Abstract
Using data from a stratified random sample of 281 foreign-born adolescents and their parents, this study provides data on migration-related trauma exposures and examines how the migration process influences the risk of experiencing trauma and developing Post-Traumatic Stress Disorder (PTSD). We find that 29% of foreign-born adolescents and 34% of foreign-born parents experienced trauma during the migration process. Among those that experienced trauma, 9% of adolescents and 21% of their parents were at risk for PTSD. Pre-migration poverty combined with clandestine entry into the US increased the risk of trauma and the subsequent development of PTSD symptoms. Post-migration experiences of discrimination and neighborhood disorder further exacerbated this risk, while social support and familism mitigated it. Our results emphasize the importance of understanding how factors prior to, during, and after migration combine to influence the health of immigrants.
Keywords: immigrant, Latino, Hispanic, PTSD, trauma, health, acculturation
Approximately 37 million immigrant adults and 3 million immigrant children (ages 0–17) live in the United States (US Census 2010). Over half (53%) are Hispanic of Latin American or Caribbean origin (Acosta & Partirica de la Cruz, 2011). Before, during, and after migration to the US many of these Latino immigrants are at risk for experiencing trauma and developing symptoms of Post-Traumatic Stress Disorder (PTSD). These traumatic experiences can have severe and long-term impacts not only on the mental health of immigrants but also on their adjustment to life in the US (Makley and Falcone, 2010). Trauma can led to difficulties at work for adults and difficulties at school among children (Eisenman, et al., 2008; Kataoka, et al., 2009; MacMillan, 2001; Porche, et al., 2011).
According to the American Psychiatric Association (APA), trauma is defined as having experienced, witnessed or been confronted with an event that involves actual or threatened death or serious injury, or threat to the physical integrity of oneself or others (APA, 2000). Common checklists of trauma experiences include questions about whether individuals have either experienced or witnessed a life-threatening accident; fire, flood, or a natural disaster; combat or war; rape or sexual molestation; childhood abuse or neglect; or someone being badly injured or killed (Kessler, et al., 1995; Copeland et al., 2007). Symptoms of PTSD can include re-experiencing the event; avoiding thoughts, feelings or experiences associated with the event; and increased arousal, such as difficulty sleeping, irritability, and hyper-vigilance (APA, 2000).
First recognized as a syndrome suffered by war veterans, most PTSD research among immigrants focuses on refugees from war-torn areas (Bronstein and Montgomery, 2011; Johnson and Thompson, 2008; Lustig, et al., 2004). These studies report rates of PTSD between 19–54% among refugee children, rates well above prevalence rates of 2–9% in studies of the general population. Among adult refugees in community-based samples, rates vary between 14–19%. Traumatic exposures for refugee populations typically include combat experience and war or terror victimization (e.g., forced separation from family, torture, and having a friend or family member killed).
Immigrants who are not classified as refugees, especially those with low socioeconomic status and those who migrate to a country without authorization, can experience some of the same traumas experienced by refugees. Yet few scholars have investigated the prevalence of traumatic experiences or PTSD in a community-based sample of Latino immigrant adults and their children. Evidence suggests that the majority of men (61%) and women (51%) in the US experience at least one potentially traumatic event in their lifetimes (Kessler, et al., 1995). Potentially traumatic events are prevalent among children as well. In one large longitudinal study of children, 68% reported experiencing a potentially traumatic event by the age of 16 (Copeland et al., 2007). Both of these studies focus on a primarily white, non-Latino population and neither indicates that Spanish-speaking individuals were included in their samples.
The only US-based population study of Latino adults (ages 18+) found that approximately 16% experienced any anxiety-related disorder and 4% experienced PTSD within their lifetimes, but these prevalence rates differed significantly by Hispanic background or country of origin (Alegria, et al., 2008; Alegria, et al., 2007). Other studies of Latino populations based primarily on convenience samples from health care facilities have found much higher rates of PTSD (18–38%), especially among those exposed to natural disasters, war and political violence, life-threatening illnesses, or sexual abuse (Cervantes, et al., 1989; Eisenman, et al., 2003; Heilemann, Kury, and Lee, 2005; Santa-Maria and Cornille, 2007; Steel, Chey, and Silove, 2010; Yule, 2001). Additionally, some studies suggest that Hispanics and immigrants develop PTSD at much higher rates than US-born whites or African Americans (Marshall, Schell, and Miles, 2009; Pole, Gone, and Kulkarni, 2008); whereas others find just the opposite (Heilemann, Kury, and Lee, 2005; Alegria, et al., 2007, 2008; Roberts et al., 2011).
US-based studies of PTSD among children have found rates of 3–8% in adolescents and young adults (De Bellis and Van Dillen, 2005; Yule, 2001). One study of immigrant children (ages 8–15) from Los Angeles found that 32% reported clinically-significant levels of PTSD symptoms (Jaycox, et al., 2002). But others find lower rates and suggest that foreign-born Latino youth are less at risk of PTSD than US-born Latino youth (Flores, et al,. 2010; Kataoka, et al., 2009). None of these studies specifically explores how the migration process influences trauma exposure and the development of PTSD.
Given the growth of Latino immigrant populations in the US (Acosta & Partirica de la Cruz, 2011), it is essential to understand how the migration process shapes their health and adjustment. Migration to the US is a dynamic process which begins in immigrants’ home countries (pre-migration), extends through the time spent in transit to a new destination (during migration) and continues upon their arrival in receiving countries (post-migration; Perreira and Ornelas, 2011). Yet the vast majority of previous research on the immigrants and their children focuses only on post-migration factors that influence immigrants’ well-being. Few studies have documented how the migration process (before, during, and after settlement in a new country) contributes to mental health among Latino immigrant parents and their children (Cervantes, et al., 2012; Ornelas and Perreira, 2011; Potochnick and Perreira, 2010; Santa-Maria and Cornille, 2007).
Examining migration as a process unfolding over time and within families, this study provides prevalence data on the exposure of immigrant adolescents and their parents to trauma before, during, and (for parents) after migration. In addition, this study examines risk and protective factors at each stage of the migration process that influence the development of PTSD symptoms. We conclude with a discussion of strategies to reduce traumatic exposures among immigrant children and their caregivers and mitigate their risk for developing PTSD.
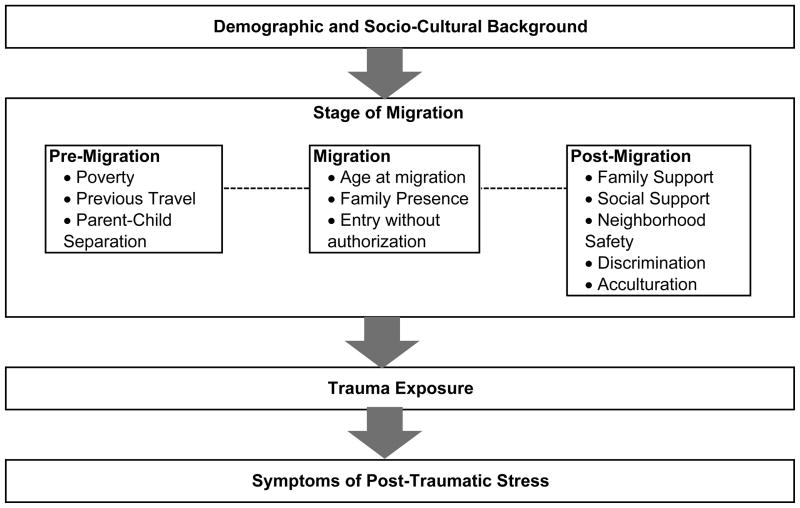
Our framework for this analysis stems from segmented assimilation theory and developmental theories which emphasize the role of contexts on the well-being of immigrants (Portes and Rumbaut, 2001; Rumbaut, 1991; Garcia-Coll and Magnuson, 1997). Segmented assimilation theory suggests that both the contexts of exit and reception influence the mental health of immigrant parents and their children. Critical factors include immigrants’ socioeconomic status in their country of origin, their motivations for leaving, the safety of their journey, and the social context into which they arrive (Portes and Rumbaut, 2001; Rumbaut 1991). Developmental theories posit that the consequences of migration for children will vary by their age as well as the socio-cultural, neighborhood, and family resources available to them (Garcia-Coll and Magnuson, 1997; Lusting et al., 2004). Moreover, experiences at one stage of migration can influence experiences at another stage of migration (Perreira and Ornelas, 2011). Thus, the risk of experiencing trauma and developing PTSD can accumulate throughout the migration process. Figure 1 provides a conceptual overview of these relationships.
Figure 1.
The Migration Process and the Risk for Trauma and PTSD
Pre-migration Experiences
A variety of factors influence parent’s decisions to migrate and to bring their children to the US (Massey and Espinosa, 1997). Among these, economic hardships in their home countries and previous experiences with migration to the US can critically shape their migration and settlement experiences. For children who immigrate, a protracted separation from parents who have immigrated earlier can add to the hardships experienced before and during migration and can result in family conflict when children are re-united with their parents in the US (Suarez-Orozco, Tadorova, and Louie, 2002).
Many immigrants who have lived in poverty prior to their migration to the US have endured years of chronic stress and have been exposed to war and political violence (Eisenman, et al., 2003; Infante, et al., 2011). With limited educations and income, these impoverished immigrants have few legal avenues for migrating to the US and often enter clandestinely, without authorization (Donato and Armenta, 2011; Riosmena and Massey, 2012). They are consequently at increased risk for exposure to trauma and the development of PTSD.
While chronic poverty prior to migration can potentially increase the challenges of migration and settlement, previous visits to the US may facilitate migration and settlement. Immigrants learn through experience how best to navigate the migration process, avoid problems, and find work and resources to assist with their settlement (Massey, Durand, and Malone, 2002). At the same time, each additional migration can lead to new trauma exposures and increase the risk of developing PTSD, especially for those entering without authorization.
Historically, males have undertaken the risk of migration while leaving their wives and children behind. In recent decades though, women have increasingly migrated alone or with their spouses while leaving their children in the care of friends or relatives (Donato, 2010). Suarez-Orozco and colleagues (2002, 2006) have estimated that almost one-third of foreign-born children stay in their countries of origin with a relative before re-uniting with their parents in the US. Scholars typically expect parent-child separation to increase the stress of migration and the risk of developing PTSD after exposure to trauma (Masten and Narayan, 2012; Santa-Maria and Cornille, 2007). This may be especially true in the absence of an alternative caregiver with whom the child can form an emotional bond (Masten and Narayan, 2012). Among refugee populations, forced family separation and the death of primary caregivers result in the presence of unaccompanied children who display high levels of psychological distress (Bronstein and Montgomery, 2011; Ludwig et al., 2004).
In non-refugee immigrant populations, parents may choose to migrate first and bring their children to the US at a later date (and older age) as a protective strategy. These children are not left alone or with strangers but are typically left with extended family with whom they already have social and psychological attachments (Suarez-Orozco, Tadorova, and Louie, 2002). This sequential family migration strategy allows parents to migrate safely, adjust to life in the US, and save money to help bring their children to the US through either legal or safer modes of entry without authorization. Previous studies provide some evidence of a link between family separations and depression among immigrant children (Suarez-Orozco, Tadorova, and Louie, 2002). However, no clear links between family separation and anxiety or anxiety-related disorders such as PTSD have been established among non-refugee immigrant populations.
Migration Experiences
After deciding to migrate to the US, immigrant parents and their children must next decide how best to migrate. Although the vast majority of immigrants (approx. 80%) enter the US with legal authorization on family, work, refugee, student or tourist visas, many Mexicans and other Central Americans have limited access to these visas and enter more frequently without authorization (Donato and Armenta, 2011). Even those who enter with legal authorization may sometimes overstay their visas and join the ranks of the unauthorized population living in the US. As a result, the majority (approx. 70%) of the unauthorized immigrant population is of Mexican or other Central American origin (Infante, et al., 2011).
Entry to the US without legal authorization can involve arduous journeys with exposure to extreme physical hardships as well as violence (DeLuca, McEwen, and Keim, 2010; Infante, et al., 2011; Rasmussen, et al., 2007). Consequently, those who enter without authorization may be at substantial risk of trauma and the development of PTSD. Children immigrating at younger ages are particularly vulnerable to victimization during the migration journey (Cavazos-Rehg, Zayas, and Spitznagel, 2007; DeLuca, et al., 2010) and can have fewer social resources to promote their resilience and forestall the development of mental health problems such as PTSD (Alegria, et al,. 2007; Vega, et al., 2004). Alternatively, young children may also be protected from developing PTSD after a traumatic exposure by lack of awareness due to cognitive immaturity (Masten and Narayan 2012). For these reasons, we expect young children to be at greater risk of trauma but potentially lower risk of developing frequent PTSD symptoms. Adults can also mitigate the risk of trauma during migration for themselves and their children by traveling as part of a larger family unit that can both offer protection from potential assailants and buffer family members from the effects of stress. Thus, we expect that children and their parents who migrate as a family unit will be less at risk for trauma and PTSD.
Post-migration Experiences
Upon entering the US, immigrants can be exposed to several additional hardships which both increase the likelihood that they will experience trauma and that trauma will result in subclinical or clinical levels of PTSD symptoms. In particular, research shows that immigrants with distinctive phenotypical characteristics or religious practices experience high rates of racial-ethnic discrimination in the US and elsewhere (Suarez-Orozco and Qin, 2006). Moreover, perceived racial-ethnic discrimination acts as a social stressor making some immigrants and ethnic minorities in the US feel threatened and powerless and as a biological stressor promoting biochemical changes that increase the risk of poor physical and mental health outcomes (Flores, et al., 2010). Thus, some scholars argue that racial-ethnic discrimination is not only stressful but potentially traumatizing (Bryant-Davis and Ocampo, 2005).
As an economically disadvantaged group, Latino immigrants in the US also find themselves segregated into more impoverished and high crime neighborhoods and schools where additional exposures to violence and discrimination can occur (Charles, 2006; Oropesa, 2012; Orfield and Lee, 2005). These exposures can directly increase the risk for PTSD (Jaycox, et al., 2002; Kataoka, et al. 2009). Moreover, experiences of discrimination and neighborhood disorder marginalize immigrants and can keep them from accessing sources of institutional support in their communities which could alleviate the stresses of migration and settlement (Fortuna, 2008; Garcia-Coll, et al,. 1996; Pole, et al., 2008).
In contrast to discrimination and neighborhood disorder, the presence of strong family and social support systems typically protect parents and their children from exposure to trauma after migration and the development of PTSD (Masten and Narayan, 2012; Pole, et al., 2005). Household caregiving responsibilities and strict parental controls can leave immigrant children with little time or opportunity to engage in risky behaviors (Suarez-Orozco and Qin, 2006) and imbue them with a sense of family obligation which motivates them to stay out of trouble (Fuligni and Pendersen, 2002). Additionally, family and social support systems can buffer immigrants from stress and promote resiliency across the life course. Thus, previous research consistently finds positive associations between familism (i.e. a strong connection and loyalty to family), social support, and mental health (Kuperminic, et al., 2009; Alegria, et al., 2007).
Finally, one of the most heavily researched aspects of the post-migration experience – acculturation – has an ambiguous theoretical influence on mental and physical health (Finch, et al., 2009). Measured in a variety of ways (immigrant generation, years in the US, language usage, and scales measuring adaptation to US socio-cultural norms) acculturation cannot be expected to have a causal influence on exposure to trauma prior to or during migration. However, it may influence how immigrants deal with these stressful events and thus their risk for PTSD symptoms after migration. Years in the US can signal increased time since exposure to trauma for those exposed prior to or during migration; English language skills can provide a greater capacity to access health services and other institutional resources in the US; and adaptation to US socio-cultural norms can indicate a greater ease with navigating US social systems. Alternatively, time in the US can signal more cumulative exposure to post-migration discrimination and neighborhood disorder and the loss of Spanish-language skills can signal the weakening of protective ethno-cultural ties and diminished access to ethnocentric resources. Overall, too few studies with mixed results have considered the relationship between acculturation and PTSD to be conclusive (Escobar, et al., 1983; Heilman, Kury, and Lee, 2005; Marshall and Orlando, 2002; Ortega and Rosensheck, 2000).
METHODS
Study Design
We used data from the Latino Adolescent Migration, Health, and Adaptation Project (LAMHA), a population-based study of 281 foreign-born Latino youth (ages 12–18) and their primary caregivers (ages 25–60) in North Carolina. Between 2004–2006, LAMHA data were collected through a stratified-random, cluster sample of foreign-born Latino youth enrolled in high school or middle school (for details see Potochnick and Perreira, 2010). Parents and children could complete the survey in either Spanish or English. Due to low-literacy levels in the population, the parent survey was interviewer-administrated while the youth survey was interviewer-assisted (i.e. interviewers were available to answer questions if needed).
Sample
The sample reflects the background of first-generation immigrant youth and their caregivers living in North Carolina, one of the top 10 new immigrant receiving states in the United States (Fortuny, 2010). For the most part, youth participants had only recently immigrated to the US -- 65% had lived in the US for 5 years or fewer and 15% had moved to the US before their 6th birthday. The majority had emigrated from Mexico (78%) and spoke primarily Spanish at home (58%). Their primary caregivers were mostly biological mothers (76%) in their mid-thirties to early forties who had lived in the US for more than 5 years (74%). Primary caregivers other than biological mothers included fathers (14%) and other relatives (10%) such as an aunt or grandparent. We refer to all primary caregivers as parents throughout the remainder of this analysis. Most parents lived with a spouse or partner (73%) and neither they nor their partner had completed high school (67%). Most parents were also employed (74%) and living below the 2006 Federal Poverty Level (54%). Though poor, with an annual family income of $27,205, 50% of parents remitted an average of $240 per month to family in their home countries.
After deleting observations with missing data on the independent variables (Nadolescent=12, Nparent=22), the analytic sample for models of any traumatic experience was 269 for adolescents and 259 for caregivers. No data were missing on the dependent variables. After deleting observations with missing data on the dependent (Nadolescent=4, Nparent=0) and independent variables (Nadolescent=7, Nparent=13), the analytic sample for models of PTSD symptoms was 270 for adolescents and 268 for parents. Based on observed variables, all missing data were at random and on independent variables, such as parent’s age or years of parent-child separation, which could not be imputed.
Measures
We derived all measures utilized in this study from either adolescent interviews or parent interviews. Surveys of both adolescents and their parents included questions on their immigration histories, family relationships, school and community experiences, socioeconomic backgrounds, and health. All measures included in the LAMHA surveys had been previously evaluated for use with Latino and Spanish-speaking populations. Several were adapted from the Children of Immigrant Longitudinal Survey (CILS; Portes and Rumbaut 2001). For all scales used in this analysis, we report internal reliability measures and reference validation studies for each scale.
Traumatic experiences
This study focused on migration-related traumas experienced directly by participants. Respondents were asked about traumatic experiences in three separate sets of questions at three different points during their interview. Interviewers asked adult and adolescent respondents if they had experienced several types of events: (1) in the year prior to moving to the US, (2) during their journey to the US, and (3) ever in their lifetimes (prior to migration, during migration, or after migration). Respondents were prompted about specific types of events such as natural disasters, the arrest of a family member, the murder of a family member, crime, terrorism, war, and serious injury or illness. At each of these three times when respondents were prompted to share their experiences, they were also prompted through an open-ended question to share additional details and other types of traumatic experiences. Respondents mentioned other experiences such as domestic violence, assault, rape, and severe illness or injury (e.g., dehydration and hunger) in response to these open-ended questions. In accordance with the DSM-IV definition of trauma, responses to all open-ended questions were coded as traumatic events when they involved “actual or threatened death or serious injury, or threat to the physical integrity of oneself or others” (APA, 2000:427). Because it focuses on trauma directly experienced by respondents and associated with their migration experiences, our measure of trauma is more restrictive than measures focusing on life-time trauma that has either been experienced directly or witnessed (Kessler et al, 1995; Copeland et al., 2007).
PTSD symptoms
Adolescents completed the Trauma Symptom Checklist for Children –Abbreviated version (TSCC-A), a 44-item checklist that yields six clinical scales – Anxiety, Anger, Depression, Disassociation, and Post-Traumatic Stress (Briere, 1996). Item responses ranged from never (=0) to almost all the time (=3). Relying on only the 10-item post-traumatic stress scale, we followed standard protocol and classified adolescents as at risk for sub- or clinical PTSD if they had a T-score of 60 or greater. Raw scores ranged from 0 to 30 and are converted into standard T-scores (mean=50, SD=10) based on population norms which vary by gender and age. Internal consistency in our sample was good (α=.85).
Adult caregivers completed the 17-item Modified PTSD Symptom Scale (MPSS-SR; Falsetti, et al., 1993). The MPSS-SR can be used to assess both frequency and severity of symptoms. In addition, a PTSD diagnosis meeting the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, fourth edition) classification can be assigned if after experiencing trauma at least one re-experiencing symptom, three avoidance symptoms, and two arousal symptoms are endorsed (APA, 2000). Assessed over the past 2 weeks on a scale ranging from not at all (=0) to 5 or more times per week (=4), MPSS-SR frequency scores are equivalent to scores generated from the PTSD Symptom Scale (Foa, et al., 1993). Scores range from 0 to 51 and a frequency of 15 or greater is considered clinically significant in a community-based sample. The MPSS-SR demonstrated good overall consistency in our sample (α=.91). Following the guidelines for use of this scale, we classified adults as at risk for PTSD if the met either the frequency score threshold or the DSM-IV criteria (APA, 2000).
Pre-migration factors
We considered three pre-migration factors. Following guidelines for measuring poverty in Mexico (CONEVAL 2010), we classified parents and children as living in extreme poverty prior to migration (1=yes, 0=no) if they reported that their homes abroad had dirt floors and lacked indoor plumbing. We also considered whether or not the child or parent had previously traveled to the US (1=yes, 0=no). Lastly, in models focused on adolescents, we considered whether the child had been separated from his/her primary caregiver for at least one year prior to migration.
Migration factors
For both parents and children, we determined whether they had entered the US without authorization (1=yes, 0=no) and whether they had migrated with a family member (1=yes, 0=no). To determine whether they had entered without authorization, we used data from parents on their and their child’s place of birth, US citizenship, and the type of visas they and their child utilized to enter the country. Individuals indicating that they were not US citizens and who utilized no visa to enter the country were classified as having entered the US without authorization. In models focused on adolescents, we also included an indicator variable for migrating to the US at age 6 or less, a time of potentially low vulnerability to mental health problems. Ninety-five percent of youth who migrated to the US at age 6 or less were also accompanied by a family member.
Post-migration Factors
We assessed the effects of two groups of post-migration factors – acculturation and social environment. Acculturation was measured by years in the US, 4-items on language usage from the Short Acculturation Scale for Hispanics (SASH; Marin, et al., 1987), and the 10-item Psychological Acculturation Scale (PAS; Tropp et al., 1999). For both the SASH and PAS, items are answered on a 5-point Likert scale ranging from 1 (= Spanish only/Latinos only) to 5 (= Anglos only/English only). Items were then averaged to create scores ranging from 1 to 5 (α=.77 in our adult sample; α=.77 in our youth sample). Responses to language questions were highly skewed in our sample. Therefore, after scoring the SASH, we created an indicator variable (1=yes, 0=no) for being Spanish language dominant when the child had a score of less than two or when the parent had a score of 1.
Unlike the SASH, the PAS contained no questions on language usage. Instead, it focused exclusively on social contacts and cultural understanding. In our sample, internal consistency was high among adults (α=.88) and youth (α=.91). Among adults, correlations with the SASH score and years in the US were .54 and .17 (p < .05), respectively. Among youth, correlations with the SASH score and years in the US were .26 and .42 (p < .05), respectively.
In our evaluation of the post-migration social environment, we assessed two potential stressors – discrimination and living in an unsafe neighborhood. For both adolescents and parents, we identified whether they had “ever been discriminated against in the US” because of their race/ethnicity (1=yes, 0=no). We asked parents (but not youth) if any of the following were not a problem (=0), a minor problem (=1), or a major problem (=2) in their neighborhood: little respect for rules, laws, and authority; assaults and muggings; delinquency or gangs; or drug use or drug dealing out in the open (Oropesa, 2012; Portes and Rumbaut 2001). We then identified a neighborhood as unsafe (1=yes, 0=no) if they indicated that any of these issues was at least a minor problem.
We also assessed four potential buffers from stress– social support, familism, parent living with a partner, and church attendance. We measured adolescent social support using the 8-item social support scale included in the School Success Profile (Bowen, Rose, and Bowen, 2005). Affirmative responses were counted to create a scale ranging from 0 to 8 (=high support) with an internal consistency of .91 in our sample. We measured parents’ social support using the 12-item Interpersonal Support Evaluation List (ISEL; Cohen, et al., 1985). After reverse coding six items, items were summed to create a scale ranging from 0 to 36 (= high support) with an internal consistency of .76 in our sample. For both parents and adolescents, we utilize Gil and Vega’s (1996) 7-item familism scale (αadults=.87; αyouth=.91). Each item is evaluated on a 5-point Likert scale and items are averaged to create a score ranging from 1 to 5 (= high familism). Parents reported whether they were living with a spouse or partner (1=yes, 0=no). Both parents and adolescents reported whether they attended church once per week or more (1= yes, 0=no). Social support was modestly correlated with familism, among both parents (r =.13, p < .05) and adolescents (r =.15, p <.05). Because the PAS emphasizes socio-cultural contact, it was also modestly correlated with social support among adolescents (r =.12, p <.05).
Demographic controls
In all models we controlled for sex (female=1), age, and whether at least one parent had completed high school (yes=1).
Comorbid Conditions
We assessed depression and anxiety which frequently co-occur with PTSD. Among adolescents, scores of 20 or greater on the Children’s Depression Inventory (CDI, α=.85,; Kovacs 1992) and scores of 56 or more on the 10-item Multidimensional Anxiety Scale for Children (MASC-10, α=.72; March, et al. 1997) indicate clinically significant symptoms of depression and anxiety, respectively. Among adults, scores of 16 or greater on the Center for Epidemiological Studies –Depression (CES-D, α=.72) scale indicate clinically significant symptoms (Radloff, 1977). Data on anxiety were not available for adults.
Analytic Approach
We began by estimating the prevalence of traumatic experiences that occurred among immigrant youth and their caregivers prior to migration, during migration, and, for parents only, post-migration. We then estimated unadjusted (available upon request) and adjusted logit models to identify what pre-migration, migration, and post-migration factors are associated with reports of exposure to any trauma. Analyses were conducted separately for youth and their parents. Next, we evaluated the prevalence of PTSD using the MPSS-SR for caregivers and the TSCC-A for youth, their co-occurrence, and their co-morbidities with depression and anxiety. Finally, we estimated unadjusted (available upon request) and adjusted negative binomial regressions (NGB) to identify the strength of associations between traumatic experiences, pre-migration, migration, and post-migration factors and raw PTSD scores among youth and zero inflated NGB regressions among parents. NGB regressions account for the fact that symptom frequencies have a binomial distribution with over dispersion (Cameron and Trivedi, 1998). Zero-inflated models adjust for the large number of PTSD scores equal to zero among parents (89%; Greene, 2003). In parent models, PTSD scores can equal zero because the MPSS-SR is only completed by those adults reporting a traumatic experience and scores are set to zero for all others. NGB regressions are most easily interpreted by exponentiating the coefficient to obtain the multiplicative effect of each variable. In these models, a coefficient on x of exp(β)=1.3 would indicate that x is associated with a 30% increase in PTSD symptom frequency; whereas a coefficient of exp(β)=.7 indicates that x is associated with a 30% decrease in symptom frequency.
In additional analyses, we also estimated the risk of having PTSD (rather than symptoms of PTSD) using exact logit models for rare events (King and Ryan 2002; Meehta and Patel 1995). Results from exact logits were fully consistent with results from logit models of any trauma experience and NGB regressions of PTSD symptoms. Thus, we do not include them here.
For more parsimony, variables of interest which were never significant in either unadjusted or adjusted models and not necessary to control for confounding were dropped from all final models. For example, post-migration social support was not included in models of pre-migration and migration-related trauma among adolescents. But these factors are considered in models of trauma among parents.
RESULTS
Migration Experiences
Table 1 shows the distributions of pre-migration, migration, and post-migration characteristics in our samples of adolescents and their caregivers. Most children (68%) had been separated from their parents for at least one year prior to immigrating to the US but few (7%) had lived in extreme poverty. Though some children (15%) and their parents (23%) had visited the US prior to their most recent migration, most children (74%) and parents (69%) in our sample entered the US without authorization and were not legal permanent residents or US citizen. Most children (89%) and parents (68%) had also traveled to the US accompanied by another adult family member. Those who did not travel to the US together with a family member, migrated with a stranger or migrated alone. Once in the US, all children in this sample were reunited with their parents (90%) or other relative such as an aunt or grandparent (10%).
Table 1.
Sample Characteristics (N=281)
| Adolescents
|
Parents
|
|||
|---|---|---|---|---|
| M/% | (s.e.) | M/% | (s.e) | |
| Pre-Migration Experience | ||||
| Lived in extreme poverty | 7% | (2.9) | 7% | (2.9) |
| Previous travel to US | 15% | (3.9) | 23% | (4.1) |
| Parent(s) and child separated at least 1 yr | 68% | (4.4) | 68% | (4.4) |
| Migration Experience | ||||
| Child aged 6 or less when moved to US | 16% | (3.4) | - | - |
| Entered US without authorization | 74% | (4.5) | 69% | (4.8) |
| Migrated with a family member | 89% | (2.8) | 68% | (4.6) |
| Post-Migration Experience | ||||
| Acculturation | ||||
| Years in the U.S. (range: 0–17) | 4.5 | (0.3) | 7.2 | (0.4) |
| Psychological acculturation (range:1–5) | 2.1 | (0.1) | 1.7 | (0.1) |
| Primarily utilizes Spanish | 29% | (5.3) | 63% | (5.0) |
| Social Environment | ||||
| Ever experienced discrimination | 38% | (4.7) | 32% | (4.5) |
| Neighborhood unsafe | 18% | (3.0) | 18% | (3.0) |
| Adolescent social support (range: 0–8) | 5.6 | (0.1) | - | - |
| Parent social support (range: 0–36) | - | - | 26.9 | (0.8) |
| Parent living with partner | 73% | (5.2) | 73% | (5.2) |
| Familism (range: 1–5) | 4.3 | (0.1) | 4.5 | (0.0) |
| Attends church weekly | 50% | (5.2) | 42% | (5.1) |
| Demographic Characteristics | ||||
| Female | 55% | (5.0) | 84% | (3.4) |
| Age | 14.5 | (0.2) | 38.7 | (0.7) |
| Parent(s) completed high school | 35% | (4.7) | 35% | (4.7) |
Note: Data are weighted. Standard errors are adjusted for clustering and stratification of sample.
Because most parents and their children had lived in the US for fewer than 10 years, neither they (mean PAS score=1.7) nor their children (mean PAS score=2.1) reported high levels of psycho-social acculturation. In contrast, most children (71%) but few parents (36%) spoke, read, or thought in English at least as much as Spanish. After moving to the US, some youth and their parents reported experiencing discrimination (38% and 32%, respectively). Nearly, one-fifth of parents also reported that they and their children lived in unsafe neighborhoods with crime, gang, and drug problems. Helping buffer them against these stressors, both parents and youth reported high levels of social support and familism. In addition, 73% of parents lived with a spouse or partner and attended church weekly (42%).
Prevalence of Traumatic Events, PTSD symptoms, and Co-morbid Conditions
In 50% of the immigrant families we interviewed either a parent or child reported experiencing trauma (Table 2). In 13% of families, both the parent and child reported experiencing trauma. Overall, 29% of youth had had a traumatic experience either in the year prior to immigrating or during their migration to the US. Among youth, 9% had been victims of a natural disaster, had had a family member arrested or killed prior to immigrating to the US, or reported escaping war or persecution in their home countries. In addition, 23% had been robbed, physically attacked, or accidentally injured; or had become ill during their migration journey.
Table 2.
Traumatic Migration Experiences and PTSD Symptoms among Latino Immigrants (N=281)
| Adolescents (ages 12–18) | Parents (ages 25–60) | At Least One Family Member | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| n | % | n | % | n | % | |
| Trauma Pre-Migration | ||||||
| Family member or friend arrested | 11 | 5% | 5 | 2% | 16 | 7% |
| Family member or friend killed | 9 | 5% | 10 | 6% | 16 | 7% |
| Victim of a natural disaster | 8 | 5% | 8 | 5% | 14 | 7% |
| Victim of war or terrorism | <5 | <1% | 10 | 3% | 11 | 4% |
| Trauma During Migration | ||||||
| You were robbed | 14 | 3% | 22 | 5% | 33 | 8% |
| You were physically attacked | <5 | <1% | 6 | 2% | 10 | 3% |
| You were accidentally injured | 33 | 11% | 22 | 4% | 49 | 14% |
| You became sick | 41 | 15% | 18 | 6% | 54 | 20% |
| Lifetime Trauma(a) | ||||||
| Family/Friend arrested or killed pre-migration | 17 | 7% | 14 | 7% | 28 | 11% |
| Victim of a natural disaster | 8 | 5% | 25 | 13% | 31 | 15% |
| Victim of war or terrorism | <5 | <1% | 16 | 7% | 16 | 7% |
| Victim of crime or violence | 15 | 4% | 49 | 17% | 61 | 20% |
| Victim of injury/illness during migration | 62 | 21% | 30 | 7% | 80 | 26% |
| Traumatic Experiences (Overall) | ||||||
| Any Traumtic Experience | 80 | 29% | 89 | 34% | 136 | 50% |
| Any Trauma (excluding injury/illness) | 33 | 12% | 72 | 30% | 94 | 35% |
| Any Pre-Migration Experience | 22 | 9% | 27 | 11% | 43 | 16% |
| Any During Migration Experience | 68 | 23% | 47 | 11% | 98 | 31% |
| PTSD Symptoms (Adolescents, N=277) | ||||||
| ALL: PTS T-score ≥ 60 (raw mean=5.20, se=.33) | 15 | 4% | - | - | - | - |
| ANY TRAUMA (N=79): PTS T-score >= 60 | 6 | 9% | - | - | - | - |
| NO TRAUMA (N=198): PTS T-score >= 60 | 9 | 2% | - | - | - | - |
| PTSD Symptoms (Parents Expriencing Trauma, N=89) | ||||||
| PTSD Any Symptoms (mean=4.69, se=1.13) | - | - | 31 | 52% | - | - |
| At Risk for PTSD | - | - | 13 | 21% | - | - |
Note: percentages and means are weighted, cell sizes less than 5 are not reported
Includes trauma experiences after migration for caregivers (but not adolescents).
Many more caregivers than youth characterized their migration experience as “very stressful” (47% vs. 22%). Several (11%) had been a victim of a natural disaster, had had a family member arrested or killed, or had experienced war or terrorism in the year prior to immigrating to the US. Additionally, 11% had been robbed, physically attacked, or accidentally injured, or had become ill during their migration journey. At the time that we interviewed them, 17% of parents reported having been a victim of crime or violence during their lifetimes; 13% reported living through a natural disaster; and 7% reported experiencing a war or act of terrorism. Overall, 34% of parents had had at least one traumatic migration-related experience in their lifetimes.
Although high percentages of youth and their parents reported traumatic experiences, they did not report frequent traumatic symptoms (Table 2). On average, youth had an average raw PTSD score of 5.2 and only 4% of the sample had sub- or clinical frequencies of PTSD symptoms. Among those adolescents who experienced trauma, the prevalence of sub- or clinical PTSD symptoms was significantly higher than those who had not experienced trauma (9% vs. 2%, p<.05). Moreover, frequencies of sub- or clinical PTSD symptoms co-occurred with parents’ PTSD. Fourteen percent of the youth at risk for PTSD also had parents at risk for PTSD; whereas only 7% of youth at low risk for PTSD had parents with PTSD. Youth at risk for PTSD also had higher rates of depression (28% vs. 5%, p<.05) and anxiety (67% vs. 29%, p<.05) than those at lower risk of PTSD.
Only parents who reported a trauma completed survey items about PTSD symptoms. Among these parents (n=89), 52% reported experiencing at least one of 17 symptoms of PTSD a few times a week or almost every day; and a substantial percentage (21%) were considered at risk for PTSD (Table 2). Like their adolescent children, parents at risk for PTSD also reported higher rates of depression than those not at risk (81% vs. 9 %, p<.01).
Associations with Traumatic Events
For both adolescents and parents, we found that extreme poverty and entry without authorization were strongly associated with one another and with the likelihood of experiencing trauma (Table 3). All youth and 98% of parents exposed to extreme poverty prior to migration entered the US without authorization. Compared to those not exposed to extreme poverty, youth exposed to extreme poverty prior to migration had a 4.4 higher odds of experiencing trauma. Compared to those who entered the US with authorization, parents who entered the US without authorization had a 3.1 higher odds of experiencing trauma. Experiences of discrimination and exposure to unsafe neighborhoods with crime, gang, and drug problems further added to parents’ risk of experiencing trauma.
Table 3.
Adjusted Associations with Any Traumatic Experience (Logits)
| Adolescents
|
Parents
|
|||
|---|---|---|---|---|
| OR | [95% CI] | OR | [95% CI] | |
| Pre-Migration Experience | ||||
| Lived in extreme poverty | 4.36 | (1.30 14.57)** | 1.55 | (0.25 9.44) |
| Previous travel to US | 0.49 | (0.15 1.65) | 0.80 | (0.31 2.06) |
| Parent(s) and child separated at least 1 yr | 0.45 | (0.20 1.03)* | - | - - |
| Migration Experience | ||||
| Child aged 6 or less when moved to US | 3.79 | (1.00 14.32)** | - | - - |
| Entered US without authorization | 1.12 | (0.38 3.31) | 3.12 | (1.22 8.00)** |
| Migrated with a family member | 0.93 | (0.28 3.13) | 0.57 | (0.24 1.33) |
| Post-Migration Acculturation | ||||
| Years in the U.S. (range: 0–17) | 0.77 | (0.65 0.91)*** | 1.11 | (1.02 1.21)** |
| Psychological acculturation (range:1–5) | 0.47 | (0.27 0.81)*** | 1.23 | (0.61 2.49) |
| Primarily utilizes Spanish | 0.56 | (0.20 1.56) | 2.11 | (0.86 5.18) |
| Post-Migration Social Environment | ||||
| Ever experienced discrimination | - | - - | 4.05 | (1.65 9.92)*** |
| Neighborhood unsafe | - | - - | 2.36 | (1.00 5.59)* |
| Parent social support (range: 0 – 36) | - | - - | 0.94 | (0.89 0.99)** |
| Parent living with partner | - | - - | 0.36 | (0.14 0.93)** |
| Familism (range: 1–5) | - | - - | 1.00 | (0.48 2.11) |
| Demographic Characteristics | ||||
| Female | 1.04 | (0.46 2.34) | 3.09 | (1.05 9.15)** |
| Age | 1.23 | (0.96 1.58) | 0.99 | (0.94 1.05) |
| Parent(s) completed high school | 0.83 | (0.34 2.04) | 1.26 | (0.54 2.96) |
| Constant | 0.46 | (0.01 31.18) | 0.18 | (0.00 14.41) |
| Model Statistics | ||||
| N | 269 | 259 | ||
| F | 2.22 | 2.18 | ||
p<.10,
p<.05,
p<.01
Note: Data are weighted. Standard errors are adjusted for clustering and stratification of sample.
For children, factors associated with a lower risk of potentially traumatic experiences included higher levels of psychological acculturation, time in the US, older age at migration, and a delayed migration where the child migrated to the US one or more years after their parent. Those factors protecting immigrant parents from potentially traumatic experiences included the presence of a spouse or partner in the household and strong social support systems.
Associations with PTSD Symptoms
As expected, the experience of a potentially traumatic event was associated with an increased risk of PTSD for both immigrant adolescents and their parents (Table 4). In unadjusted models, adolescents who reported any traumatic experience had PTSD symptom scores an average of 31% (1.5 points at the mean) higher than those who reported no trauma. Among parents, trauma experienced prior to migration was associated with an increase of PTSD symptom scores by 160% (i.e. 2.9 points at the mean). After adjusting for other covariates, the influence of traumatic events on PTSD symptom scores declined only slightly to exp(β)=1.29 for adolescents and increased slightly to exp(β)=2.71 for their parents.
Table 4.
Unadjusted and Adjusted Associations with PTSD Symptoms (Negative Binomial Regressions)
| Adolescents
|
Parents
|
|||
|---|---|---|---|---|
| exp(B) | [95% CI] | exp(B) | [95% CI] | |
| Unadjusted Associations | ||||
| Any traumatic experience (a) | 1.31 | (1.00 1.71)** | - | - - |
| Any trauma before migration | 1.11 | (0.74 1.67) | 2.60 | (1.40 4.83)*** |
| Any trauma during migration | 1.40 | (1.06 1.83)** | 1.50 | (0.79 2.16) |
| Adjusted Associations | ||||
| Traumatic Experiences | ||||
| Any traumatic experience | 1.29 | (1.01 1.64)** | - | - - |
| Any trauma before migration | 2.71 | (1.02 7.17)** | ||
| Pre-migration Experience | ||||
| Lived in extreme poverty | - | - - | 1.11 | (0.65 1.90) |
| Previous travel to US | - | - - | 2.92 | (1.21 7.02)** |
| Migration Experience | ||||
| Child aged 6 or less when moved to US | 0.80 | (0.65 0.99)** | - | - - |
| Entered US without authorization | 1.15 | (0.90 1.47) | - | - - |
| Post-Migration Acculturation | ||||
| Psychological Acculturation (range: 1–5) | 1.07 | (0.94 1.21) | - | - - |
| Post-Migration Social Environment | ||||
| Ever experienced discrimination | 1.26 | (1.01 1.57)** | - | - - |
| Neighborhood unsafe | 1.38 | (1.08 1.76)** | - | - - |
| Parent living with partner | 1.12 | (0.86 1.45) | 0.85 | (0.38 1.91) |
| Familism (range: 1–5) | 0.85 | (0.76 0.95)** | 0.74 | (0.46 1.19) |
| Demographic Characteristics | ||||
| Female | 1.20 | (0.96 1.49) | 19.59 | (2.25 171)*** |
| Age | 1.03 | (0.97 1.10) | 1.00 | (0.93 1.07) |
| Parent(s) completed high school | 0.89 | (0.70 1.13) | 1.97 | (0.83 4.65) |
| Constant | 3.69 | (1.25 10.88)** | 0.95 | (0.02 37) |
| Inflate Model | ||||
| Constant Only (a) | - | - - | 1.34 | (0.64 2.05)*** |
| Model Statistics | ||||
| N | 270 | 268 | ||
| Log Likelihood/F-statistic | 4.93 | 10.02 | ||
p<.10,
p<.05,
p<.01
Note: Data are weighted. Standard errors adjusted for clustering and stratification of sample.
PTSD Scores for caregivers only reported by caregivers who had a traumatic experience
In addition to being associated with traumatic experiences, the frequency of PTSD symptoms in adolescents was associated with other migration and post-migration factors (Table 4). Among youth, a lower age at migration and familism were protective and negatively associated with PTSD symptoms. In contrast, ever experiencing discrimination and living in unsafe neighborhoods were associated with an increased risk of PTSD symptoms. Among parents, the frequency of PTSD symptoms was positively associated with poverty prior to migration, previous migration experiences, and female gender. Living with a spouse or partner familism, acculturation (language, psychological or years in the US), discrimination, and living in an unsafe neighborhood were never associated with PTSD symptoms among parents and were ultimately excluded to improve the parsimony of our models.
DISCUSSION
This study is one of the first to comprehensively examine the influence of stressors at various stages of migration on the well-being of immigrant families, and thus represents an important contribution to the literature. Five key results emerge from this research.
First, we found that 34% of Latino immigrant parents and 29% of Latino immigrant adolescents experienced trauma. Among those who experience trauma, 21% of parents and 9% of adolescents are at risk for PTSD. Studies of primarily non-immigrant and non-Hispanic white populations in the US report that as many as 51% of women and 61 % of men and 68% of adolescents in the US have experienced a potentially traumatic event during their lifetimes (Kessler et al., 1995; Copeland et al., 2007). A large portion of these are life-threatening accidents, including traffic accidents, (14–25%), witnessing someone badly injured or killed (14–36%), and in the case of children, hearing about a traumatic event (21%). These are not the types of directly experienced migration-related traumas captured by this study. Nevertheless, the risk of PTSD among those who reported a potentially traumatic event was quite similar in our Latino immigrant sample to the rates of PTSD in these previous studies. Approximately, 20% of women and 3% of adolescents exposed to trauma developed PTSD (Kessler et al., 1995; Copeland et al., 2007). In other words, most individuals experiencing potentially traumatic events do not develop PTSD. The same is true of immigrants. They are resilient and many survive potentially traumatic events without developing PTSD.
Second, we show that factors that contributed to immigrants’ resilience included social support among parents as well as acculturation, time in the US, and familism among children. This has become a nearly ubiquitous finding in the research on mental health among immigrants (Cook, et al., 2009; Perreira and Ornelas, 2011; Kuperminc, et al., 2009). High levels of familism create a safe, nurturing environment for the development of children where they can rely on the protective guidance and emotional support of their parents. Similarly, parents can rely on instrumental and emotional support of their spouses and extended family networks.
Third, our research adds to the wealth of evidence that the context of exit profoundly shapes the health consequences of migration (Portes and Rumbaut 2001; Rumbaut 1991). Most importantly, we show that poverty prior to migration together with entry to the US without authorization were strongly associated with the likelihood of exposures to trauma in both adolescent children and their parents. These findings are not surprising given the dangerous conditions under which many Mexican and Central American immigrants migrate to the US. Those beginning the journey under conditions of financial hardship may also have fewer resources for ensuring a safer trip. Those who migrate to improve their economic situation may continue to struggle with financial hardship after arriving in the US, especially if they are working to send home remittances or pay off debts incurred during migration (Negi, 2011).
Fourth, in contrast to the literature on unaccompanied refugee children (Bronstein and Montgomery, 2011; Ludwig et al., 2004), we find a negative-association between parent-child separation and the likelihood of experiencing a potentially traumatic event. We find a positive association between young age at migration and trauma experiences. In our sample, forced family separations did not occur. Family separations were voluntary and children separated from their parents prior to migration lived with other family members such as a grandparent. At the time that we interviewed them, all children and parents had been re-united with their families. Our results support the hypothesis that parent-child separation reflects a strategy of delayed migration where the parent migrates first and the child follows at a later date and older age. This strategy allows parents to gather the resources needed to ensure a safer passage and reduce the likelihood that their child will experience a potentially traumatic event.
Lastly, our research contributes to understanding how the context of reception influences the health consequences of migration (Portes and Rumbaut 2001; Rumbaut 1991). Both discrimination and neighborhood disorder contributed to the risk of post-migration trauma and the development of PTSD symptoms. These findings are consistent with previous research on the harmful effects of both discrimination and neighborhood disorder on the mental health of both adolescent and adult Latinos (Cook, et al., 2009; Potochnick and Perreira, 2010).
Though our sample of immigrants is primarily Mexican, we expect that similar results would be found among other groups of immigrants characterized by low SES relative to the US population and immigrants who move from countries where they have experienced natural disasters, war, or political violence. Additionally, we expect similar results for other populations who migrate to the US without legal status. Migration-related traumas are likely a common experience not only for refugees but also for many other immigrant populations.
By exclusively focusing on Latino immigrants and asking detailed questions about the full migration process, the Latino Adolescent, Migration, and Adaptation (LAMHA) study provided a unique opportunity to examine how factors before, during, and after migration influence mental health outcomes such as PTSD. At the same time, this study is based on a relatively small, cross-sectional sample with limited power to detect weaker associations and analyze potential modifying effects. Additionally, all retrospective studies of trauma are subject to recall bias and memories of traumatic experiences can sometimes be suppressed or forgotten (Maughan and Rutter, 1997; Raphael, Cloitre, and Dohrenwend, 1991). Those who experience PTSD may also be those most likely to recall trauma, a problem making it difficult to disentangle causal relations in a cross-sectional study. Given the sensitive nature of the topic, respondents may also have chosen not to share some of their experiences with interviewers. We aimed to reduce recall and reporting bias by inquiring about respondents’ experiences at different stages of the migration process and at different points in the interview as interviewers built rapport with respondents.
Finally, data collection for this study took place before the increase in immigration enforcement activities within the interior of the United States. These enforcement activities included Department of Homeland Security (DHS) worksite enforcement actions between 2006–2008, the authorization local law enforcement officers to question noncitizens about their immigration status, and the authorization of local law enforcement officers to detain noncitizens with immigration violations for up to 48 hours (Capps et al., 2007; Chaundry et al., 2010). Each of these activities has resulted in the arrest, detention, and deportation of immigrant parents, mostly fathers, with both foreign-born and US-born children (Wessler, 2012). Such arrests, detentions, and deportations result in the forced and potentially traumatic separation of parents from children (Chaundry et al., 2010; Dreby, 2012; Hagan, Eschbach, Capps 2008). Though the participants in this study did not experience deportations and forced separation, future work should identify and evaluate the consequences of these experiences.
To build upon this analysis and others, future research on the health of immigrant populations and their children must collect more comprehensive and longitudinal data about the migration process and settlement experiences of immigrants. We cannot fully understand the role of migration in health and development without considering how experiences prior to and during migration shape the context of settlement in the US.
Trauma occurs frequently in the lives of immigrant youth and their parents. More than anything else, extreme economic hardship, limited legal means for authorized entry to the US for poorer Mexicans and other Central Americans, and discrimination within the US increase the risk of trauma. These traumatic experiences can result in the development of acute and chronic mental health problems including PTSD, generalized anxiety, and depression. The consequences of poor mental health to parents and their children can be severe and include lower academic achievement among children, reduced employment opportunities and lost wages among parents, and stressful family relations (Eisenman, et al., 2008; Kataoka, et al., 2009; MacMillan, 2001; Porche, et al., 2011). Thus, immigration policy reforms promoting safe and legal migrations and efforts to reduce discrimination and improve the settlement experiences of immigrants can promote their civic engagement in their local communities as well as their health and ability to contribute to the US economy.
Acknowledgments
The LAMHA Project was funded by a grant from the William T. Grant Foundation and directed by Krista M. Perreira and Mimi V. Chapman. This research was also supported by grant, 5 R24 HD050924, Carolina Population Center, awarded to the Carolina Population Center at The University of North Carolina at Chapel Hill by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Persons interested in obtaining LAMHA restricted use data should see http://www.cpc.unc.edu/projects/lamha for further information. The authors would also like to express their appreciation to Paula Gildner for her management of the data collection process; Stephanie Potochnick for her assistance with data cleaning; and all the schools, immigrant families, and adolescents who participated in our research project
Contributor Information
Krista M. Perreira, Department of Public Policy, University of North Carolina, Chapel Hill
India Ornelas, Department of Health Services, University of Washington, Seattle.
References
- Acosta YD, De La Cruz GP. The Foreign Born From Latin America and the Caribbean: 2010. Washington, DC: US Census Bureau; 2011. [Google Scholar]
- Alegría M, et al. Looking Beyond Nativity: The Relation of Age of Immigration, Length of Residence, and Birth Cohorts to the Risk of Onset of Psychiatric Disorders for Latinos. Research on Human Development. 2007;4:19–47. doi: 10.1080/15427600701480980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, et al. Understanding Differences in Past Year Psychiatric Disorders for Latinos Living in the US. Social Science & Medicine. 2007;65:214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, et al. Prevalence of Mental Illness in Immigrant and Non-Immigrant U.S. Groups. American Journal of Psychiatry. 2008;165:359–69. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Bowen GL, Rose RA, Bowen NK. The Reliability and Validity of the School Success Profile. Philadelphia: Xlibris; 2005. [Google Scholar]
- Briere J. Trauma Symptom Checklist for Children, Professional Manual. Lutz, FL: Psychological Assessment Resources, Inc; 1996. [Google Scholar]
- Bronstein I, Montgomery P. Psychological Distress in Refugee Children: A Systematic Review. Clinical Child and Family Psychology Review. 2011;14:44–56. doi: 10.1007/s10567-010-0081-0. [DOI] [PubMed] [Google Scholar]
- Bryant-Davis T, Ocampo C. Racist Incident-Based Trauma. The Counseling Psychologist. 2005;33:479–500. [Google Scholar]
- Cameron AC, Trivedi PK. Regression Analysis of Count Data. Cambridge: Cambridge University Press; 1998. [Google Scholar]
- Capps R, Chaudry A, Castañeda RM, Santos R. Paying the Price: The Impact of Immigration Raids on America’s Children. Washington, DC: The Urban Institute; 2007. http://www.urban.org/UploadedPDF/411566_immigration_raids.pdf. [Google Scholar]
- Cervantes R, Fisher D, Cordova D, Napper L. The Hispanic Stress Inventory-Adolescent Version: A Culturally Informed Psychosocial Assessment. Psychological Assessment. 2012;24(1):187–196. doi: 10.1037/a0025280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervantes R, Salgado De Snyder V, Padilla A. Posttraumatic Stress in Immigrants from Central America and Mexico. Hospital & Community Psychiatry. 1989;40:615–619. doi: 10.1176/ps.40.6.615. [DOI] [PubMed] [Google Scholar]
- Charles CZ. Won’t You Be My Neighbor? NY, NY: Russel Sage Foundation; 2006. [Google Scholar]
- Chaudry A, Capps R, Pedroza JM, Castañeda RM, Santos R, Scott MM. Facing Our Future: Children in the Aftermath of Immigration Enforcement. Washington, DC: The Urban Institute; 2010. http://www.urban.org/UploadedPDF/412020_FacingOurFuture_final.pdf. [Google Scholar]
- Cohen S, Wills T. Stress, Social Support, and the Buffering Hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Consejo Nacional De Evaluación De La Política De Desarrollo Social (CONEVAL) [Accessed on January 8, 2011];Metodología Para La Medición Multidimensional De La Pobreza En México. 2010 < www.coneval.gob.mx/coneval2/htmls/medicion_pobreza/homemedicionpobreza.jsp>.
- Cook B, Alegria M, Lin JY, Guo J. Pathways and Correlates Connecting Latinos’ Mental Health with Exposure to the United States. American Journal of Public Health. 2009;99:2247–2254. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic Events and Posttraumatic Stress in Childhood. Archives of General Psychiatry. 2007;64(5):577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Debellis MD, Van Dillen T. Childhood Post-Traumatic Stress Disorder: An Overview. Child and Adolescent Psychiatric Clinics of North America. 2005;14:745–772. doi: 10.1016/j.chc.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Deluca LA, Mcewen MM, Keim SM. United States-Mexico Border Crossing: Experiences and Risk Perceptions of Undocumented Male Immigrants. Journal of Immigrant and Minority Health. 2010;12:113–123. doi: 10.1007/s10903-008-9197-4. [DOI] [PubMed] [Google Scholar]
- Donato KM. U.S. Migration from Latin America: Gendered Patterns and Shifts. The ANNALS of the American Academy of Political and Social Science. 2010;630:78–92. doi: 10.1177/0002716210368101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donato KM, Armenta A. What Do We Know About Undocumented Migration. Annual Review of Sociology. 2011;37:529–43. [Google Scholar]
- Dreby J. The Burden of Deportation on Children in Mexican Immigrant Families. Journal of Family and Marriage. 2012;74(4):828–845. [Google Scholar]
- Eisenman DP, et al. PTSD in Latino Patients: Illness Beliefs, Treatment Preferences, and Implications for Care. Journal of General Internal Medicine. 2008;23:1386–1392. doi: 10.1007/s11606-008-0677-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenman DP, Gelber L, Liu H, Shapiro MF. Mental Health and Health-Related Quality of Life among Adult Latino Primary Care Patients Living in The United States With Previous Exposure To Political Violence. Journal of the American Medical Association. 2003;290:627–34. doi: 10.1001/jama.290.5.627. [DOI] [PubMed] [Google Scholar]
- Escobar JI, et al. Posttraumatic Stress Disorder in Hispanic Vietnam Veterans: Clinical Phenomenology and Sociocultural Characteristics. Journal of Nervous and Mental Disease. 1983;171:585–596. doi: 10.1097/00005053-198310000-00001. [DOI] [PubMed] [Google Scholar]
- Falsetti SA, et al. The Modified PTSD Symptom Scale: A Brief Self-Report Measure of Posttraumatic Stress Disorder. Behavioral Assessment Review. 1993 Jun;:161–162. [Google Scholar]
- Finch BK, Do P, Seeman T, Frank R. Could ‘Acculturation’ Effects Be Explained By Latent Health Disadvantages Among Mexican Immigrants? International Migration Review. 2009;43:471–495. [Google Scholar]
- Flores E, et al. Perceived Racial/Ethnic Discrimination, Posttraumatic Stress Symptoms, and Health Risk Behaviors Among Mexican American Adolescents. Journal of Counseling Psychology. 2010;57:264–73. doi: 10.1037/a0020026. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and Validity of A Brief Instrument for Assessing Posttraumatic Stress Disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Fortuna LR, Porche MV, Alegria M. Political Violence, Psychosocial Trauma, and The Context of Mental Health Services Use Among Immigrant Latinos in The United States. Ethnicity and Health. 2008;13:435–463. doi: 10.1080/13557850701837286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuny K. Children of Immigrants: 2008 State Trends Update. Washington, DC: Urban Institute; 2010. [Accessed on April 3, 2011]. < Http://Www.Urban.Org/Uploadedpdf/412212-Children-of-Immigrants.Pdf>. [Google Scholar]
- Fuligni AJ, Pedersen S. Family Obligation and The Transition to Young Adulthood. Developmental Psychology. 2002;38:856–68. doi: 10.1037//0012-1649.38.5.856. [DOI] [PubMed] [Google Scholar]
- García-Coll C, et al. An Integrative Model for the Study of Developmental Competencies in Minority Children. Child Development. 1996;(67):1891–1914. [PubMed] [Google Scholar]
- Garcia-Coll C, Magnuson K. The Psychological Experience of Immigration: A Developmental Perspective. In: Landale N, editor. Immigration and the Family: Research and Policy on US Immigrants. Hillsdale, NJ: Erlbaum; 1997. pp. 91–131. [Google Scholar]
- Gil A, Vega W. Two Different Worlds: Acculturation Stress and Adaptation among Cuban and Nicaraguan Families. Journal of Social and Personal Relationships. 1996;13:435–456. [Google Scholar]
- Gonzales N, Fabrett F, Knight G. Acculturation, Enculturation and the Psychological Adaptation of Latino Youth. In: Villarruel F, et al., editors. Handbook of U.S. Latino Psychology: Developmental and Community-Based Perspectives. Thousand Oaks (CA): Sage Publications; 2009. pp. 115–134. [Google Scholar]
- Greene WH. Econometric Analysis. 6. Upper Saddle River (NJ): Prentice Hall, Inc; 2008. [Google Scholar]
- Hagan J, Eschbach K, Rodriguez N. U.S. Deportation Policy, Family Separation, and Circular Migration. International Migration Review. 2008;24(1):64–88. [Google Scholar]
- Heilmann MV, Kury FS, Lee KA. Trauma and Posttraumatic Stress Disorder Symptoms among Low Income Women of Mexican Descent in the United States. Journal of Nervous and Mental Disease. 2005;193:665–672. doi: 10.1097/01.nmd.0000180741.93635.ab. [DOI] [PubMed] [Google Scholar]
- Infante C, et al. Violence Committed Against Migrants in Transit: Experiences on the Northern Mexican Border. [Accessed April 15, 2012];Journal of Immigrant and Minority Health. 2011 doi: 10.1007/S10903-011-9489-Y. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, et al. Violence Exposure, Posttraumatic Stress Disorder, and Depressive Symptoms Among Recent Immigrant School Children. Journal of The Amercian Academy of Child and Adolescent Psychiatry. 2002;41:1104–1110. doi: 10.1097/00004583-200209000-00011. [DOI] [PubMed] [Google Scholar]
- Johnson H, Thompson A. The Development and Maintenance of Post-Traumatic Stress Disorder (PTSD) in Civilian Adult Survivors of War Trauma and Torture: A Review. Clinical Psychology Review. 2008;28(1):36–47. doi: 10.1016/j.cpr.2007.01.017. [DOI] [PubMed] [Google Scholar]
- Kataoka S, et al. Violence Exposure and PTSD: The Role of English Language Fluency in Latino Youth. Journal of Child and Family Studies. 2009;18:334–341. [Google Scholar]
- Kessler RC, et al. Posttraumatic Stress Disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- King EN, Ryan TP. A Preliminary Investigation of Maximum Likelihood Logistic Regression versus Exact Logistic Regression. The American Statistician. 2002;56:163–170. [Google Scholar]
- Kovacs M. The Children’s Depression Inventory. North Towanda (NY): Multi-Health Systems Inc; 1992. [Google Scholar]
- Kuperminc G, Wilkins N, Roche C, Alvarez-Jimenez A. Risk, Resilience, and Positive Development among Latino Youth. In: Villaruel F, et al., editors. Handbook of U.S. Latino Psychology. Los Angeles: Sage; 2009. pp. 213–234. [Google Scholar]
- Lustig SL, et al. Review of Child and Adolescent Refugee Mental Health. Journal of The American Academy of Child and Adolescent Psychiatry. 2004;43:25–36. doi: 10.1097/00004583-200401000-00012. [DOI] [PubMed] [Google Scholar]
- Macmillan R. Violence and The Life Course. The Consequence of Victimization for Personal and Social Development. Annual Review of Sociology. 2001;27:1–22. [Google Scholar]
- Makley AT, Falcone RA., Jr Posttraumatic Stress Disorder in the Pediatric Trauma Patient. Seminars in Pediatratic Surgery. 2010;19:292–299. doi: 10.1053/j.sempedsurg.2010.06.006. [DOI] [PubMed] [Google Scholar]
- March JS, et al. The Multidimensional Anxiety Scale for Children (MASC): Factor Structure, Reliability and Validity. Journal of American Academy of Child and Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Marin G, et al. Development of a Short Acculturation Scale for Hispanics. Hispanic Journal of Behavioral Science. 1987;9:183–205. [Google Scholar]
- Marshall GN, Orlando M. Acculturation and Peritraumatic Dissociation in Young Adult Latino Survivors of Community Violence. Journal of Abnormal Psychology. 2002;111:166–174. doi: 10.1037//0021-843x.111.1.166. [DOI] [PubMed] [Google Scholar]
- Marshall G, Schell TL, Miles JNV. Ethnic Differences in Posttraumatic Distress: Hispanics’ Symptoms Differ in Kind and Degree. Journal of Consulting and Clinical Psychology. 2009;77:1169–1178. doi: 10.1037/a0017721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey D, Espinosa K. What’s Driving Mexico-US Migration? A Theoretical, Empirical, and Policy Analysis. American Journal of Sociology. 1997;102:939–99. [Google Scholar]
- Massey D, Durand J, Malone NJ. Beyond Smoke and Mirrors: Mexican Immigration in An Era of Economic Integration. New York: Russell Sage Foundation; 2009. [Google Scholar]
- Masten AS, Narayan AJ. Child Development in the Context of Disaster, War, and Terrorism: Pathways of Risk and Resilience. Annual Review of Psychology. 2012;63:227–57. doi: 10.1146/annurev-psych-120710-100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan B, Rutter M. Retrospective reporting of childhood adversity: issues in assessing long-term recall. Journal of Personal Disorder. 1997;11:19–33. doi: 10.1521/pedi.1997.11.1.19. [DOI] [PubMed] [Google Scholar]
- Mehta CR, Patel NR. Exact Logistic Regression: Theory and Examples. Statistics in Medicine. 1995;14:2143–2160. doi: 10.1002/sim.4780141908. [DOI] [PubMed] [Google Scholar]
- Negi NJ. Identifying Psychosocial Stressors of Well-Being and Factors Related To Substance Use among Latino Day Laborers. Journal of Immigrant and Minority Health. 2011;13:748–755. doi: 10.1007/s10903-010-9413-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orfield G, Lee C. Why Segregation Matters: Poverty and Educational Inequality. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Ornelas IJ, Perreira K. The Role of Migration in The Development of Depressive Symptoms Among Latino Immigrant Parents in The USA. Social Science & Medicine. 2011;73:1169–1177. doi: 10.1016/j.socscimed.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oropesa RS. Neighborhood Disorder and Social Cohesiveness among Immigrants in a New Destination: Dominicans in Reading, PA. Urban Studies. 2012;49:115–132. doi: 10.1177/0042098011403014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega AN, Rosenheck R. Posttraumatic Stress Disorder among Hispanic Vietnam Veterans. American Journal of Psychiatry. 2000;157:615–619. doi: 10.1176/appi.ajp.157.4.615. [DOI] [PubMed] [Google Scholar]
- Perreira KM, I, Ornelas J. The Physical and Psychological Well-Being of Immigrant Children. The Future of Children. 2011;21:195–218. doi: 10.1353/foc.2011.0002. [DOI] [PubMed] [Google Scholar]
- Pole N, Gone JP, Kulkarni M. Posttraumatic Stress Disorder among Ethnoracial Minorities in the United States. Clinical Psychology Scientific Practice. 2008;15:35–61. [Google Scholar]
- Pole N, Best SR, Metzler T, Marmar CR. Why Are Hispanics at Greater Risk for PTSD? Cultural Diversity and Ethnic Minority Psychology. 2005;11:144–161. doi: 10.1037/1099-9809.11.2.144. [DOI] [PubMed] [Google Scholar]
- Porche MV, Fortuna LR, Lin J, Alegria M. Childhood Trauma and Psychiatric Disorders as Correlates of School Dropout in a National Sample of Young Adults. Child Development. 2011;82:982–998. doi: 10.1111/j.1467-8624.2010.01534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portes A, Rumbaut R. Legacies: The Story of the Immigrant Second Generation. New York, NY: Russell Sage Foundation; 2001. [Google Scholar]
- Potochnick S, Perreira K. Depression and Anxiety among First-Generation Immigrant Latino Youth: Key Correlates and Implications for Future Research. Journal of Nervous and Mental Disease. 2010;198:470–477. doi: 10.1097/NMD.0b013e3181e4ce24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychology Measures. 1977;1:385–401. [Google Scholar]
- Raphael KG, Cloitre M, Dohrenwend BP. Problems of recall and misclassification with checklist methods of measuring stressful life events. Health Psychology. 1991;10:62–74. doi: 10.1037//0278-6133.10.1.62. [DOI] [PubMed] [Google Scholar]
- Rasmussen A, Rosenfeld B, Reeves K, Keller AS. The Subjective Experience of Trauma and Subsequent PTSD in a Sample of Undocumented Immigrants. Journal of Nervous and Mental Disease. 2007;195:137–143. doi: 10.1097/01.nmd.0000254748.38784.2f. [DOI] [PubMed] [Google Scholar]
- Riosmena F, Massey D. Pathways to El Norte: Origins, Destinations, and Characteristics of Mexican Migrants to The United States. International Migration Review. 2012;46:3–36. doi: 10.1111/j.1747-7379.2012.00879.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, et al. Race/Ethnic Differences in Exposure to Traumatic Events, Development of Post-Traumatic Stress Disorder, and Treatment-Seeking for Post-Traumatic Stress Disorder in the United States. Psychological Medicine. 2011;41:71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumbaut RG. The Agony of Exile: A Study of The Migration and Adaptation of Indochinese Refugee Adults and Children. In: Athey JL, editor. Refugee Children: Theory Research, and Services. Baltimore: Johns Hopkins Press; 1991. pp. 53–91. [Google Scholar]
- Santa-Maria ML, Cornille T. Traumatic Stress, Family Separations, and Attachment among Latin American Immigrants. Traumatology. 2007;13:26–31. [Google Scholar]
- Steel Z, et al. Association of Tortures and Other Potentially Traumatic Events With Mental Health Outcomes Among Populations Exposed to Mass Conflict and Displacement. Journal of the American Medical Association. 2009;302:537–548. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- Suárez-Orozco C, Qin DB. Gendered Perspectives in Psychology: Immigrant Origin Youth. International Migration Review. 2006;40:165–198. [Google Scholar]
- Suárez-Orozco C, Todorova I, Louie J. “Making up for lost time”: The experience of separation and reunification among immigrant families. Family Process. 2002;41:625–643. doi: 10.1111/j.1545-5300.2002.00625.x. [DOI] [PubMed] [Google Scholar]
- Tropp LR, Coll CG, Alarcon O, Vazquez Garcia HA. Psychological Acculturation: Development of a New Measure for Puerto Ricans on The U.S. Mainland. Educational and Psychological Measurement. 1999;59:351–367. doi: 10.1177/00131649921969794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census. 2010 American Community Survey 1-Year Estimates. Washington, DC: US Census Bureau; 2010. Selected Characteristics of The Native and Foreign-Born Populations, S0501. [Google Scholar]
- Vega WA, Sribney W, Aguilar-Gaxiola S, Kolody B. 12-Month Prevalence of DSM-III-R Psychiatric Disorders among Mexican Americans: Nativity, Social Assimilation, and Age Determinants. Journal of Nervous and Mental Disease. 2004;192:532–54. doi: 10.1097/01.nmd.0000135477.57357.b2. [DOI] [PubMed] [Google Scholar]
- Wessler S. Colorlines. New York: Applied Research Center; 2012. Dec 17, Nearly 205K Deportations of Parents of U.S. Citizens in Just Over Two Years. http://colorlines.com/archives/2012/12/us_deports_more_than_200k_parents.html.1. [Google Scholar]
- Yule W. Post-Traumatic Stress Disorder in Children and Adolescents. International Review of Psychiatry. 2001;13:194–200. [Google Scholar]