Abstract
Background and aims
Clinical lumbar instability causes pain and socioeconomic suffering; however, an appropriate treatment for this condition is unknown. This article examines the effect of a 10 week core stabilization exercise (CSE) program and 3 month follow-up on pain-related outcomes in patients with clinical lumbar instability.
Methods
Forty-two participants with clinical lumbar instability of at least 3 months in duration were randomly allocated either to 10 weekly treatments with CSE or to a conventional group (CG) receiving trunk stretching exercises and hot pack. Pain-related outcomes including pain intensity during instability catch sign, functional disability, patient satisfaction, and health-related quality of life were measured at 10 weeks of intervention and 1 and 3 months after the last intervention session (follow-up); trunk muscle activation patterns measured by surface electromyography were measured at 10 weeks.
Results
CSE showed significantly greater reductions in all pain-related outcomes after 10 weeks and over the course of 3 month follow-up periods than those seen in the CG (P<0.01). Furthermore, CSE enhanced deep abdominal muscle activation better than in the CG (P<0.001), whereas the CG had deterioration of deep back muscle activation compared with the CSE group (P<0.01). For within-group comparison, CSE provided significant improvements in all pain-related outcomes over follow-up (P<0.01), whereas the CG demonstrated reduction in pain intensity during instability catch sign only at 10 weeks (P<0.01). In addition, CSE showed an improvement in deep abdominal muscle activation (P<0.01), whereas the CG revealed the deterioration of deep abdominal and back muscle activations (P<0.05).
Conclusion
Ten week CSE provides greater training and retention effects on pain-related outcomes and induced activation of deep abdominal muscles in patients with clinical lumbar instability compared with conventional treatment.
Keywords: clinical lumbar instability, quality of life, detraining effect, trunk muscle activation, core stabilization exercise
Introduction
Low back pain (LBP) poses a serious challenge to worldwide health care systems. Clinical lumbar instability is a subgroup of LBP.1 It has been described as the inability of the spine to maintain its normal displacement pattern under physiologic loads without any initial or additional neurological deficits, major deformity, or incapacitating pain.2 It results in pain, functional disability, and/or reflexive muscular spasm.3,4 In Thailand, patients with clinical lumbar instability are frequently referred for physical therapy intervention. No specific exercise has been available for this group of patients as of yet.
Core stabilization exercise (CSE) with the abdominal drawing-in maneuver (ADIM) technique has been found to primarily activate the deep abdominal muscles with minimal activity of the superficial muscles. Previous studies promoted the benefits of the CSE in terms of reducing pain and disability for patients with clinical lumbar instability.5–7 It was hypothesized that trunk muscle recruitment in patients with clinical lumbar instability was changed to adapt to underlying spinal instability resulting from osteoligamentous laxity or damage.1,5,8 There are two main types of trunk muscles: deep and superficial. Internal oblique (IO), transversus abdominis (TrA), and lumbar multifidus (LM) are deep trunk muscles; whereas external oblique (EO), rectus abdominis (RA), and erector spinae (ES) are superficial trunk muscles.1,5 It is considered that the role of the deep trunk muscles is to provide a stiffening effect on the lumbar spine through its attachment to the thoracolumbar fascia, in conjunction with an increase in intra-abdominal pressure, and eventually this could result in spinal stability in patients with clinical lumbar instability.6,9–11
In addition to pain and functional disability, patient satisfaction12 and health-related quality of life (HRQOL)13 have gained interest recently in treatment evaluation of LBP. None of the previous studies have reported the effect of CSE on patient satisfaction and HRQOL in patients with clinical lumbar instability, and there is no information on detraining effects on improved sensitivity of pain after exercise treatment. Therefore, the aim of this study was to investigate the effect of 10 week CSE training and 3 month follow-up on pain during instability catch sign (ICS), functional disability, patient satisfaction, and HRQOL in patients with clinical lumbar instability.
Materials and methods
Study design
The study was a randomized assessor-blind controlled trial with four measurement points, including baseline, at the tenth week, and 1 and 3 months after stopping the exercise program (follow-up). It was conducted in the Physical Therapy Laboratory at Khon Kaen University, Thailand. This study was approved by the Ethics Committee for Human Research at Khon Kaen University, based on the Declaration of Helsinki.
Participants
Patients aged 20–60 years who had had LBP for 3 months or longer were recruited from the Orthopaedic Outpatient Department, the Physical Medicine and Rehabilitation Outpatient Department, and the Physical Therapy Department of Srinagarind Hospital, Khon Kaen Province, Thailand. They underwent a history-taking interview and a physical examination by an orthopedic surgeon who was unaware of the treatment procedure. Anteroposterior, lateral, and flexion-extension radiographs were used to exclude other spinal conditions. An ICS was performed to confirm the diagnosis of clinical lumbar stability. A positive ICS was defined as a sudden painful snap when a patient extends his/her back from the trunk forward-bending position into the upright position.3,4 To be eligible, patients must have a pain intensity of at least 5 out of 10, based on a numeric rating scale during ICS, and have a positive sign in one of the following provocation tests: painful catch, apprehension sign, or prone instability test. Eligible participants gave their written informed consent before their participation. They were excluded if they had other spinal pathology that might interfere with the study protocol,2 were pregnant, and/or regularly performed CSE or trunk stretching exercises.
Sample size determination
The sample size, using a formula of repeated measures analysis of variance, was estimated on the basis of pain during ICS, using a numerical rating scale at 3-month follow-up and assuming 90% power, 5% of significance, and 15% of attrition rate. To detect a clinically meaningful difference between groups of two scores on a numerical rating scale,14 a total sample size of 42 was required.
Exercise intervention
Eligible participants were enrolled in the study and randomly assigned to one of the two groups: CSE and conventional group (CG) by a block randomization with block sizes of two, four, and six. Randomization results were concealed in sealed and opaque envelopes with consecutive numbering. Lasting approximately 20 minutes, all training sessions of both groups took place at the Physical Therapy Laboratory twice a week for 10 weeks. Exercises were demonstrated and supervised by a research assistant blinded to the outcome assessment.
CSE
Details of this exercise have been described in our previous study (see supplementary material).10 The 10-week exercise program was divided into three phases. The first phase, weeks 1 and 2, focused on correctly isolating low-load activation of the TrA and LM muscles, using an ADIM technique in prone lying and sitting. Then, coactivation of TrA and LM were taught. A pressure biofeedback device (Chattanooga Australia Pty Ltd, Brisbane, QLD, Australia) and electromyography biofeedback (MP100, BIOPAC Systems Inc., Goleta, CA, USA) were used to provide feedback and facilitate correct performance during training. The second phase, weeks 3–7, started as soon as individuals could accurately control the TrA and LM muscles. The exercises progressed to the application of low load to the muscles through controlled movements of the upper and lower extremities. The last phase, weeks 8–10, aimed to integrate this coactivation into functional tasks. The participants were trained to maintain coactivation of TrA and LM during walking and two chosen tasks previously known to aggravate pain. At the end of the tenth week, 47.62% of participants were at the third phase, 38.09% were at the second phase, and 14.29% remained at the first phase.
CG
This group performed active trunk stretching exercises, which are the standard treatment for LBP in Thailand.15 The exercises consisted of ten repetitions of an alternating single knee to chest; as well as a lateral trunk-bending in standing. Each exercise was to be held for 10 seconds. Immediately after the exercises, a hydrocollator (60°C) (Enraf-Nonius Medical Equipment Company Ltd., Bangkok, Thailand), was placed over the lumbar area in the supine position for 15 minutes.
Both groups were required to practice the demonstrated exercises at home on a daily basis. To monitor their compliance, they were asked to record this in their logbook. In addition, every week, the same physical therapist made a phone call to participants in both groups to motivate them to continue their home exercises. After 10 weeks of training, all participants were asked to completely stop their exercise.
Measurements
Primary outcome
Primary outcome of this study was pain during ICS assessed by the 11-point numeric rating scale (range, 0–10), where 0 represents no pain and 10 represents the worst pain.16 Participants were asked to mark the line to indicate their level of pain.
Secondary outcomes
Secondary outcome measures included functional disability, patient satisfaction, HRQOL, and activation ratio of trunk muscles. Functional disability was evaluated using the Thai version of the Roland-Morris Disability Questionnaire (RMDQ).17 This 24-item questionnaire assesses physical disability specific to LBP. The participants were asked whether any statements characterized them on evaluation day. The total score is calculated by adding up the number of items answered with a “yes,” which ranges from 0 (no disability) to 24 (maximum disability). The internal consistency reliability of Thai RMDQ ranges from 0.71 to 0.93.18 It is also reproducible and sensitive to change over time for patients with LBP.
Patient satisfaction with treatment outcome was measured by the 11-point scale of Global Perceived Effect. It ranges from −5 (vastly worse) through 0 (no change) to +5 (completely recovered).12 The HRQOL was measured with the Thai version of the Medical Outcomes Study 36-item short-form Health Survey version 2.0 (SF-36V2).17 The Thai SF-36V2 measures eight quality-of-life domains collapsed into two summary scales: physical component summary (PCS), which consists of physical functioning, role physical, bodily pain, and general health, and mental component summary (MCS), which consists of vitality, social functioning, role emotion, and mental health. The internal consistency reliability of the Thai SF-36V2 was high in patients with LBP (Cronbach’s alpha of the PCS, 0.93; MCS, 0.92; range, 0.72–0.93 for eight domains).17 The correlation coefficients were higher between scales with similar constructs than for those with competing construct. The interscale correlation coefficients ranged from 0.21 to 0.51, with the correlation coefficient of the vitality and mental health being 0.71.18
Trunk muscle activities were measured by surface electromyography (sEMG). After light skin abrasion and alcohol cleansing, four pairs of electrodes were placed over the right side of four trunk muscles: TrA and IO, RA, LM, and iliocostalis lumborum pars thoracis (ICLT). Details of electrode placement were consistent with a previous study.10 The ground electrodes of the right RA and ICLT muscles were placed over the ribcage, and the other two ground electrodes of the right TrA and IO and LM muscles were placed over the right iliac crest. The EMG signals were sampled at 1,000 Hz with gain of 1,000, 10–500-Hz bandwidth, and a 110-dB common mode rejection ratio. The task, ADIM with 10-second hold, was performed three times with a 1 minute rest between trials. Normalization of abdominal and back muscle activities was done by using submaximal voluntary isometric contractions. For the abdominal muscles, participants raised both feet 1 cm from the floor in a crook lying position with a 5 second hold. For the back muscles, participants performed a double knee raise 5 cm from the floor in prone lying position with 5 second hold. The root mean square values of EMG signals produced during an isometric hold of these activities were then used to normalize the sEMG signals obtained during the ADIM. The activation ratio of the abdominal (TrA and IO/RA) and back (LM/ICLT) muscles were then calculated, using the normalized data.
Statistical analyses
Data are presented as means, standard deviations, and 95% confidence interval. All analyses were performed on the basis of intention-to-treat with the last observation carried forward. SPSS version 11.0 (IBM Corporation, Armonk, NY, USA) was used for data analysis. All data were normally distributed and were tested by the Shapiro–Wilk test. A 2 × 4 (group × time) repeated measures analysis of variance was applied for each variable. Post hoc analysis for pairwise comparison followed when a significant main effect was found. The level of significance was set at P<0.05.
Results
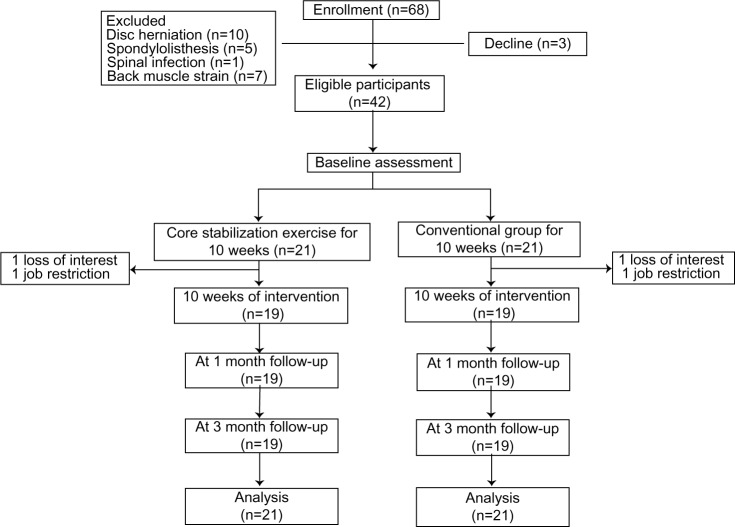
Sixty-eight patients responded to the recruitment advertisements, and after the screening test, 42 eligible participants entered the study. The reasons for exclusion were LBP with other spinal conditions such as disk herniation, spondylolisthesis, spinal infection, and back muscle strain. There were three patients who declined before the study began. Of the 42 participants, 21 were randomly assigned to the CSE group and 21 to the CG group. Figure 1 demonstrates progress through this study. Although the loss to follow-up was two participants for each group at 10 weeks of intervention, it was within the 15% attrition rate. The reasons for loss to follow-up were loss of interest about intervention or job restrictions.
Figure 1.
Flow of participants through the study.
The baseline characteristics of CSE and the CG are shown in Table 1. All characteristics and baseline outcomes were equally balanced between the groups.
Table 1.
Baseline characteristics of the participants
| Characteristics | Core stabilization exercise group (n=21) | Conventional group (n=21) | P-value |
|---|---|---|---|
| Age (years), mean (SD) | 44.73±9.21 | 44.93±7.86 | 0.87 |
| Sex, n (% female) | 17 (80.95) | 17 (80.95) | 1.00 |
| Height (cm), mean (SD) | 160.33±11.17 | 159.40±5.23 | 0.71 |
| Weight (kg), mean (SD) | 57.67±10.76 | 58.77±6.09 | 0.78 |
| Body mass index (kg/m2), mean (SD) | 22.44±2.67 | 23.23±4.9 | 0.65 |
| Low back pain duration (month), mean (SD) | 46.70±47.70 | 44.80±45.50 | 0.52 |
Abbreviation: SD; standard deviation.
Pain intensity during instability catch sign
A group × time interaction effect on pain during ICS was revealed (F(3,120)=17.23; P<0.001). The CSE group provided significantly greater reduction in pain intensity during ICS than the CG at 10 weeks and throughout the 3 month follow-up periods (Table 2). Pairwise comparisons illustrated that the CSE group showed a significant reduction in pain intensity during ICS from baseline to each follow-up period. However, the conventional group revealed only significant reduction in pain intensity during ICS from baseline to 10 weeks.
Table 2.
Comparison between core stabilization exercise (n=21) and conventional group (n=21) on pain intensity during instability catch sign, functional disability, patient satisfaction, and health-related quality of life
| Variables | Core stabilization exercise, mean (SD) | Conventional group, mean (SD) | Core stabilization exercise versus mean ± SD (95%CI) |
|---|---|---|---|
| Pain intensity during instability catch sign (scores) | |||
| Baseline | 6.29 (1.34) | 6.29 (1.27) | ns |
| 10 weeks of intervention | 2.00 (1.64) | 5.05 (1.52) | 3.05±0.50 (2.04 to 4.06)b |
| 1-month follow-up | 2.43 (1.36) | 5.71 (1.27) | 3.29±0.41 (2.46 to 4.11)b |
| 3-month follow-up | 2.95 (1.16) | 5.81 (1.12) | 2.86±0.53 (1.79 to 3.93)b |
| Roland-Morris Disability Questionnaire (scores) | |||
| Baseline | 7.95 (3.50) | 8.23 (3.11) | ns |
| 10 weeks of intervention | 2.81 (2.42) | 7.71 (2.71) | 4.90±1.00 (2.88 to 6.93)b |
| 1-month follow-up | 3.29 (2.65) | 8.29 (2.81) | 5.00±0.84 (3.30 to 6.70)b |
| 3-month follow-up | 3.67 (2.42) | 6.43 (4.27) | 2.76±1.07 (0.60 to 4.93)a |
| Patient satisfaction (scores) | |||
| Baseline | 0 | 0 | ns |
| 10 weeks of intervention | 3.38 (1.50) | 2.24 (1.26) | 1.14±0.43 (0.28 to 2.01)a |
| 1-month follow-up | 3.14 (1.39) | 1.29 (0.96) | 1.86±0.37 (1.11to 2.60)b |
| 3-month follow-up | 2.81 (1.33) | 1.14 (1.12) | 1.67±0.38 (0.89 to 2.44)b |
| Physical component summary of SF-36V2 (scores) | |||
| Baseline | 36.92 (7.61) | 37.00 (4.84) | ns |
| 10 weeks of intervention | 47.22 (10.08) | 38.27 (7.55) | 8.95±2.75 (3.39 to 14.50)a |
| 1-month follow-up | 47.23 (9.58) | 38.83 (8.36) | 8.40±2.78 (2.79 to 14.01)a |
| 3-month follow-up | 44.70 (10.10) | 36.70 (7.84) | 7.99±2.79 (2.35 to 13.63)a |
| Mental component summary of SF-36V2 (scores) | |||
| Baseline | 43.98 (7.97) | 43.70 (7.11) | ns |
| 10 weeks of intervention | 51.87 (7.25) | 50.83 (5.80) | ns |
| 1-month follow-up | 51.10 (6.95) | 48.62 (7.65) | ns |
| 3-month follow-up | 49.94 (8.08) | 48.30 (6.24) | ns |
Notes:
P<0.01;
P<0.001.
Abbreviations: SF-36V2, short-form Health Survey version 2.0; CI, confidence interval; ns, nonsignificant; SD, standard deviation.
Functional disability
A significant group × time interaction effect on functional disability was detected (F(3,120)=8.42; P<0.001). Pairwise comparisons revealed that CSE provided significantly greater decreased functional disability than the CG at 10 weeks and through the 3 month follow-up periods (Table 2).
Functional disability was significantly decreased after intervention in the CSE group (F(3,60)=33.44; P<0.001); however, the CG showed no significant changes from baseline to each follow-up period (F(3,60)=1.79; P=0.159). Pairwise comparisons revealed that the CSE showed a significant decrease in functional disability during follow-up periods when compared with the baseline.
Patient satisfaction
A significant group × time interaction effect on patient satisfaction was observed (F(3,120)=10.95; P<0.001). The CSE group showed a significantly greater increase in patient satisfaction than the CG at 10 weeks and through the 3-month follow-up periods (Table 2).
Patient satisfaction was significantly increased after the intervention period in the CSE group (F(3,60)=70.71; P<0.001) and the CG (F(3,60)=29.44; P<0.001). Pairwise comparisons revealed that the CSE group showed a significant increase in patient satisfaction through follow-up periods when compared with the baseline. Similarly, the CG also showed a significant increase in patient satisfaction during follow-up periods.
Health-related quality of life
The CSE group showed significantly greater improvement in PCS than the CG at 10 weeks and through 3-month follow-up periods (Table 2). Quality of life was significantly improved after the intervention period in the CSE group (F(3,60)=27.56; P<0.001 for PCS and F(3,60)=9.26; P<0.001 for MCS), whereas the CG showed a significant difference in MCS only (F(3,60)=6.11; P=0.001). The CSE group showed a significant increase in PCS and MCS through follow-up periods when compared with baseline, whereas the CG showed a significantly increased MCS at 10 weeks of intervention only.
Trunk muscle recruitment patterns
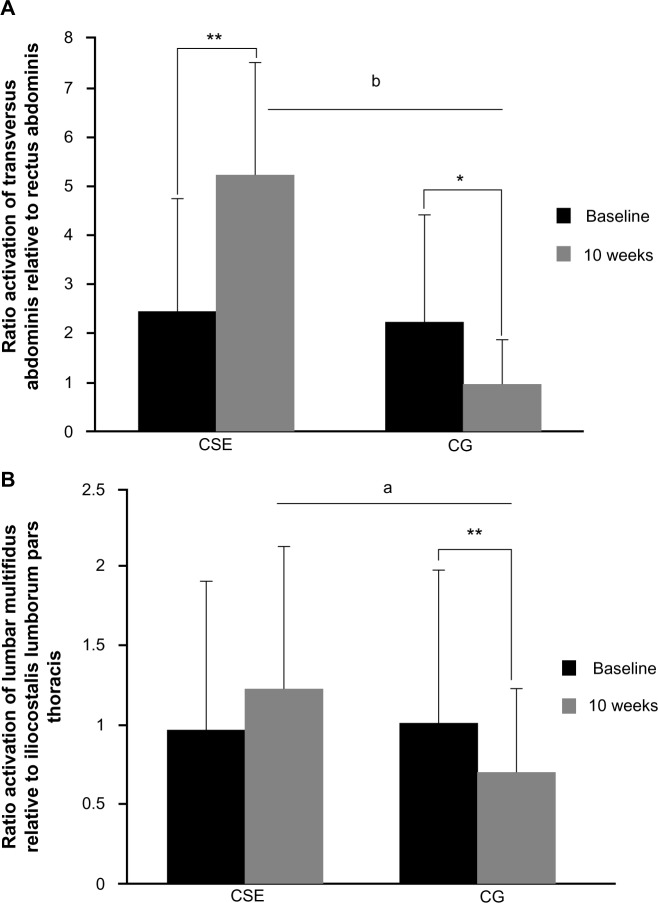
The CSE group provided significant improvement in the TrA and IO/RA ratio when compared with the CG (Table 2). A significant improvement in the TrA and IO/RA ratio was found after 10 weeks of CSE, whereas the CG showed significant reduction in this ratio activation compared with the baseline value (Figure 2A). The CG showed significant deterioration of the LM/ICLT ratio when compared with CSE (Table 2). There was no significant improvement in LM/ICLT ratio after 10 weeks of CSE (P=0.297). However, the CG revealed significant reduction in this activation ratio compared with the baseline value (Figure 2B).
Figure 2.
Ratio activation of transversus abdominis and internal oblique relative to rectus abdominis muscles (A) and ratio activation of lumbar multifidus relative to iliocostalis lumborum pars thoracis muscle (B) before and after intervention of core stabilization exercise (CSE) (n=21) and conventional group (CG) (n=21).
Notes: *P<0.05 for difference between baseline and each follow-up value; **P<0.01 for difference between baseline and each follow-up value; aP<0.05 for difference in post value between groups; bP<0.001 for difference in post value between groups.
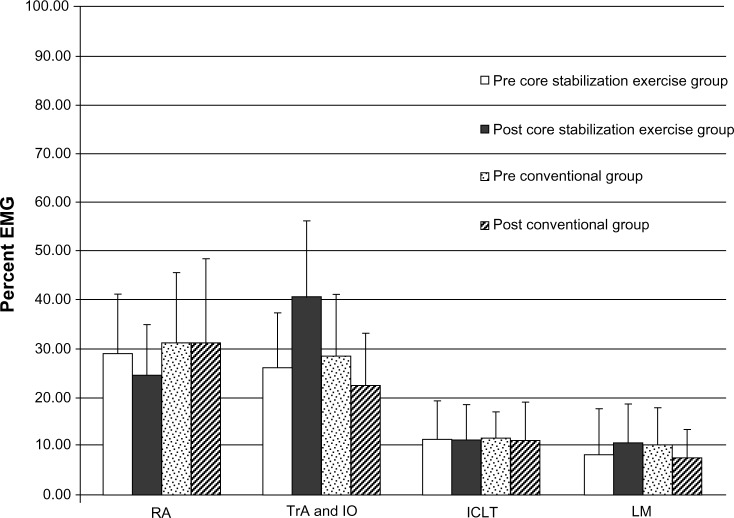
Interestingly, when we looked at the normalized muscle activation level in each muscle, we found that after the 10-week CSE, the normalized muscle activation levels of the deep muscles (TrA and LM) were greater than those measured at baseline. In contrast, the normalized muscle activation level in superficial muscles (RA and ICLT) was more deteriorated than those measured at baseline (Figure 3).
Figure 3.
Mean and standard deviation of the normalized muscle activation level in the pre- and post-core stabilization exercise (n=21) and the pre- and post conventional group (n=21).
Abbreviations: EMG, electromyography; RA, rectus abdominis; TrA, transversus abdominis; IO, internal oblique; ICLT, iliocostalis lumborum pars thoracis; LM, lumbar multifidus.
Discussion
This randomized controlled trial investigated the effects of a 10-week CSE training and 3-month follow-up on pain during ICS, functional disability, patient satisfaction and HRQOL in patients with clinical lumbar instability. The major finding was that all outcomes of the CSE group not only improved significantly after 10 weeks of training but also continued to have an effect after ceasing the exercise for 3 months.
The findings supported the hypothesis related to trunk muscle recruitment pattern in patients with clinical lumbar instability. After 10 weeks of CSE training, the activation ratio of the abdominal muscles (TrA and IO/RA) was significantly increased, with higher activation of TrA and IO muscles. Although the activation ratio of the back muscles (LM/ICLT) did not differ significantly from its baseline, it also had a tendency to increase. Gardner-Morse and Stokes19 propose that the deep abdominal muscles play a more important role than superficial abdominal muscles in providing spinal stability. Despite their short moment arms, the deep abdominal muscles are tonic muscles functioning as stabilizers of lumbar segments, whereas the superficial abdominal muscles are tonic muscles generating movements and providing overall stability. In addition, the authors further stated that at least 10% of spinal segmental stiffness caused by poor neuromuscular control and altered abdominal recruitment could lead to abnormal spinal movement.20 Therefore, the plausible explanation for diminution of pain during ICS and functional disability was that the CSE helps promote the changes in activation ratio of the abdominal and back muscles,9,10,14 leading to a direct potential stabilization of the lumbar spine via generation of intra-abdominal pressure and increased thoracolumbar fascial tension.10,14,16,21 It is likely that after 10-week training, the trunk muscle activation pattern in the participants in the CSE group has become automatically generated. The results are in agreement with the work of Javadian et al,3 who reported that despite stopping CSE for 3 months, the pain intensity and functional disability of patients with LBP remained the same.
At baseline, participants in both groups had an average of 12 items on the RMDQ of a possible 24, indicating a high level of disability. Immediately at the end of the training, the CSE group had improved, on average, by 5.14 points on the RMDQ scale, whereas the RMDQ of the CG group remained largely unchanged, reflecting the chronic nature of this condition. The improvement continued through 3 months after stopping the exercise.
These improvements in functional ability in the treatment group were in parallel with significant increases in patient satisfaction and HRQOL. Both groups were very similar at baseline, with no significant differences between the group means. The CSE group showed a significant increase in the PCS of HRQOL at 10 weeks, as well as 3 months afterward. The CG, in contrast, exhibited reduced or unchanged scores.
Even though the main finding of this study suggested that CSE was superior to the conventional treatment for treating patients with clinical lumbar instability, the interpretation of the results should be done with caution because of a limitation of sEMG. The EMG signals may be interfered with by crosstalk from other superficial muscles, especially for the LM muscles. Further studies should use indwelling EMG signals to accurately measure individual muscle activation.
Conclusion
This study has demonstrated that 10 week CSE provides 3 month retention effects on pain intensity during ICS, functional disability, patient satisfaction, and HRQOL in patients with clinical lumbar instability. Ratio of abdominal muscle activation has changed significantly after core stabilization training. Deep trunk muscles appeared to activate more than superficial trunk muscles in the exercise group compared with the CG. Improved trunk muscle recruitment pattern, hence, could be an efficient means to achieve trunk stability, reduce pain and disability, and improve quality of life in patients with clinical lumbar instability.
Supplementary material
Core stabilization exercise
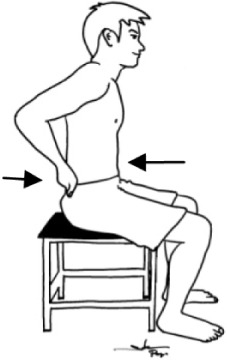
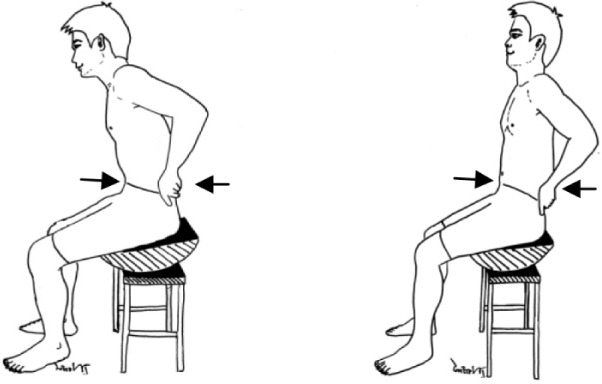
Instruction: This document demonstrates the use of core stabilization exercise and consists of illustrations of each exercise over the course of 10 weeks. Arrows indicate a specific trunk muscle activation is required in that exercise. Intensity of exercise is based on your exercise performance. Each session of exercise is done for 20 minutes per session, two sessions per week, and daily home exercises should be done following the instructions of this document.
| Week | Core stabilization exercise |
|---|---|
| Isolated transversus abdominis and lumbar multifidus training | |
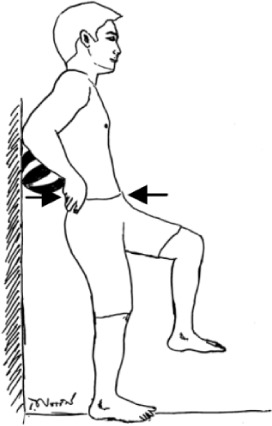
| 1 | Train transversus abdominis muscle activation in a prone lying position without spinal and pelvic movements for 10 seconds with ten repetitions. Keep respiration normal. You gently draw in the lower anterior abdominal wall below the navel level (abdominal drawing-in maneuver) with supplemented contraction of pelvic floor muscles, control your breathing normally, and have no movement of the spine and pelvis while lying prone on a couch with a small pillow placed beneath your ankles. |
| |
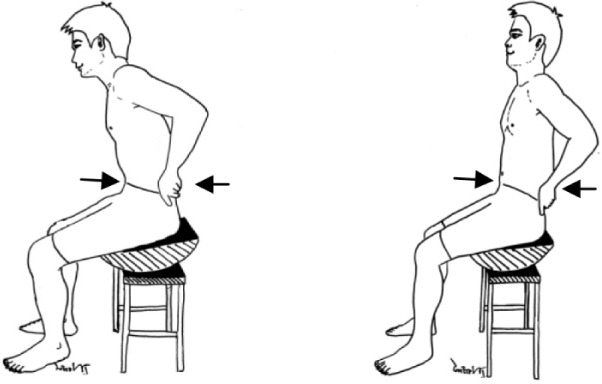
| Train lumbar multifidus muscle activation in an upright sitting position. You raise the contralateral arm while performing the abdominal drawing-in maneuver in a sitting position on a chair. | |
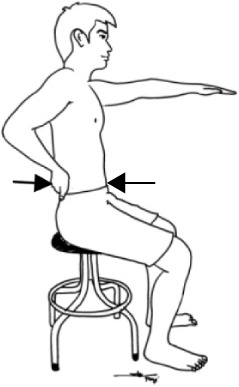
| |
| Integrated transversus abdominis and lumbar multifidus training light activities | |
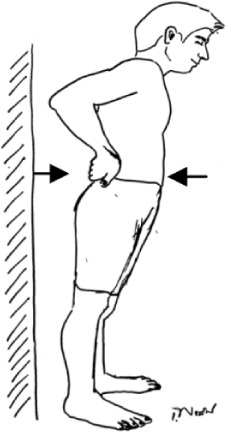
| 2 | Perform cocontraction of transversus abdominis and lumbar multifidus muscles while sitting on a chair. You use the index and middle fingers to palpate contraction of transversus abdominis muscle and the opposite two fingers to palpate contraction of lumbar multifidus muscle. This exercise progresses from 10- to 60-second holds of cocontraction for ten repetitions. |
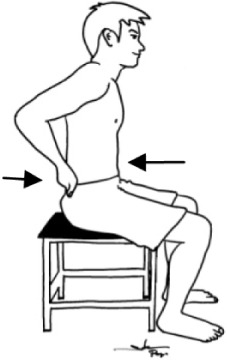
| |
| Train cocontraction of these muscles with trunk forward and backward while sitting on a chair and keeping your lumbar spine and pelvis in a neutral position. The second exercise this week required 10-second holds with ten repetitions. | |

| |
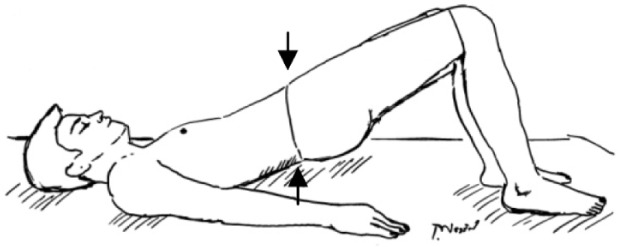
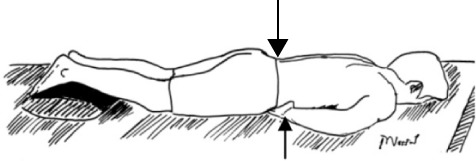
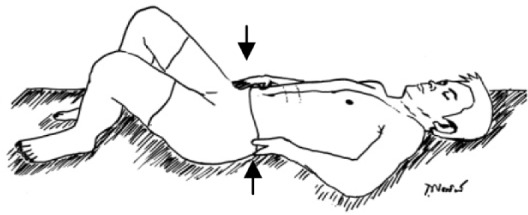
| 3 | Perform cocontraction of the two muscles in a crooked lying position with both hips at 45 degrees and both knees at 90 degrees. Then you abduct one leg to 45 degrees of hip abduction and hold it for 10 seconds. |
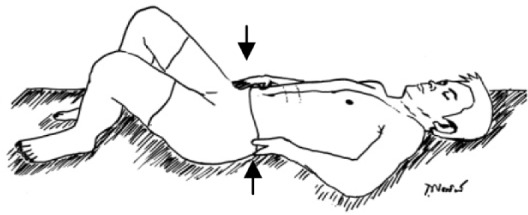
| |
| Train cocontraction of these muscles in a crooked lying position with both hips at 45 degrees and both knees at 90 degrees. Then you slide a single leg down until the knee is straight, maintain it for 10-second holds and then slide it back up to the starting position. | |
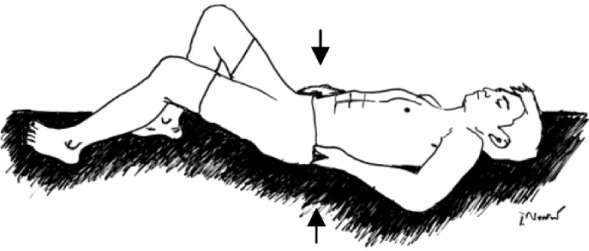
| |
| 4 | Perform cocontraction of the two muscles while sitting on a balance board. You perform cocontraction of the muscles with trunk forward, backward, and sideways while sitting on a balance board and keeping your lumbar spine and pelvis in a neutral position. You perform each pose for 10-second holds with ten repetitions. |
| |
| Integrated transversus abdominis and lumbar multifidus training heavier activities | |
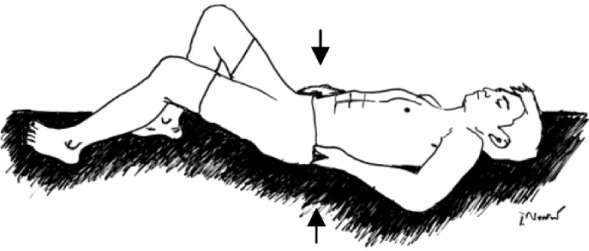
| 5 | Perform cocontraction of the two muscles while raising the buttocks off a couch from a crooked lying position until your shoulders, hips, and knees are straight. You sustain this pose for 10 seconds and then lower the buttocks back down to the couch with ten repetitions. |
| |
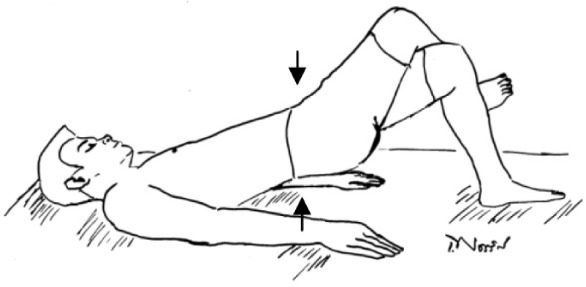
| Train muscle cocontraction while raising the buttocks off a couch from a crooked lying position with one leg crossed over the supporting leg. You raise the buttocks off the couch until the shoulders, hips, and knees are straight. You sustain this pose for 10 seconds and then lower the buttocks back down to the couch with ten repetitions. | |
| |
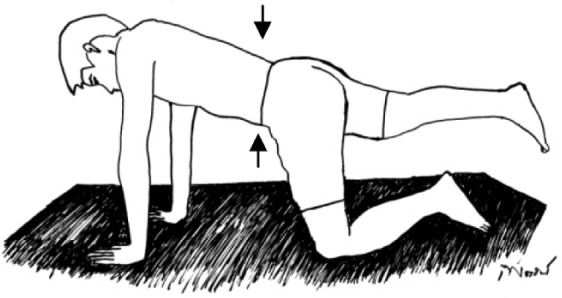
| 6 | Perform cocontraction of the two muscles while raising a single leg from a four-point kneeling position and keeping your back in a neutral position. You sustain this pose for 10 seconds and then return the leg to the starting position with ten repetitions. |
| |
| Train muscle cocontraction while raising an arm and alternate leg from a four-point kneeling position and keeping your back in a neutral position. You sustain this pose for 10 seconds and then return to the starting position with ten repetitions. | |

| |
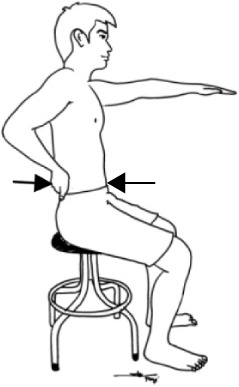
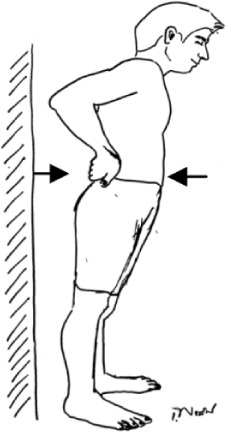
| 7 | Perform cocontraction of the two muscles in a standing position while a mini ball is behind your upper back and against the wall. You flex the hip and knee of one leg to 90 degrees. Sustain this pose for 10 seconds and then return to the starting position with ten repetitions. |
| |
| Train the muscle cocontraction in a standing position with ankle movement. Perform ankle movement in the forward-backward direction while keeping your lumbar spine in a neutral position. Sustain this pose for 10 seconds and then return to the starting position with ten repetitions. | |
| |
| Integrated transversus abdominis and lumbar multifidus training in pain aggravating activities | |
| 8–10 | Perform muscle cocontraction while walking at normal, faster and fastest speed for 5 minutes at weeks 8, 9, and 10 respectively. In addition, choose two aggravating activities or tasks that you anticipate would cause pain or instability and perform muscle cocontraction while doing these activities or tasks without having pain. Each aggravating activity or task is performed for 2.5 minutes. |

| |
Acknowledgments
The authors thank the study participants. This study was supported by grants from the Graduate School (GS 54112101) and the Back, Neck and Other Joint Pain Research Group, Khon Kaen University, Thailand. The authors are also grateful to Ian Thomas, Faculty of Science, Khon Kaen University, Thailand, for English proofreading of this article.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Silfies SP, Squillante D, Maurer P, Westcott S, Karduna AR. Trunk muscle recruitment patterns in specific chronic low back pain populations. Clin Biomech (Bristol, Avon) 2005;20(5):465–473. doi: 10.1016/j.clinbiomech.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 2.White AA, Panjabi MM. Clinical Biomechanics of the Spine. Philadelphia, PA: Lippincott-Raven; 1990. [Google Scholar]
- 3.Javadian Y, Behtash H, Akbari M, Taghipour-Darzi M, Zekavat H. The effects of stabilizing exercises on pain and disability of patients with lumbar segmental instability. J Back Musculoskelet Rehabil. 2012;25(3):149–155. doi: 10.3233/BMR-2012-0321. [DOI] [PubMed] [Google Scholar]
- 4.Kotilainen E, Valtonen S. Clinical instability of the lumbar spine after microdiscectomy. Acta Neurochir (Wien) 1993;125(1–4):120–126. doi: 10.1007/BF01401838. [DOI] [PubMed] [Google Scholar]
- 5.Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5(4):383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 6.O’Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine (Phila Pa 1976) 1997;22(24):2959–2967. doi: 10.1097/00007632-199712150-00020. [DOI] [PubMed] [Google Scholar]
- 7.Cresswell AG, Oddsson L, Thorstensson A. The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure while standing. Exp Brain Res. 1994;98(2):336–341. doi: 10.1007/BF00228421. [DOI] [PubMed] [Google Scholar]
- 8.Hodges PW, Cresswell AG, Daggfeldt K, Thorstensson A. In vivo measurement of the effect of intra-abdominal pressure on the human spine. J Biomech. 2001;34(3):347–353. doi: 10.1016/s0021-9290(00)00206-2. [DOI] [PubMed] [Google Scholar]
- 9.Barker PJ, Guggenheimer KT, Grkovic I, et al. Effects of tensioning the lumbar fasciae on segmental stiffness during flexion and extension: Young Investigator Award winner. Spine (Phila Pa 1976) 2006;31(4):397–405. doi: 10.1097/01.brs.0000195869.18844.56. [DOI] [PubMed] [Google Scholar]
- 10.Areeudomwong P, Puntumetakul R, Jirarattanaphochai K, et al. Core stabilization exercise improves pain intensity, functional disability and trunk muscle activity of patients with clinical lumbar instability: a pilot randomized controlled study. J Phys Ther Sci. 2012;24:1007–1012. [Google Scholar]
- 11.Bjerkefors A, Ekblom MM, Josefsson K, Thorstensson A. Deep and superficial abdominal muscle activation during trunk stabilization exercises with and without instruction to hollow. Man Ther. 2010;15(5):502–507. doi: 10.1016/j.math.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Kamper SJ, Maher CG, Herbert RD, Hancock MJ, Hush JM, Smeets RJ. How little pain and disability do patients with low back pain have to experience to feel that they have recovered? Eur Spine J. 2010;19(9):1495–1501. doi: 10.1007/s00586-010-1366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jirarattanaphochai K, Jung S, Sumananont C, Saengnipanthkul S. Reliability of the medical outcomes study short-form survey version 2.0 (Thai version) for the evaluation of low back pain patients. J Med Assoc Thai. 2005;88(10):1355–1361. [PubMed] [Google Scholar]
- 14.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976) 2008;33(1):90–94. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 15.Pensri P, Foster NE, Srisuk S, Baxter GD, McDonough SM. Physiotherapy management of low back pain in Thailand: a study of practice. Physiother Res Int. 2005;10(4):201–212. doi: 10.1002/pri.16. [DOI] [PubMed] [Google Scholar]
- 16.Mannion AF, Balagué F, Pellisé F, Cedraschi C. Pain measurement in patients with low back pain. Nat Clin Pract Rheumatol. 2007;3(11):610–618. doi: 10.1038/ncprheum0646. [DOI] [PubMed] [Google Scholar]
- 17.Jirarattanaphochai K, Jung S, Sumananont C, Saengnipanthkul S. Reliability of the Roland – Morris Disability Questionnaire (Thai version) for the evaluation of low back pain patients. J Med Assoc Thai. 2005;88(3):407–411. [PubMed] [Google Scholar]
- 18.Lim LL, Seubsman SA, Sleigh A. Thai SF-36 health survey: tests of data quality, scaling assumptions, reliability and validity in healthy men and women. Health Qual Life Outcomes. 2008;6:52. doi: 10.1186/1477-7525-6-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gardner-Morse MG, Stokes IA. Trunk stiffness increases with steady-state effort. J Biomech. 2001;34(4):457–463. doi: 10.1016/s0021-9290(00)00226-8. [DOI] [PubMed] [Google Scholar]
- 20.Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003;84(12):1858–1864. doi: 10.1016/s0003-9993(03)00365-4. [DOI] [PubMed] [Google Scholar]
- 21.Goldby LJ, Moore AP, Doust J, Trew ME. A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine (Phila Pa 1976) 2006;31(10):1083–1093. doi: 10.1097/01.brs.0000216464.37504.64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
| Week | Core stabilization exercise |
|---|---|
| Isolated transversus abdominis and lumbar multifidus training | |
| 1 | Train transversus abdominis muscle activation in a prone lying position without spinal and pelvic movements for 10 seconds with ten repetitions. Keep respiration normal. You gently draw in the lower anterior abdominal wall below the navel level (abdominal drawing-in maneuver) with supplemented contraction of pelvic floor muscles, control your breathing normally, and have no movement of the spine and pelvis while lying prone on a couch with a small pillow placed beneath your ankles. |
| |
| Train lumbar multifidus muscle activation in an upright sitting position. You raise the contralateral arm while performing the abdominal drawing-in maneuver in a sitting position on a chair. | |
| |
| Integrated transversus abdominis and lumbar multifidus training light activities | |
| 2 | Perform cocontraction of transversus abdominis and lumbar multifidus muscles while sitting on a chair. You use the index and middle fingers to palpate contraction of transversus abdominis muscle and the opposite two fingers to palpate contraction of lumbar multifidus muscle. This exercise progresses from 10- to 60-second holds of cocontraction for ten repetitions. |
| |
| Train cocontraction of these muscles with trunk forward and backward while sitting on a chair and keeping your lumbar spine and pelvis in a neutral position. The second exercise this week required 10-second holds with ten repetitions. | |

| |
| 3 | Perform cocontraction of the two muscles in a crooked lying position with both hips at 45 degrees and both knees at 90 degrees. Then you abduct one leg to 45 degrees of hip abduction and hold it for 10 seconds. |
| |
| Train cocontraction of these muscles in a crooked lying position with both hips at 45 degrees and both knees at 90 degrees. Then you slide a single leg down until the knee is straight, maintain it for 10-second holds and then slide it back up to the starting position. | |
| |
| 4 | Perform cocontraction of the two muscles while sitting on a balance board. You perform cocontraction of the muscles with trunk forward, backward, and sideways while sitting on a balance board and keeping your lumbar spine and pelvis in a neutral position. You perform each pose for 10-second holds with ten repetitions. |
| |
| Integrated transversus abdominis and lumbar multifidus training heavier activities | |
| 5 | Perform cocontraction of the two muscles while raising the buttocks off a couch from a crooked lying position until your shoulders, hips, and knees are straight. You sustain this pose for 10 seconds and then lower the buttocks back down to the couch with ten repetitions. |
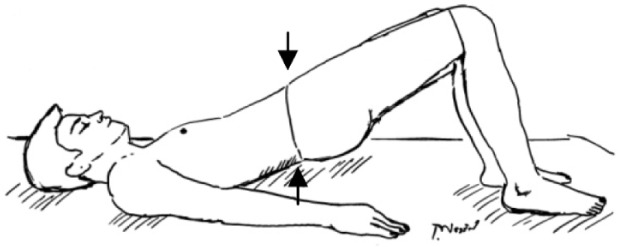
| |
| Train muscle cocontraction while raising the buttocks off a couch from a crooked lying position with one leg crossed over the supporting leg. You raise the buttocks off the couch until the shoulders, hips, and knees are straight. You sustain this pose for 10 seconds and then lower the buttocks back down to the couch with ten repetitions. | |
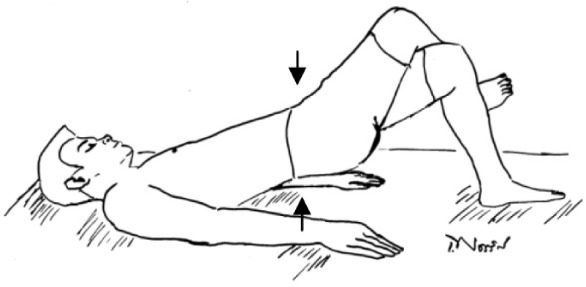
| |
| 6 | Perform cocontraction of the two muscles while raising a single leg from a four-point kneeling position and keeping your back in a neutral position. You sustain this pose for 10 seconds and then return the leg to the starting position with ten repetitions. |
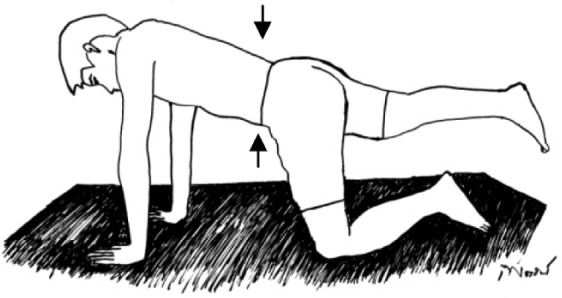
| |
| Train muscle cocontraction while raising an arm and alternate leg from a four-point kneeling position and keeping your back in a neutral position. You sustain this pose for 10 seconds and then return to the starting position with ten repetitions. | |

| |
| 7 | Perform cocontraction of the two muscles in a standing position while a mini ball is behind your upper back and against the wall. You flex the hip and knee of one leg to 90 degrees. Sustain this pose for 10 seconds and then return to the starting position with ten repetitions. |
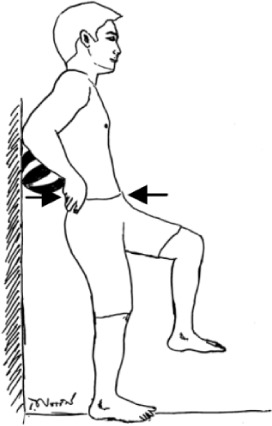
| |
| Train the muscle cocontraction in a standing position with ankle movement. Perform ankle movement in the forward-backward direction while keeping your lumbar spine in a neutral position. Sustain this pose for 10 seconds and then return to the starting position with ten repetitions. | |
| |
| Integrated transversus abdominis and lumbar multifidus training in pain aggravating activities | |
| 8–10 | Perform muscle cocontraction while walking at normal, faster and fastest speed for 5 minutes at weeks 8, 9, and 10 respectively. In addition, choose two aggravating activities or tasks that you anticipate would cause pain or instability and perform muscle cocontraction while doing these activities or tasks without having pain. Each aggravating activity or task is performed for 2.5 minutes. |

| |