Abstract
Long-term care use among older Mexican-Americans is poorly understood, despite the adverse effects on health and economic disadvantage in this vulnerable population. This study examines gender-based risk of long-term care use in 628 women and 391 men, age 70 and over in the 2000-01 and 2004-05 waves of the Hispanic Established Populations for Epidemiologic Studies of the Elderly. Logistic regression models are employed to assess the impact of the opportunity cost implications of family support (kin availability and co-residence) relative to health care needs (quality-adjusted life years (QALY) weighted scores and functional limitations) on women's risk of entry into a nursing home. A small percentage (∼5%) of men and women had entered a long-term care facility. Women had lower weights for QALY weights and greater disability than men, but on average were more likely to live with or in closer proximity to an adult child. Higher disability rates (p < .01) increased the risk of institutionalization regardless of gender because disability increases time burdens. Families with fewer adult children faced higher time burdens per child in caring for elderly parents; particularly for elderly mothers. Demographic trends suggest that the number of adult children available to share the caregiving load may decrease long-term care use.
Keywords: Mexican American, long-term care, caregiving, opportunity costs
Introduction
The impact of long-term care needs of older and disabled persons on health care costs have previously only garnered minimal attention or oversight in the nation's budget (Holtz-Eakin 2005). As baby boomers begin to enter retirement, the solvency of Medicare and the Social Security garners the majority of the attention in the media and among policy makers (Keehan et al. 2012). Elder care is more off-budget, and garners less attention. However, off-budget costs are still real, and come in the form of opportunity cost—the responsibility of caring for dependent elderly family members remains in the hands of family caregivers. The cost of caring for aging relatives may disproportionately impact low- to middle-income families the most, which makes Hispanics particularly vulnerable. According to the U.S. Census, Hispanics had a poverty rate of 26.6% in 2010, an increase from 2009 (McCartnery, Bishaw, & Fontenot 2013).
A host of factors have been shown to increase risk of entering costly nursing home care. Many of these factors could be considered within the context of a time cost model, but heretofore have not. In a meta-analysis of 77 studies, Gaugler, Duval, Anderson, and Kane (2007) found that nursing home use was strongest for persons with three or more Activities of Daily Living (ADLs), cognitive impairment, and prior nursing home use. For Mexican Americans specifically, the high costs of nursing homes (Abraido-Lanza et al. 2006; Kaye, LaPlante & Harrington 2009), and cultural preferences to care for aging relatives are powerful predictors of long-term care use (Gaugler et al. 2006; Herrera et al. 2008; Nguywn et al. 2003). Older age and widowhood can increase nursing home placement (Andel, Hyer, & Slack, 2007), and living alone can also increase the risk for falls, a predictor of long-term care (Elliott, Painter, & Hudson, 2009).
The fact that elder care is hidden ‘off-budget’ masks another looming crisis, one concerned with growing indirect costs borne by families rather than by the government or the network of long-term support service providers. These indirect costs on families may have long-term devastating effects. For families caring for their elderly parents at home, significant time is spent providing that level of care (Kane, Kane & Ladd 1998). The opportunity costs come in the form of compensation foregone due to reduced participation in the workforce, diminished savings, and careers not pursued. Indirect costs ultimately affect budgets at the state and federal level, as reduced incomes lower sales and income tax revenues. The cumulative effect of these financial sacrifices can become even more formidable, both for individuals and for society. For instance, excessive elder care burdens could limit the family's ability to pay for college educations.
The risk of institutionalization has not previously applied opportunity cost analysis to an economic perspective for older Mexican Americans or other Hispanic groups. Time considerations have a long history in economics. This perspective dates back to Gary Becker's theory of time allocation and opportunity costs (Becker 1965). Most recently, the concept of “time poverty” has been applied to obesity and diet (Kalenkoski & Hamrick 2012). The economic perspective for our analysis is viewed from the family, rather than state or federal governments. For instance, opportunity costs increase as the time needed to provide elder care increases (cooking, cleaning, financial management, transportation, and other activities of daily living). Furthermore, the opportunity costs of caring for an elderly parent at home are higher for those with higher wages, simply because the monetary value of their work hours is higher.
This study adds to the literature by examining the influence of time inputs of adult children associated with the risk for long-term care in their aging Mexican-American parents. Opportunity costs at the individual level typically the time of the activity, caregiving in this case, at individual's wage. But in this sample there is little variation in wages. Our purpose then, is to assess the way in which time commitment requirements (i.e., time to reach elderly parents by adult children, time inputs for care due to limitations in ADL, and whether these times can be shared by other adult child siblings) affect the use of nursing homes. We analyze longitudinal data from a unique sample of Mexican-origin individuals 65 and over residing in the United States to determine how time commitments, which are a proxy for opportunity cost in terms of career salaries and wages foregone, positively affect the likelihood of using nursing homes for elder care for both men and women.
We segment our model by gender for several reasons. Compared to men, women have a higher probability of nursing home admission and lifetime use of care (He et al. 2005). Also women comprise the vast majority (70 percent) of nursing home residents, primarily because they have higher life expectancy than men after age 65 (Houser 2007). In addition, women are more often on the receiving end of caretaking; 57% of care recipients are women, and the remaining 43% are men (O'Brien 2005). Because they live longer than men by at least five years; the risk of disability increases with aging and the subsequent need for assistance (Stone 2011). For this reason, the risk of nursing home care may differ by gender.
Background and Prior Research
Mexican Americans have traditionally low levels of utilization of institutional care (Angel et al. 2004). One factor is the direct cost; keeping elders at home and in the community is cheaper, even for families whom are dual eligible for Medicaid and Medicare (Abraido-Lanza et al. 2006; Kaye, LaPlante & Harrington 2009). Another factor, the cultural tradition of caring for aging relatives, has long been a powerful predictor of long-term care use – a value moderated by familism (Gaugler et al. 2006; Herrera et al. 2008; Nguywn et al. 2003; Sabogal et al. 1987). Mexican Americans exhibit a strong cultural preference to care for elderly family members within the home (Angel et al. 1996). However, over the last 10 years, rates of entry into nursing homes for Hispanics has risen by 54.9%, possibly suggesting that an increase in time inputs by family members are increasing their opportunity costs, as immigrants stand to lose more wages and as care burdens are concentrated on fewer siblings (Crystal & Shea 2003). The degree of elder-care responsibilities is likely to increase as the elderly Mexican American population grows old with disabling physical and cognitive problems (Langa et al. 2004). Among those with the financial means to care for family members at home, time constraints, caregiver stress, and fewer family members available to care for aging parents may explain this increase in nursing home use (Fennell et al. 2010). To date, no study has attempted to estimate the effect of opportunity costs (or time commitments) of caring for frail or older Mexican-American relatives, particularly among adult children, on institutionalization. Understanding this is crucially important, as the older Hispanic population is projected to increase dramatically over the next four decades. By 2050, Hispanics 65 and older are expected to reach 17.5 million, up from 2.9 million in 2010. Those 85 and over, the group at highest risk of dependency, are also projected to quickly climb, increasing nine-fold from 305,000 in 2010 to 2.9 million in 2050.
Opportunity Costs Framework
To illustrate the concept of opportunity costs, we present Equation 1, which shows hypothesized drivers of adult children's opportunity costs that must be negotiated when caring for elderly parents. Equation 1: Adult Child's Opportunity Costs = Wage x (Care Time per elder adult per period+ travel time per period) / [# of living adult children + Spouse].
The adult child's opportunity costs are valued in monetary terms, valued at the wage. In the numerator, the primary driving force is older Mexican Americans's care time determined by their functional independence and health. Care time is considered one of the strongest documented predictors of long-term care needs, where higher functional incapacity is directly correlated with greater care time inputs. Time inputs may involve assisting the older relative with cooking, cleaning, administration of medications, and other chores. In our model they are largely determined by difficulties in performing instrumental and daily activities of living as well as self-reported health. Although wages are not directly measured in this study, opportunity costs experienced by adult children are proportional to time spent for elder care. As noted earlier, opportunity costs represent the loss of foregone activities considered to have value to adult children. That is, when adult children are spending time caring for elderly parents, they are using that time for alternative purposes, such as direct and indirect loss of earnings from relinquishing second part-time jobs, overtime, advancement training, as well as intangible pursuits such as personal enrichment, or engagement in leisure activities. There are other intergenerational effects, such as reduced savings for college expenses.
Specific Hypotheses
The adult child's opportunity costs will increase as the care time needed by the elderly parent increases. Those opportunity costs are expected to vary by the availability and proximity of adult children, presence of a spouse, and other variables depicted in the denominator of Equation 1. First, we hypothesize that adult children's care time and opportunity costs may hypothetically be curtailed by the presence of other living siblings and spouse to elderly parent for several reasons. The presence of other active siblings and/or spouse would presumably lead to a distribution in the care chores. This also increases the probability that at least one adult child will step in and avail themselves as primary caregivers. Less time is thus afforded by any one sibling, thereby diminishing the opportunity costs borne by any one caregiver. Secondly, we hypothesize that opportunity costs are influenced by the transit time for that adult child to reach the elderly parent, as noted earlier. Traveling further distances to provide care to aging parents adds to adult children's opportunity costs, and may also introduce complexity to their caregiving role if scheduling becomes difficult. Alternatively, close proximity, including co-residence with the elderly parent, may lead to increased time spent providing care around the clock, or be interpreted by other siblings as a cue to lessen their own involvement in caregiving, and in turn only exacerbate the opportunity costs of the co-residing child.
Familial Network, Availability, and Cultural Factors
The majority (79%) of home care of older Mexican Americans is currently borne by family members, a proportion higher than any other racial/ethnic group (Otiniano, Snih & Goodwin 2012). Family caregivers spend significant amounts of time caring for elderly parents at home, particularly when they are afflicted with dementia or diabetes conditions that disproportionately affect older Latinos (Novak & Riggs 2004; Wen, Shepherd & Parchman 2004). For example, diabetes is estimated to affect approximately one-third of Mexican Americans age 75 and above (White-Means & Rubin 2004). Likewise, by the year 2050 the number of Latinos diagnosed with Alzheimer's disease and related dementias could increase more than 6 times, from the current figure of less than 200,000 patients to as many as 1.3 million (Novak & Riggs 2004).
Mexican Americans have a higher fertility rate than other ethnic groups (Durand, Telles & Flashman 2006). This may change in the future, as the U.S. birth rate for Mexican immigrants fell by 23% between 2007 and 2010 in response to the economic recession (Pew Hispanic Research Center 2011). However, historic fertility rates have led to a greater number of family members available to share in helping Hispanic aging parents. For instance, the total time input for helping aging parents may be the same, but may be shared among more siblings (Juster & Suzman 1995; Pinquart & Sörensen 2005). Geographic dispersion of families also increases the time required to help aging parents because of increased travel time to reach them when they need help. Mexican-American women, especially daughters, are the primary caregivers for elderly parents (Jolicoeur & Madden 2002). According to a 2008 study, approximately 74% of Hispanic caregivers are female, of these, 41% felt that they did not have a choice (Evercare and National Alliance for Caregiving 2008). Within Hispanic culture, the care of aging parents has been traditionally considered the responsibility of children, and this burden is strongly associated with female children (Sands et al. 2008). However, the pool of available female caregivers has been shrinking. The trend of women entering the workforce has shrunk the network of female family caregivers available for aging relatives, which increases the average load on siblings left to care for parents because professional women are less available (Reinhard et al., 2011). There is little evidence to document the extent to which available family support affects older adults' need for and access to both informal (family) and formal (institutional) caregiving systems (Angel & Angel 2009).
Financial Resources
One potentially important predictor of access to long-term care is Medicaid. In 2012, the average cost of nursing home care was $88,000 per year, about 241% of older adults' average annual income (Ujvari 2012). This expense puts long-term nursing home stays outside the reach of the vast majority of Americans without ample savings and generous private long-term care insurance (Assistant Secretary for Planning and Evaluation 2008; Bernstein 2012). For the eligible poor, Medicaid coverage is often viewed as a necessary but not sufficient condition to seek long-term care among disabled older adults (O'Brien 2005). Medicaid is the largest financial source for institutional and some community-based long-term care services. Approximately two-thirds of older adult nursing home residents rely on Medicaid to pay for their care (Stone 2011). About 26.6% of Hispanics live in poverty (McCartnery, Bishaw, & Fontenot, 2013); for older Hispanic women who live alone that number increases to 38.8 % (U.S. Census Bureau, 2012). Mexican Americans have less formal education and are less likely to work in high-salary jobs (Angel & Angel 2009). Thus, they are more impoverished, have few assets, and are likely to have no private, long-term care insurance in retirement. However, Mexican Americans are more likely than non-Hispanic whites to participate in the Medicaid program in later life (Angel & Angel 2009). Therefore, even though affordability remains an issue, the low prevalence rate of nursing home use may not entirely be due to affordability.
Despite the flourishing population of older Mexican Americans and alarming rates of disability (Markides et al. 2007), there remains scant research on the role of the kinship network structure in diffusing adult children's' time burden in caring for aging women. To that end, we examine gender differences in adult children's opportunity costs on older Mexican Americans' use of long-term nursing homes or assisted living facilities (as measured by the availability of and proximity of adult children, presence of a spouse, and care needs). We then estimate the likelihood of long-term care use as the opportunity costs of caring for elderly parents increase.
Study Sample
We employ data from the Hispanic Established Populations for Epidemiologic Study of the Elderly (H-EPESE). The H-EPESE is a large, multi-stage probability sample of older Mexican Americans who reside in five southwestern states: Texas, California, New Mexico, Arizona, and Colorado (Markides et al. 1997). The dataset includes information on mental and physical health, psychosocial characteristics, and health and long-term care use. Information from a knowledgeable proxy, such as a family member or caretaker, was obtained for individuals who were unable to complete the entire interview themselves because of infirmity or cognitive incapacity. Baseline data were completed in 1993-94 (wave 1), with follow-up interviews in 1995-96 (wave 2), 1998-99 (wave 3), 2000-01 (wave 4) and 2004-05 (wave 5). Our analysis draws on Mexican-American men (n = 391) and women (n = 628) over the age of 70 (N = 1,009) interviewed in 2000–01 (wave 4) and at the follow up in 2004-05 (wave 5). Subsample analysis of men and women from wave 4 and 5 were also analyzed to assess gender-specific differences. The response rates for the two waves were 81% and 74%, respectively. The share of proxy interviews in 2004 was 6.9% and at the follow-up, 8.3%. Respondents were offered the choice of conducting the interview in Spanish or English. Only complete responses on long-term care use were included in the final analyses. The selection for the final subsample for analysis is summarized in the flowchart in Figure 1.
Figure 1.
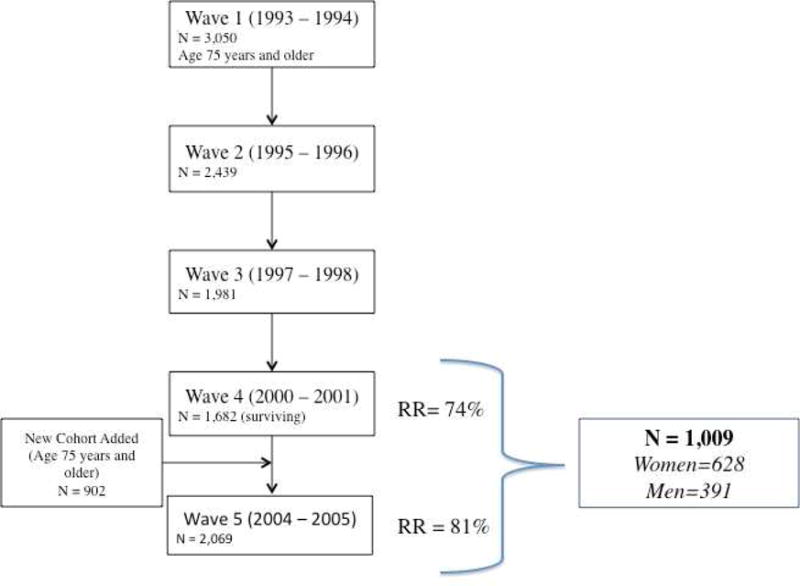
Flowchart describing the final sample used in the analysis for the present study, drawn from the Hispanic Established Populations for Epidemiologic Study of the Elderly (H-EFESE).
Methods
The variables for the analysis are nursing home and assisted living facility use (dependent variable). Time inputs consisted of 1) older adults' care needs (Quality Adjusted Life Years weighted by self-rated health, Instrumental Activities of Daily Living, Activities of Daily Living); 2) family support (number of adult children and presence of a spouse, presumed to share the time burdens of care); and 3) proximity defined by the transit time between children and elderly parent. Analyses were adjusted for demographic characteristics (e.g., age and health insurance).
Nursing home and assisted living facility use
Long-term care refers to institutional types of living arrangements. In wave 5 (2004–05), the H-EPESE interview inquired if respondents had entered a nursing home, skilled nursing facility, or assisted living facility after 2002, after the completion of wave 4 (2000-01). An affirmative response is coded “1” if it occurred after wave 4 (2000–01), and “0” otherwise. Short-term use of nursing homes, such as post hospitalization or rehabilitative care, was excluded from this definition. Following their first entry into a nursing home, participants were excluded in subsequent waves in the analyses. The final analytic sample reflects the total number of older adults who responded to a question on nursing homes in wave 5 (2004-05), and who were previously non-institutionalized. We then utilized subsamples of only women (N = 628) and only men (N = 391) to examine gender-specific nuances in the care of aging Mexican-Americans.
Care time
Care time was measured by older adults' need for assistance, as determined by 1) Quality-Adjusted Life-Years (QALY weights) (Murray 1994), 2) Activities of Daily Living (ADL) (Katz 1983) and 3) Instrumental Activities of Daily Living (I-ADL) (Lawton & Brody 1969). Each of these indicators of care time was modeled separately in the regression analyses.
QALY score weights are used as a proxy (summary) measure of quality of life, and a correlate of time inputs required from kin in the care of aging or disabled parents. QALY scores from wave 4 (2000-01) were used for this purpose, as this is the period when decisions about institutionalization in wave 5 (2004–05) are being considered. QALY weights were weighted by participants' response to a one-item self-rated health question (1 = excellent to 5 = poor) and 6 levels of functional impairment in daily and instrumental activities (as measured by ADL and I-ADL disability). The one-item self-rated health scale is a valid subjective measure of mortality, and predictor of mortality among Latinos when adjusting for acculturation but varies by income (Angel, Prickett & Angel 2012;Isaacs 2009). Most health surveys use a measure of self-rated health, predominantly assessed by a single subjective question (Butrica, Iams and Smith 2003/2004). Self-rated health has been found to be a strong predictor of mortality, not only in the elderly, but also in different age groups and cultures (Angel & Mudrazijia 2011). It is also an effective indicator of present health status, because it may reflect the various dimensions of health, including individuals' emotional, social, and cultural attributions of and reactions to physical health limitations, which are unlikely to be adequately addressed in a single study (Butrica, Iams & Smith 2003/2004). As such, the use of a one-item, self-rated health scale is an effective measure of the health of participants.
The Katz Index of Activities of Daily Living (ADLs) was used to measure health and functioning. The scale ranges from 0 to 7 and indicates whether the respondent required help in: bathing, dressing, eating, grooming, toileting, transferring, and walking across a room (Katz et al. 1963). Another measure was used with a similar scale from 0 to 7 to indicate whether help was required with the following Instrumental Activities of Daily Living (I-ADLs): light housework, preparation of meals, taking medications, grocery and clothes shopping, using the telephone, and managing money (Lawton & Brody 1969).
The 6 levels of functional ability were: 1 = limited in ADL; 2 = limited in I-ADL; 3 = Unable-major; 4 = Limited-major; 5 = Limited-other; and 6 = Not limited. We used family support variables from wave 4 (2000-01) to predict nursing home use in wave 5 (2004-05). This accounts for time lag between the period when families are juggling caregiving challenges and contemplating adjustments in long-term care, to actual entry into a facility in wave 5 (2004-05).
Kin availability
We expected that a higher number of living adult children, cohabitation with a spouse and/or adult child, and closer proximity to the nearest adult child would represent higher capacity to provide support by family. Family support was ascertained by the older adults' 1) number of living children, and 2) whether they lived with an adult child (1 = yes, 0 = no). Proximity to nearest adult child was measured in hours travel time. Time demands on adult children are likely buffered by the presence or absence of the elderly parent's spouse is alive. Thus, living with a spouse was also included (1 = yes, 0 = no).
Demographic characteristics
The analyses took into account other factors that likely affect long-term care use, including stratification by gender and the respondent's age as a continuous variable in years. Health insurance coverage was dichotomized as “1” if participants reported having Medicaid only or dual coverage by Medicare and Medicaid, and “0” for all other forms or lack of insurance. This designation concurs with aforementioned findings, which maintain that access to these public sources of long-term care financing is a significant predictor of long-term care use.
Analyses
QALY weights were computed according to participants' self-rated health (excellent, very good, good, fair, or poor) and level of independence according to the ADL and I-ADL scales (Appendix A). The H-EPESE had analogous questions to the National Health Interview Survey (NHIS) form which the QALY weights were drawn (Erickson, Wilson & Shannon 1995). Three logistic regression models were tested to estimate the likelihood of older Mexican Americans entering a nursing home or assisted living facility, as predicted by kin opportunity costs, family support, and demographic characteristics. Each model included only QALY weights, ADLs, or I-ADLs. While the outcome measure (nursing home and assisted living facility use) was drawn from wave 5 (2004–05), predictor variables in the model from the previous wave were included for analyses. All analyses were performed using SAS® 9.2. These steps and analyses were repeated in subsamples of only women (N=628) and only men (N=381).
QALY weights to be estimated are shown in the Appendix. Scores ranged from .1 to 1, with lower scores indicating higher functional impairment and worse self-rated health. Thus, low QALY weights reflect greater time spent on the care of elderly parents and higher risk of nursing home use. For example, participants reporting “poor” health and “limited in ADL” scored 0.1. In addition, we chose to dichotomize ADL and I-ADL indices as none versus one or more dependency due to their asymmetry and model these separately, to examine their individual influence on nursing home care.
Results
Approximately 5% of the total sample of men and women were newly institutionalized in a nursing home at wave 5 (2004–05), as shown in Table 1. Mexican American women and men had a mean age of 78.3 and 77.9 years (p < .01), respectively, and an average of five living children. Men were more likely than women to be living with their spouse only (p < .01); while a larger fraction of women than men reported living with at least one adult child. The average travel time for the nearest living child to visit an elderly parent was shorter for women (15 minutes) than for men (30 minutes). The mean QALY weights in our sample were higher for men than for women (p < .01). Conversely, female respondents reported more I-ADL disability then men (p < .01) and also required greater assistance with at least one ADL (p < .01). Women also have a higher participation than men in the Medicaid program, but the differences were not statistically significantly different from one another.
Table 1. Older Mexican-Americans use of long-term care by time inputs.
| Women (N = 628) |
Men (N = 391) |
|||
|---|---|---|---|---|
|
| ||||
| Mean | SD | Mean | SD | |
| Use of nursing-home or assisted living facility Care time | .05 | .21 | .05 | .22 |
| QALYa weights ** | .49 | .27 | .62 | .26 |
| ADLb** | .20 | .40 | .12 | .33 |
| I-ADLc** | .53 | .50 | .27 | .45 |
| Kin availability | ||||
| Number of living children | 4.80 | 2.81 | 5.39 | 2.74 |
| Child Proximity (hours) | .26 | 1.35 | .53 | 2.50 |
| Child Co-residence** | .34 | .47 | .26 | .44 |
| Live with spouse** | .35 | .48 | .78 | .41 |
| Covariates | ||||
| Age (years) | 78.3 | 5.20 | 77.9 | 4.80 |
| Any Medicaid | .36 | .48 | .26 | .44 |
QALY = Quality-adjusted Life Years
ADL = Activities of Daily Living
I-ADL = Instrumental Activities of Daily Living.
p < .01
Beta coefficients are shown for the final three logistic regression models in the pooled sample (Table 2). Nursing home facility use was modeled by adult child's opportunity costs, calculated from estimated care needs (i.e., QALY weights, ADLs, and I-ADLs), kin availability (i.e., number of adult children, living with spouse and/or adult child, proximity to nearest adult child), and controls for age and Medicaid coverage. Because the QALY weight is highly correlated with ADL and I-ADL variables, we present separate models for each of these variables independently, with controls for kin support, health insurance, and age. Subsequent models presented in Table 3 are the same regression analyses stratified by gender.
Table 2.
Logistic Regressions Of Opportunity Costs' Effect On Long-Term Care (N = 1,009).
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| QALYa weights | -2.10** | - | - |
| ADLb | - | 1.01** | - |
| I-ADLc | - | - | 0.94** |
| Male | .58 | .45 | .53 |
| Number of children | -.12* | -.11 | -0.12* |
| Child Proximity | -.29 | -.33 | -.25 |
| Child Co-residence | .06 | .09 | 0.10 |
| Live with spouse | -.10 | -0.13 | -0.07 |
| Age | .05* | 0.06* | 0.05* |
| Any Medicaid | .42 | 0.45 | 0.45 |
QALY = Quality-adjusted Life Years
ADL = Activities of Daily Living
I-ADL = Instrumental Activities of Daily Living.
p < .05.
p < .01.
Table 3.
Logistic Regressions Of Kin Opportunity Costs' Effect On Long-Term Care Use Among Older Mexican-American Men (N = 1,009).
| Women (N = 628) |
Men (N = 391) |
|||||
|---|---|---|---|---|---|---|
|
| ||||||
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
|
|
|
|||||
| QALYa weights | -3.07** | - | - | -1.04 | - | - |
| ADLb | - | 1.22** | - | - | .53* | - |
| I-ADLc | - | - | 1.21** | - | - | .67 |
| Number of Children | .17* | -.15* | -.17* | .00 | .01 | .01 |
| Child Proximity | -.25 | .10 | .05 | -.20 | -.22 | -.18 |
| Child Co-residence | .46 | .53 | .51 | -.47 | -.47 | -.46 |
| Live with spouse | -.10 | -.11 | -.03 | -.42 | -.45 | -.42 |
| Age | .03 | .03 | .04 | .07 | .08 | .06 |
| Medicaid | .29 | .33 | .31 | .25 | .25 | .27 |
QALY = Quality-adjusted Life Years
ADL = Activities of Daily Living
I-ADL = Instrumental Activities of Daily Living.
p < .05;
p < .01
In Table 2, Model 1 estimates the effect of opportunity costs and kin availability on long-term care use controlling for QALY weights; Model 2 considers ADLs alone; and Model 3 examines I-ADLs. In all three models, our three measures of opportunity costs (i.e., QALY weights, ADLs, and I-ADLs) significantly predicted entry into a nursing home or assisted living facility. In Model 1, lower QALY weights (i.e., higher functional impairment and worse self-rated health) increased the risk for entry into a nursing home or assisted living facility (B = -2.14, P < .01). In Models 2 and 3, ADLs (B = 0.96, P< .01) and I-ADLs (B = 0.98, P< .01) significantly increased risk for institutionalization, respectively.
Table 3 presents the logistic regression model stratified by gender. The model excludes controls for gender used in the pooled model in Table 2. The results are largely the same for women with one important exception. Mexican-American women with a higher number of living adult children were at a lower risk of entering a nursing home or assisted living facility. This finding is consistent with our theory that larger kinship networks would reduce long-term care use (Model 1 (QALY weights), B = -.17, p< .05; Model 2 (ADLs), B = -.15, p< .05; and Model 3 (I-ADLs), B = -.17, p< .05).
The results in Table 2 for men differ from women on care time and kin availability measures. Among the sample of older Mexican-American men, ADL disability was the only statistically significant determinant among the multiple predictors of nursing home use. Like their female counterparts, men who reported receiving help with personal care had an increased likelihood of nursing home use (B = .53, p < .05) as shown in Model 2. This finding was expected, as the need for ADL assistance is one of the most common reasons for admission to a nursing home. In addition to conducting separate models for each gender, we ran one model using interaction terms with gender and each variable. We found that while interaction terms produced slightly different estimates, none were significantly different from zero. The predicted effects of other variables in the model, while in the expected direction, are more ambiguous and may be due to insufficient statistical power.
Discussion
The opportunity costs of providing care to aging parents can become daunting on adult children, and reach a tipping point that lead Mexican-American families to seek institutional long-term care. Elderly parents' care needs, which are highly correlated with the time inputs required, are the strongest correlate of long-term care use and, consequently, adult children's opportunity costs. We hypothesized that adult children's time inputs in furnishing assistance would increase in proportion to the functional health needs of the elderly parent, but alleviated by dispersion (equal or unequal) of care responsibilities among siblings, the parent's spouse, and their proximity to the elderly parent. Moreover, the size of the kinship network and proximity to the elderly parent would purportedly increase the probability that at least one of them would step into the caregiving role, thereby preventing long-term stays in nursing homes or assisted living facilities even as care requirements increased. For Mexican-American men, at least, it appears that marriage matters more than the convoy of support provided by grown children. On the other hand, for Mexican-American women, where widowhood is common, having more children to rely on is significant in reducing the risk of long-term care.
As predicted, we found that estimated care time was largely driven by older adults' QALY weights and physical health limitations, which increased the adult child's opportunity costs, and consequently, raised the elderly parent's risk of entering a nursing home or assisted living facility. Travel times to care for elderly parents were low in this sample (15 minutes), which reflects the common, albeit declining, practice that Mexican-American families reside in close proximity or large households. In contrast to our hypothesis, the adult child's opportunity costs, were not tempered by the availability of kin, the presence of the older adults' spouse, or close proximity to the elderly parent, in predicting long-term care use for men.
These findings suggest that even when adult children and/or spouses are present and relatively close in proximity, the older adults' physical limitations may require much more time and attention than the immediate family can provide. The inconsequential role of kinship size and proximity to elderly parents' long-term care use did not persist in our regression models with the subsample of females. In fact, we observed that women with a higher number of living adult children were at a lower risk of entering a nursing home or an assisted living facility, compared to women with fewer children.
In the best of scenarios, larger families may engage secondary caregivers in dividing the workload to reduce time inputs per adult child. It is important, however, to avoid assumptions that a large family network evenly shares the caregiving responsibilities. An elderly parent may have ten offspring, but only one or two may be able or willing to provide care. Many factors have the potential to influence which family member will care for the elderly parent. The primary caregiver may self-select or be coerced into the role, for a variety of reasons. They may have or be perceived to have the greatest availability, more resources, lower job commitment, better relationship with the parent, or be geographically most convenient. Gender is also a significant factor. Female children are more likely to be caregivers than males, especially in the Mexican-American culture, and assume the role without being given the choice or a say in the matter. Thus, having more children or a larger care network in sheer size does not necessarily translate into more readily available or quality care provision. Larger kinship networks therefore do not imply an equitable distribution of caregiving responsibilities. Rather, they may simply increase the probability that one of the offspring will step up to provide care.
The benefit of having many children on reducing women's risk of long-term care may be short-lived for future generations, in light of the sharp decline in fertility rates among Mexican-American women over the past decades. In 1960, Mexican-American women in the U.S. averaged 3.6 children per woman; by 2009 they averaged 2.0 children. Similar trends were observed in Mexico, where the fertility rate decreased from 7.3 to 3.6 children per woman (Pew Hispanic Research Center 2011). As the family network shrinks, the safety net for elderly parents will likely decrease as the potential pool of caregivers becomes scarce.
One important aspect of caring for the elderly is that co-residence has the potential to significantly reduce the amount of power that the child caring for the parent has in comparison to his or her siblings. Because of this, co-residency may not emerge as the best solution, resulting in elderly parents ending up in nursing homes rather than being cared for by children. This potentially explains the increase in rate that elderly parents are being admitted to nursing homes and assisted living facilities. In our sample, women were far more likely than men to live with an adult child and, as they become increasingly impaired, the demands adult children face will invariably become more serious. Such psychological and emotional potential dependency burden inherent in co-residence may create undue hardship on grown children caring for elderly parents as they enter into deep old age.
Possible limitations of the study include differences in the proportion of men and women in the sample, and overall small number to enter a nursing home. Additionally, this study excludes the use of home- and community-based support services, which aid older adults with staying at home. It is also important to note that selection bias may explain why most opportunity cost variables were insignificant in our model for men. The premature death of unhealthy men at the follow-up interview may result in an overrepresentation of healthier men among our older males cohort. This may result in an overrepresentation of healthier, better functioning men, who require less assistance from adult children (i.e. fewer time inputs) and also less likely to enter a nursing home. Men are also likely to reside with a spouse compared to older women, it may It is possible that the number of children has less bearing on men because of gender variation in longevity. Females outlive males in most countries. Thus, in their final years wives are able to serve as the primary caregiver for their husband, while children provide a supporting role, if any. Women are more likely to outlive their spouse, to be widowed or to live alone, and so there is a decreased likelihood that they will have a partner to care for them (Noel-Miller C 2010). Instead, elderly females may rely on support networks from adult children and friends more than elderly males. The relative importance of adult children to mothers, but not fathers, on the risk of entering nursing homes has been corroborated in other research.
Another restrictive component to this analysis was the estimation of wages, rather than through direct measurement. Like most aging studies, few capture this data, unless exclusively focused on caregivers. Future studies involving cohorts of older adults should also include information on adult children's opportunity costs (both quantifiable and intangible) in the form of wages lost, employment and financial strains, and other pursuits foregone. This is the major scalar omitted in Equation 1. The absence of survey information on opportunity costs may have led to an underestimate of the true opportunity costs felt by adult children because there is no variation in how the value of time varies by adult child. This sample included mostly low to middle-income families, thus wage and salary information may be relatively low. Given high poverty rates in the Hispanic community, family members caring for aging Mexican Americans may be particularly vulnerable to external factors that influence their ability to earn a living and save. In future generations, the wages of adult children of Hispanics may rise, and the increased variation in wages may make this an important determinant of nursing home use. In addition, opportunity costs borne by adult children must account for cultural perceptions about their personal obligation to furnish care to frail or disabled aging parents, or knowledge and attitudes about the range of long-term support services, including home- and community-based care. The long running, largest epidemiological study of older Mexican Americans employed for this research does not currently contain data on the adult caregivers (focal children) of participants, but will be available for the first time in the next few years.
As the population of older Mexican Americans increases and disability rates among this population climb, families may have to compromise on long-held traditional practices of providing all aspects of care to infirm relatives at home. This may be especially salient for older women with fewer children to assume the caregiving role. The majority of older Mexican Americans will enter old age with few or no assets, or quickly spend their savings to eventually qualify and rely exclusively on Medicaid as their long-term care insurer. While this paper focused on nursing homes and assisted living facilities, it is likely that older Mexican Americans' will opt for non-institutional long-term care among the wide range of home- and community-based services provided by the aging services network not sure what was trying to be said here. These are funded through Section 1915(c) Medicaid state waivers, cost-sharing, and the Older Americans Act. While Medicaid reimbursement for nursing homes remained unchanged between 1999 and 2008, expenditures for home- and community-based services for elderly and disabled grew by an astounding 163% (Ng & Harrington 2012). As financial pressures escalate, the U.S. government will continue to support states in rebalancing their long- term care system, shifting funds away from costly nursing homes to more affordable community-based care that enables older adults to age in place and retain more autonomy over their care. The Deficit Reduction Act of 2005 and Affordable Care Act of 2010 are just a few legislative examples of initiatives intended to support this migration of funding. This emphasis on home-and community-based care may be good news for Mexican-American families grappling with the decision to abandon home-based care. However, health and long-term care policies must ensure that these options sufficiently offset the extensive time burdens of care facing the often lone adult child; acknowledge the withering of a shared care system once common among Mexican-American families; and require providers to design culturally and linguistically compatible support services to increase their appeal, use, and effectiveness.
Acknowledgments
Funding support for this study was provided by a grant from the National Institute on Minority Health and Health Disparities (NCMHD), Grant #: R01MD005894 (P.I. Jacqueline L. Angel).
Appendix A
Quality-Adjusted Life Years Weights Activity Scale Definitions By Self-Rated Health And Activity Limitation.
| Activity Limitation | Excellent | Very Good | Good | Fair | Poor |
|---|---|---|---|---|---|
| Not Limited | 1.00 | 0.92 | 0.84 | 0.63 | 0.47 |
| Limited-other | 0.87 | 0.79 | 0.72 | 0.52 | 0.38 |
| Limited-major | 0.81 | 0.74 | 0.67 | 0.48 | 0.34 |
| Unable-major | 0.68 | 0.62 | 0.55 | 0.38 | 0.25 |
| Limited in I-ADLa | 0.57 | 0.51 | 0.45 | 0.29 | 0.17 |
| Limited in ADLb | 0.47 | 0.41 | 0.36 | 0.21 | 0.10 |
I-ADL = Instrumental Activities of Daily Living.
ADL = Activities of Daily Living
References
- Abraido-Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. American Journal of Public Health. 2006;96:1342–46. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali J, Avison WR. Employment transitions and psychological distress: The contrasting experiences of single and married mothers. Journal of Health and Social Behavior. 1997;38(4):345–62. [PubMed] [Google Scholar]
- Andel R, Hyer K, Slack A. Risk factors for nursing home placement in older adults with and without dementia. Journal of Aging and Health. 2007;19(2):213–228. doi: 10.1177/0898264307299359. [DOI] [PubMed] [Google Scholar]
- Angel JL, Angel RJ, McClellan JL, Markides KS. Nativity, declining health, and preferences in living arrangements among elderly Mexican Americans: Implications for long term care. The Gerontologist. 1996;36:464–473. doi: 10.1093/geront/36.4.464. [DOI] [PubMed] [Google Scholar]
- Angel JL, Angel RJ, Aranda MP, Miles TP. Can the family still cope? Social support and health as determinants of nursing home use in the older Mexican-origin population. Journal of Aging and Health. 2004;16:338–54. doi: 10.1177/0898264304264203. [DOI] [PubMed] [Google Scholar]
- Angel JL, Mudrazijia S. Public Policy and Aging Report. Washington DC: 2011. Raising the retirement age: is it fair for low-income workers and minorities? pp. 14–21. [Google Scholar]
- Angel JL, Prickett K, Angel RJ. Retirement security for black, non-Hispanic white, and Mexican-origin women: the changing roles of marriage and work. Journal of Women, Politics and Policy. 2012 In Press. [Google Scholar]
- Angel RJ, Angel JL. Hispanic families at risk: the new economy, work, and the welfare state. New York, NY: Springer Sciences; 2009. [Google Scholar]
- Assistant Secretary for Planning and Evaluation. Private longterm care insurance: following an admission cohort over 28 months to track claim experience, service use and transitions. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation U.S. Department of Health and Human Services; 2008. [Google Scholar]
- Becker GS. A theory of the allocation of time. Economic Journal. 1965;75(299):493–517. [Google Scholar]
- Bernstein N. With medicaid, long-term care of elderly looms as a rising cost. The New York Times; 2012. Sep 6, p. A1. 2012. [Google Scholar]
- Butrica BA, Iams HM, Smith KE. Social Security Bulletin. Baltimore, MD: Social Security Administration; 2003/2004. The changing impact of social security on retirement income in the united states. [Google Scholar]
- Crystal S, Shea D. Economic outcomes in later life: public policy, health, and cumulative advantage. New York: Springer: Springer Sciences; 2003. [Google Scholar]
- Durand J, Telles E, Flashman J. The demographic foundations of the Latino population Transforming our common destiny: Hispanics in the United Stat. Washington, DC: National Academy of Sciences; 2006. [Google Scholar]
- Elliott S, Painter J, Hudson S. Living alone and fall risk factors in community-dwelling middle age and older adults. Journal of Community Health. 2009;34(4):301–310. doi: 10.1007/s10900-009-9152-x. [DOI] [PubMed] [Google Scholar]
- Erickson P, Wilson R, Shannon I. Years of healthy life. Healthy people 2000. NCHS Statistical Notes. 1995;7(7):1–15. doi: 10.1037/e583992012-001. [DOI] [PubMed] [Google Scholar]
- Evercare and National Alliance for Caregiving. Hispanic family caregiving in the U S: findings from a national study. Bethesda, MD: Evercare; 2008. [Google Scholar]
- Fennell ML, Zhang FZ, Clark MA, Mor V. Elderly Hispanics more likely to reside in poor-quality nursing homes. Health Affairs. 2010;29:65–73. doi: 10.1377/hlthaff.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE Duval, Anderson KA, Kane RL. Predicting nursing home admission in the U.S.: a meta-analysis. BMC Geriatrics. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Kane RL, Rosaline A, Newcomer R. Predictors of institutionalizationin Latinos with dementia. Journal of Cross Cultural Gerontology. 2006;21:139–55. doi: 10.1007/s10823-006-9029-8. [DOI] [PubMed] [Google Scholar]
- He W, Sengupta M, Velkoff VA, DeBarros KA. Current Population Reports Special Studies. U.S. Census Bureau; 2005. 65+ in the United States:2005. [Google Scholar]
- Herrera AP, Lee JW, Palos G, Torres I. Cultural influences in the patterns of long-term care use among Mexican-American family caregivers. Journal of Applied Gerontology. 2008;27:141–65. [Google Scholar]
- Holtz-Eakin D. The long-term budget outlook. Washington, DC: Congressional Budget Office; 2005. [Google Scholar]
- Houser A. Women and long-term care. Washington DC: AARP; 2007. [Google Scholar]
- Isaacs JB. Spending on children and the elderly: An issues brief. Washgington, DC: Brookings Institution; 2009. [Google Scholar]
- Jolicoeur PM, Madden T. The good daughters: Acculturation and caregiving among Mexican-American women. Journal of Aging Studies. 2002;16:107–20. [Google Scholar]
- Thomas JF, Suzman R. The health and retirement study: an overview. Journal of Human Resources. 1995;30:S7–S56. [Google Scholar]
- Kalenkoski CM, Hamrick KS. How Does Time Poverty Affect Behavior? A Look at Eating and Physical Activity. Applied Economic Perspectives and Policy 2012 [Google Scholar]
- Kane RA, Kane RL, Ladd RC. The heart of long-term care. New York, NY: Oxford University Press; 1998. [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the agedthe index of adl: a standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185(12):914–19. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Katz S. Assessing self maintenance: Activities of daily living, mobility and instrumental activities of daily living. Journal of the American Geriatrics Society. 1983;31(12):721–26. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- Kaye HS, LaPlante MP, Harrington C. Do noninstitutional long-term care services reduce Medicaid spending? Health Affairs. 2009;28:262–72. doi: 10.1377/hlthaff.28.1.262. [DOI] [PubMed] [Google Scholar]
- Keehan SP, Cuckler GA, Sisko AM, Madison AJ, Smith SD, Lizonitz JM, Poisal JA, Wolfe CJ. National health expenditure projections: modest annual growth until coverage expands and economic growth accelerates. Health Affairs. 2012;31(7):1600–12. doi: 10.1377/hlthaff.2012.0404. [DOI] [PubMed] [Google Scholar]
- Langa KM, Valenstein MA, Fendrick AM, Kabeto MU, Vijan S. Extent and cost of informal caregiving for older Americans with symptoms of depression. American Journal of Psychiatry. 2004;161:857–863. doi: 10.1176/appi.ajp.161.5.857. [DOI] [PubMed] [Google Scholar]
- Langa KM, Chernew ME, Kabeto MU, Rosaline A. National estimates of the quantity and cost of informal caregiving for the elderly with dementia. Journal of General and Internal Medicine. 2001;16:770–78. doi: 10.1111/j.1525-1497.2001.10123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langa KM, Vijan S, Hayward RA. Informal caregiving for diabetes and disabetic complications among elderly Americans. Journal of Gerontolgoy: Social Sciences. 2002;57:S177–86. doi: 10.1093/geronb/57.3.s177. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EP. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- Markides KS, Eschbach K, Ray LA, Peek MK. Census disability rates among older people by race/ethnicity and type of hispanic origin. In: Angel JL, Whitfield KE, editors. The health of aging hispanics: the mexican-origin population. New York, NY: Springer; 2007. [Google Scholar]
- Markides KS, Rudkin L, Angel RJ, Espino D. Health status of Hispanic elderly. In: Martin LG, Soldo BJ, editors. Racial and ethnic differences in the health of older Americans. Washington, DC: National Academy Press; 1997. pp. 285–300. [PubMed] [Google Scholar]
- McCartnery S, Bishaw A, Fontenot K. U.S. Census Poverty rates for selected detailed race and Hispanic groups by State and place: 2007-2011. American Community Survey Briefs. 2013 Feb; 2013. [Google Scholar]
- Murray C. Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bulletin of the World Health Organization. 1994;72:429–445. [PMC free article] [PubMed] [Google Scholar]
- Nguywn HT, Black SA, Ray LA, Espino DV, Markides KS. Cognitive impairment and mortality in older Mexican Americans. Journal of the American Geriatric Association. 2003;51:178–83. doi: 10.1046/j.1532-5415.2003.51055.x. [DOI] [PubMed] [Google Scholar]
- Novak K, Riggs J. Health Affairs. Chicago, IL: Alzheimer's Association; 2004. Hispanics/Latinos and alzheimer's disease. [Google Scholar]
- O'Brien E. Long-term care: Understanding Medicaid's role for the elderly and disabled. Washington, DC: Kaiser Family Foundation; 2005. [Google Scholar]
- Otiniano ME, Snih SA, Goodwin JS. Factors associated with poor glycemic control in older Mexican American diabetics aged 75 years and older. Journal of Diabetes Complications. 2012;26:181–86. doi: 10.1016/j.jdiacomp.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Hispanic Research Center. Health Affairs. Washington, DC: Pew Hispanic Research Center; 2011. The Mexican-American boom: Births overtake immigration. [Google Scholar]
- Pinquart M, Sörensen S. Ethnic differences in stressors, and physiological outcomes of family caregiving: A meta-analysis. Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- Reinhard SC, Kassner E, Houser A, Mollica R. Raising expectations: A state scorecard on long-term services and supports for older adults, people with physical disabilities, and family caregivers. Washington, DC: AARP; 2011. [Google Scholar]
- Sabogal F, Marin G, Otero-Sabogal R, Marin BV, Perez-Stable EJ. Hispanic familism and acculturation: What changes and what doesn't? Hispanic Journal of Behavioral Sciences. 1987;9:397–412. [Google Scholar]
- Sands LP, Xu H, Weiner M, Rosenman MB, Craig BA, J Thomas J. Comparison of resource utilization for Medicaid dementia patients using nursing homes versus home and community based waivers for long-term care. Medical Care. 2008;46:449–53. doi: 10.1097/MLR.0b013e3181621eae. [DOI] [PubMed] [Google Scholar]
- Stone R. Long-term care for the elderly. Washington, DC: Urban Institute Press; 2011. [Google Scholar]
- U.S. Census Bureau. Current Population Survey, Annual Social and Economic Supplement. Income, Poverty, and Health Insurance Coverage in the United States: 2011. 2012 Sep;:60–243. 2013. [Google Scholar]
- Ujvari K. Long term care insurance: 2012 Update. Washington, DC: AARP Public Policy Institute; 2012. [Google Scholar]
- Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exercise among older Mexican Americans with type 2 diabetes. Diabetes Educator. 2004;30:980–93. doi: 10.1177/014572170403000619. [DOI] [PubMed] [Google Scholar]
- White-Means SI, Rubin R. Trade-offs between formal home health care and informal family caregiving. Journal of Family and Economic Issues. 2004;25:335–38. [Google Scholar]


