Abstract
OBJECTIVES
There is a shortage of information on metabolic costs of daily physical activities in older adults and the effect of having mobility impairments. The primary purpose of this study was to evaluate metabolic equivalent (MET) values on common daily tasks in men and women aged > 70 years compared to normative criteria. A secondary purpose was to determine the effect of having mobility impairments.
DESIGN
Cross-sectional observational study.
SETTING
University based research clinic
PARTICIPANTS
Forty-five participants aged 70 to 90 years of age (mean: 76.3 ± 5.1) volunteered to complete 17 daily activities, each lasting 10 minutes.
MEASUREMENTS
Oxygen consumption (VO2 = ml•kg−1•min−1) was measured through a mask by a portable gas analyzer and MET values were calculated as measured VO2/3.5 ml•kg−1•min−1. Values were compared to both normative values and between participants with and without mobility impairments.
RESULTS
Compared to the established normative criteria, measured METs were different in 14 of 17 tasks performed. Compared to measured METs, normative values underestimated walking leisurely (0.87 ± 0.12 METs) walking briskly (0.87 ± 0.12 METs ), and bed making (1.07 ± 0.10 METs ), but overestimated gardening (1.46 ± 0.12 METs) and climbing stairs (0.73 ± 0.18). Participants with impairments had significantly lower METs while gardening, vacuuming/sweeping, stair climbing, and walking briskly. However, when METs were adjusted for performance speed the metabolic costs were 16–27% higher for those with mobility impairments.
CONCLUSION
Compared to normative values, metabolic costs of daily activities are substantially different in older adults and having mobility impairments increases this metabolic cost. These results may have implications for practitioners to appropriately prescribe daily physical activities for healthy and mobility impaired older adults.
Keywords: Energy expenditure, Aging, Disability, Metabolic Efficiency
INTRODUCTION
To study and prescribe appropriate daily activities for older adults, the estimated metabolic costs of specific daily activities needs to be accurate.1 Normative data for such purposes is provided by the Compendium of Physical Activities that standardizes subjective assessments by assigning a metabolic equivalent value (MET) to hundreds of activities and is used by researchers and practitioners alike.1, 2 However, little work has examined metabolic costs of daily activities in older persons.3
Metabolic costs of physical activities, particularly those that require mobility, tend to rise with increasing age.4, 5 Poor efficiency of movement exacerbated by co-activation of antagonistic muscle groups is partially responsible for elevated costs of mobility in older persons.6 However, much of this work is limited to wide age group comparisons without additional knowledge of whether impaired physical function in older persons influences metabolic cost. Studying the relationship between metabolic work and physical impairments might provide a basis to understand the declines in mobility performance or fatigue that are associated with increasing age.
To improve knowledge regarding the metabolic costs of daily activities in older adults, we set out to compare measured and estimated MET values in a sample of men and women between 70 and 90 years of age. We also aimed to evaluate differences in metabolic costs for people reporting mobility impairments. The results from this work are intended to document MET value estimates for older persons that could be used to accurately prescribe daily activities for practitioners.
METHODS
Participants and demographics
Adults 70 to 90 years of age were targeted through local mailings, flyers, and advertisements to participate in this study. Prior to participation, all participants underwent telephone and in person screening to ensure their safety of participation. Exclusions included significant head injury, severe Parkinson’s disease or neurological disorders, severe uncorrected vision or hearing impairment, extensive alcohol abuse, current use of anabolic hormones, active cancer, active cardiopulmonary disease, shortness of breath during daily normal activities, contraindications to exercise (e.g. cardiac pacemaker, implanted cardiac defibrillator), or stroke with mobility impairment. A Mini-Mental State Exam (MMSE) score of less than 23 excluded individuals with cognitive impairment (one participant was excluded on this criteria). The study was approved by the University of Florida Institutional Review Board and all participants gave written informed consent.
Participants underwent a series of questionnaires. First, the Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F) Scale (Version 4) was self-administered.7 Participants also completed the SF-12v2 Health Survey by interview-administration and normalized were reported according to established algorithms.8,9 Participants completed a disability questionnaire used in the Established Populations for Epidemiologic Studies of the Elderly.10 Duration of physical activity (minutes per day) over the past seven days was assessed by an interviewer administered questionnaire modeled from the Yale Physical Activity Survey.11 Participants reporting of any difficulty walking ¼ mile, getting up from a chair, climbing a flight of stairs, or performing light housework were categorized as mobility impaired. Participants reporting no difficulty on the tasks were categorized as not having mobility impairment.
Experimental approach
Participants were asked to perform a battery of tasks in a laboratory setting and under the supervision of a research assistant. Prior to commencing each task, participants received standardized instructions to perform the activities without overexertion. Tasks were performed for approximately 10 minutes (average amount of task performance: 9.1 ± 1.8 min) to allow a steady state metabolic rate to be reached. Participants were asked to refrain from speaking during tasks. The experiment was conducted over two days, separated by at least 3 days, to reduce fatigue (Day 1 = 7 tasks; Day 2 = 10 tasks). On the first day, participants underwent the following tasks: Standing, rapid walk, gardening, playing cards, sweeping/vacuuming, washing windows, ironing. On the second day, participants underwent the following tasks: laying down, making a bed, doing laundry, walking at a leisurely pace, conducing computer work, grocery shopping, preparing/serving food, washing dishes, raking leaves, climbing stairs. On average, participants rested 4.4 ± 3.1 minutes between each task to prevent metabolic carry over between tasks. More rest was given following tasks that resulted in higher metabolic costs (usual walk: 6.7 ± 4.0; rapid walk: 6.9 ± 2.4 min, gardening: 6.5 ± 3.0 min of rest). Rate of perceived exertion was assessed at the end of each task using the Borg CR10 RPE Scale.12
Daily Activities
Standing: Standing in place on a carpeted area and watching television.
Walking at a leisurely and rapid pace: Participants were asked to walk a distance of 400-meters at leisurely and rapid self-selected paces. The two walking tasks were performed on separate testing days to minimize fatigue.
Gardening: Participants were asked to fill ceramic pots from a soil basin, carry the pots (weight approximately 5 kg) across a 4-meter room, place on the ground and plant plastic flowers.
Playing Cards: Participants were asked to sit and play cards (e.g. solitaire or war) with the research assistant.
Sweeping/Vacuuming: Participants were first asked to perform five minutes of vacuuming a 2 × 2 meter carpet vertically and then horizontally. Then the participants transitioned to sweeping dirt debris into a dustpan and placing it into a trash bin.
Washing Windows: A 9-panel window (0.91 × 1.5 meters) was placed vertically on the floor and participants were asked to clean the window with paper towels and a spray bottle with cleaner.
Ironing: Participants used a ~1 kg iron. Ironed clothes were placed on a hanger.
Laying: Participants lied in bed without moving and without falling asleep.
Making a bed: Participants removed a set of sheets from a bed, placed them in a basket, and replacing with clean sheets. The task was repeated until time elapsed.
Laundry: Participants simulated pulling clothes from a washing machine and placing them in the dryer. Clothes removed from the dryer were placed on a table and folded.
Computer Work: Participants sat and typed a document in a word processing program.
Grocery Shopping: A course was arranged to mimic grocery shopping. Participants were asked to shop for items on a list and navigate three different rooms for these items. Once items were found, they placed them into a carrying basket (Total mass accumulated = 5 kg).
Preparing and serving food: Participants prepared and serve two peanut butter and jelly sandwiches and a smoothie.
Washing Dishes: Using a laboratory sink, participants rinsed and washed dishes by hand and placed them on drying rack.
Raking Leaves: A 10 × 10 meter carpeted space was used to conduct the raking task where pieces of paper were shredded and sprinkled across the space. The participants were asked to rake the paper into piles and place into a large box simulating a trashcan.
Stair climbing: Participants were asked to ascend and descend a flight of stairs (9 steps, step height 20 cm) at a self-selected pace without overexertion. Ascent/descent time was determined by the total number of flights completed by the number of minutes performing the task (flights per minute).
During each task, participants wore a portable Cosmed K4b2. The Cosmed weighs 1.5 kg, including the battery and specially designed harness and has been validated against Douglas bags during steady-state exercise.13 Prior to data collection, the oxygen and carbon dioxide sensors were calibrated using a gas mixture sample of 16.0% Oxygen and 5.0% Carbon dioxide, and a room air calibration. The turbine flow meter was calibrated using a 3.0-liter syringe. A flexible facemask was positioned over the participant’s mouth and nose and attached to the flow meter. Oxygen consumption (VO2 = ml•kg−1•min−1) was measured breath-by-breath and subsequently averaged over 10-second periods. Data cleaning revealed 83 of the 763 tests performed did not meet quality control standards. Most errors occurred in sedentary tasks: standing, playing cards, laying and computer work. Previous studies have noted this potential limitation of the equipment in low metabolically demanding tasks.14
Data analysis
Baseline characteristics and comparisons across groups were evaluated using Chi-square for categorical variables and analysis of variance (ANOVA) for continuous variables. Differences between MET values of the Compendium of Physical Activities and measured METs were tested using t-test’s by setting the Compendium as a constant value. Type-I error correction was performed with Holm’s procedure.15 Comparisons of METs between groups were performed using a 2-way ANOVA where the task and group served as fixed variables. A significant group by task interaction was found (p<0.001) and Tukey’s-Honestly Significant Difference (HSD) post-hoc tests were conducted to evaluate group differences. Metabolic costs were adjusted for speed by creating a ratio of MET/speed for walking and stair climbing tasks. This calculation allowed for an understanding of whether physical impairment alters the energy cost of performing an activity despite performance speed. This approach is similar to biomechanics studies that estimated metabolic costs of walking while manipulation or adjusting for task speed.16 Differences in metabolic costs were determined using analysis of covariance (ANCOVA) adding covariates of body mass index, history of cardiovascular disease and current osteoarthritis. Values are presented as means ± standard deviation unless otherwise noted.
RESULTS
The descriptive statistics are listed in table 1. The participants were of average body mass, cognition and had at least one prevalent disease condition. Individuals reporting mobility impairments were significantly older and were more likely to have a history of cardiovascular conditions than participants not reporting impairments. Scores on the physical component of the SF-12v2 were lower in participants reporting mobility impairments compared to the group without impairments. Additionally, participants reporting mobility impairments had slower walking (20% for usual & 27% for rapid paces) and stair-climbing speeds (13%) than individuals without impairments. Self-reported physical activity levels were marginally higher in the participants without impairments, but these were not statistically different.
Table 1.
Descriptive Statistics for the 70–87 year olds.
| Total (n=45) | Not impaired (n=31) | Mobility impaired (n=14) |
P-value for difference in impairment status |
|
|---|---|---|---|---|
| Female, % (n) | 55.5 (25) | 38.7 (19) | 57.1 (6) | 0.249 |
| Age in years | 76.3 ± 5.1 | 75 ± 4.4 | 79.3 ± 5.2 | 0.006* |
| BMI (kg/m2) | 26.7 ± 3.8 | 26.5 ± 3.9 | 27.2 ± 3.8 | 0.595 |
| MMSE score | 28.5 ± 1.4 | 28.8 ± 1.4 | 27.9 ± 1.4 | 0.063 |
| Education (Years of school completed) | 14.4 ± 4.9 | 15.1 ± 4.9 | 13.1 ± 4.9 | 0.223 |
| FACIT composite score | 45.7 ± 6.3 | 46.1 ± 6.4 | 44.9 ± 6.3 | 0.537 |
| SF-12v2 physical composite summary score | 48.9 ± 7.7 | 51.7 ± 5.6 | 42.8 ± 8.5 | 0.001* |
| SF-12v2 mental composite summary score | 56.3 ± 6.8 | 56.2 ± 4.9 | 56.6 ± 10.2 | 0.855 |
| 400 meter rapid walk speed (meter/sec) | 1.1 ± 0.25 | 1.3 ± 0.19 | 0.96 ± 0.22 | <0.001* |
| 400 meter usual walking speed (meter/sec) | 1.0 ± 0.18 | 1.1 ± 0.12 | 0.87 ± 0.18 | <0.001* |
| Stair-climbing speed (flights/min) | 2.5 ± 0.72 | 2.7 ± 0.67 | 2.1 ± 0.67 | 0.007* |
| Total physical activity minutes per day (min) | 32.5 ± 27.3 | 37.0 ± 27.9 | 21.9 ± 23.3 | 0.094 |
| History of cardiovascular disease, % (n) | 17.4 (8) | 9.7 (3) | 35.7 (5) | 0.034* |
| Diabetes, % (n) | 6.6 (3) | 6.4 (2) | 7.1 (1) | 0.931 |
| Osteoarthritis, % (n) | 32.6 (15) | 35.5 (11) | 28.5 (4) | 0.649 |
| History of cancer, % (n) | 15.2 (7) | 16.1 (5) | 14.3 (2) | 0.874 |
| Hypertension, % (n) | 23.9 (11) | 25.8 (8) | 21.4 (3) | 0.752 |
| Osteoporosis, % (n) | 6.5 (3) | 9.7 (3) | 0 (0) | 0.228 |
| Total number of disease conditions | 1.0 ± 0.80 | 1.0 ± 0.83 | 1.1 ± 0.73 | 0.881 |
p-value < 0.05
BMI = Body Mass Index
Participants reporting of any difficulty walking ¼ mile, getting up from a chair, climbing a flight of stairs, or performing light housework were categorized as mobility impaired.
The metabolic costs measured for each task are compared with the predicted metabolic costs from the Compendium of Physical Activities in Table 2. Walking briskly (P=0.001), bed-making, laundry, and walking leisurely had significantly higher MET values than predicted. In contrast, gardening, playing cards, washing windows, ironing, lying in bed, working on the computer, preparing/serving food, washing dishes, raking leaves, and stair-climbing were significantly lower than predicted.
Table 2.
Comparison of estimated and measured metabolic equivalents (MET) across 17 daily activities in adults 70–87 years of age.
| Activity | N | VO2 (ml/kg/min) |
Measured METS |
Estimated METS† |
Estimated minus measured MET° |
Estimated vs. measured METs P-value |
RPE |
|---|---|---|---|---|---|---|---|
| Standing | 30 | 3.67 ± 0.90 | 1.03 ± 0.23 | 1.0 | −0.03 ± 0.04 | 0.430 | 1.09 ± 1.66 |
| Walking briskly | 39 | 15.11 ± 4.18 | 4.28 ± 1.09 | 3.0‡ | −1.28 ± 0.17 | 0.001* | 2.48 ± 1.87 |
| Gardening | 40 | 8.92 ± 3.03 | 2.53 ± 0.75 | 4.0 | 1.46 ± 0.12 | <0.001* | 2.21 ± 2.06 |
| Playing cards | 32 | 4.06 ± 1.08 | 1.15 ± 0.28 | 1.5 | 0.35 ± 0.05 | <0.001* | N/A |
| Sweeping / Vacuuming | 41 | 11.84 ± 2.99 | 3.37 ± 0.75 | 3.65 | 0.28 ± 0.12 | 0.022 | 2.89 ± 2.15 |
| Washing windows | 41 | 8.01 ± 2.27 | 2.28 ± 0.57 | 3.0 | 0.72 ± 0.09 | <0.001* | 2.50 ± 2.00 |
| Ironing | 40 | 6.97 ± 1.63 | 1.99 ± 0.43 | 2.3 | 0.31 ± 0.07 | <0.001* | 1.89 ± 1.69 |
| Lying in bed | 28 | 3.17 ± 0.52 | 0.89 ± 0.12 | 1.0 | 0.11 ± 0.02 | <0.001* | N/A |
| Making the bed | 44 | 10.88 ± 2.53 | 3.07 ± 0.70 | 2.0 | −1.07 ± 0.10 | <0.001* | 2.11 ± 1.39 |
| Doing Laundry | 43 | 8.86 ± 2.07 | 2.50 ± 0.57 | 2.15 | −0.35 ± 0.09 | <0.001* | 2.19 ± 1.28 |
| Walking leisurely | 44 | 11.97 ± 2.84 | 3.38 ± 0.79 | 2.5‡ | −0.87 ± 0.12 | <0.001* | 2.15 ± 2.02 |
| Computer work | 40 | 3.86 ± 0.78 | 1.09 ± 0.20 | 1.8 | 0.71 ± 0.03 | <0.001* | N/A |
| Grocery shopping | 45 | 9.50 ± 2.00 | 2.68 ± 0.56 | 2.5 | −0.18 ± 0.08 | 0.033 | 2.60 ± 2.29 |
| Preparing / serving food | 45 | 6.13 ± 1.46 | 1.73 ± 0.39 | 2.25 | 0.52 ± 0.06 | <0.001* | 1.41 ± 1.45 |
| Washing dishes | 45 | 6.54 ± 1.50 | 1.84 ± 0.40 | 2.3 | 0.45 ± 0.06 | <0.001* | 1.76 ± 1.67 |
| Raking leaves | 45 | 10.14 ± 2.56 | 2.86 ± 0.67 | 4.15 | 1.29 ± 0.09 | <0.001* | 3.31 ± 2.10 |
| Stair climbing | 40 | 16.94 ± 4.21 | 4.77 ± 1.14 | 5.5 | 0.73 ± 0.18 | <0.001* | 5.27 ± 2.63 |
Note: mobility impairment defined as reporting of any difficulty walking ¼ mile, getting up from a chair, climbing a flight of stairs, or performing light housework.
Estimated METs taken from Ainsworth et al. 1
Difference calculated for each participant = (estimated MET – measured MET)
Estimated and predicted values are significantly different after adjusting for multiple comparison testing using the Holms procedure: p < 0.05.
Values estimated for self-selected walking speed at: rapid = 1.1 m/sec (2.5 mph) and leisurely = 1.0 m/sec (2.0 mph)
RPE: Rating of perceived exertion. Scale range: 0 to 10 with 10 being the most exertion.
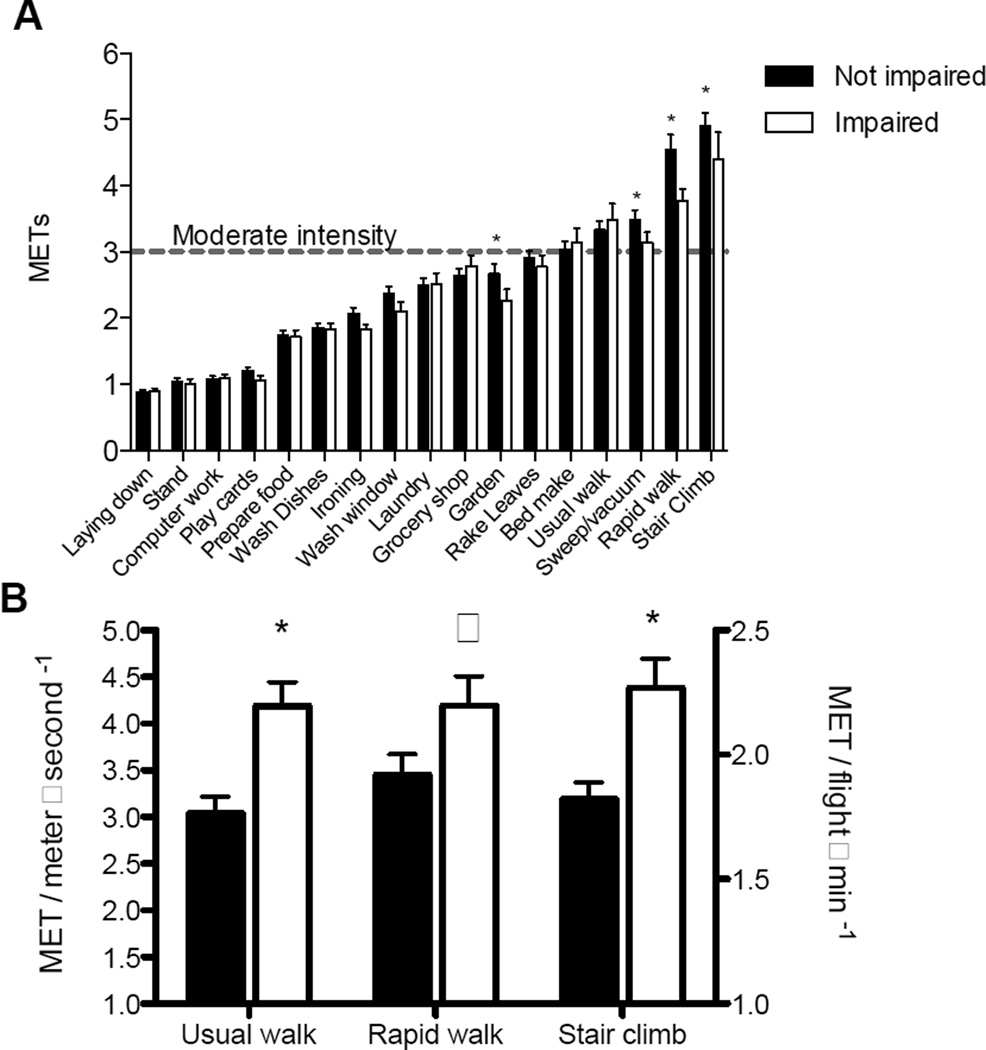
Those who reported mobility impairments had on average lower MET values for brisk walking (17%), stair climbing (10%), sweeping/vacuuming (10.1%), and gardening (15%) compared to participants without impairment (Figure 1A). Data in Figure 1B demonstrate that older adults who report mobility impairments have higher metabolic costs relative to their performance speed. After adjustment for body mass index, history of cardiovascular disease and current osteoarthritis MET values normalized for speed were significantly elevated with rapid pace walking and stair ascending/descending for participants reporting mobility impairments.
Figure 1.
A.) Absolute metabolic equivalent values separated into individuals who self-reported mobility impairment or no impairment performing mobility tasks. B.) Metabolic equivalents (MET) normalized for self-selected rapid and usual walking speed (meters per sec) and stair climbing speed (flight per minute). Values for 1B are predicted means and standard errors adjusted for body mass index, history of cardiovascular disease and current osteoarthritis. Mobility impairment defined as reporting of any difficulty walking ¼ mile, getting up from a chair, climbing a flight of stairs, or performing light housework. *p-value < 0.05, ^ p-value = 0.07.
DISCUSSION
The results from this study provide new information regarding the metabolic costs of common daily activities for individuals >70 years old in comparison to normative data provided by the Compendium of Physical activities. The data suggests that MET values of older persons are distinctly different than those estimated in the Compendium. Additionally, older persons who report physical impairments have lower absolute MET values when performing walking, vacuuming/sweeping and gardening tasks. However, when MET values were adjusted for performance speed, older adults with mobility impairments have increased metabolic costs.
The Compendium of Physical Activities was created as a tool for clinicians and scientists to easily estimate the metabolic demand of common physical activities. However, very little research has compared the estimates across different age groups and populations. Fourteen out of 17 tasks performed were significantly different than estimated by the Compendium. While this may seem extreme, it was made clear in the original publication by Ainsworth and colleagues 1 that correction factors for different populations would need to be created to adjust MET values accordingly. Several household tasks were overestimated by the Compendium that included shopping, gardening, playing cards, washing windows, lying in bed, computer work, serving food, washing dishes, raking leaves and climbing stairs. There are a number of explanations for these deviations that might not be age-related. For example, tasks were performed in a controlled laboratory that is often associated with lower metabolic costs compared to home environments.17,18 Additionally, we did not control the speed of movement that is known to influence MET values and we would expect that older adults move more slowly during task performance causing underestimated values. Regarding lower METs while lying, there are several publications suggesting that resting metabolic rate (RMR) is significantly lower in older adults and thus future studies should consider normalizing to measured RMR as opposed to standardized values (i.e. 3.5 ml/kg/min).19
Other studies of older adult with co-mobidities have demonstrated similar results to the current study.4,6,17 In one study, the Compendium overestimated measured MET values during vacuuming, washing dishes, and bed making in older women with a history of cardiovascular disease, at magnitudes similar to the current study (bed making = 3.42, vacuuming = 2.7, washing dishes = 1.8, ironing = 1.9 METs).20 These observations are not limited to older adults; a recent study in a large sample of young to middle-aged adults found that gardening and painting were underestimated by the Compendium.3
There is an abundance of literature suggesting that older adults having elevated metabolic costs of walking at speeds ranging from very slow to fast.21–23 The data from the current study suggest that metabolic costs of walking are elevated with mobility impairments independent of the side effects of overt disease conditions. This finding has important implications on how certain daily activities are prescribed for lower functioning older adults where the metabolic costs reach a significant physiological effort.
This study has a number of limitations. It did not include a control group of young individuals, and therefore it cannot be determined whether the discordance between measured and estimated MET levels is due to age. To determine whether the Compendium values should be adjusted for adults 70+ years and older, it will be necessary for younger and older adults to be tested under identical methodological conditions. Additionally, all activities were performed in a laboratory setting and MET values might not translate to participant’s ordinary environment.17,18 Metabolic costs corrected for performance speed were not calculated for most of the tasks because no standardized unit for distance could be derived. As an example, determining the number of dishes per minute would require a more standardized approach that ensured everyone washed the same sized dishes in a specific order. Instead, we chose a more ecologically valid experiment to help improve the generalizability of the findings.
Older adults reporting mobility impairments have lower absolute MET levels, but higher relative MET costs adjusted for performance speed. This indicates that mobility impairments increase the physiological effort of performing mobility tasks. These results are important for appropriately recommending the intensity and duration of daily activities for older adults. Further research is necessary to determine whether differences between measures versus normative MET values on common daily tasks can be attributable to age-associated physiological changes.
Acknowledgments
Sponsor’s Role: This research was supported by the Paffenbarger-Blair Fund for Epidemiological Research on Physical Activity from the American College of Sports Medicine Foundation. Todd Manini was partially supported by NIA Claude D. Pepper Center P30AG. The results of the present study do not constitute endorsement by the American College of Sports Medicine.
Footnotes
The authors report no conflict of interest.
| Elements of Financial/Personal | Jeffery Knaggs | Kelly Larkin | Todd Manini |
|---|---|---|---|
| Employment or Affiliation | No | No | No |
| No | No | No | |
| Grants/Funds | No | No | No |
| No | No | No | |
| Honoraria | No | No | No |
| No | No | No | |
| Speaker Forum | No | No | No |
| No | No | No | |
| Consultant | No | No | No |
| No | No | No | |
| Stocks | No | No | No |
| No | No | No | |
| Royalties | No | No | No |
| No | No | No | |
| Expert Testimony | No | No | No |
| No | No | No | |
| Board Member | No | No | No |
| No | No | No | |
| Patents | No | No | No |
| No | No | No | |
| Personal Relationship | No | No | No |
Authors contributions.
Study concept & Design: Manini
Data collection & analysis: Knaggs, Larkin & Manini
Manuscript writing: Manini, Knaggs, & Larkin
REFERENCES
- 1.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 2.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Kozey SL, Lyden K, Howe CA, Staudenmayer JW, Freedson PS. Accelerometer Output and MET Values of Common Physical Activities. Med Sci Sports Exerc. 2010 doi: 10.1249/MSS.0b013e3181d479f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones LM, Waters DL, Legge M. Walking speed at self-selected exercise pace is lower but energy cost higher in older versus younger women. J Phys Act Health. 2009;6:327–332. doi: 10.1123/jpah.6.3.327. [DOI] [PubMed] [Google Scholar]
- 5.Voorrips LE, van Acker TM, Deurenberg P, van Staveren WA. Energy expenditure at rest and during standardized activities: a comparison between elderly and middle-aged women. Am J Clin Nutr. 1993;58:15–20. doi: 10.1093/ajcn/58.1.15. [DOI] [PubMed] [Google Scholar]
- 6.Mian OS, Thom JM, Ardigo LP, Narici MV, Minetti AE. Metabolic cost, mechanical work, and efficiency during walking in young and older men. Acta physiologica (Oxford, England) 2006;186:127–139. doi: 10.1111/j.1748-1716.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- 7.Bonomi AE, Cella DF, Hahn EA, et al. Multilingual translation of the Functional Assessment of Cancer Therapy (FACT) quality of life measurement system. Qual Life Res. 1996;5:309–320. doi: 10.1007/BF00433915. [DOI] [PubMed] [Google Scholar]
- 8.Resnick B, Nahm ES. Reliability and validity testing of the revised 12-item Short-Form Health Survey in older adults. J Nurs Meas. 2001;9:151–161. [PubMed] [Google Scholar]
- 9.Ware JE, Kosinski M, Turner-Bowker DM, Gandek B, Keller SD. How to score version-2 of the SF-12 Health Survey (With a Supplement Documenting Version 1) Lincoln, RI: Quality Metric Incorporated; 2002. [Google Scholar]
- 10.Cornoni-Huntley J, Ostfeld AM, Taylor JO, et al. Established populations for epidemiologic studies of the elderly: study design and methodology. Aging (Milano) 1993;5:27–37. doi: 10.1007/BF03324123. [DOI] [PubMed] [Google Scholar]
- 11.Dipietro L, Caspersen CJ, Ostfeld AM, Nadel ER. A survey for assessing physical activity among older adults. Med Sci Sports Exerc. 1993;25:628–642. [PubMed] [Google Scholar]
- 12.Borg G. Perceived exertion and pain scales. Champaign IL: Human Kinetics; 1988. [Google Scholar]
- 13.McLaughlin JE, King GA, Howley ET, Bassett DR, Jr, Ainsworth BE. Validation of the COSMED K4 b2 portable metabolic system. Int J Sports Med. 2001;22:280–284. doi: 10.1055/s-2001-13816. [DOI] [PubMed] [Google Scholar]
- 14.Littlewood RA, White MS, Bell KL, Davies PS, Cleghorn GJ, Grote R. Comparison of the Cosmed K4 b(2) and the Deltatrac II metabolic cart in measuring resting energy expenditure in adults. Clinical nutrition (Edinburgh, Scotland) 2002;21:491–497. doi: 10.1054/clnu.2002.0580. [DOI] [PubMed] [Google Scholar]
- 15.Holm S. A simple sequentially rejective multiple test procedure. Scand J Statistics. 1979;6:65–70. [Google Scholar]
- 16.Malatesta D, Simar D, Dauvilliers Y, et al. Energy cost of walking and gait instability in healthy 65- and 80-yr-olds. J Appl Physiol. 2003;95:2248–2256. doi: 10.1152/japplphysiol.01106.2002. [DOI] [PubMed] [Google Scholar]
- 17.Gunn SM, Brooks AG, Withers RT, Gore CJ, Plummer JL, Cormack J. The energy cost of household and garden activities in 55- to 65-year-old males. Eur J Appl Physiol. 2005;94:476–486. doi: 10.1007/s00421-004-1302-3. [DOI] [PubMed] [Google Scholar]
- 18.Withers RT, Brooks AG, Gunn SM, Plummer JL, Gore CJ, Cormack J. Self-selected exercise intensity during household/garden activities and walking in 55 to 65-year-old females. Eur J Appl Physiol. 2006;97:494–504. doi: 10.1007/s00421-006-0177-x. [DOI] [PubMed] [Google Scholar]
- 19.Byrne NM, Hills AP, Hunter GR, Weinsier RL, Schutz Y. Metabolic equivalent: one size does not fit all. J Appl Physiol. 2005;99:1112–1119. doi: 10.1152/japplphysiol.00023.2004. [DOI] [PubMed] [Google Scholar]
- 20.Wilke NA, Sheldahl LM, Dougherty SM, Hanna RD, Nickele GA, Tristani FE. Energy expenditure during household tasks in women with coronary artery disease. Am J Cardiol. 1995;75:670–674. doi: 10.1016/S0002-9149(99)80651-1. [DOI] [PubMed] [Google Scholar]
- 21.Malatesta D, Simar D, Dauvilliers Y, et al. Aerobic determinants of the decline in preferred walking speed in healthy, active 65- and 80-year-olds. Pflugers Arch. 2004;447:915–921. doi: 10.1007/s00424-003-1212-y. [DOI] [PubMed] [Google Scholar]
- 22.Martin PE, Rothstein DE, Larish DD. Effects of age and physical activity status on the speed-aerobic demand relationship of walking. J Appl Physiol. 1992;73:200–206. doi: 10.1152/jappl.1992.73.1.200. [DOI] [PubMed] [Google Scholar]
- 23.Ortega JD, Fehlman LA, Farley CT. Effects of aging and arm swing on the metabolic cost of stability in human walking. J Biomech. 2008;41:3303–3308. doi: 10.1016/j.jbiomech.2008.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bendall MJ, Bassey EJ, Pearson MB. Factors affecting walking speed of elderly people. Age Ageing. 1989;18:327–332. doi: 10.1093/ageing/18.5.327. [DOI] [PubMed] [Google Scholar]
- 25.Cunningham DA, Rechnitzer PA, Pearce ME, Donner AP. Determinants of self-selected walking pace across ages 19 to 66. J Gerontol. 1982;37:560–564. doi: 10.1093/geronj/37.5.560. [DOI] [PubMed] [Google Scholar]
- 26.Leiper CI, Craik RL. Relationships between physical activity and temporal-distance characteristics of walking in elderly women. Phys Ther. 1991;71:791–803. doi: 10.1093/ptj/71.11.791. [DOI] [PubMed] [Google Scholar]
- 27.Peterson DS, Martin PE. Effects of age and walking speed on coactivation and cost of walking in healthy adults. Gait Posture. 2010;31:355–359. doi: 10.1016/j.gaitpost.2009.12.005. [DOI] [PubMed] [Google Scholar]