Abstract
Purpose
Multiple hereditary exostoses of the forearm typically form in the distal ulna, causing disturbances in the growth of the ulna and functional disability. Multiple hereditary exostoses inhibit the growth of the ulna, leading to an acquisition of a varus deformity in the radius, which sometimes leads to dislocation of the radial head, the development of limitations in the pronation-supination of the forearm, and cosmetic problems.
Materials and Methods
We retrospectively reviewed the cases of four patients who had deformities of the forearm with radial head dislocation associated with multiple hereditary exostoses, and evaluated the radiologic and clinical results of excision of the osteochondromas from the distal ulna and gradual ulnar lengthening with an Ilizarov external fixator.
Results
Good clinical and radiological results were obtained after a mean follow-up of 25 months. At the most recent follow-up, radial bowing, ulnar shortening, carpal slip, and the pronation/supination arch of the forearm had improved. There was little change in terms of preoperative radial articular angle and the flexion/extension arch of the elbow by the most recent follow-up.
Conclusion
Treatment of four forearms from four patients by excision of osteochondromas and gradual lengthening of the ulna with an Ilizarov external fixator spontaneously reduced dislocations of the radial heads without the need for any additional operative intervention. All patients were satisfied with the final results.
Keywords: Multiple hereditary exostosis, Ilizarov external fixator, gradual lengthening
INTRODUCTION
The first description of a patient with multiple exostosis has been attributed to Hunter in 1786. In 1814, Boyer published the first description of a family with multiple hereditary exostosis (MHE).1,2 Although exostoses are histological benign lesions, they can cause a variety of clinical problems. Patients with MHE most frequently report pain, cosmetic concerns and limitations to the adjacent joint. Deformities of the forearm and wrist occur in 39-59% of patients with multiple hereditary exostoses.3,4 Some commonly seen deformities in this condition are bowing of the radius, shortening of the ulna, ulna drift of the carpus, and occasionally dislocation or subluxation of the radial head. These complex deformities cause a loss of forearm pronation-supination.
Recent literature offers divergent views regarding treatment of these deformities. Some recommend aggressive early operative intervention to prevent or reduce the progression of deformities and/or functional impairment, particularly with regard to radial head dislocation. Others stated that these surgical procedures do not produce any predictable functional improvement. Excision of the exostoses may be performed for cosmetic reasons or to resolve local irritation alone.
Acute or gradual lengthening of the ulna, hemiphyseal stapling of the distal aspect of the radius, corrective osteotomy of the radius or excision or open reduction of a displaced radial head may be included in corrective or reconstructive surgery of the forearm.5 However, there are no reports about the results of surgical treatment in patients with multiple hereditary exostoses who had a preoperatively dislocated radial head treated by excision of the osteochondroma and gradual lengthening. Our hypothesis was that patients who had a dislocated radial head would suffer limitations to the range of motion of the forearm, which would be improved by gradual lengthening of ulnar using the Ilizarov technique.
MATERIALS AND METHODS
Patients
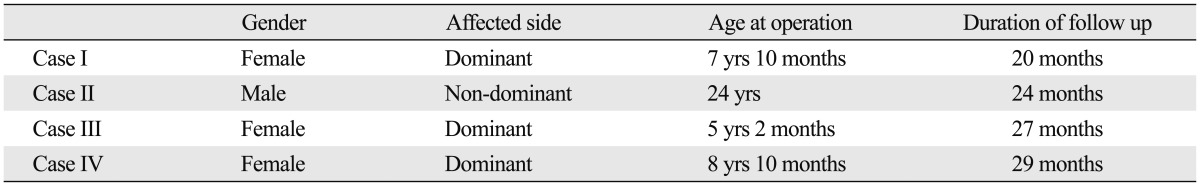
We retrospectively reviewed the cases of four patients who had deformities on one forearm each and radial head dislocation associated with multiple hereditary exostosis. The patients were treated at our hospital between 2006 and 2009. There were three girls and one boy, ranging in age from 5.2 to 24.0 years (average, 11.5 years). The follow-up period ranged from 20 to 29 months (mean: 25 months). The deformations were present in three dominant side forearms and one non-dominant side forearm, and restriction of pronation/supination of the forearm before surgery was found in all cases (Table 1).
Table 1.
Demographic Data of the Four Patients Treated for Forearm Deformity
Operative technique
The operative technique was as follows. First, we removed the osteochondromas of the distal ulna. Second, we took ulnar transverse mid-diaphyseal subperiosteal osteotomy and positioned an Ilizarov external fixator. We used a temporary radial head reduction pin in all cases. The patients had a seven-day resting period and 1 mm/day of gradual lengthening with careful monitoring of neurovascular status, adjusted joint pain and swelling, and pin tract infection. We lengthened the ulna by 5 mm plus variance, with the expectation of subsequent recurrence of ulnar shortening, except in one case that had already reached skeletal maturity, 24-year-old male. We removed the temporary radial head reduction pin when we were able to determine the radial head reduction, using serial follow-up X-rays (Fig. 1).
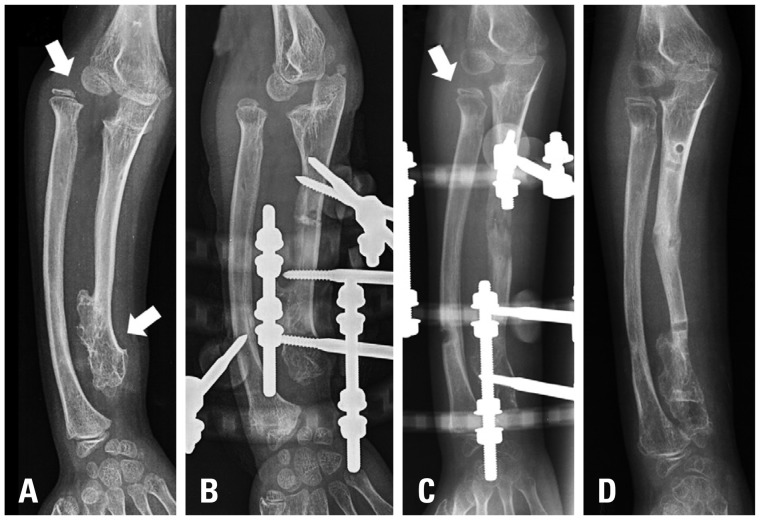
Fig. 1.
This patient was 7 years and 10 months old. (A) The preoperative X-ray shows dislocated radial head (arrow) and distal ulnar osteochondroma (arrow). (B) Immediate postoperative X-ray shows a temporary reduction pin for the dislocated radial head. (C) 33 mm lengthening was done and we removed the temporary reduction pin six weeks after the operation. The arrow indicates the reduced radial head. (D) At the most recent follow-up X-ray, we found a reduced radial head.
Radiological and clinical evaluation
Radiological assessment consisted of upper extremity antero-posterior radiograph with the hand and elbow in an anatomic position. A lateral radiograph of the forearm that included the hand, wrist, and elbow was obtained. We classified the forearm deformity using the Masada and Ono Classification system according to their morphological characteristics (Fig.2).5 Radiographic review compared the preoperative and most recent follow-up radiographs. We measured the radial articular angle (RAA), radial length (RL), radial bowing (RB), percentage of RB, carpal slip (CS), ulnar length (UL), ulnar shortening, percentage of ulnar shortening at forearm anterior-posterior plane radiography, and radial head stability at elbow lateral plane radiography (Fig. 3). We measured the amount of ulnar lengthening (AUL) at the most recent follow-up forearm anterior-posterior plane radiography and calculated the external fixation index (EFI). EFI was obtained by dividing the total duration of external fixation by the length gained.
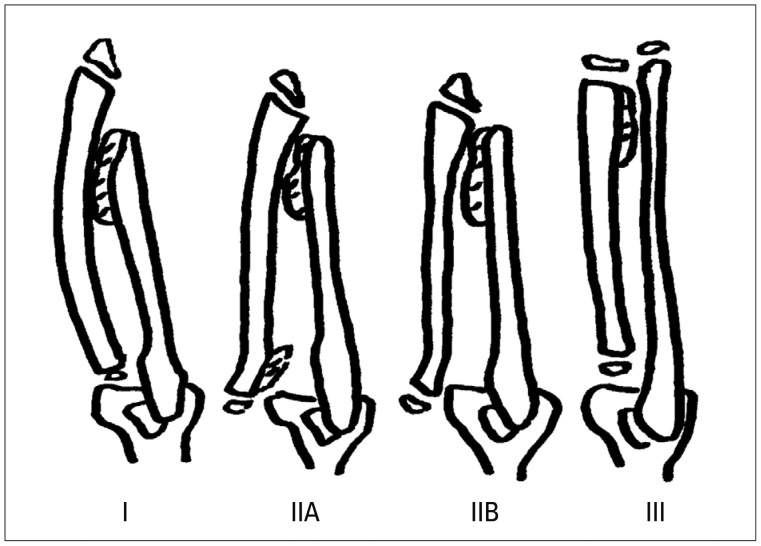
Fig. 2.
Classification of MHE forearm deformities. Type 1: the main osteochondroma formation is in the distal portion of the ulna, but the radial head is not dislocated. Type IIA: the radial head is dislocated because of an osteochondroma at the proximal metaphysic of the radius. Type IIB: in addition to ulnar shortening the radial head is dislocated. Type III: the main osteochondroma formation is in the metaphysic of the distal radius, and there is relative shortening of the radius. MHE, multiple hereditary exostosis.
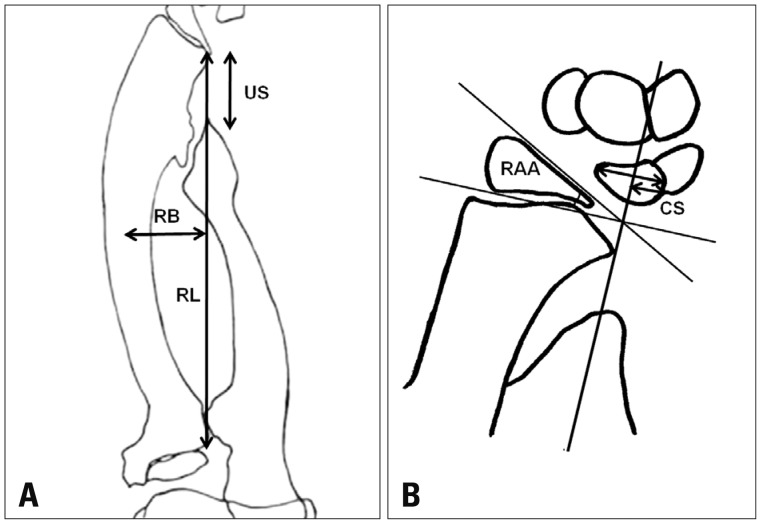
Fig. 3.
Radiologic assessment. (A) Ulnar shortening: measured by a line drawn from the distal end of the ulna to the linear axis. Radial bowing: the distance that the radial diaphysis deviates from the linear axis of the forearm divided by the length of the linear axis. (B) The ulna tilt of the distal radial articular surface was recorded as the radial articular angle. The ulna drift of the carpus was assessed by the carpal slip. RL, radial length; RB, radial bowing; CS, carpal slip; RAA, radial articular angle; US, ulna shortening.
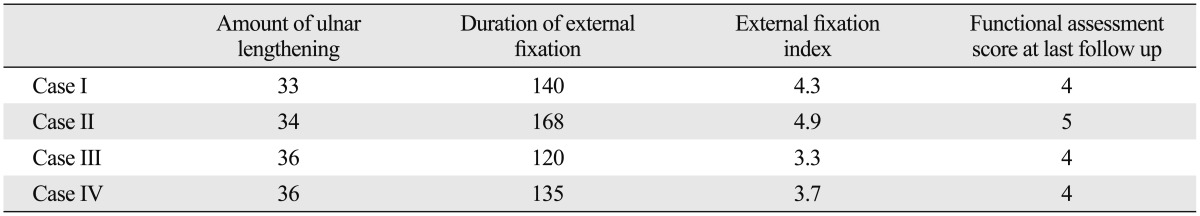
We evaluated the range of pronation/supination, elbow flexion/extension at the preoperative and most recent visit to the outpatient department. Also, each patients was asked to rate the function of the extremity according to specific criteria (Table 2).6
Table 2.
Functional Assessment Criteria by the Patient
Statistical evaluation
Data were analyzed using SPSS statistical analysis software program version 15.0 (SPSS Inc., Chicago, IL, USA). Testing for statistical significance was performed using the Wilcoxon signed rank test. Statistical significance was considered at p≤0.05.
RESULTS
The presenting symptoms were a loss of range of motion of the forearm and cosmetic problems in all four patients. All cases were Class IIB type classified by the Masada and Ono Classification, which means that the radial head is dislocated because of an osteochondroma in the distal portion of the ulna and there are small osteochondromas in the part of the radius. Dislocation of the radial head, which was observed preoperatively in all patients, was naturally reduced with a temporary reduction half pin that was located within 6 weeks. In Case 1, we could see radial head subluxation at 20 months follow up, but there was no further progression of the limitation of elbow range of motion. In other cases, stably reduced radial head was observed upon recent follow-up radiographic evaluation.
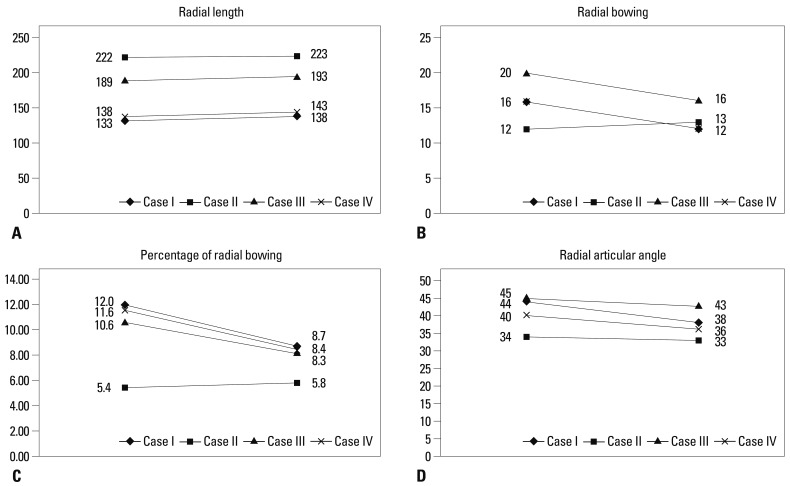
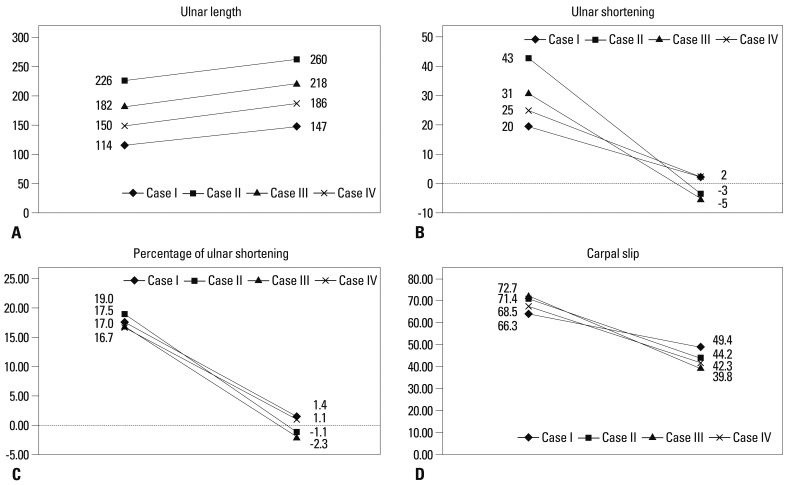
The average preoperative RL, RB, percentage of RB and RAA were 170.5 (133.0-222.0) mm, 16.0 (12.0-20.0) mm, 9.9 (5.4-12.0) % and 40.7 (34.0-45.0) degrees. At the time of most recent follow up, they were 174.2 (138.0-223.0) mm, 13.2 (12.0-16.0) mm, 7.8 (5.8-8.7) % and 37.5 (33.0-43.0) degree. When all of the patients were compared, there was a tendency towards improvement that was not significant in any of these four parameters (Fig. 4).
Fig. 4.
Preoperative and postoperative radial length, radial bowing, percentage of radial bowing, radial articular angle. (A) Average preoperative radial length was 170.5 mm, and 174.2 mm at the last follow up. (B) Average preoperative radial bowing was 16.0 mm, and 13.2 mm at the last follow up. (C) Average preoperative percentage of radial bowing was 9.9%, and 7.8% at the last follow up. (D) The average preoperative radial articular angle was 40.7 degree, and 37.5 degree at the last follow up. Testing for statistical significance was performed using the Wilcoxon signed rank test, but we found no statistical significance.
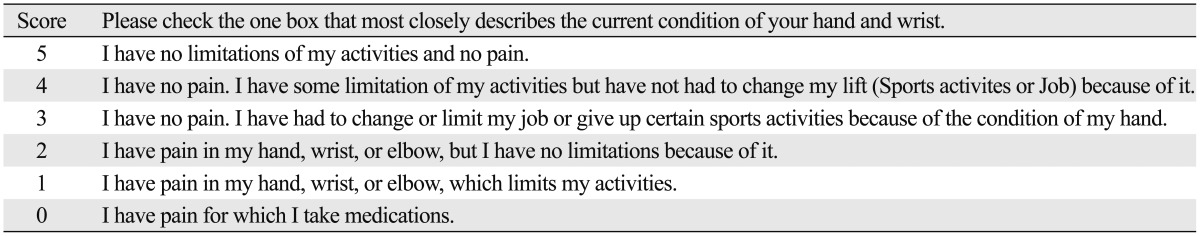
The average preoperative UL, ulnar shortening and percentage of ulnar shortening were 168.0 (114.0-226.0) mm, 29.7 (20.0-43.0) mm and 17.5 (16.7-19.0) %, respectively. At the time of most recent follow, they were 202.7 (147.0-260.0) mm, -1.0 (-5.0-2.0) mm and -0.3 (-2.3-1.4) %, respectively. CS was improved, preoperatively 69.5 (65.3-72.7)% and most recent follow up 43.9 (39.8-49.4) % (Fig. 5).
Fig. 5.
Preoperative and postoperative ulnar length, ulnar shortening, percentage of ulnar shortening, carpal slip. (A) Average preoperative ulnar length was 168.0 mm, and 202.7 mm at the last follow up. (B) Average preoperative ulnar shortening was 29.7 mm, and -1.0 mm at the last follow up. (C) Average preoperative percentage of ulnar shortening was 17.5%, and -0.3% at the last follow up. (D) The average preoperative carpal slip was improved, preoperatively 69.5%, and most recent follow up 43.9%. Testing for statistical significance was performed using the Wilcoxon signed rank test, but we found no statistical significance.
The average AUL and duration of external fixation index were 34.5 (33.0-36.0) mm and 140.7 (120.0-168.0) days, respectively. Thus, the external fixation index was an average of 4.1 (3.3-4.9) day/mm. All four patients were satisfied with the functional and cosmetic results. One patient scored 5 points and the others 4 points on the functional assessment score (Table 3). There was a tendency towards improvement in forearm pronation/supination and elbow flexion/extension lag, however, we were unable to determine any significant statistical improvement. Only one complication occurred in the forearm during the distraction osteogenesis procedure. This callus fracture was treated with a long arm splint for three weeks. Other common complications such as nerve palsies, tightness of the flexor tendons, and pin track sepsis were not found in this series.
Table 3.
Results of Ulnar Lengthening in Four Forearms with Multiple Hereditary Exostosis
DISCUSSION
The pathogenesis of forearm deformities in patients with multiple hereditary exostosis is complex and not yet fully understood. However, there have been several hypotheses to explain this situation. The forearm deformity caused by shortening of the ulnar relative to the radius in patients with multiple hereditary exostosis is related to four factors. First, the cross-sectional area of the distal ulnar physis is only one-quarter that of the distal radius. The distal ulnar physis being significantly smaller means that its growth can be more severely affected by the disease in the wrist.7 Second, the distal ulna is more commonly involved in the condition than the distal radius.4 Third, there is more longitudinal growth at the distal ulnar physis than at the distal radial physis.8 Finally, the distal ulnar physis contributes more to total UL than the distal radial physis contributes to RL. The contribution of the distal ulnar physis versus the distal radius physis to the overall growth of the ulna and the radius are 85 and 75% respectively.5,8 It is evident that although deformities in the upper extremity due to hereditary multiple exostosis are varied, it is well tolerated by most patients. Even when rated solely based on the loss of range of motion, the average physical impairment was slight. Most patients had good preoperative flexion-extension of their wrists and elbows, and motion of forearm pronation-supination was commonly mainly affected. Objective measurements indicated that the measurable clinical function of the hand is largely preserved within the degree of deformity that is customary for these patients. This certifies to the adaptability of growing children when they confronted a slowly developing deformity. However, if the radial head is dislocated, significant limitation to the range of motion of the forearm can observed. Stanton and Hansen6 reported that a dislocated radial head was significantly associated with a loss of pronation, a higher impairment rating, and greater ulnar shortening. It is necessary to treat operatively when the radial head is dislocated.
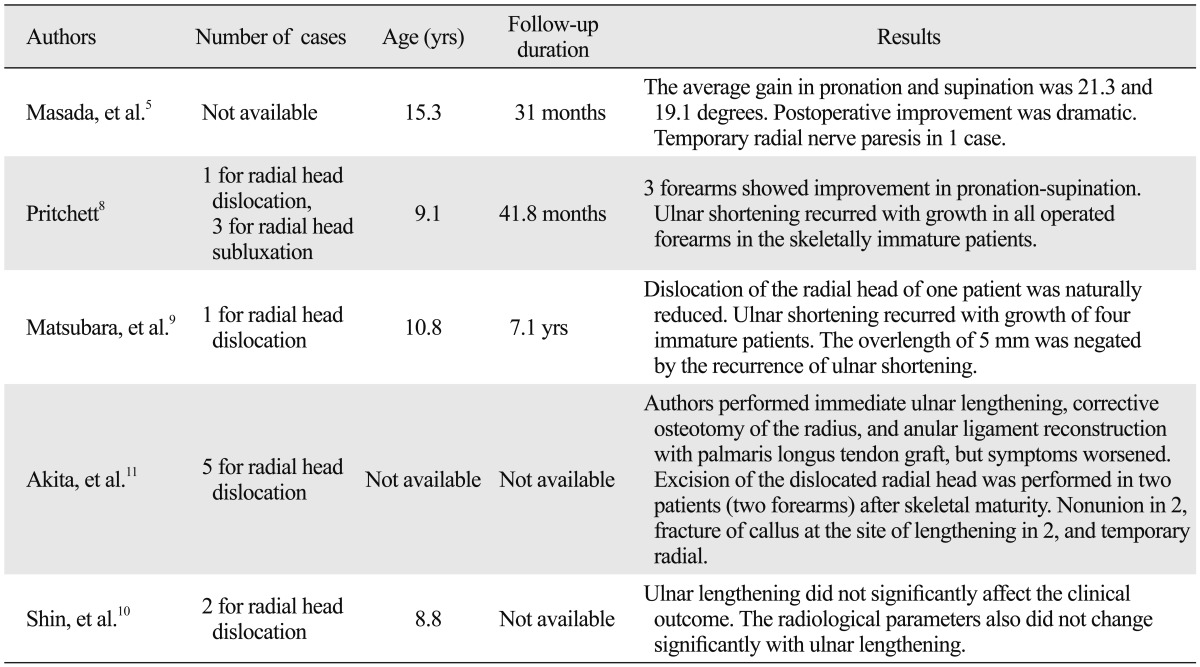
There have been few reports about the results of ulnar lengthening with a dislocated radial head. In 2006, Matsubara, et al. reported that seven forearm cases had radial head dislocation. Dislocation of the radial head of an 11-year-old girl was naturally reduced without any operative intervention after gradual lengthening of the ulna. Ulnar shortening recurred with the growth of four immature patients. In 2007, Akita, et al. reported dislocation of the head of the radius in five extremities/eight forearms. They performed immediate ulnar lengthening, corrective osteotomy of the radius, and annular ligament reconstruction, along with open reduction of the dislocated radial head. These treatments were not effective in either case. Exicision of the dislocated radial head was performed in two patients (two forearms) after their skeletal maturity was reached. Other reports regarding the lengthening of the ulna in patients with radial head dislocation and multiple hereditary exostoses are presented in Table 4.5,8-11
Table 4.
Literature Review of Results of Preoperatively Dislocated Radial Head Treated by Excision of Osteochondroma and Ulnar Gradual Lengthening
Although a number of techniques for the surgical treatment of forearm deformities have been described, the operative treatment for such deformities in patients with multiple hereditary exostosis with radial head dislocation remains unclear. Known surgical interventions include simple excision of the osteochondromas, acute or gradual ulnar lengthening, corrective radial osteotomy, hemi-epiphyseal stapling of the distal radius, creation of a one-bone forearm and the Sauve-Kapandiji procedure.12 The rationale for ulnar lengthening is that the hypoplastic ulna, the keystone of the complex deformity, tethers the radial physis, theoretically diminishing ulnar support of the carpus and increasing ulnar sided pressure on the radial epiphysis. In the present series, progression of the deformity during the growth period was observed in skeletally immature patients. Fortunately, no forearm has yet required a second ulnar lengthening in the four patients so treated.
Exostosis was removed if there was interference with joint movement or if the lesion was prominent, painful, and/or cosmetically undesirable. The indications for performing this procedures were a discrepancy of >5 mm between the lengths of the ulna and radius, a RAA of >30 degrees, a CS of >60%, bowing of the radius, or a combination of these changes.11 Most patients had a combination of these changes. Symptomatic dislocation of the head of the radius was defined as interfering with joint movement.
Ulnar lengthening should theoretically improve ulnar translocation at the wrist, but no statistically significant clinical or radiological improvements were noted in our patients. Fogel, et al.7 performed ten ulnar lengthening procedures in eight patients, and found that relative shortening of the ulna usually recurred after the lengthening and also that, in agreement with our findings, ulnar lengthening did not result in a statistically significant improvement in rotation of the forearm, RAA or CS.
The timing of the surgery is extremely important, and there have been some reports regarding this issue. Some recommend early intervention, which has more potential for remodeling and leads to better surgical results.5,8,13,14 Masada, et al.5 noted recurrence of ulnar shortening after lengthening in 13 forearms. Nine of the 13 forearms also underwent radial osteotomy; it is possible that these improvements were secondary to the osteotomy.
Intervention at a later age is sometimes recommended, because a recurrent operation can be avoided by postponing the procedure and good function can be acquired despite significant deformity after skeletal maturity.15,16
The use of an external fixator causes the interosseous membrane to drag the radius distally. In Type IIb deformities, the use of an external fixator helps to reduce the dislocated radial head.5,8,17
The disadvantage of ulnar lengthening is that the deformity in young patients will recur and further lengthening may be needed. Some patients, particularly those with short arms or asymmetrical involvement, may accept the possible need for additional operations. Pritchett reported the results of ulnar lengthening in ten forearms (eight patients). He found that the deformity tended to recur in younger patients and that further lengthening was sometimes required. He recommended initial overcorrection in skeletally immature patients.8 We therefore over-lengthened by 5 mm in prepubescent patients. Initial overcorrection by 5 mm is well tolerated and is recommended for skeletally immature patients. To prevent recurrence, it is better to over-lengthen the shorter ulna. Most patients required lengthening of between 20 and 40 mm, considering the recurrence. By lengthening gradually, patients can avoid neurovascular system problems and the shorter radius can be lengthened as well. Stapling or hemi-epiphysiodesis of the distal radial physis, or shortening of the radius to prevent recurrence, was reported by Siffert and Levy.18 This procedure is not acceptable because the affected limbs will be shorter. Furthermore, dislocation of the radial head can be reduced using gradual lengthening with an external fixator. Therefore, we believe that our method is a good way to treat forearm deformities caused by osteochondromas.
In conclusion, we treated four patients with dislocated radial heads in the forearm with excision of osteochondromas and gradual lengthening of the ulna with an Ilizarov external fixator. Spontaneous reduction of dislocated radial head was observed in all four cases, and the radiological and clinical results of the procedure were satisfactory.
ACKNOWLEDGEMENTS
This study was approved by Yonsei University Health System, Severence Hospital, Institutional Review Board (IRB# 4-2012-0192).
Footnotes
An abstract of this work was presented at Cairo, 6th International Meeting of the ASAMI 2010.
The authors have no financial conflicts of interest.
References
- 1.Solomon L. Bone growth in diaphysial aclasis. J Bone Joint Surg Br. 1961;43-B:700–716. doi: 10.1302/0301-620X.43B4.700. [DOI] [PubMed] [Google Scholar]
- 2.Wood VE, Sauser D, Mudge D. The treatment of hereditary multiple exostosis of the upper extremity. J Hand Surg Am. 1985;10:505–513. doi: 10.1016/s0363-5023(85)80074-5. [DOI] [PubMed] [Google Scholar]
- 3.Schmale GA, Conrad EU, 3rd, Raskind WH. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am. 1994;76:986–992. doi: 10.2106/00004623-199407000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Shapiro F, Simon S, Glimcher MJ. Hereditary multiple exostoses. Anthropometric, roentgenographic, and clinical aspects. J Bone Joint Surg Am. 1979;61:815–824. [PubMed] [Google Scholar]
- 5.Masada K, Tsuyuguchi Y, Kawai H, Kawabata H, Noguchi K, Ono K. Operations for forearm deformity caused by multiple osteochondromas. J Bone Joint Surg Br. 1989;71:24–29. doi: 10.1302/0301-620X.71B1.2914999. [DOI] [PubMed] [Google Scholar]
- 6.Stanton RP, Hansen MO. Function of the upper extremities in hereditary multiple exostoses. J Bone Joint Surg Am. 1996;78:568–573. doi: 10.2106/00004623-199604000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Fogel GR, McElfresh EC, Peterson HA, Wicklund PT. Management of deformities of the forearm in multiple hereditary osteochondromas. J Bone Joint Surg Am. 1984;66:670–680. [PubMed] [Google Scholar]
- 8.Pritchett JW. Lengthening the ulna in patients with hereditary multiple exostoses. J Bone Joint Surg Br. 1986;68:561–565. doi: 10.1302/0301-620X.68B4.3488318. [DOI] [PubMed] [Google Scholar]
- 9.Matsubara H, Tsuchiya H, Sakurakichi K, Yamashiro T, Watanabe K, Tomita K. Correction and lengthening for deformities of the forearm in multiple cartilaginous exostoses. J Orthop Sci. 2006;11:459–466. doi: 10.1007/s00776-006-1047-4. [DOI] [PubMed] [Google Scholar]
- 10.Shin EK, Jones NF, Lawrence JF. Treatment of multiple hereditary osteochondromas of the forearm in children: a study of surgical procedures. J Bone Joint Surg Br. 2006;88:255–260. doi: 10.1302/0301-620X.88B2.16794. [DOI] [PubMed] [Google Scholar]
- 11.Akita S, Murase T, Yonenobu K, Shimada K, Masada K, Yoshikawa H. Long-term results of surgery for forearm deformities in patients with multiple cartilaginous exostoses. J Bone Joint Surg Am. 2007;89:1993–1999. doi: 10.2106/JBJS.F.01336. [DOI] [PubMed] [Google Scholar]
- 12.Rodgers WB, Hall JE. One-bone forearm as a salvage procedure for recalcitrant forearm deformity in hereditary multiple exostoses. J Pediatr Orthop. 1993;13:587–591. [PubMed] [Google Scholar]
- 13.Peterson HA. Multiple hereditary osteochondromata. Clin Orthop Relat Res. 1989:222–230. [PubMed] [Google Scholar]
- 14.Ip D, Li YH, Chow W, Leong JC. Reconstruction of forearm deformities in multiple cartilaginous exostoses. J Pediatr Orthop B. 2003;12:17–21. doi: 10.1097/01.bpb.0000043728.21564.0d. [DOI] [PubMed] [Google Scholar]
- 15.Abe M, Shirai H, Okamoto M, Onomura T. Lengthening of the forearm by callus distraction. J Hand Surg Br. 1996;21:151–163. doi: 10.1016/s0266-7681(96)80090-8. [DOI] [PubMed] [Google Scholar]
- 16.Arms DM, Strecker WB, Manske PR, Schoenecker PL. Management of forearm deformity in multiple hereditary osteochondromatosis. J Pediatr Orthop. 1997;17:450–454. [PubMed] [Google Scholar]
- 17.Dal Monte A, Andrisano A, Capanna R. Lengthening of the radius or ulna in asymmetrical hypoplasia of the forearm (report on 7 cases) Ital J Orthop Traumatol. 1980;6:329–342. [PubMed] [Google Scholar]
- 18.Siffert RS, Levy RN. Correction of wrist deformity in diaphyseal aclasis by stapling. Report of a case. J Bone Joint Surg Am. 1965;47:1378–1380. [PubMed] [Google Scholar]