Abstract
Purpose
To evaluate the diagnostic performance of maternal inflammatory marker: C-reactive protein (CRP) in predicting early onset neonatal sepsis (that occurring within 72 hours after birth).
Materials and Methods
126 low birth weight newborns (gestation 32±3.2 wk, birth weight 1887±623 g) and their mothers were included. Neonates were divided into sepsis group (n=51) including both proven (positive blood culture) and suspected (negative blood culture but with more than 3 abnormal clinical signs), and controls (n=75). Mothers were subgrouped into CRP positive ≥1.22 mg/dL (n=48) and CRP negative <1.22 mg/dL (n=78) group, determined by Receiver Operating Characteristic curves, and odds ratio was calculated for neonatal sepsis according to maternal condition.
Results
Maternal CRP was significantly higher in neonatal sepsis group than in control (3.55±2.69 vs. 0.48±0.31 mg/dL, p=0.0001). Maternal CRP (cutoff value >1.22 mg/dL) had sensitivity 71% and specificity 84% for predicting neonatal sepsis. Maternal CRP positive group had more neonatal sepsis than CRP negative group (71% vs. 29%, p<0.001). Odds ratio of neonatal sepsis in maternal CRP positive group versus CRP negative group was 10.68 (95% confidence interval: 4.313-26.428, p<0.001).
Conclusion
The risk of early onset neonatal sepsis significantly increased in the case of positive maternal CRP (≥1.22 mg/dL). In newborn of CRP positive mother, the clinician may be alerted to earlier evaluation for possible neonatal infection prior to development of sepsis.
Keywords: Neonatal sepsis, chorioamnionitis, maternal C-reacitve protein
INTRODUCTION
Maternal and peripartum risk factors influence early onset neonatal sepsis. The most frequent risk factors are chorioamnionitis and maternal systemic infection.1,2 Intrauterine infection increases morbidity and mortality of diseases such as severe maternal infectious shock, disseminated intravascular coagulopathy, adult respiratory distress syndrome (RDS), and renal failure.3 Also, intrauterine infection and inflammation induce preterm labor at least one-third of spontaneous preterm deliveres.4,5 The 12.7% of all pregnancies is preterm birth in the United States. Preterm birth is responsible for 75% of perinatal mortality and more than half the long-term morbidity of survivors.6 The birth of preterm infants increases neonatal sepsis, pneumonia, dyspnea, and death rate by 2 to 4 times.7,8 Early-onset sepsis is associates with an increased risk of RDS, bronchopulmonary dysplasia, severe intraventricular hemorrhage or periventricular leukomalacia,9 and transfusion.10 The effect of risk of intrauterine infection on fetus and neonate is higher than on the mother.11
Simple, rapid, noninvasive, and safe tests of markers of intrauterine infection could be useful in prediction of morbidity among pregnant women, with or without labor. If maternal infections during pregnancy are diagnosed and treated early, the mortality and morbidity of neonates should be decreased.
In the literature, several diagnostic methods of peripartum intrauterine infection have been considered. There are amnionic fluid culture, procalcitonin, C-reactive protein (CRP) interleukin (IL)-6, IL-8, IL-10, IL-18, tumor necrosis factor-alpha (TNF-alpha), interferon gamma, and others.12 Of them, maternal CRP has been reported to be valuable for early detection of neonatal sepsis.13,14 Conflicting results on use of maternal CRP in prediction of neonatal sepsis have been reported.15,16
The objective of the study is to determine the accuracy of maternal serum CRP in prediction of neonatal sepsis.
MATERIALS AND METHODS
We studied the preterm infants (<37 wk) who were admitted to the neonatal intensive care unit, Severance Hospital, from January 2001 to June 2003. We choosed the preterm infants (n=236) and their mothers (n=210) who were examined both a laboratory test and placental pathology in peripartum period. We excluded twins (n=52) and preterm infants who have anormaly, metabolic disease, chromosome and genetic disease. Also, we excluded their mothers who have maternal eclampsia, preeclampsia, hepatitis, cardiovascular disease, rheumatoid disease, gastroenteric disease like as crhon's disease, oncologic disease, polycystic ovary syndrome, and connective tissue disease which cause elevated CRP. Finally, one hundred twenty six preterm infants (gestation 32±3.2 wk, birth weight 1887±623 g,) and their mothers (31±3.6 years, delivery frequency 2.8±1.5 times) were included.
Preterm infants were divided into neonatal sepsis group (51 cases) and control group (75 cases). Neonatal sepsis was defined as proven with positive blood culture (3 cases) and as suspected with negative blood culture, but more than 3 categories of positive clinical signs among 6 categories within 3 days of birth;17 1) longer than 1 hour of unstable body temperature (axillary temperature: fever >37.5℃, hypothermia <36.5℃), 2) cardiovascular abnormality (heart rate <100, or >160 per minute, hypotension requiring inotropics), 3) respiratory abnormality (respiration rate >60 per minute, dyspnea, apnea, increased oxygen demand or treatment with mechanical ventilator), 4) metabolic acidiosis (arterial blood gas analysis: pH <7.35, base deficit ≥6), 5) gastrointestinal tract abnormality (vomiting, abdominal distension, abnormal gastric intolerance, bloody stool and umbilical erythema), 6) neurological abnormality (drowsiness, muscle weakness, excessive irritability and convulsion). In addition, gestational age, birth weight, delivery type, Apgar score, blood test [CRP, white blood cell (WBC)], and culture, use of mechanical ventilator were examined in preterm infants. Neonatal hematologic test was performed at 6 hours after birth. We started ampicillin and gentamycin treatment in newborns with clinical signs18,19 [difficulty feeding, convulsion, movement only when stimulated, repiratory rate ≥60, severe chest indrawing, axillary temperature ≥37.5℃, axillary temperature <35.5℃, the time of premature rupture of membrane (PROM) ≥18 hrs, intrapartum fever ≥38℃ and suspected infection] and positive hematologic results (for example, WBC & CRP increased, platelet decreased <150000) as determined by the clinician at hospital day 1.20 We treated antibiotics in sepsis group (n=51) and control group (n=33).
According to the materal infectious condition, 126 mothers were classified as histological chorioamnionitis (44 cases), clinical chorioamnionitis (15 cases), and other infections group (5 cases) such as intrapartum fever, urinary tract infection, enteritis, and other systemic infectious diseases; and control group (62 cases). Histolgical chorioamnionitis was defined as pathological changes of infection in amnion, chorio-decidua, umbilical cord, or chorionic plate tissues.21 Clinical chorioamnionitis6 was defined by >2 of 6 signs: 1) fever >38℃, 2) hysteralgia, 3) fetal tachydardia (>160 times/minute), 4) maternal tachydardia (>100/minute), 5) malodorous vaginal discharge, 6) increased WBC count (≥12000/mm3). Other infection group was 5 cases: vaginitis caused by candida (1 case), respiratory infection symptoms (2 cases), and enteritis with vomiting and diarrhea (1 case). Mother's age, past parous history, gestation age, presence or absence of PROM, delivery method, blood test (CRP, complete blood count, culture and others), histological findings of the placenta, cervice culture, amniocentesis, and prenatal use of antibiotics were recorded.
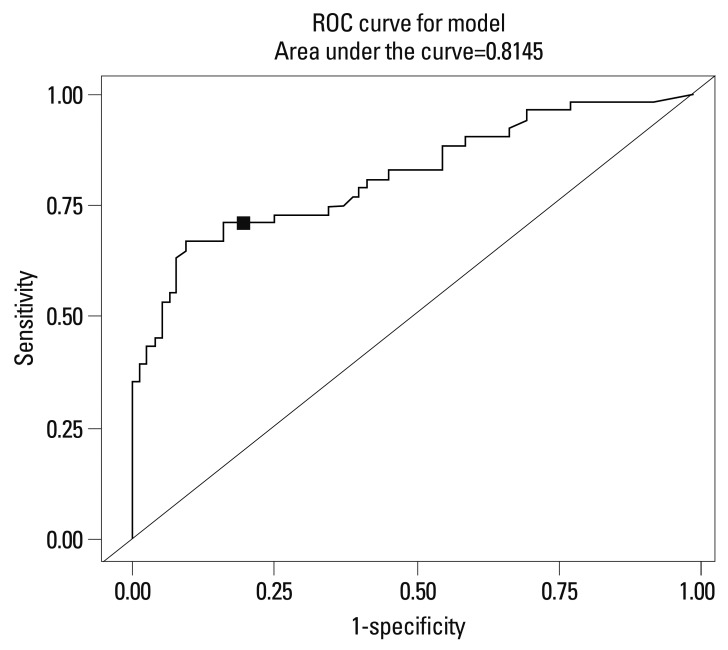
The Receiver Operating Characteristic (ROC) plot22,23 depicts the relation of sensitivity and specificity of maternal CRP to neonatal sepsis. The ROC cutoff value in our study subjects was maternal CRP 1.22 mg/dL with sensitivity 71% and specificity 84%. Based on this value, We defined maternal CRP positive group as CRP ≥1.22 mg/dL and maternal CRP negative group CRP <1.22 mg/dL (Fig. 1). Clinical characteristics of these two groups was compared in relation to neonatal sepsis, histological chorioamnionitis, clinical chorioamnionitis and other infection groups.
Fig. 1.
Cutoff value determined by Receive Operating Characteristic (ROC) curves: sensitivity 71%, specificity 84%.
CRP was measured by nephlometry using the Beckman Array System protein analyzer (Global Medical Instrumentation, Inc., Ramsey, MN, USA).
Statistical analysis
For data analysis, SAS v9.2 was used. Student t-test and Fisher's exact test were used for comparison of two variables. The relative risk of neonatal sepsis according to maternal infection status, and maternal CRP positive group versus negative group, were analyzed by logistic regression. Statistical significance was defined as p-value <0.05.
RESULTS
Comparison of neonatal sepsis and control groups
In the neonatal sepsis group, gestational age was lower than controls. Neonatal CRP performed on day of admission in the sepsis group was significantly higher than controls (Table 1). The maternal CRP of neonatal sepsis group was 3.03 (±2.93) mg/dL, significantly higher than controls 0.71 (±0.65), p-value was <0.001. In the neonatal sepsis group, histological chorioamnionitis was more frequent than controls; clinical chorioamnionitis, other infection group, and the use antibiotics were higher in sepsis than controls, but was not statistically significant (Table 2). The mortality rate was 6 among total 126 cases (4.8%), and were all in the sepsis group (51 cases), or 12.8% (6 cases/51 cases).
Table 1.
Characteristics of Newborns with Neonatal Sepsis
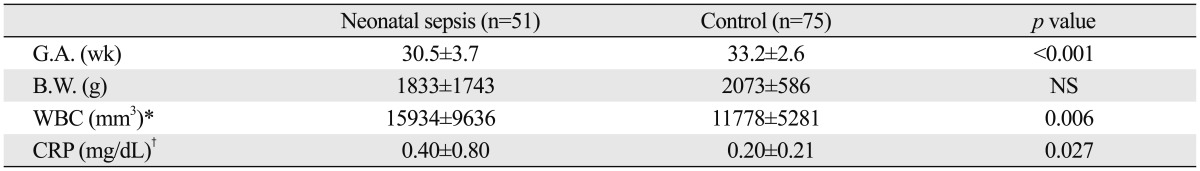
NS, not significant; WBC, white blood cell; CRP, C-reactive protein; G.A., gestational age; B.W., birth weight; SD, standard deviation.
Data mean±SD.
*At birth, WBC.
†At birth, CRP.
Table 2.
Demographic Characteristics of Mothers with Neonatal Sepsis
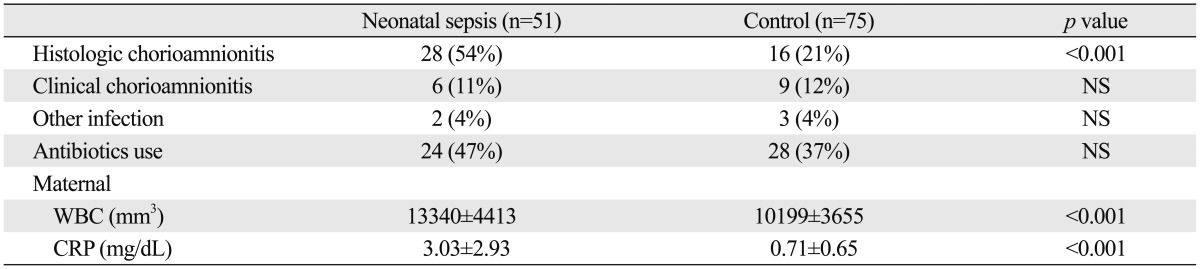
NS, not significant; WBC, white blood cell; CRP, C-reactive protein; SD, standard deviation.
Data mean±SD.
Maternal characteristics by maternal CRP
The maternal CRP positive compared with negative group had more histologic chorioamnionitis and increased WBC count (Table 3).
Table 3.
Maternal Characteristics by Maternal CRP
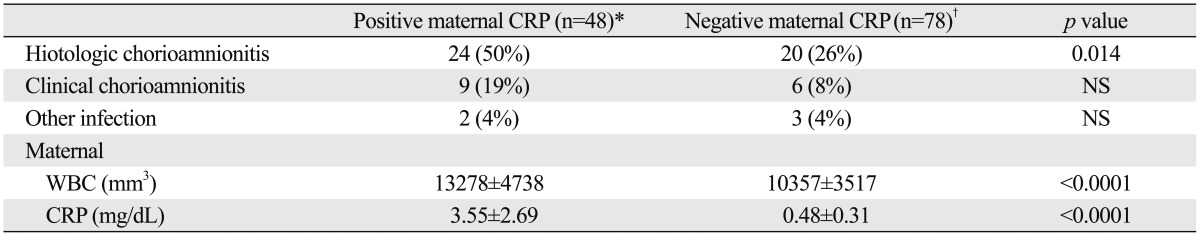
NS, not significant; WBC, white blood cell; CRP, C-reactive protein; SD, standard deviation.
Data mean±SD.
*Cutoff value for positive maternal CRP: ≥1.22 mg/dL.
†Cutoff value for negative maternal CRP: <1.22 mg/dL.
Relative risk of neonatal sepsis
In comparison with the negative group, the relative risk of the maternal CRP positive group for neonatal sepsis was 10.7, (95% confidence interval 4.3-26.4) with p-value of 0.001 (Table 4).
Table 4.
Relative Risk of Maternal CRP for Neonatal Sepsis
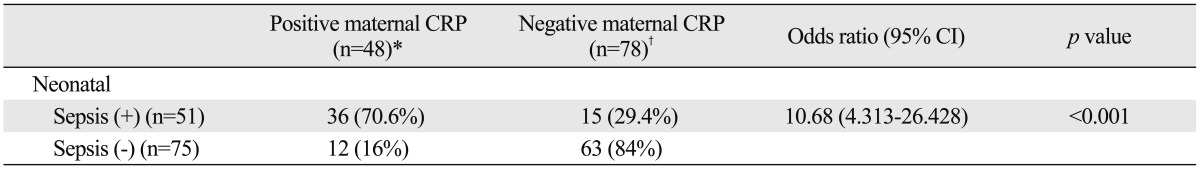
CI, confidence interval; CRP, C-reactive protein.
*Cutoff value for positive maternal CRP: ≥1.22 mg/dL.
†Cutoff value for negative maternal CRP: <1.22 mg/dL.
DISCUSSION
In this study, we found that maternal positive CRP is a risk factor for neonatal sepsis. CRP is an acute phase protein produced in the liver, and has the characteristics of reaching maximal concentration 48 hours after stimulation from cytokines, IL-1, TNF, and particularly IL-6, and decreases to half after 8 or 9 hours. CRP is increased significantly in cases with infection, inflammatory reaction, tissue damage, and tissue necrosis.24 CRP maintains a constant value regardless of the gestation period in pregnancy,25 significantly elevated maternal CRP implies maternal infection and its associated neonatal infection.7 Yoon, et al.7 have reported that maternal WBC and CRP were significiantly increased not only in amniotic fluid culture positive subjects but also in neonatal sepsis. In our study, maternal CRP in neonatal sepsis group was significantly higher compared with controls, reflecting maternal effects on neonatal infection.
Among neonatal sepsis group, blood cultures during hospitalization was confirmed in 3 cases. In the other 48 cases, sepsis was defined by clinical criteria, and blood culture was negative. Clinician were not aware of maternal CRP values. Generally, regarding clinical signs of sepsis, the first signs appeared within 12 hours of birth and in order of frequency, was respiratory distress, cardiovascular (hypotension), and temperature abnormality, for >1 hour. Digestive and neurological abnormality signs occurred 3 days after birth.
By ROC curve, the sensitivity and specificity of maternal CRP for neonatal sepsis in our data (1.22 mg/dL as cutoff point), was 71% and 84%, respectively. Sensitivity and specificity were improved compared with past reports; the cutoff value of CRP 0.7 mg/dL26 was 56% sensitivity and 77% specificity, and using 1.2 mg/dL,27 it was 56% sensitivity, 76% specificity. Recently Celik, et al.28 reported that the cutoff value of CRP 0.48 mg/dL was 67% sensitivity and 97% specificity. Based on this, in maternal CRP positive group, neonatal sepsis incidence occurred in 71%, significantly higher than CRP negative group. Maternal WBC, and mean value of CRP were significantly higher than CRP negative group.
The frequency of maternal histological chorioamnionitis was significantly higher in neonatal sepsis group, and maternal CRP positive group. Thus, maternal infection was associated with increased neonatal sepsis and maternal CRP.
In maternal CRP positive group, the relative risk of neonatal sepsis was 10.7 times greater than the negative group (p<0.001). Neonatal sepsis can be predicted by maternal CRP. Therefore, active treatment of mothers before delivery, intensive follow up observation, and treatment of neonates after delivery should decrease the morbidity and mortality of disease.
In conclusion, maternal positive CRP is a significant risk factor for neonatal sepsis.
Maternal CRP ≥1.22 mg/dL has 71% predictability for diagnosis of neonatal sepsis. Therefore, through the simple maternal CRP test prior to delivery, the risk level of early neonatal sepsis could be predicted.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Schuchat A, Zywicki SS, Dinsmoor MJ, Mercer B, Romaguera J, O'Sullivan MJ, et al. Risk factors and opportunities for prevention of early-onset neonatal sepsis: a multicenter case-control study. Pediatrics. 2000;105(1 Pt 1):21–26. doi: 10.1542/peds.105.1.21. [DOI] [PubMed] [Google Scholar]
- 2.Martius JA, Roos T, Gora B, Oehler MK, Schrod L, Papadopoulos T, et al. Risk factors associated with early-onset sepsis in premature infants. Eur J Obstet Gynecol Reprod Biol. 1999;85:151–158. doi: 10.1016/s0301-2115(99)00018-4. [DOI] [PubMed] [Google Scholar]
- 3.Seaward PG, Hannah ME, Myhr TL, Farine D, Ohlsson A, Wang EE, et al. International multicenter term PROM study: evaluation of predictors of neonatal infection in infants born to patients with premature rupture of membranes at term. Premature Rupture of the Membranes. Am J Obstet Gynecol. 1998;179(3 Pt 1):635–639. doi: 10.1016/s0002-9378(98)70056-0. [DOI] [PubMed] [Google Scholar]
- 4.Romero R, Gotsch F, Pineles B, Kusanovic JP. Inflammation in pregnancy: its roles in reproductive physiology, obstetrical complications, and fetal injury. Nutr Rev. 2007;65(12 Pt 2):S194–S202. doi: 10.1111/j.1753-4887.2007.tb00362.x. [DOI] [PubMed] [Google Scholar]
- 5.Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000;342:1500–1507. doi: 10.1056/NEJM200005183422007. [DOI] [PubMed] [Google Scholar]
- 6.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoon BH, Yang SH, Jun JK, Park KH, Kim CJ, Romero R. Maternal blood C-reactive protein, white blood cell count, and temperature in preterm labor: a comparison with amniotic fluid white blood cell count. Obstet Gynecol. 1996;87:231–237. doi: 10.1016/0029-7844(95)00380-0. [DOI] [PubMed] [Google Scholar]
- 8.Asrat T. Intra-amniotic infection in patients with preterm prelabor rupture of membranes. Pathophysiology, detection, and management. Clin Perinatol. 2001;28:735–751. doi: 10.1016/s0095-5108(03)00074-5. [DOI] [PubMed] [Google Scholar]
- 9.Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Changes in pathogens causing early-onset sepsis in very-low-birth-weight infants. N Engl J Med. 2002;347:240–247. doi: 10.1056/NEJMoa012657. [DOI] [PubMed] [Google Scholar]
- 10.Jeon GW, Sin JB. Risk factors of transfusion in anemia of very low birth weight infants. Yonsei Med J. 2013;54:366–373. doi: 10.3349/ymj.2013.54.2.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eschenbach DA. Amniotic fluid infection and cerebral palsy. Focus on the fetus. JAMA. 1997;278:247–248. [PubMed] [Google Scholar]
- 12.Bender L, Thaarup J, Varming K, Krarup H, Ellermann-Eriksen S, Ebbesen F. Early and late markers for the detection of early-onset neonatal sepsis. Dan Med Bull. 2008;55:219–223. [PubMed] [Google Scholar]
- 13.Hirsch W, Koppitz D, Morack G, Gerhardt C. [C-reactive protein in the maternal serum and risk of fetal infection in premature rupture of the fetal membranes and threatened premature labor] Zentralbl Gynakol. 1989;111:1411–1416. [PubMed] [Google Scholar]
- 14.Skrablin S, Lovric H, Banovic V, Kralik S, Dijakovic A, Kalafatic D. Maternal plasma interleukin-6, interleukin-1beta and C-reactive protein as indicators of tocolysis failure and neonatal outcome after preterm delivery. J Matern Fetal Neonatal Med. 2007;20:335–341. doi: 10.1080/14767050701227877. [DOI] [PubMed] [Google Scholar]
- 15.van der Heyden JL, van Teeffelen SS, Coolen AC, Halbertsma FJ, Aardenburg R, Mertens HJ, et al. Is it useful to measure C-reactive protein and leukocytes in patients with prelabor rupture of membranes? Am J Perinatol. 2010;27:543–547. doi: 10.1055/s-0030-1248941. [DOI] [PubMed] [Google Scholar]
- 16.Trochez-Martinez RD, Smith P, Lamont RF. Use of C-reactive protein as a predictor of chorioamnionitis in preterm prelabour rupture of membranes: a systematic review. BJOG. 2007;114:796–801. doi: 10.1111/j.1471-0528.2007.01385.x. [DOI] [PubMed] [Google Scholar]
- 17.Mehr SS, Sadowsky JL, Doyle LW, Carr J. Sepsis in neonatal intensive care in the late 1990s. J Paediatr Child Health. 2002;38:246–251. doi: 10.1046/j.1440-1754.2002.00768.x. [DOI] [PubMed] [Google Scholar]
- 18.Young Infants Clinical Signs Study Group. Clinical signs that predict severe illness in children under age 2 months: a multicentre study. Lancet. 2008;371:135–142. doi: 10.1016/S0140-6736(08)60106-3. [DOI] [PubMed] [Google Scholar]
- 19.CG Antibiotics for early-onset neonatal infection: antibiotics for the prevention and treatment of early-onset neonatal infection. Manchester: National Institute for Health and Clinical Excellence; 2012. NICE clinical guidesines. [Google Scholar]
- 20.Edmond K, Zaidi A. New approaches to preventing, diagnosing, and treating neonatal sepsis. PLoS Med. 2010;7:e1000213. doi: 10.1371/journal.pmed.1000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoon BH, Romero R, Kim CJ, Jun JK, Gomez R, Choi JH, et al. Amniotic fluid interleukin-6: a sensitive test for antenatal diagnosis of acute inflammatory lesions of preterm placenta and prediction of perinatal morbidity. Am J Obstet Gynecol. 1995;172:960–970. doi: 10.1016/0002-9378(95)90028-4. [DOI] [PubMed] [Google Scholar]
- 22.Beck JR, Shultz EK. The use of relative operating characteristic (ROC) curves in test performance evaluation. Arch Pathol Lab Med. 1986;110:13–20. [PubMed] [Google Scholar]
- 23.Irwin RJ, Irwin TC. A principled approach to setting optimal diagnostic thresholds: where ROC and indifference curves meet. Eur J Intern Med. 2011;22:230–234. doi: 10.1016/j.ejim.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 24.Zimmerman MA, Selzman CH, Cothren C, Sorensen AC, Raeburn CD, Harken AH. Diagnostic implications of C-reactive protein. Arch Surg. 2003;138:220–224. doi: 10.1001/archsurg.138.2.220. [DOI] [PubMed] [Google Scholar]
- 25.Picklesimer AH, Jared HL, Moss K, Offenbacher S, Beck JD, Boggess KA. Racial differences in C-reactive protein levels during normal pregnancy. Am J Obstet Gynecol. 2008;199:523. doi: 10.1016/j.ajog.2008.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoon BH, Jun JK, Park KH, Syn HC, Gomez R, Romero R. Serum C-reactive protein, white blood cell count, and amniotic fluid white blood cell count in women with preterm premature rupture of membranes. Obstet Gynecol. 1996;88:1034–1040. doi: 10.1016/s0029-7844(96)00339-0. [DOI] [PubMed] [Google Scholar]
- 27.Pfeiffer KA, Reinsberg J, Rahmun A, Schmolling J, Krebs D. Clinical application of maternal serum cytokine determination in premature rupture of membranes--interleukin-6, an early predictor of neonatal infection? Acta Obstet Gynecol Scand. 1999;78:774–778. [PubMed] [Google Scholar]
- 28.Celik IH, Demirel FG, Uras N, Oguz SS, Erdeve O, Biyikli Z, et al. What are the cut-off levels for IL-6 and CRP in neonatal sepsis? J Clin Lab Anal. 2010;24:407–412. doi: 10.1002/jcla.20420. [DOI] [PMC free article] [PubMed] [Google Scholar]