Abstract
The aim of this paper is to determine the role of enzymatic vitrectomy performed by intravitreal injection of autologous plasmin enzyme (APE) in the management of diabetic retinopathy and diabetic macular edema (DME). Diabetic patients with proliferative diabetic retinopathy or DME and evident posterior hyaloid adherence to the retinal surface were included. All cases were treated with an initial intravitreal injection of APE and reevaluated one month later, measuring changes in best-corrected visual acuity (BCVA), macular thickness and the status of the posterior hyaloid. A second APE injection was performed in cases with no evident posterior vitreous detachment (PVD) after the initial treatment. Sixty-three eyes were included in the present review. A complete PVD appeared in 38% of cases (24 eyes) after one injection of plasmin and the total increased to 51% (32 eyes) after the second injection, separated at least by one month. The central macular thickness improved in all cases (100%) and BCVA in 89%. Finally, in 50% of eyes with proliferative diabetic retinopathy, a high reduction of new vessels regression was observed. Enzymatic vitrectomy could be considered a good therapeutic alternative in diabetic retinopathy and macular edema.
Keywords: Enzymatic vitrectomy, Autologous plasmin, Diabetic macular edema, Diabetic retinopathy
Core tip: Diabetes mellitus might be considered as a pandemic disease with its incidence and prevalence increasing exponentially, even becoming epidemic. The aim of the present review was to analyze the clinical efficacy of the intravitreal injection of autologous plasmin enzyme in the treatment of diabetic retinopathy and diabetic macular edema and to determine the role of enzymatic vitrectomy as a therapeutic approach in such cases.
INTRODUCTION
Diabetes mellitus (DM) causes diabetic retinopathy (DR) and diabetic macular edema (DME) as a consequence of diabetic microangiopathy. Nowadays, DM might be considered as a pandemic disease with its incidence and prevalence increasing exponentially, even becoming epidemic. The prevalence of DR increases with the time of evolution of the systemic disease, with nearly 100% of patients showing some degree of diabetic retinopathy after 20 years of evolution. On the other hand, DME develops in 14%-25% of patients after 10 years of DM[1-3]. DR is a major cause of visual loss and a leading cause of blindness, whereas DME is the most common cause of visual loss in people under 50 years of age in developed countries[4,5].
Retinal neovascularization is a significant risk factor for severe visual loss in patients with DM, with optic disk new vessels as the maximum expression of such risk[6]. Laser photocoagulation has been the mainstay of treatment for DME and DR, but only 60% of patients with proliferative diabetic retinopathy (PDR) respond to panretinal photocoagulation, with regression of the neovascularization within 3 mo[2]. Laser photocoagulation mainly preserves vision rather than restoring it in cases of DME and PDR[7-9].
More recently, new therapeutic approaches have been developed for the management of both PDR and DME, including intravitreal injections of steroids (triamcinolone, sustained release intravitreal corticosteroid implant) or vascular endothelial factor inhibitors (VEGF), such as pegaptanib (Macugen; OSI pharmaceuticals, Melville, NY), bevacizumab (Avastin; Genentech, San Francisco, CA), ranibizumab (Lucentis; Genentech, San Francisco, CA) and aflibercept (Eylea, Regeneron Pharmaceutical, Inc, Tarrytown, NY), achieving vision improvement in a significant number of patients[10-12].
The incidence of DME and the progression rate of PDR are significantly lower in patients with spontaneous or surgical posterior vitreous detachment (PVD). It has been demonstrated that the adherence of the posterior hyaloid to the inner limiting membrane plays an important role in the development of DME and also in the growth of new vessels and its consequences, vitreous hemorrhage and tractional retinal detachment[13-17].
Enzymatic vitrectomy or pharmacological vitreolysis by intravitreal injection of autologous plasmin enzyme (APE) has been proposed as an effective neoadjuvant treatment for vitreous surgery by facilitating the surgical detachment of the posterior hyaloid and vitreoretinal membranes[18-20].
Plasmin, a serine protease, is active against laminin and fibronectin, located in the interface between the posterior vitreous cortex and the internal limiting membrane, and is responsible for the attachment of the vitreous to the retinal surface[21].
The aim of the present review was to analyze the clinical efficacy of the intravitreal injection of APE in the treatment of DR and DME and to determine the role of enzymatic vitrectomy as a therapeutic approach in such cases.
RESEARCH
The primary outcome was considered as the proportion of patients with a complete PVD following intravitreal injection of APE. The secondary outcomes were: number of patients with improvement in visual acuity and/or central macular thickness measured by optical coherence tomography (OCT); regression of new vessels in cases of PDR; and safety assessment of intravitreal injection of APE.
Before the injection of APE, all patients underwent a comprehensive ocular examination, including best corrected visual acuity (BCVA), slit-lamp examination, tonometry, indirect ophthalmoscopy, macular thickness measurement and assessment of posterior hyaloid status by OCT, color photographs and fluorescein angiography.
APE injection
A total volume of 0.2 mL of APE was obtained by a simplified method[21] and prepared 45 min prior to injection, sterilized through a 0.22 μm pore filter. Patients received unilateral intravitreal injections of APE through pars plana using a 30-gauge needle according to the routine procedure of intravitreal injections.
TREATMENT
A total of 63 eyes of 52 patients were included in the present study. Of them, 10 eyes showed PDR with optic disk new vessels and 53 eyes showed DME (33 refractory DME cases and 20 treatment-naïve patients).
Primary outcome: posterior vitreous detachment
A complete PVD appeared in 38% of cases (24 eyes) after one injection of plasmin and the total increased to 51% (32 eyes) after the second injection, separated at least by one month.
Secondary outcomes
Central macular thickness decreased in all cases with DME, even in cases without PVD following intravitreal injections of APE. BCVA improved in 89% of the treated eyes (56) (Figures 1, 2).
Figure 1.
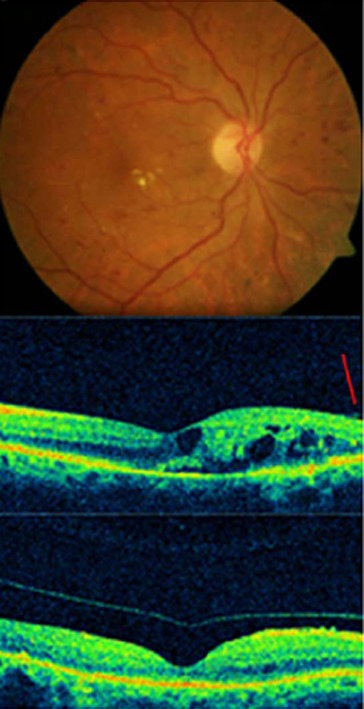
Complete posterior vitreous detachment and complete resolution of macular edema in a diabetic patient treated with autologous plasmin.
In cases with PDR, a highly significant regression in the new vessel area was observed in 5 cases (50%) (Figure 3); in 2 cases a partial regression was evidenced (20%), whereas the 3 remaining cases did not experience any change (30%).
Figure 3.
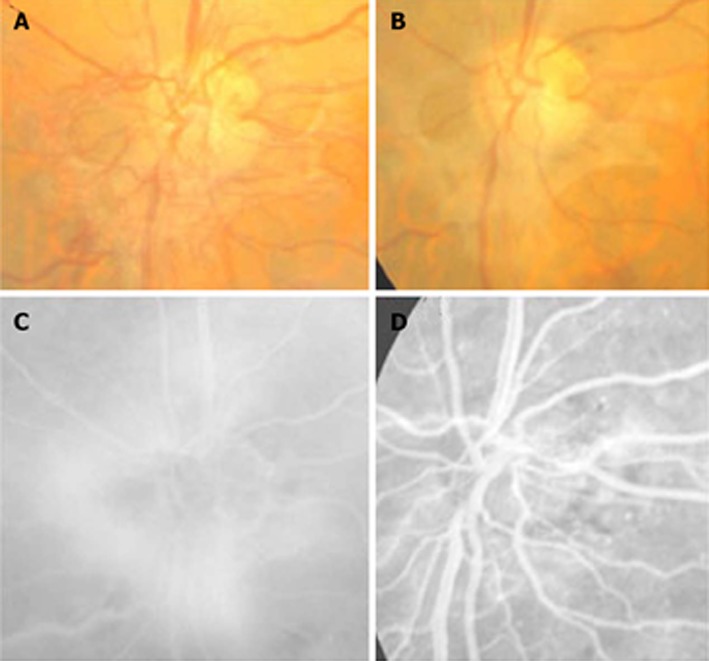
Regression of the new vessels of the optic disc in a treated eye with plasmin. A, B: Color images before and after treatment; C: Fluorescein angiogram shows the active vessels; D: The important but not complete resolution of leakage.
Safety profile
The treatment was well tolerated in all cases. No side effects were evidenced through the follow-up (uveitis, vitreous hemorrhage, cataract, ocular hypertension or retinal detachment).
DISCUSSION
The analyzed data suggested a possible role for enzymatic vitreolysis by intravitreal injection of APE for the management of PDR and DME. The efficacy of this procedure is related to the biochemical modification of the vitreous composition induced by the enzymatic separation or weakening of the union between the posterior vitreous cortex and the internal limiting membrane, leading to the development of PVD, and the liquefaction of the vitreous gel[22]. This procedure is dynamic with an important impact on the vitreous cavity. PVD not only has a protective role in a variety of retinal disorders, but also induces changes in the intraocular concentration of molecules, including VEGF, and increases intravitreal molecular diffusion coefficients and intravitreal oxygen levels[23-26]; this could also contribute to the good results obtained with this therapy.
APE employed in the present study was obtained by a simplified method and can be prepared in the operating room 45 min prior to the intravitreal injection. This constitutes a significant advantage compared to previously described techniques that required a longer and more expensive procedure. On the other hand, the method we propose has a wide variability and we cannot exactly recognize the concentration of APE that is injected and it depends on the plasminogen levels in each patient[27-30].
We achieved an overall efficacy of 50% in terms of inducing PVD in cases of DME and PDR, without any significant ocular side effects.
In conclusion, enzymatic vitrectomy performed by the intravitreal injection of APE might be effective and could be considered as an alternative for diabetic patients before performing other treatments, such as intravitreal injections of anti-VEGF or steroids, surgical vitrectomy or laser. Further studies are necessary to assess the efficacy and safety for the longer term and most convenient therapeutic strategy, including association of treatments, in diabetic patients to get better and more permanent results.
Footnotes
P- Reviewers: Le YZ, Ido Y, Romero-Aroca P S- Editor: Wen LL L- Editor: Roemmele A E- Editor: Lu YJ
References
- 1.DCCT Research Group. The effect of intensive treatment of diabetes in the development and progression of long-term complications in insulin-dependent diabetes. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 2.Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. XV. The long-term incidence of macular edema. Ophthalmology. 1995;102:7–16. doi: 10.1016/s0161-6420(95)31052-4. [DOI] [PubMed] [Google Scholar]
- 3. Available from: http://www.cdc.gov/diabetes/news/docs/dpp.htm.
- 4.Williams R, Airey M, Baxter H, Forrester J, Kennedy-Martin T, Girach A. Epidemiology of diabetic retinopathy and macular oedema: a systematic review. Eye (Lond) 2004;18:963–983. doi: 10.1038/sj.eye.6701476. [DOI] [PubMed] [Google Scholar]
- 5.Klein R, Klein BE, Moss SE. Visual impairment in diabetes. Ophthalmology. 1984;91:1–9. [PubMed] [Google Scholar]
- 6.Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:823–833. [PubMed] [Google Scholar]
- 7.Lee CM, Olk RJ. Modified grid laser photocoagulation for diffuse diabetic macular edema. Long-term visual results. Ophthalmology. 1991;98:1594–1602. doi: 10.1016/s0161-6420(91)32082-7. [DOI] [PubMed] [Google Scholar]
- 8.Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch Ophthalmol. 1985;103:1796–1806. [PubMed] [Google Scholar]
- 9.Vander JF, Duker JS, Benson WE, Brown GC, McNamara JA, Rosenstein RB. Long-term stability and visual outcome after favorable initial response of proliferative diabetic retinopathy to panretinal photocoagulation. Ophthalmology. 1991;98:1575–1579. doi: 10.1016/s0161-6420(91)32085-2. [DOI] [PubMed] [Google Scholar]
- 10.Ford JA, Elders A, Shyangdan D, Royle P, Waugh N. The relative clinical effectiveness of ranibizumab and bevacizumab in diabetic macular oedema: an indirect comparison in a systematic review. BMJ. 2012;345:e5182. doi: 10.1136/bmj.e5182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Massin P, Audren F, Haouchine B, Erginay A, Bergmann JF, Benosman R, Caulin C, Gaudric A. Intravitreal triamcinolone acetonide for diabetic diffuse macular edema: preliminary results of a prospective controlled trial. Ophthalmology. 2004;111:218–224; discussion 224-225. doi: 10.1016/j.ophtha.2003.05.037. [DOI] [PubMed] [Google Scholar]
- 12.Haller JA, Kuppermann BD, Blumenkranz MS, Williams GA, Weinberg DV, Chou C, Whitcup SM. Randomized controlled trial of an intravitreous dexamethasone drug delivery system in patients with diabetic macular edema. Arch Ophthalmol. 2010;128:289–296. doi: 10.1001/archophthalmol.2010.21. [DOI] [PubMed] [Google Scholar]
- 13.Akiba J, Arzabe CW, Trempe CL. Posterior vitreous detachment and neovascularization in diabetic retinopathy. Ophthalmology. 1990;97:889–891. doi: 10.1016/s0161-6420(90)32486-7. [DOI] [PubMed] [Google Scholar]
- 14.Ono R, Kakehashi A, Yamagami H, Sugi N, Kinoshita N, Saito T, Tamemoto H, Kuroki M, Lshikawa SE, Kawakami M. Prospective assessment of proliferative diabetic retinopathy with observations of posterior vitreous detachment. Int Ophthalmol. 2005;26:15–19. doi: 10.1007/s10792-005-5389-2. [DOI] [PubMed] [Google Scholar]
- 15.Tagawa H, McMeel JW, Trempe CL. Role of the vitreous in diabetic retinopathy. II. Active and inactive vitreous changes. Ophthalmology. 1986;93:1188–1192. doi: 10.1016/s0161-6420(86)33608-x. [DOI] [PubMed] [Google Scholar]
- 16.Schepens CL, Avila MP, Jalkh AE, Trempe CL. Role of the vitreous in cystoid macular edema. Surv Ophthalmol. 1984;28 Suppl:499–504. doi: 10.1016/0039-6257(84)90232-7. [DOI] [PubMed] [Google Scholar]
- 17.Ikeda T, Sato K, Katano T, Hayashi Y. Attached posterior hyaloid membrane and the pathogenesis of honeycombed cystoid macular edema in patients with diabetes. Am J Ophthalmol. 1999;127:478–479. doi: 10.1016/s0002-9394(98)00382-1. [DOI] [PubMed] [Google Scholar]
- 18.Gandorfer A, Putz E, Welge-Lüssen U, Grüterich M, Ulbig M, Kampik A. Ultrastructure of the vitreoretinal interface following plasmin assisted vitrectomy. Br J Ophthalmol. 2001;85:6–10. doi: 10.1136/bjo.85.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asami T, Terasaki H, Kachi S, Nakamura M, Yamamura K, Nabeshima T, Miyake Y. Ultrastructure of internal limiting membrane removed during plasmin-assisted vitrectomy from eyes with diabetic macular edema. Ophthalmology. 2004;111:231–237. doi: 10.1016/j.ophtha.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Azzolini C, D’Angelo A, Maestranzi G, Codenotti M, Della Valle P, Prati M, Brancato R. Intrasurgical plasmin enzyme in diabetic macular edema. Am J Ophthalmol. 2004;138:560–566. doi: 10.1016/j.ajo.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 21.Li X, Shi X, Fan J. Posterior vitreous detachment with plasmin in the isolated human eye. Graefes Arch Clin Exp Ophthalmol. 2002;240:56–62. doi: 10.1007/s004170100351. [DOI] [PubMed] [Google Scholar]
- 22.Sebag J. Molecular biology of pharmacologic vitreolysis. Trans Am Ophthalmol Soc. 2005;103:473–494. [PMC free article] [PubMed] [Google Scholar]
- 23.Goldenberg DT, Trese MT. Pharmacologic vitreodynamics and molecular flux. Dev Ophthalmol. 2009;44:31–36. doi: 10.1159/000223943. [DOI] [PubMed] [Google Scholar]
- 24.Barnett JM, McCollum GW, Fowler JA, Duan JJ, Kay JD, Liu RQ, Bingaman DP, Penn JS. Pharmacologic and genetic manipulation of MMP-2 and -9 affects retinal neovascularization in rodent models of OIR. Invest Ophthalmol Vis Sci. 2007;48:907–915. doi: 10.1167/iovs.06-0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sebag J, Ansari RR, Suh KI. Pharmacologic vitreolysis with microplasmin increases vitreous diffusion coefficients. Graefes Arch Clin Exp Ophthalmol. 2007;245:576–580. doi: 10.1007/s00417-006-0394-3. [DOI] [PubMed] [Google Scholar]
- 26.Quiram PA, Leverenz VR, Baker RM, Dang L, Giblin FJ, Trese MT. Microplasmin-induced posterior vitreous detachment affects vitreous oxygen levels. Retina. 2007;27:1090–1096. doi: 10.1097/IAE.0b013e3180654229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Udaondo P, Díaz-Llopis M, García-Delpech S, Cervera E, Salom D. [Autologous plasmin for intravitreal injection without associated vitrectomy: a simple preparation method with streptokinase] Arch Soc Esp Oftalmol. 2008;83:153–154. doi: 10.4321/s0365-66912008000300004. [DOI] [PubMed] [Google Scholar]
- 28.Díaz-Llopis M, Udaondo P, Salom D, García-Delpech S, Romero FJ. [Intravitreal autologous plasmin without associated-vitrectomy. Pharmacological vitreolysis, a perfeccionated method using urokinase] Arch Soc Esp Oftalmol. 2008;83:291–292. doi: 10.4321/s0365-66912008000500003. [DOI] [PubMed] [Google Scholar]
- 29.Wang F, Wang Z, Sun X, Wang F, Xu X, Zhang X. Safety and efficacy of dispase and plasmin in pharmacologic vitreolysis. Invest Ophthalmol Vis Sci. 2004;45:3286–3290. doi: 10.1167/iovs.04-0026. [DOI] [PubMed] [Google Scholar]
- 30.Ulrich JN, Spannagl M, Kampik A, Gandorfer A. Components of the fibrinolytic system in the vitreous body in patients with vitreoretinal disorders. Clin Experiment Ophthalmol. 2008;36:431–436. [PubMed] [Google Scholar]


