Abstract
Purpose
Our study aims to analyze prognosis after implantable cardioverter-defibrillator (ICD) implantation in Korean patients with Brugada syndrome (BrS).
Materials and Methods
This was a retrospective study of BrS patients implanted with an ICD at one of four centers in Korea between January 1998 and April 2012. Sixty-nine patients (68 males, 1 female) were implanted with an ICD based on aborted cardiac arrest (n=38, 55%), history of syncope (n=17, 25%), or induced ven tricular tachyarrhythmia on electrophysiologic study in asymptomatic patients (n=14, 20%). A family history of sudden cardiac death and a spontaneous type 1 electrocardiography (ECG) were noted in 13 patients (19%) and 44 patients (64%), respectively.
Results
During a mean follow-up of 59±46 months, 4.6±5.5 appropri ate shocks were delivered in 19 patients (28%). Fourteen patients (20%) experienced 5.2±8.0 inappropriate shocks caused by supraventricular arrhythmia, lead failure, or abnormal sensing. Six patients were admitted for cardiac causes during follow-up, but no cardiac deaths occurred. An episode of aborted cardiac arrest was a significant predictor of appropriate shock, and the composite of cardiac events in the Cox pro portional hazard model [hazard ratio (95% confidence interval) was 11.34 (1.31-97.94) and 4.78 (1.41-16.22), respectively]. However, a spontaneous type 1 ECG was not a predictor of cardiac events.
Conclusion
Appropriate shock (28%) and inappropriate shock (20%) were noted during a mean follow-up of 59±46 months in Korean BrS patients implanted with an ICD. An episode of aborted cardiac ar rest was the most powerful predictor of cardiac events.
Keywords: Brugada syndrome, implantable cardioverter-defibrillator, sudden death, syncope, Korea
INTRODUCTION
Brugada syndrome (BrS) is a heritable arrhythmogenic disease characterized by a typical electrocardiographic pattern of a coved-type ST-segment elevation, followed by a negative T wave in the right precordial leads (V1 to V3).1 Patients with BrS have an increased risk for sudden cardiac death due to ventricular tachyarrhythmia in a structurally normal heart.2 An implantable cardioverter-defibrillator (ICD) is the first line treatment for this population.2 Data on outcomes during follow-up of ICD therapy in patients with BrS have been published.3,4 Many authors have made an effort to identify high risk patients for sudden cardiac death in order to facilitate the optimal use of ICDs.5,6 A history of aborted sudden cardiac death or syncope and the presence of a spontaneous type 1 Brugada electrocardiography (ECG) have been reported to predict adverse cardiac events.5-7 Risk stratification and the optimal treatment strategy for asymptomatic patients with BrS remain undefined.8 Furthermore, studies on the follow-up of ICD therapy and risk stratification for sudden cardiac death in Korean patients with BrS are limited.
The objective of the present study was to detail clinical outcomes after implantation of ICDs in Korean patients with BrS and to determine which factors can predict adverse cardiac outcomes in these patients.
MATERIALS AND METHODS
This retrospective cohort study included Korean patients who were diagnosed with BrS and underwent ICD therapy at one of four university hospitals in Korea between January 1998 and April 2012. Patients were diagnosed with BrS based on characteristic ECG patterns divided into three categories (types 1 to 3).9 Type 1 ECG was characterized by a prominent coved ST-segment elevation displaying J wave amplitude or ST-segment elevation ≥2 mm or 0.2 mV at its peak followed by a negative T-wave in the right precordial leads.9 Patients were categorized as having spontaneous type 1 ECG when their ECGs showed this characteristic pattern at least once at baseline or during follow-up. Pharmacological provocation test was performed with class 1 antiarrhythmic drug, intravenous flecainide (2 mg/kg body weight over 10 minutes with a maximum of 150 mg). ECGs were reviewed and classified by two experienced cardiologists. The patients who had a history of other heart disease or any evidence of structural heart disease (such as previous myocardial infarction, cardiomyopathy including right ventricular cardiomyopathy, angina, coronary artery disease, or left ventricular hypertrophy) on diagnostic tests such as echocardiography, exercise stress test, or coronary angiography were excluded. Acute ischemia and metabolic or electrolyte disorders were excluded by laboratory tests. Electrophysiologic study was performed for risk stratification based on the clinical judgment of the participating hospitals. A maximum of three ventricular extrastimuli were delivered from two ventricular sites. The electrophysiologic study was considered positive if sustained ventricular arrhythmia was induced.
Initial clinical presentation was categorized as aborted sudden cardiac arrest, syncope, or asymptomatic. Sudden cardiac arrest was defined as a sudden and unexpected cardiac arrest or death occurring within one hour of symptom onset. Syncope was defined as a transient loss of consciousness accompanied by a loss of postural tone. Patients experiencing any other symptoms such as chest pain, dyspnea, and palpitation assumed to be not associated with ventricular tachyarrhythmia were classified into the asymptomatic group. Patient demographics and clinical characteristics, family history of sudden cardiac death or BrS, and electrophysiologic testing were collected from a review of medical records. The dates and causes of all admissions after ICD implantation were investigated.
Single- or dual-chamber ICDs were implanted according to the physician's clinical decision. All data of appropriate and inappropriate shocks were analyzed by experienced specialists. Appropriate shocks were defined as shocks delivered for tachyarrhythmia assumed to be from ventricular origin, considering the onset, stability, QRS morphology, and termination of arrhythmia. Shocks were classified as inappropriate when delivered without ventricular arrhythmia. The composite of cardiac events included appropriate shocks, admission for any cardiac cause, and inappropriate shocks.
Continuous variables are described as mean±SD. Categorical variables are expressed as number and percentage (%). Fisher's exact test or chi-square test was used to investigate statistical differences among frequencies for categorical variables. Kruskal-Wallis test was performed to compare means between the continuous variables. Survival curves were plotted using the Kaplan-Meier method for different subgroups and compared using the log-rank test. Multivariate analysis using the Cox proportional hazard model was performed to identify independent predictors of appropriate shocks and composite of cardiac events, and the hazard ratio (HR) and the 95% confidence interval (CI) were calculated. Time from ICD implantation to the first event was analyzed using a model which included the following variables: initial clinical presentation, family history of sudden cardiac death, and the presence of spontaneous type 1 ECG pattern. A p value <0.05 was considered to be statistically significant. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 18.0 for Windows (SPSS Inc., Chicago, IL, USA).
RESULTS
Sixty-nine patients with BrS implanted with an ICD at one of four centers in Korea were included in this study. The study population consisted of 68 males and one female, with a mean age of 46.2±13.5 years (range, 18 to 86 years) at the time of ICD implantation. Baseline characteristics of our study population are presented in Table 1. Forty-four patients (64%) had spontaneous type 1 ECG. Among the remaining patients who had type 2 or type 3 on resting ECG, 2 patients were revealed to have type 1 ECG after provocation test with a class 1 antiarrhythmic drug. ICDs were implanted based on an episode of aborted cardiac arrest (n=38, 55%) or syncope of unknown origin (n=17, 25%). Asymptomatic patients (n=14, 20%) were implanted with ICDs because of induced ventricular tachyarrhythmia on electrophysiologic study. Table 2 shows the patients' baseline characteristics according to initial clinical presentation. The patients in the asymptomatic group were diagnosed with BrS mainly on routine health examination or a family screening test. Five patients in this asymptomatic group had other symptoms assumed to not be associated with ventricular tachyarrhythmia (3 patients, palpitation; 1 patient, chest pain; 1 patient, dyspnea). Six patients had nocturnal agonal respiration, all of whom had an episode of aborted cardiac arrest or syncope. Family history of sudden cardiac death and BrS were noted in 13 patients (19%) and 4 patients (6%), respectively.
Table 1.
Baseline Characteristics of Korean Brugada Syndrome Patients Implanted with an Implantable Cardioverter-Defibrillator
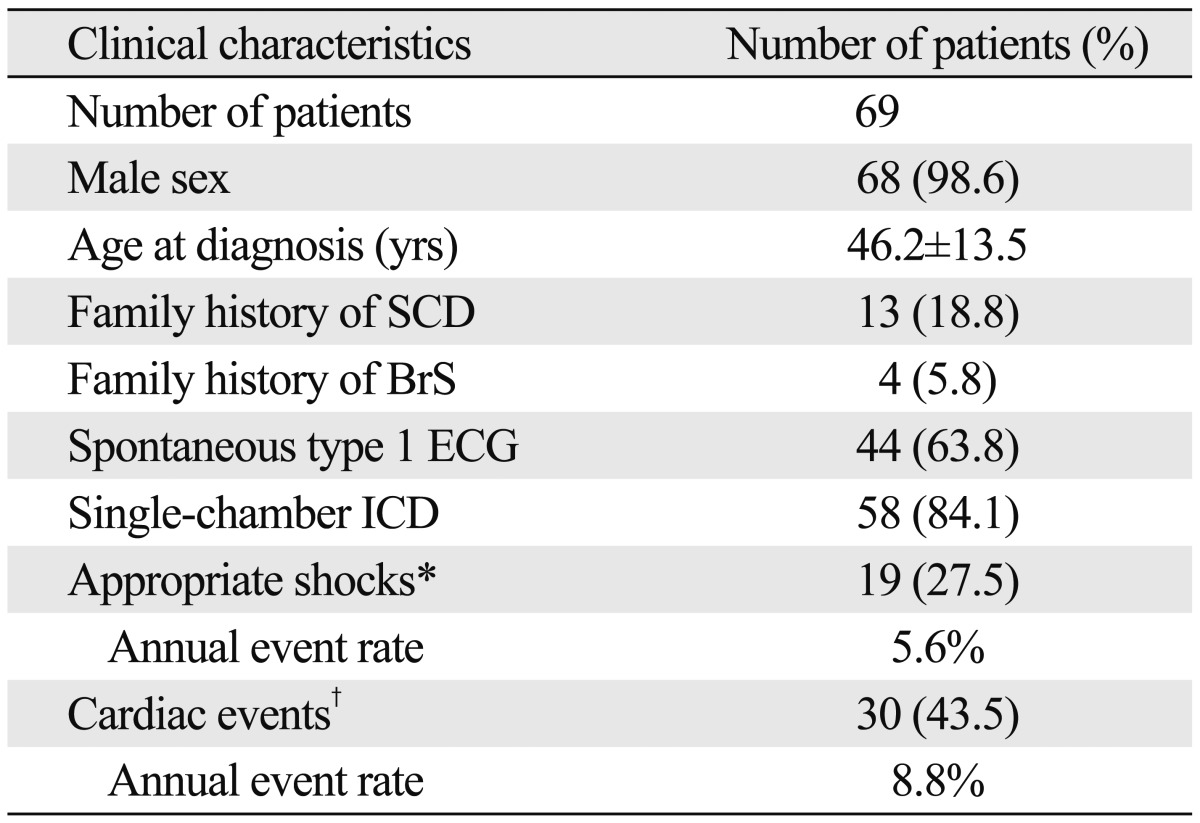
BrS, Brugada syndrome; ECG, electrocardiography; ICD, implantable cardioverter-defibrillator; SCD, sudden cardiac death; SD, standard deviation.
Data are expressed as mean±SD or as number (%).
*Number of patients who experienced appropriate shocks during the follow-up period.
†Number of patients who experienced appropriate shocks, inappropriate shocks, or an unplanned admission for a cardiac cause.
Table 2.
Baseline Characteristics According to the Initial Clinical Presentation
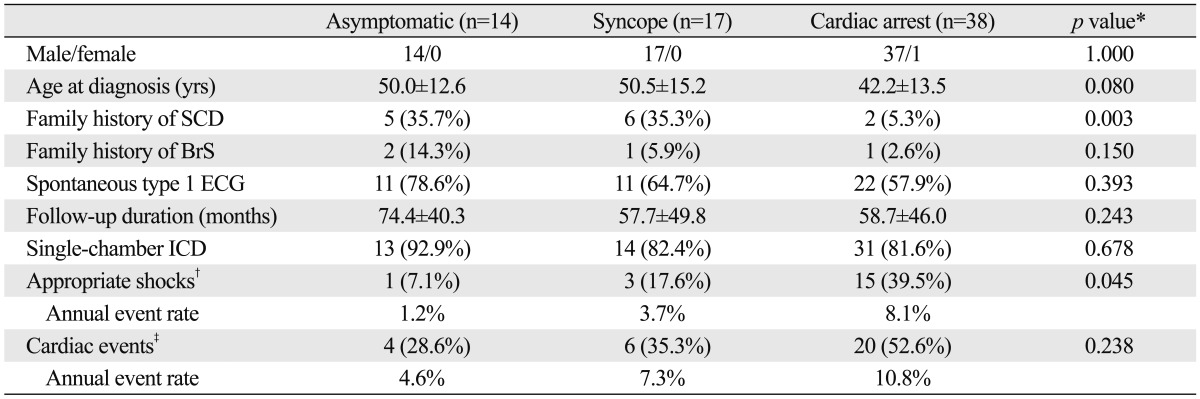
BrS, Brugada syndrome; ECG, electrocardiography; ICD, implantable cardioverter-defibrillator; SCD, sudden cardiac death; SD, standard deviation.
Data are expressed as mean±SD or as number (%). In the analysis of the frequency of family history of SCD, cardiac arrest vs. syncope group (p=0.008) and cardiac arrest vs. asymptomatic patients (p=0.011) showed statistically significant differences. In the analysis of appropriate shocks, difference between cardiac arrest and asymptomatic groups was statistically significant (p=0.040).
*p values were calculated with Fisher's exact test or chi-square test for categorical variables and Kruskal-Wallis test for continuous variables.
†Number of patients who experienced appropriate shocks during the follow-up period.
‡Number of patients who experienced appropriate shocks, inappropriate shocks, or an unplanned admission for a cardiac cause.
We analyzed clinical characteristics according to ECG type (Type 1 pattern spontaneously or after drug challenge test vs. Type 2 or 3 ECG pattern). Statistically significant differences of clinical characteristics between the two groups were not found (Table 3).
Table 3.
Baseline Characteristics According to the Electrocardiographic Type
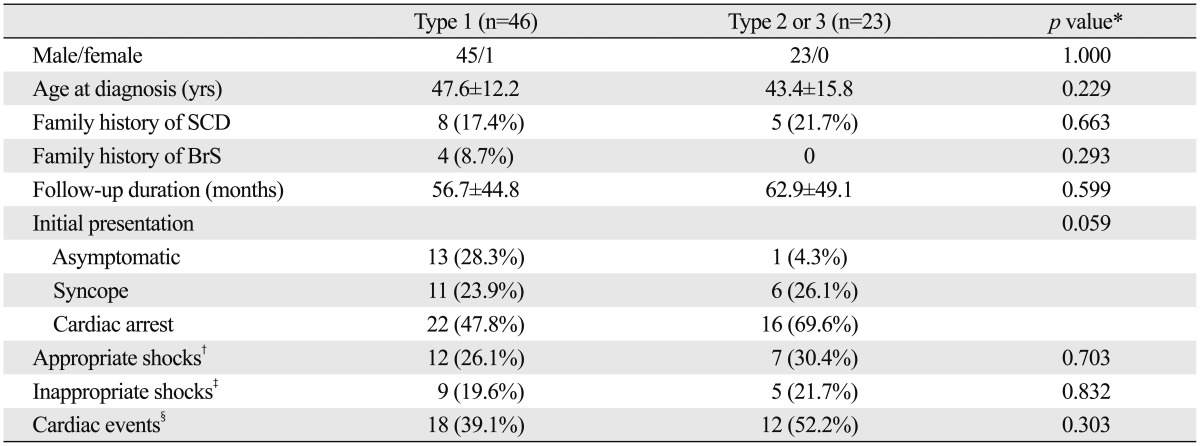
BrS, Brugada syndrome; SCD, sudden cardiac death; SD, standard deviation.
Data are expressed as mean±SD or as number (%).
*p values were calculated with Fisher's exact test or chi-square test for categorical variables and Student's t-test for continuous variables.
†Number of patients who experienced appropriate shocks during the follow-up period.
‡Number of patients who experienced inappropriate shocks during the follow-up period.
§Number of patients who experienced appropriate shocks, inappropriate shocks, or an unplanned admission for a cardiac cause.
A single-chamber ICD was implanted in 58 patients (84%), and a dual-chamber ICD was implanted in 11 patients (16%). During a mean follow-up of 59±46 months (range, 1 to 166 months) after ICD implantation, 19 patients (28%) experienced 88 episodes of appropriate shocks (4.6±5.5 shocks per patient, range 1 to 23). The mean time from ICD implantation to first appropriate shock was 16±22 months (range, 11 days to 89 months). Seventy-three inappropriate shocks (5.2±8.0 shocks per patients, range 1 to 29) were delivered in 14 patients (20%) with a mean time to first inappropriate shock of 28±32 months (range, 53 days to 89 months). The leading cause of inappropriate shock was supraventricular arrhythmia (6 patients) such as sinus tachycardia, atrial fibrillation, and atrial tachycardia. Lead failure (2 patients) and abnormal sensing (2 patients) were other causes. During the follow-up period, 6 patients (9%) were admitted for cardiac causes. No patient died from cardiac causes, but a 47-year-old male patient died of lung cancer three years after ICD implantation.
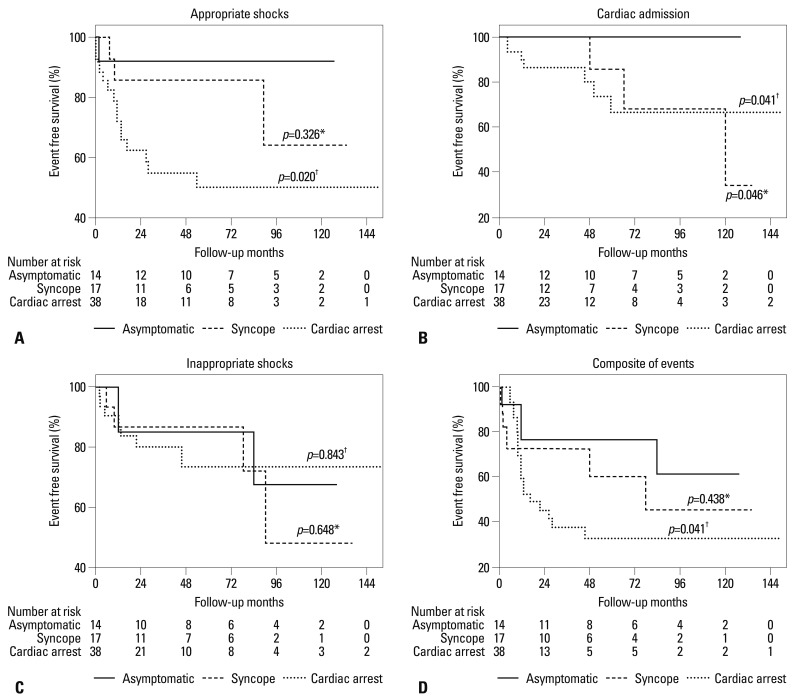
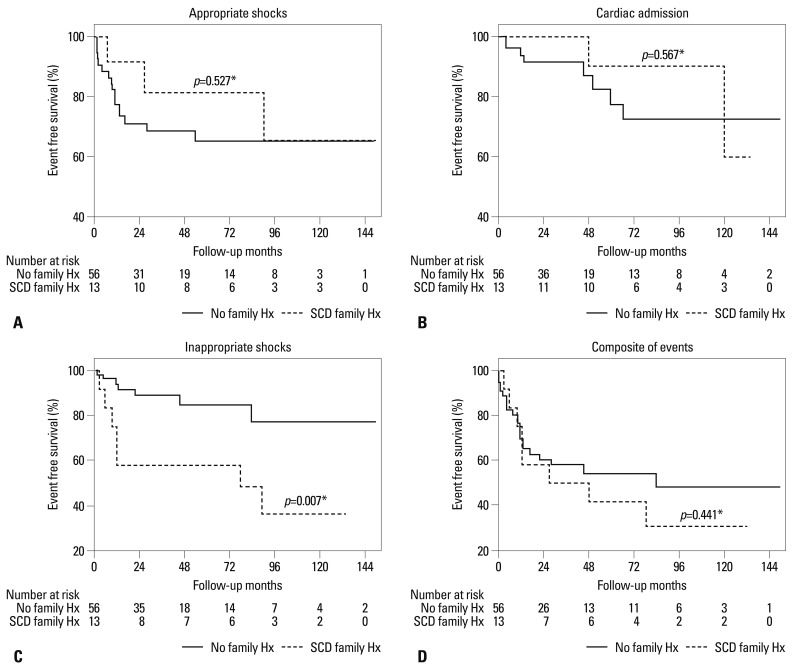
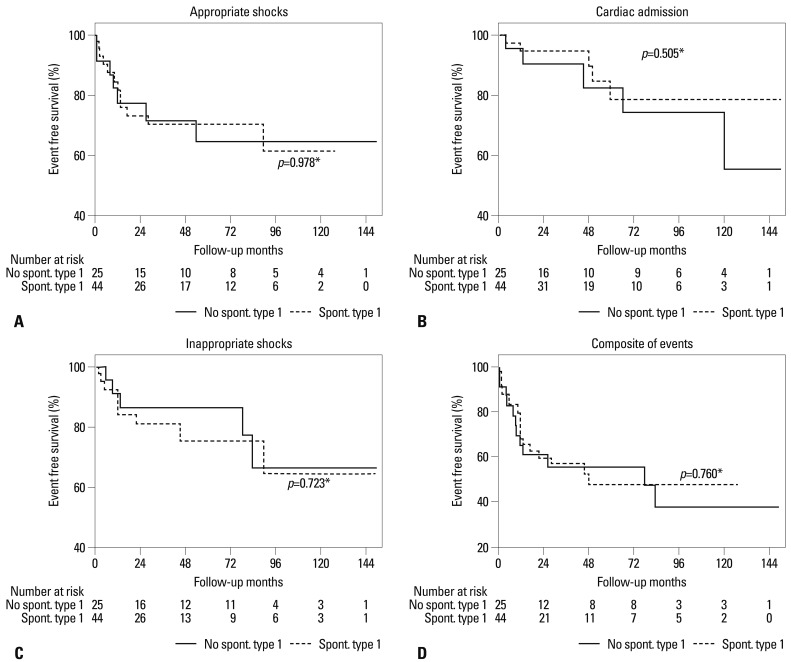
Kaplan-Meier curves of each cardiac event in the three different groups classified by initial clinical presentation are presented in Fig. 1. Patients with aborted cardiac arrest had a shorter time to first appropriate shock than asymptomatic patients (p=0.020), but appropriate shock-free survival was not significantly different between patients with a history of syncope and asymptomatic patients (p=0.326). A history of aborted cardiac arrest or syncope predicted a significantly shorter cardiac admission-free survival (p=0.041 and 0.046, respectively). Aborted cardiac arrest was associated with shorter event-free survival based on the composite of adverse cardiac events compared with the asymptomatic group (p=0.041). A family history of sudden cardiac death had a significant association with inappropriate shock, but not with other outcomes (Fig. 2). The presence of spontaneous type 1 ECG demonstrated no statistical differences in any cardiac event (Fig. 3). Univariate and multivariate Cox proportional hazard models for appropriate shocks, inappropriate shocks, or composite of cardiac events are presented in Table 4. Time to first event in appropriate shocks and the composite of cardiac events were shorter in patients with aborted cardiac arrest than in asymptomatic patients [HR (95% CI) was 11.34 (1.31-97.94) and 4.78 (1.41-16.22), respectively]. A history of syncope seemed to be associated with shorter appropriate shock-free survival, but was not statistically significant (p=0.329). Of 3 patients with a history of syncope who experienced appropriate shocks, one patient had nocturnal agonal respiration, and 2 patients had no associated symptoms except an episode of syncope. Six syncope patients who had had concomitant presyncope (n=3), palpitation (n=3), dyspnea (n=1), or chest pain (n=1) did not experience any appropriate shock. Of 69 patients with BrS in our study, 10 patients complained of palpitation at diagnosis. Only one of 10 patients with palpitations, episodes of aborted cardiac arrest and syncope experienced appropriate shock during the follow-up period. Appropriate shock did not occur in 3 patients who had dyspnea. Appropriate shock was delivered in one patient who had a history of aborted cardiac arrest, of a total of 7 patients who complained of chest pain. A family history of sudden cardiac death was significantly associated with the composite of cardiac events (Table 4), mainly due to its association with a shorter inappropriate shock-free survival. We included age, the presence of palpitations, and supraventricular tachycardia before implantation of ICD in the multivariate model to investigate predictive factors of inappropriate shocks. While a family history of sudden cardiac death was a significant predictor of inappropriate shock [HR (95% CI) was 6.62 (1.64-26.71)], the presence of palpitations or supraventricular tachycardia was not.
Fig. 1.
Kaplan-Meier analysis of cardiac event-free survival, based on initial clinical presentation. (A) Appropriate shock-free survival. (B) Cardiac admission-free survival. (C) Inappropriate shock-free survival. (D) Composite of events (appropriate shock, cardiac admission, and inappropriate shock). *p was obtained by the log-rank test comparing patients with a history of syncope to asymptomatic patients. †p was obtained by the log-rank test comparing patients with an episode of aborted cardiac arrest to asymptomatic patients.
Fig. 2.
Kaplan-Meier analysis of cardiac event-free survival, based on the presence of a family history of sudden cardiac death. (A) Appropriate shock-free survival. (B) Cardiac admission-free survival. (C) Inappropriate shock-free survival. (D) Composite of events (appropriate shock, cardiac admission, and inappropriate shock). SCD indicates sudden cardiac death. *p was obtained by the log-rank test comparing patients with and without a family history of sudden cardiac death. SCD, sudden cardiac death.
Fig. 3.
Kaplan-Meier analysis of cardiac event-free survival, based on the presence of a spontaneous type 1 ECG pattern. (A) Appropriate shock-free survival. (B) Cardiac admission-free survival. (C) Inappropriate shock-free survival. (D) Composite of events (appropriate shock, cardiac admission, and inappropriate shock). *p was obtained by the log-rank test comparing patients with and without a spontaneous type 1 ECG pattern. ECG, electrocardiography.
Table 4.
Univariate and Multivariate Analyses Using the Cox Proportional Hazard Model for Cardiac Events
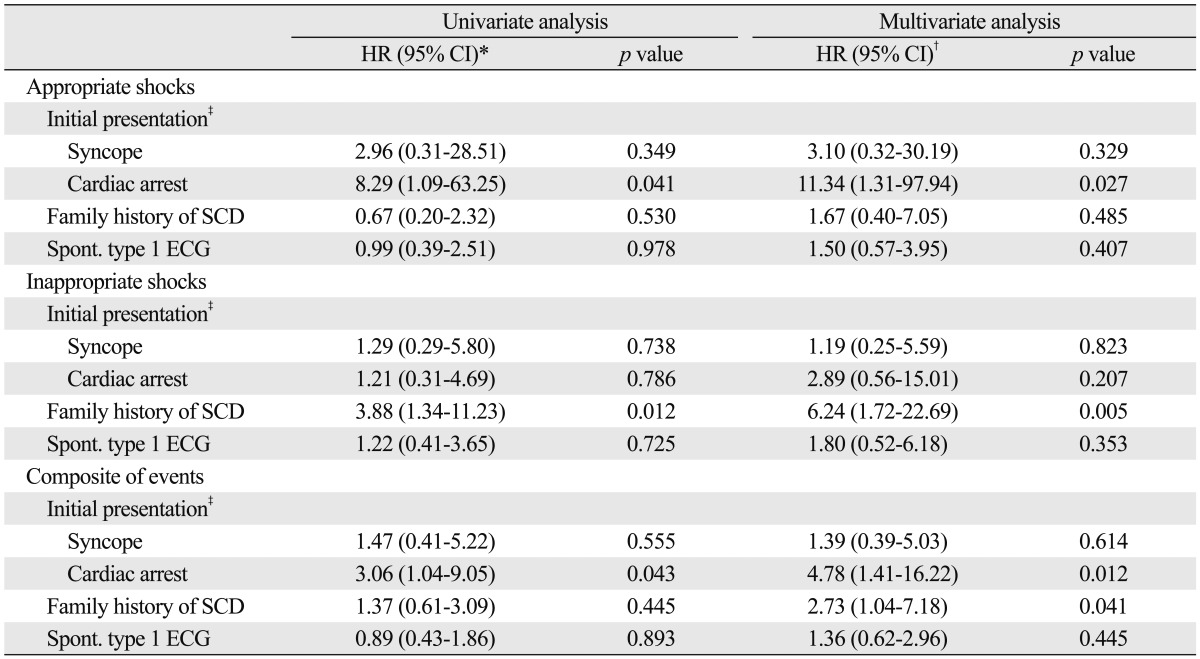
ECG, electrocardiography; SCD, sudden cardiac death; HR, hazard ratio; CI, confidence interval.
*HR and 95% CI for appropriate shocks, inappropriate shocks, or composite of appropriate shocks, unplanned admission for cardiac cause, and inappropriate shocks was obtained with univariate Cox proportional hazard model for each clinical variable.
†HR and 95% CI for appropriate shocks, inappropriate shocks, or composite of appropriate shocks, unplanned admission for cardiac cause, and inappropriate shocks was obtained using the multivariate Cox proportional hazard model including all the clinical variables (initial presentation, family history of SCD, and spontaneous type 1 ECG).
‡HR (95% CI) according to initial clinical presentation for each cardiac event was calculated using the asymptomatic group as the reference category.
DISCUSSION
This study analyzed clinical outcomes after ICD implantation in Korean patients with BrS and investigated factors that may predict these outcomes. During a mean follow-up period of five years, 19 patients (28%) experienced appropriate shocks for ventricular tachyarrhythmia. The frequency of inappropriate shocks (14/69, 20%) was lower than that of appropriate shocks in our study population, contrary to previous studies that reported a higher inappropriate shock rate (20.5% or 36.2%).3,4 No cardiac deaths occurred during the follow-up period.
An episode of aborted cardiac arrest was the most powerful predictor of adverse cardiac events in our population. It was significantly associated with appropriate shocks, cardiac admission, and the composite of cardiac events in our analysis. ICD implantation as secondary prevention for patients with an episode of aborted cardiac arrest is the current consensus.10 A history of syncope and spontaneous type 1 ECG have been reported to be predictors of arrhythmic events,5,11 but failed to show significant association with cardiac events in our study. Other studies on the outcomes of ICD implantation in patients with Brugada syndrome have shown similar results.4 We found a statistically significant association between an episode of syncope and cardiac admission (p=0.046 by long-rank test in Kaplan-Meier analysis). A recent study reported that only 40% of syncope episodes in patients with BrS appeared to be arrhythmic events when considering clinical features, and that the remaining 60% of syncope episodes were poor predictors of future arrhythmic events.12 This finding may explain the weak correlation between an episode of syncope and cardiac event-free survival in our analysis. Associated symptoms and signs such as the presence of prodromes, triggering circumstances, blurred vision, and duration of loss of consciousness can be useful to predict the prognosis of syncope in patients with BrS.12,13 It is important to conduct a thorough investigation into the clinical features of syncope episodes in patients with BrS in order to identify optimal candidates for ICD therapy. In our study, an episode of syncope seemed to be associated with appropriate shock when the patients had nocturnal agonal respiration. On the other hand, the presence of other associated symptoms such as presyncope, palpitation, chest pain, or dyspnea was not predictive for appropriate shocks. None of the 18 patients who complained of these symptoms experienced appropriate shocks except for two patients who also had a history of aborted cardiac arrest. The ECG pattern can fluctuate among the three aforementioned types in the same patient with BrS.2,14 A prospective study has reported high variability between diagnostic and non-diagnostic ECGs in BrS and recommended repetitive ECG recordings for proper risk stratification.15 ECG patterns in BrS can change depending on multiple factors such as fever, vagotonic agents, and meals.2,16 This variability of ECG patterns in BrS might have weaken the predictive power of spontaneous type 1 ECG for cardiac events in our study. Guidelines on number, timing, and patient condition are needed to determine proper performance of ECGs for confirmation of spontaneous type 1 ECG. In accordance with the results of our study, a family history of sudden cardiac death has been reported to be not a significant predictor of cardiac events.8 Interestingly, a family history of sudden cardiac death predicted shorter inappropriate shock-free survival in our analysis, but the underlying mechanism of this finding is unclear.
Most patients of this study were male (68 males and 1 female). It is known that BrS shows an autosomal dominant mode of transmission with low penetrance. Despite equal genetic transmission of the disease, the clinical phenotype is eight to ten times more prevalent in males than in females. The explanation for this interesting sex-related difference remains unknown. It has been noted that the Ito-mediated action potential dome is a prerequisite for the development of phase 2 reentry-dependent tachyarrhythmia, and that BrS is predominantly seen in males, whose Ito is significantly greater than that seen in females.17 We need to further elucidate the ionic and cellular basis of BrS.
The main limitations of this study are its retrospective design and the limited number of patients. Because of its retrospective nature, some important clinical characteristics and events could have been missed despite our attempts to thoroughly review of medical records. The small number of patients may have weakened our ability to confirm statistical significance in our analysis. Second, we included patients with type 2 or 3 ECG, and drug provocation tests were not performed for all patients. Our inclusion criteria differed from those of some other studies5,11 that included only patients with type 1 ECG (spontaneous or pharmacologically induced), therefore, they may have affected the cardiac events and clinical characteristics in our study. However, the pharmacological provocation test has been suggested to have no additional benefit for risk stratification in asymptomatic individuals with a nondiagnostic Brugada ECG.18,19 Additionally, we did not standardize the number or timing in the ECG recordings. These limitations of our study were mainly due to the retrospective multicenter study design. If drug provocation tests were performed for more patients and ECGs were serially performed with standardization of number and timing, a type 1 ECG pattern may have been uncovered in more cases. Third, this study lacked details on features of syncope events. Although experienced cardiologists reviewed the episodes of syncope and included only syncope of unknown origin, systematic comparison of its characteristics such as triggering circumstances, prodromes, and duration of loss of consciousness could help differentiate between benign and high-risk syncope. BrS is an autosomal dominant inherited disease, and mutations in the SCN5A gene were demonstrated to be the most common genotype in BrS patients,2 and the SCN5A mutation was found in one Korean BrS family.20 Genetic analysis was not performed in our study and may pose as another limitation. However, in a previous FINGER registry, the presence of an SCN5A mutation was not predictive of arrhythmic events.8
In conclusion, our study presented the clinical outcomes after ICD implantation in Korean patients with BrS. ICD was an effective therapy, since the appropriate shock rate (28%) in our study population was higher than the inappropriate shock rate (20%). An episode of aborted cardiac arrest was the most powerful predictor of future cardiac events. For correct risk stratification, the identification of high risk syncope and diagnostic ECGs must be standardized.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Mizusawa Y, Wilde AA. Brugada syndrome. Circ Arrhythm Electrophysiol. 2012;5:606–616. doi: 10.1161/CIRCEP.111.964577. [DOI] [PubMed] [Google Scholar]
- 2.Berne P, Brugada J. Brugada syndrome 2012. Circ J. 2012;76:1563–1571. doi: 10.1253/circj.cj-12-0717. [DOI] [PubMed] [Google Scholar]
- 3.Sarkozy A, Boussy T, Kourgiannides G, Chierchia GB, Richter S, De Potter T, et al. Long-term follow-up of primary prophylactic implantable cardioverter-defibrillator therapy in Brugada syndrome. Eur Heart J. 2007;28:334–344. doi: 10.1093/eurheartj/ehl450. [DOI] [PubMed] [Google Scholar]
- 4.Sacher F, Probst V, Iesaka Y, Jacon P, Laborderie J, Mizon-Gérard F, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study. Circulation. 2006;114:2317–2324. doi: 10.1161/CIRCULATIONAHA.106.628537. [DOI] [PubMed] [Google Scholar]
- 5.Eckardt L, Probst V, Smits JP, Bahr ES, Wolpert C, Schimpf R, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005;111:257–263. doi: 10.1161/01.CIR.0000153267.21278.8D. [DOI] [PubMed] [Google Scholar]
- 6.Priori SG, Napolitano C, Gasparini M, Pappone C, Della Bella P, Giordano U, et al. Natural history of Brugada syndrome: insights for risk stratification and management. Circulation. 2002;105:1342–1347. doi: 10.1161/hc1102.105288. [DOI] [PubMed] [Google Scholar]
- 7.Gehi AK, Duong TD, Metz LD, Gomes JA, Mehta D. Risk stratification of individuals with the Brugada electrocardiogram: a meta-analysis. J Cardiovasc Electrophysiol. 2006;17:577–583. doi: 10.1111/j.1540-8167.2006.00455.x. [DOI] [PubMed] [Google Scholar]
- 8.Probst V, Veltmann C, Eckardt L, Meregalli PG, Gaita F, Tan HL, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635–643. doi: 10.1161/CIRCULATIONAHA.109.887026. [DOI] [PubMed] [Google Scholar]
- 9.Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, et al. Proposed diagnostic criteria for the Brugada syndrome: consensus report. Circulation. 2002;106:2514–2519. doi: 10.1161/01.cir.0000034169.45752.4a. [DOI] [PubMed] [Google Scholar]
- 10.European Heart Rhythm Association; Heart Rhythm Society. Zipes DP, Camm AJ, Borggrefe M, Buxton AE, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) J Am Coll Cardiol. 2006;48:e247–e346. doi: 10.1016/j.jacc.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Priori SG, Gasparini M, Napolitano C, Della Bella P, Ottonelli AG, Sassone B, et al. Risk stratification in Brugada syndrome: results of the PRELUDE (PRogrammed ELectrical stimUlation preDictive valuE) registry. J Am Coll Cardiol. 2012;59:37–45. doi: 10.1016/j.jacc.2011.08.064. [DOI] [PubMed] [Google Scholar]
- 12.Sacher F, Arsac F, Wilton SB, Derval N, Denis A, de Guillebon M, et al. Syncope in Brugada syndrome patients: prevalence, characteristics, and outcome. Heart Rhythm. 2012;9:1272–1279. doi: 10.1016/j.hrthm.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 13.Take Y, Morita H, Toh N, Nishii N, Nagase S, Nakamura K, et al. Identification of high-risk syncope related to ventricular fibrillation in patients with Brugada syndrome. Heart Rhythm. 2012;9:752–759. doi: 10.1016/j.hrthm.2011.11.045. [DOI] [PubMed] [Google Scholar]
- 14.Richter S, Sarkozy A, Veltmann C, Chierchia GB, Boussy T, Wolpert C, et al. Variability of the diagnostic ECG pattern in an ICD patient population with Brugada syndrome. J Cardiovasc Electrophysiol. 2009;20:69–75. doi: 10.1111/j.1540-8167.2008.01282.x. [DOI] [PubMed] [Google Scholar]
- 15.Veltmann C, Schimpf R, Echternach C, Eckardt L, Kuschyk J, Streitner F, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006;27:2544–2552. doi: 10.1093/eurheartj/ehl205. [DOI] [PubMed] [Google Scholar]
- 16.Ikeda T, Abe A, Yusu S, Nakamura K, Ishiguro H, Mera H, et al. The full stomach test as a novel diagnostic technique for identifying patients at risk of Brugada syndrome. J Cardiovasc Electrophysiol. 2006;17:602–607. doi: 10.1111/j.1540-8167.2006.00424.x. [DOI] [PubMed] [Google Scholar]
- 17.Di Diego JM, Cordeiro JM, Goodrow RJ, Fish JM, Zygmunt AC, Pérez GJ, et al. Ionic and cellular basis for the predominance of the Brugada syndrome phenotype in males. Circulation. 2002;106:2004–2011. doi: 10.1161/01.cir.0000032002.22105.7a. [DOI] [PubMed] [Google Scholar]
- 18.Zorzi A, Migliore F, Marras E, Marinelli A, Baritussio A, Allocca G, et al. Should all individuals with a nondiagnostic Brugada-electrocardiogram undergo sodium-channel blocker test? Heart Rhythm. 2012;9:909–916. doi: 10.1016/j.hrthm.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 19.Nishizaki M, Sakurada H, Yamawake N, Ueda-Tatsumoto A, Hiraoka M. Low risk for arrhythmic events in asymptomatic patients with drug-induced type 1 ECG. Do patients with drug-induced Brugada type ECG have poor prognosis? (Con) Circ J. 2010;74:2464–2473. doi: 10.1253/circj.cj-10-0878. [DOI] [PubMed] [Google Scholar]
- 20.Lee YS, Baek JS, Kim SY, Seo SW, Kwon BS, Kim GB, et al. Childhood brugada syndrome in two korean families. Korean Circ J. 2010;40:143–147. doi: 10.4070/kcj.2010.40.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]