Abstract
Diagnosis of extremity soft-tissue tumors can be challenging. Characteristics of tumor margins can help precisely identify locally aggressive or non-aggressive behavior for surgical planning, but cannot differentiate benign from malignant lesions. Most malignant tumors can have inhomogeneous signals on T2-weighted images. Although a uniform signal on T2-weighted images can be a reliable indication of a benign lesion, a well-defined mass with homogeneous internal signal intensity does not definitively identify a benign lesion. Some common and distinctive soft-tissue lesions can have specific clinical and imaging features allowing a diagnosis without biopsy. These are known as determinate lesions. This illustrative report presents a diagnostic guide for extremity soft-tissue tumors based on tissue signal and morphological characteristics on magnetic resonance images. It is important for clinicians to be familiar with the imaging characteristics of common determinate lesions.
Keywords: Extremity, Magnetic resonance imaging, Musculoskeletal neoplasm, Sarcoma, Soft-tissue tumors
Core tip: The aim of this illustrative report is to provide a diagnostic guide for soft-tissue tumors of the extremities based on tissue signal and morphological characteristics on magnetic resonance images.
MAGNETIC RESONANCE IMAGING OF SOFT-TISSUE TUMORS OF THE EXTREMITIES: A PRACTICAL APPROACH
The functions of magnetic resonance (MR) imaging in evaluation of soft-tissue tumors of the extremities include detection, characterization, local staging, and detection of recurrence and complications after therapy.
MR imaging and computed tomography (CT) scanning can be equally accurate for detecting the size and extent of a tumor. MR imaging is more accurate than CT for evaluating individual muscle involvement and therefore can be the staging procedure of choice in patients with soft-tissue sarcoma of the extremities.
MR imaging is superior to CT in detecting recurrent soft-tissue sarcomas. A nodule or mass with a mass effect on surrounding tissue is highly indicative of recurrent tumors. However, both the tumor and organizing scar (or granulation tissue) can show marked gadolinium enhancement.
MRI determinate lesions
Some common and distinctive soft-tissue lesions have specific clinical and imaging features allowing a diagnosis without biopsy[1,2]. These are known as determinate lesions[2]. Examples of lesions with specific signal characteristics on MR imaging are lipoma (Figure 1), liposarcoma (Figure 2), hemangioma (Figure 3), ganglion and Baker cysts (Figure 4), giant cell tumor (GCT) arising from the tendon sheath (Figure 5), peripheral nerve sheath tumor (PNST) and neurofibroma (Figure 6, Figure 7 and Figure 8), subungual glomus tumor (Figure 9), localized solitary synovitis (Figure 10), muscle tear and hematoma (Figure 11), abscess (Figure 12), myonecrosis, bursitis, and aneurysm. s
Figure 1.
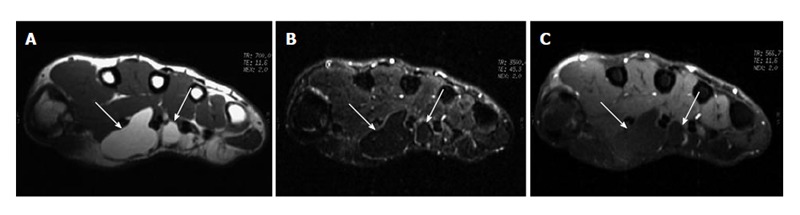
Lipoma of the tendon sheath. A: T1-weighted MR image of the right wrist shows a lobulated high-signal-intensity mass (arrows) located between the palmar muscles; B: Fat-saturated proton-density weighted MR image shows homogeneous low signal intensity of the tumor mass (arrows), suggestive of a fat component; C: There is no enhancement of the tumor mass (arrows) after gadolinium administration on fat-saturated T1-weighted image. MR: Magnetic resonance.
Figure 2.
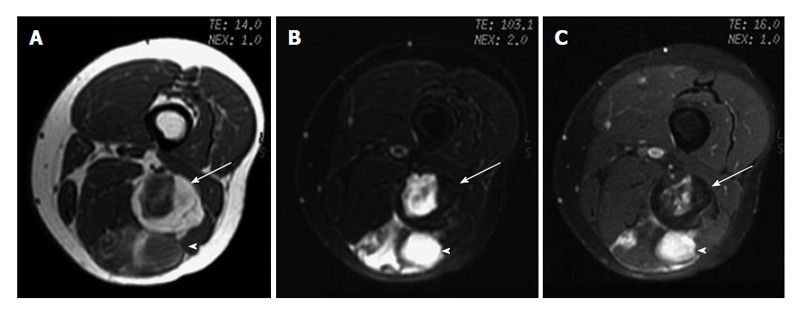
Myxoid liposarcoma. A: Axial T1-weighted image; B: Fat-saturated T2-weighted MR image; C: Fat saturated gadolinium-enhanced T1-weighted images of left thigh show a lobulated fat-containing mass (arrow) with an enhancing nonadipose mass-like area (arrowhead) on the left thigh, suggestive of myxoid stroma.
Figure 3.
Cavernous hemangioma. A: Coronal T1-weighted image; B: Fat saturated T2-weighted MR image. The left calf shows a heterogeneous serpiginous high-signal-intensity lesion (arrows) on T2-weighted image, which is caused by dilated slow-flowing vessels with methemoglobin. Some low-signal-intensity pattern (arrowhead) indicates fast-flow blood or hemosiderin or calcification. MR: Magnetic resonance.
Figure 4.

Baker cysts. A: Sagittal proton-density B: Axial gradient-echo images. The left knee shows a well-defined cystic lesion (arrowhead) connected to the knee joint by way of a narrow neck between the semimembranosus tendon (arrow) and the medial head of the gastrocnemius muscle (gm). Note that the Baker cyst contains debris (small arrows in A).
Figure 5.
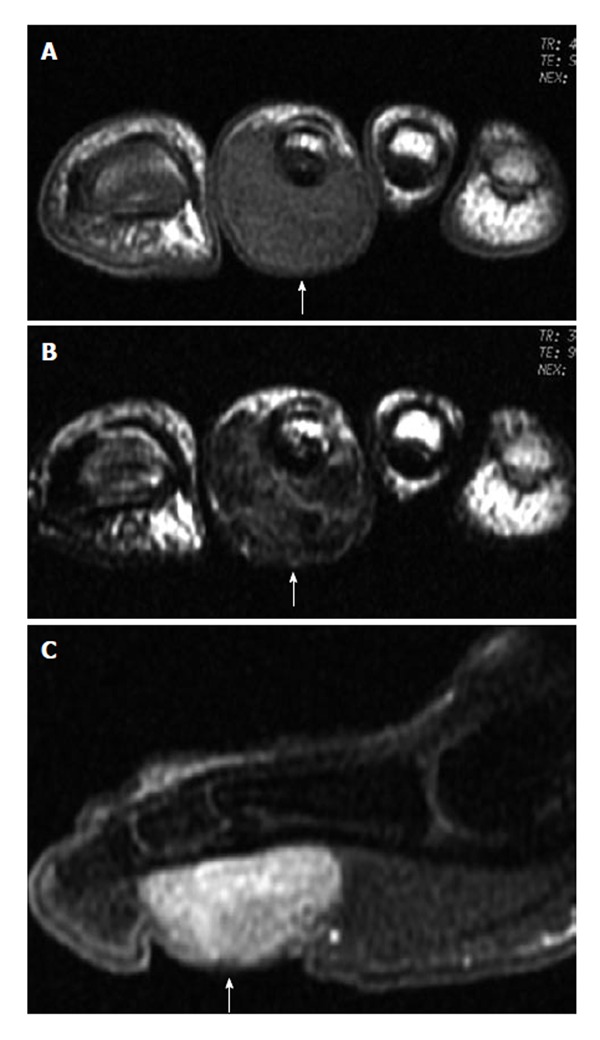
Giant cell tumor of the tendon sheath. A: T1-weighted image shows the tumor (arrow) on the plantar side; B: T2-weighted image shows heterogeneous low signal intensity of the tumor (arrow) due to hemosiderin deposition; C: Sagittal gadolinium-enhanced T1-weighted image with fat saturation shows obvious enhancement of the tumor mass (arrow).
Figure 6.
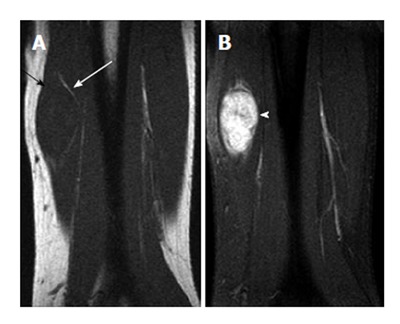
Neurofibroma of the left ulnar nerve (split-fat sign) in a 58-year-old man. A: Coronal T1-weighted image of the left forearm shows a spindle-shaped mass with isointensity relative to adjacent muscle. Note the presence of the split-fat sign (arrows). Because the neurovascular bundle is normally surrounded by fat, masses arising at this site maintain a rim of fat about them as they slowly enlarge; B: Coronal T1-weighted fat-saturated gadolinium-enhanced image shows heterogeneous enhancement of the mass (arrowhead). Recognition of the spindle shape of the tumor and contiguity of the tumor and adjacent nerve may suggest the diagnosis[6].
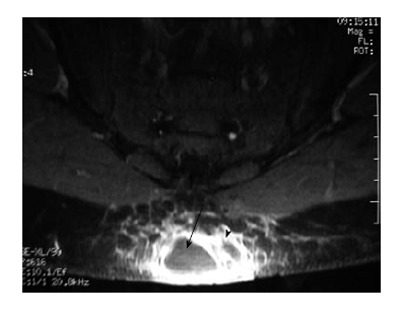
Figure 7.

Neurofibroma of the right radial nerve (target sign) in a 35-year-old man. High signal intensity of myxoid Antoni type B (arrow)[6].
Figure 8.

Neurofibroma of the left sciatic nerve (fascicular sign) in a 55-year-old woman. A hyperintense mass (arrow) with multiple small hypointense fascicle-like structures in the mass, representing the “fascicular sign”[6].
Figure 9.
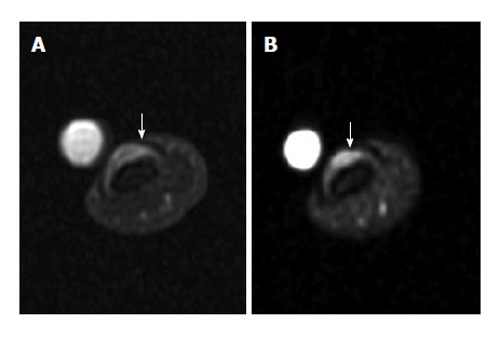
Subungual glomus tumor. A: Axial proton-density-weighted MR image of the left thumb shows a small subungual tumor (arrow); B: Fat-saturated gadolinium-enhanced T1-weighted image shows obvious enhancement of the tumor (arrow). MR: Magnetic resonance.
Figure 10.
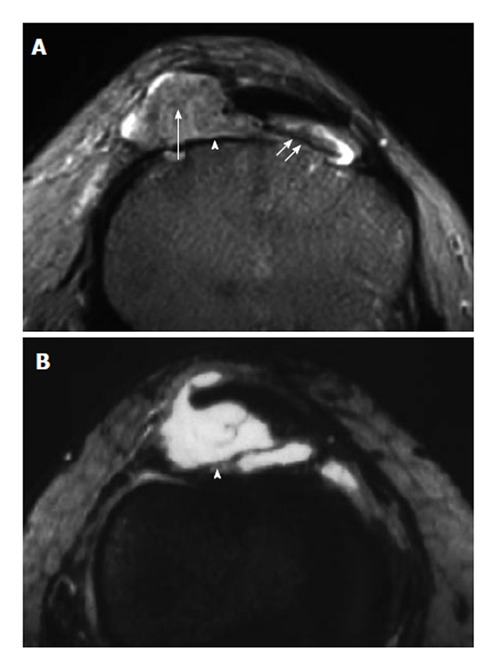
Localized nodular synovitis (solitary PVNS). A: Axial T2-weighted MR image of the knee shows a nodular mass (arrowhead), with a long pedicle (double short arrows) attaching the mass to the adjacent synovium, involving the infrapatellar fat pad. Note small circular foci of low signal intensity (arrow), corresponding to deposition of hemosiderin. B: Gadolinium-enhanced T1-weighted image with fat saturation shows obvious enhancement of the lesion (arrow) caused by capillary proliferation. (Photo courtesy of Dr. Guo-Shu Huang). MR: Magnetic resonance.
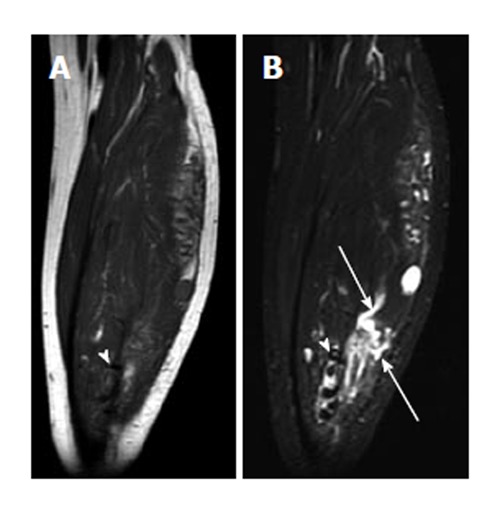
Figure 11.
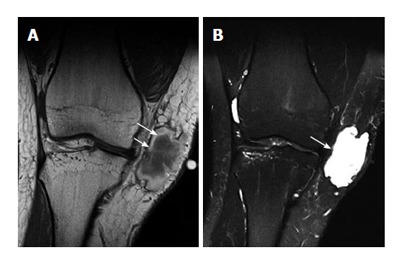
Early subacute hematoma. A: Coronal T1-weighted; B: T2-weighted MR image of the knee. On T1-weighted image, there is a hyperintensity of extracellular methemoglobin at the periphery (long arrow) of the hematoma (which is seen 2-7 d after injury). Note a very thin low-signal-intensity rim at the outermost layer of the hematoma, indicating hemosiderin (short arrow). B: Coronal T2-weighted MR image shows overall hyperintensity of the hematoma (arrow), exception made for a very thin low-signal-intensity peripheral rim caused by hemosiderin.
Figure 12.
Abscess. Axial gadolinium-enhanced T1-weighted image with fat saturation shows a mass lesion within the subcutaneous fat of the buttock, with a pronounced rim of enhancement (arrowhead), corresponding to large amounts of granulation tissue. The unenhanced central area is a fluid-debris cavity (arrow).
MRI indeterminate lesions
An indeterminate lesion is one that must be biopsied to ensure an accurate diagnosis[2]. Examples of lesions are malignant fibrous histiocytoma (Figure 13), fibroma, fibrosarcoma, leiomyoma, leiomyosarcoma, angiosarcoma (hemangiosarcoma), rhabdomyoma, rhabdomyosarcoma, synovial sarcoma, synovioma, lymphangiosarcoma, malignant hemangiopericytoma, alveolar soft parts sarcoma, epithelioid sarcoma, and angiosarcoma. Diagnosis of a lesion suspicious for a malignant tumor should never be relied on imaging alone. All suspicious tumors should be biopsied (Figures 14 and 15).
Figure 13.
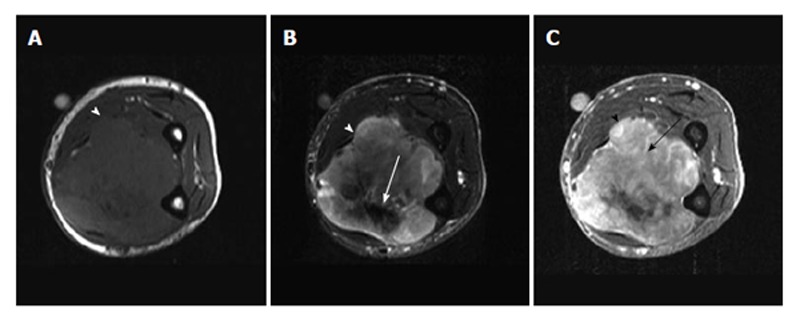
Malignant fibrous histiocytoma. A: Axial T1-weighted MR image of the forearm shows a soft-tissue tumor (arrowhead) with a relatively well-defined margin. No invasion to the adjacent radius or ulna was noted; B: Axial T2-weighted MR image shows heterogeneous signal intensity of the tumor mass (arrowhead), with an area of low signal intensity (arrow), suggesting fibrosis; C: Axial gadolinium-enhanced T1-weighted image with fat saturation shows enhancement of the parenchymal tissue (arrow) of the tumor mass (arrowhead), corresponding to the hypervascular part of the tumor. MR: Magnetic resonance.
Figure 14.
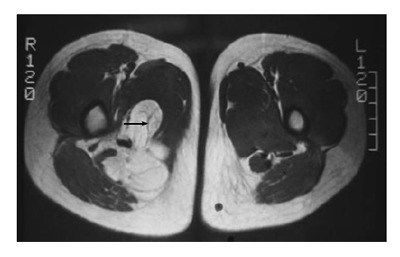
Low-grade liposarcoma. Axial T1-weighted MR image of bilateral thighs shows a lobulated high-signal-intensity mass with uneven or focal thickening septa (arrow) within the tumor on the right thigh, which can be a finding for low-grade liposarcoma. MR: Magnetic resonance.
Figure 15.
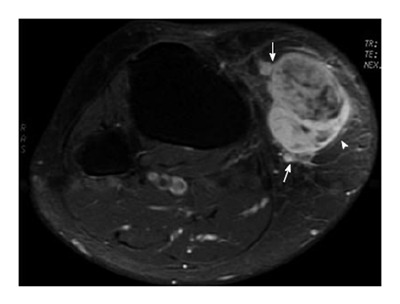
Malignant peripheral nerve sheath tumor involving the subcutis of the right knee in a 65-year-old woman. Tumor mass (arrowhead) is located in the subcutaneous area of the right knee. The mass has an ill-defined margin (arrows) with a fascicular appearance centrally.
Characteristics of tumor margins
A well-demarcated lesion or a tumor mass with a capsule can favor a benign diagnosis, whereas a less well-demarcated lesion or tumor mass with an infiltrative margin is most likely malignant. Margin characteristics can help precisely identify locally aggressive or non-aggressive behavior for surgical planning, but cannot differentiate benign from malignant lesions[3]. Clinical data always play an important role in evaluating the aggressiveness of tumors.
Characteristics of MRI signals
Fat, fibrous tissue, fluid or cyst, and protein can be characterized by specific signals on MR imaging. Most benign lesions have a uniform signal on T1-weighted and T2-weighted images, with the exception, for example, of neurofibromas and hemangiomas, which exhibit inhomogeneous signals on T2-weighted images. Most malignant tumors can have a uniform signal on T1-weighted images but inhomogeneous signals on T2-weighted images. Although a uniform signal on T2-weighted images can be a reliable indication of a benign lesion, a well-defined mass with homogeneous internal signal intensity does not definitively identify a benign lesion. Lack of uniformity does not reliably indicate malignancy[3]. Low-grade liposarcomas (Figure 14) and leiomyosarcoma, for example, are malignant lesions with misleading benign appearances. Soft-tissue lesions arising from trauma (e.g., hematoma) can mimic malignancy.
On dynamic gadolinium-enhanced MR imaging, measurement of relaxation times cannot guide evaluation, as the T1- and T2-relaxation times of benign and malignant lesions overlap significantly[4]. Whether the time-intensity-curve (TIC) shape analysis alone can differentiate malignant from benign soft-tissue tumors, or differentiate between tumor grades, remains controversial[5].
The aim of this illustrative report is to provide a diagnostic guide for soft-tissue tumors of the extremities based on tissue signal and morphological characteristics on MR images. Examples of common determinate lesions are illustrated, except that one indeterminate lesion (malignant fibrous histiocytoma) is shown as an example for comparison.
In summary, MR imaging can be helpful in evaluating soft-tissue tumors of the extremities, but it can also be misleading. The combination of signal and morphological characteristics on MR images allows radiologists to categorize many lesions as benign or malignant, although a significant proportion of the images are not specific. It is important for clinicians to be familiar with the imaging characteristics of common determinate lesions. Biopsy is needed to define the histological nature of an indeterminate soft-tissue neoplasm.
Footnotes
P- Reviewers: Nouh MR, Plataniotis G S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Liu XM
References
- 1.Wu JS, Hochman MG. Soft-tissue tumors and tumorlike lesions: a systematic imaging approach. Radiology. 2009;253:297–316. doi: 10.1148/radiol.2532081199. [DOI] [PubMed] [Google Scholar]
- 2.Papp DF, Khanna AJ, McCarthy EF, Carrino JA, Farber AJ, Frassica FJ. Magnetic resonance imaging of soft-tissue tumors: determinate and indeterminate lesions. J Bone Joint Surg Am. 2007;89 Suppl 3:103–115. doi: 10.2106/JBJS.G.00711. [DOI] [PubMed] [Google Scholar]
- 3.Lang P, Genant HK, Johnston JO, Honda G. Musculoskeletal neoplasm. In: Chan WP, Lang P, Genant HK, editors. MRI of the Musculoskeletal System. Philadelphia: W.B. Saunders; 1994. pp. 401–443. [Google Scholar]
- 4.Mirowitz SA, Totty WG, Lee JK. Characterization of musculoskeletal masses using dynamic Gd-DTPA enhanced spin-echo MRI. J Comput Assist Tomogr. 1992;16:120–125. [PubMed] [Google Scholar]
- 5.Lavini C, Buiter MS, Maas M. Use of dynamic contrast enhanced time intensity curve shape analysis in MRI: theory and practice. Reports Med Imaging. 2013;6:71–82. [Google Scholar]
- 6.Li CS, Huang GS, Wu HD, Chen WT, Shih LS, Lii JM, Duh SJ, Chen RC, Tu HY, Chan WP. Differentiation of soft tissue benign and malignant peripheral nerve sheath tumors with magnetic resonance imaging. Clin Imaging. 2008;32:121–127. doi: 10.1016/j.clinimag.2007.05.006. [DOI] [PubMed] [Google Scholar]


