considered moderate. 21 To our knowledge, the validity of self-reported heart disease from NHIS respondents has not been evaluated.
Persons with heart disease are at increased risk of hospitalization or death resulting from influenza infection, and the benefits of influenza vaccine in preventing serious complications of influenza infection are well documented. A substantial proportion of high-risk persons aged 18 to 64 are not aware that they should be vaccinated, which highlights the importance of systematic offering of influenza vaccination by physicians. Primary care providers and cardiologists should work together to ensure that secondary prevention measures such as influenza and pneumococcal vaccination are offered to their patients with heart disease. Although changing patients' attitudes and beliefs about influenza vaccination and increasing the demand for vaccination is important, provider recommendation remains a very strong predictor of vaccination. 22
Footnotes
*CDC; unpublished data.
Address for reprints: James A. Singleton, National Immunization Program, Centers for Disease Control and Prevention, 1600 Clifton Road, N.E., MS E-61, Atlanta, GA 30333
E-mail: xzs8@cdc.gov
This paper has its basis in a presentation made atthe First Symposium on Influenza and Cardiovascular Disease: Science, Practice, and Policy, held on 26 April 2003, at the Texas Heart Institute, Houston, Texas.
References
- 1.Housworth J, Langmuir AD. Excess mortality from epidemic influenza, 1957-1966. Am J Epidemiol 1974;100:40–8. [DOI] [PubMed]
- 2.Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, Fukuda K. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA 2003;289:179–86. [DOI] [PubMed]
- 3.Barker WH, Mullooly JP. Impact of epidemic type A influenza in a defined adult population. Am J Epidemiol 1980; 112:798–811. [DOI] [PubMed]
- 4.Neuzil KM, Reed GW, Mitchel EF Jr, Griffin MR. Influenza-associated morbidity and mortality in young and middle-aged women. JAMA 1999;281:901–7. [DOI] [PubMed]
- 5.Bridges CB, Thompson WW, Meltzer MI, Reeve GR, Talamonti WJ, Cox NJ, et al. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: A randomized controlled trial. JAMA 2000;284:1655–63. [DOI] [PubMed]
- 6.Wilde JA, McMillan JA, Serwint J, Butta J, O'Riordan MA, Steinhoff MC. Effectiveness of influenza vaccine in health care professionals: a randomized trial. JAMA 1999; 281:908–13. [DOI] [PubMed]
- 7.Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt K, Iwane M. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med 2003;348:1322–32. [DOI] [PubMed]
- 8.Naghavi M, Barlas Z, Siadaty S, Naguib S, Madjid M, Casscells W. Association of influenza vaccination and reduced risk of recurrent myocardial infarction. Circulation 2000;102:3039–45. [DOI] [PubMed]
- 9.Jackson LA, Yu O, Heckbert SR, Psaty BM, Malais D, Barlow WE, et al. Influenza vaccination is not associated with a reduction in the risk of recurrent coronary events. Am J Epidemiol 2002;156:634–40. [DOI] [PubMed]
- 10.Bridges CB, Harper SA, Fukuda K, Uyeki TM, Cox NJ, Singleton JA; Advisory Committee on Immunization Practices. Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP) [published erratum appears in MMWR Morb Mortal Wkly Rep 2003;52:526]. MMWR Recomm Rep 2003; 52(RR-8):1–34. [PubMed]
- 11.Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 2001;38:2101–13. [DOI] [PubMed]
- 12.Spertus JA, Radford MJ, Every NR, Ellerbeck EF, Peterson ED, Krumholz HM; Acute Myocardial Infarction Working Group of the American Heart Association/American College of Cardiology First Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke. Challenges and opportunities in quantifying the quality of care for acute myocardial infarction: summary from the Acute Myocardial Infarction Working Group of the American Heart Association/American College of Cardiology First Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke. J Am Coll Cardiol 2003;41:1653–63. [DOI] [PubMed]
- 13.US Department of Health and Human Services, Public Health Service. Healthy People 2000: national health promotion and disease prevention objectives—full reports, with commentary. Washington, DC: US Department of Health and Human Services, Public Health Service, 1991; DHHS publication no. (PHS) 91-50212.
- 14.Singleton JA, Greby SM, Wooten KG, Walker FJ, Strikas R. Influenza, pneumococcal, and tetanus toxioid vaccination of adults—United States, 1993-7. MMWR CDC Surveill Summ 2000;49:39–62. [PubMed]
- 15.Fukuda K, O'Mara D, Singleton JA. How the delayed distribution of influenza vaccine created shortages in 2000 and 2001. Pharmacy & Therapeutics 2002;27:235–42.
- 16.Nichol K, Zimerman R. Generalist and subspecialist physicians' knowledge, attitudes, and practices regarding influenza and pneumococcal vaccinations for elderly and other high-risk patients: a nationwide survey. Arch Int Med 2001; 161:2702–8. [DOI] [PubMed]
- 17.Poland GA, Shefer AM, McCauley M, Webster PS, Whitley-Williams PN, Peter G; National Vaccine Advisory Committee, Ad Hoc Working Group for the Development of Standards for Adult Immunization Practices. Standards for adult immunization practices. Am J Prev Med 2003;25:144–50. [DOI] [PubMed]
- 18.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care 2002;40:52–9. [DOI] [PubMed]
- 19.Centers for Disease Control and Prevention (CDC). Racial/ethnic disparities in influenza and pneumococcal vaccination levels among persons aged ≥65 years—United States, 1989-2001. MMWR Morb Mortal Wkly Rep 2003;52:958–62. [PubMed]
- 20.Centers for Disease Control and Prevention (CDC). Reasons reported by Medicare beneficiaries for not receiving influenza and pneumococcal vaccinations—United States, 1996. MMWR Morb Mortal Wkly Rep 1999;48:886–90. [PubMed]
- 21.Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS). Soz Praventivmed 2001;46 Suppl 1:S3-42. [PubMed]
- 22.Nichol K, Mac Donald R, Hauge M. Factors associated with influenza and pneumococcal vaccination behavior among high-risk adults. J Gen Intern Med 1996;11:673–7. [DOI] [PubMed]


