A 60-year-old man presented to the emergency department with a chief complaint of shortness of breath and lower extremity edema for approximately 1 month. On further interview, the patient reported intermittent claudication progressing to the point he could not climb a flight of stairs. His only other history was a remote abdominal stab wound suffered some 30 years prior. On examination, his blood pressure was noted to be 210/110 mm Hg. He had 1 + edema of the ankles and crackles in bibasilar lung fields. Serum creatinine was 1.9 mg/dl and rose to >4 mg/dl during admission requiring five antihypertensive agents. A search for causes of secondary hypertension revealed elevated urine catecholamines prompting abdominal imaging (Figures 1 and 2).
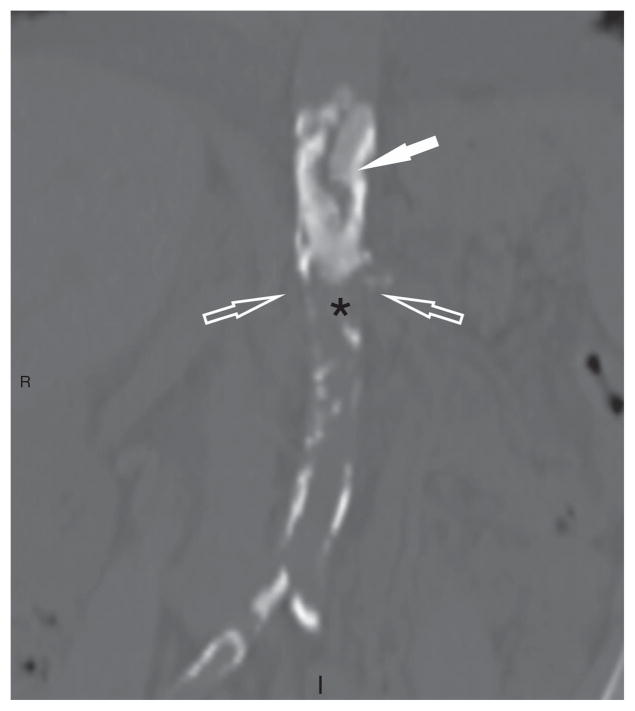
Figure 1.
Noncontrasted coronal computerized axial tomography scan in bone algorithm that demonstrates dense calcification of the thoracic aorta in a ‘coral reef’ pattern (solid white arrow, calcified aorta; asterisk, aortic lumen).
Figure 2.
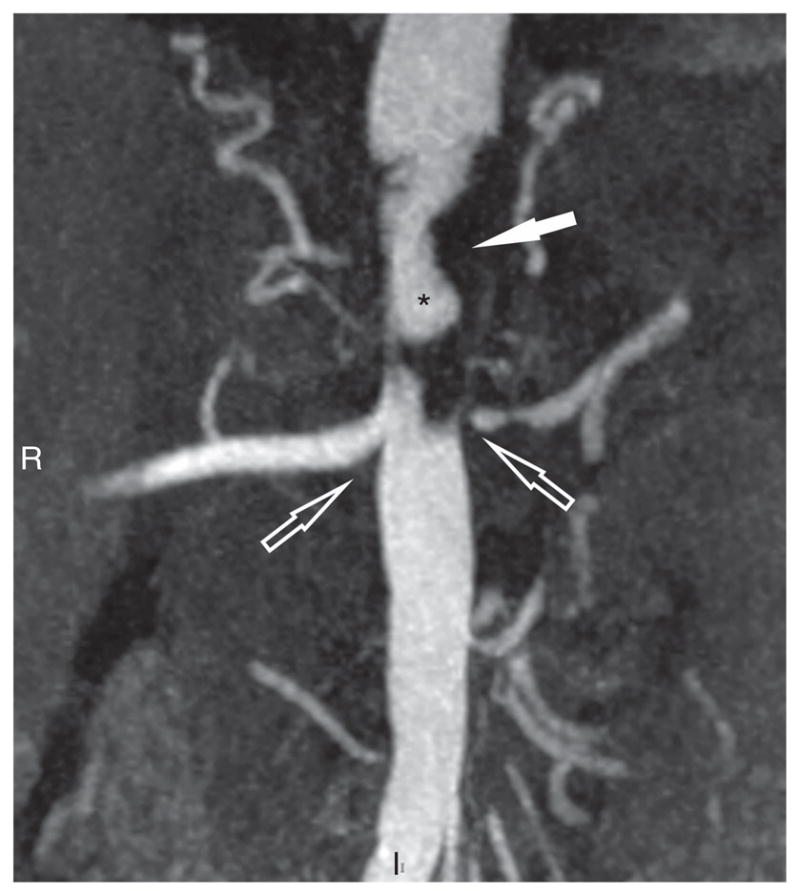
Coronal contrast enhanced magnetic resonance angiogram that demonstrates irregular hypointense T1 signal representing aortic calcifications (solid white arrow) of the suprarenal abdominal aorta (asterisk, aortic lumen), resulting in severe left renal artery ostial stenosis (hollow white arrow).
Coral reef aorta is a rare disease of unknown etiology involving calcifications arising from the dorsal aorta, typically involving the abdominal aorta from the level of the diaphragm. The most common presenting symptoms in case series are renovascular hypertension and claudication, both of which our patient experienced. Qvarfordt et al. first coined the term in 1984, given the appearance on computerized tomography scan approximating a coral reef. The most common treatment is thromboendarterectomy, which frequently necessitates reconstruction of one or both renal arteries. Our patient underwent thromboendarterectomy and after a brief period of hemodialysis has remained dialysis independent.