Abstract
Purpose
To test the fit of a theoretically driven conceptual model of pathways to STI risk among foster youth transitioning to adulthood. The model included: 1) historical abuse and foster care experiences, 2) mental health and attachment style in late adolescence, and 3) STI risk in young adulthood.
Methods
We used path analysis to analyze data from a longitudinal study of 732 youth transitioning out of foster care. Covariates included gender, race and an inverse probability weight. We also performed moderation analyses comparing models constrained and unconstrained by gender.
Results
Thirty percent reported they or a partner had been diagnosed with an STI. Probability of other measured STI risk behaviors ranged from 9% (having sex for money) to 79% (inconsistent condom use). Overall model fit was good (Standardized Root Mean Squared Residual of 0.026). Increased risk of oppositional/delinquent behaviors mediated an association between abuse history and STI risk, via increased inconsistent condom use. There was also a borderline association with having greater than 5 partners. Having a very close relationship with a caregiver and remaining in foster care beyond age 18 decreased STI risk. Moderation analysis revealed better model fit when coefficients were allowed to vary by gender versus a constrained model, but few significant differences in individual path coefficients were found between male and female-only models.
Conclusions
Interventions/policies that: 1) address externalizing trauma sequelae, 2) promote close, stable substitute caregiver relationships, and 3) extend care to age 21 years have the potential to decrease STI risk in this population.
INTRODUCTION
Young adults who age out of foster care report poorer overall health and higher rates of physical and mental health problems compared with young adults in the general population;1-4 however they remain underrepresented in health research.5 Sexual risk behaviors are of particular importance for this population. During adolescence and emerging adulthood, foster youth report higher rates of early sexual intercourse,6-9 higher numbers of partners,6,7 and are more likely to report having sex for drugs or money,2,6 having sex with a casual partner,6 and/or having a partner who has had a sexually transmitted infection (STI).2,3 Consequently, as young adults they are estimated to have between 3-14 times the risk of a biologically diagnosed STI compared with general population youth.6 STIs are known to have significant health and economic impacts,10 and related behaviors also put foster youth at higher risk of other undesirable outcomes such as teen pregnancy.2,3
Several factors may contribute to this group's STI risk. Many foster youth are exposed to childhood physical and/or sexual abuse;4,11,12 this puts them at increased risk of maladaptive “attachment” or relationships style later in life.13,14 In addition, many youth in foster care engage in oppositional and delinquent behaviors, and/or suffer from substance use and mental health disorders such as depression and post-traumatic stress disorder (PTSD).4 These problems have been associated with increased risk of STIs and related sexual behaviors in other populations.11,12,15-17
The types (non-relative, group, kinship) and/or number of placements that youth experience while in foster care may also impact this group's participation in sexual risk behaviors, via their effect on mental health or attachment style. For example, youth who experience multiple placement changes may be may be at increased STI risk because they are less likely to develop the types of meaningful connections with foster caregivers or other adults that can promote healthy relationship behaviors, and they also tend to have greater mental and other health problems. Conversely, youth in stable placements who are able to develop loving and healthy relationships with caregivers or other adults may have more stable attachment styles, lower rates of mental health problems, and lower STI risk.3,16,18-21
Finally, although recent federal legislation provides an incentive for states to extend foster care to age 21,22 youth in most states continue to be emancipated at age 18.4 Consequently, many foster youth find themselves without formalized adult support during the age at which sexual and other health risk behaviors peak.23
Little is known about how to decrease STI risk among foster youth. Extant studies evaluating STI preventive interventions in foster youth have tended to be uncontrolled or have failed show long-term positive impacts.24-26 Additional research is needed to better understand pathways to STI risk as well as factors promoting resiliency among youth in foster care, to inform the development of effective preventive interventions and policies.
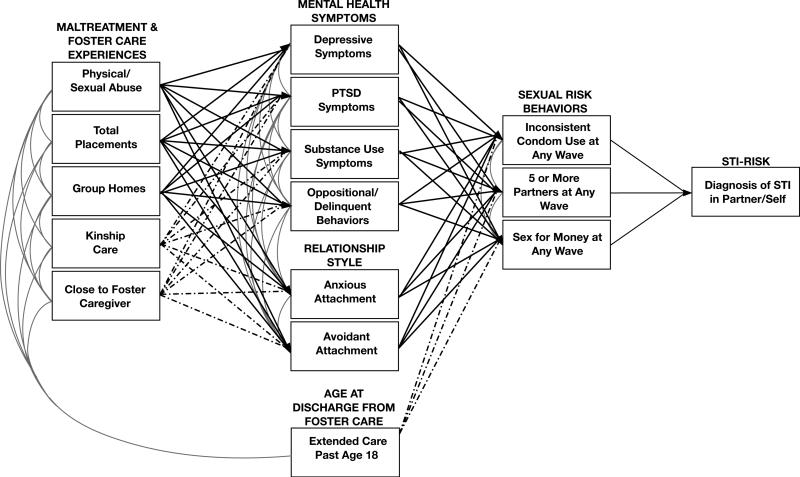
The main objectives of this study were to: 1) test the overall fit of a conceptual model for STI risk among female and male foster youth that included maltreatment and foster care experiences as well as late adolescent psychosocial factors associated with STI risk in other populations, 2) identify key pathways leading to STI risk, and 3) identify potential protective factors to inform future intervention development efforts. We hypothesized that a history of physical/sexual abuse and multiple total and group placements while in foster care would be associated with an increased risk of both mental health symptoms and maladaptive relationship style during late adolescence, and that these factors would, in turn, be associated with self-reported sexual risk behaviors and STI exposure in young adulthood. We also hypothesized that being in kinship care, having a close relationship with a foster caregiver, and remaining in care past age 18 would be associated with decreased risk of STI (Figure 1).
Figure 1.
Initial conceptual model of abuse and foster care experiences, hypothesized late adolescent psychosocial mediators, and STI risk in young adulthood for youth in foster care.
 hypothesized STI risk path
hypothesized STI risk path
 hypothesized STI protective paths
hypothesized STI protective paths
 hypothesized covariance between two variables at same time point
hypothesized covariance between two variables at same time point
METHODS
Study Design and Sample
Data were drawn from Waves 1-5 of the Midwest Evaluation of the Adult Functioning of Former Foster Youth, a longitudinal cohort study of youth in Illinois, Iowa and Wisconsin transitioning out of foster care.1-4 Youth were eligible for the study if they were in out-of-home care at age 17, and had been in out-of-home care for ≥1 year prior to recruitment. Exclusion criteria included being in a psychiatric or correctional facility, on runaway status during the entire baseline field period, or having a disability that would prevent completion of the survey. Seven hundred thirty two (732) of the 770 youth identified as eligible consented to participate and completed an in-person baseline interview (95% response rate). Participants were 17-18 years old and 52% were female. The racial composition of the sample was: 57% African-American, 31% Caucasian, and 12% “other.” Waves 2-5 were conducted when participants were 19, 21, 23-24, and 26 years old, and response rates were 81-82%.
Data Collection Procedures
All Wave 1 and most Wave 2-5 interviews were conducted in person. Audio computer-assisted self-interviewing (ACASI) techniques were used for questions about sexual behaviors and other sensitive subjects; these questions were omitted for phone interviews. Human subjects’ approval and informed consent were obtained before all interviews for the original study. The present analyses were determined exempt for human subjects review, as all data were de-identified.
Variables
Past Sexual or Physical Abuse Experiences (Y/N)
Data were combined from several sources to produce a dichotomous variable reflecting participants’ past histories of childhood abuse exposure: 2 questions regarding sexual abuse from the World Health Organization's Composite International Diagnostic Interview (“CIDI”) administered at Wave 1, 7 questions regarding sexual abuse from the National Survey of Adolescents in the United States administered at Wave 2 (restricted to events occurring prior to baseline);27,28 and 7 questions regarding past exposures to physical abuse perpetrated by biological caregivers (assessed at Wave 1) and/or foster caregivers (assessed at Wave 2), taken from the Lifetime Experiences Questionnaire.29
Total number of placements (Continuous)
We summed the self-reported number of foster home (>20 coded as “21”) and group care (>20 placements coded as “21”) placements prior to baseline (Wave 1). Sum was log transformed due to skewed distribution.
Number of group care placements (0, 1, 2, >2)
We created a categorical variable reflecting the number of group care placements participants had experienced prior to Wave 1.
Close to foster caregiver (Y/N)
Participants reported whether they felt “very close” to a current caregiver at Wave 1.
Kinship care (Y/N)
Participants reported whether any of foster caregivers had ever been relatives by Wave 1.
Extended Care (Y/N)
We used administrative data provided by the state child welfare agencies to categorize youth based on whether they remained in foster care beyond age 18. At the time of data collection, Illinois foster youth routinely remained in foster care until age 21 whereas foster youth are in Iowa and Wisconsin were typically discharged at age 18.
Depressive, PTSD, and Substance-Related Symptoms (Y/N)
We used questions from the Wave I CIDI27 to create variables reflecting whether participants had recent (i.e., after age 16) symptoms of the following disorders: depression, PTSD, and alcohol or drug abuse or dependence. All symptom criteria were based on definitions from the Diagnostic and Statistical Manual – IV.30 The depression variable was coded as “Yes” if a participant reported experiencing 5 or more depressive symptoms; PTSD was coded “Yes” if any symptoms lasting more than a month were reported, and the substance-related variable was coded as “Yes” if a participant reported any drug or alcohol-related symptoms.
Oppositional/Delinquent Behaviors (Continuous, Z-scored)
We generated a sum of 15 items from the National Longitudinal Study of Adolescent Health31 administered at Wave 1 regarding oppositional/delinquent behaviors (Cronbach's alpha = 0.82); we then standardized (z-scored) this measure for the main analyses. Examples of behaviors assessed included property damage, theft, physical violence, and the sale of illicit drugs. None of the items related to sexual behaviors (i.e., prostitution), or drug/alcohol use.
Anxious and Avoidant Attachment (Continuous, Z-scored)
We used selected Likert-type items from the anxious (11/18) and avoidant (11/18) subscales of the Experiences in Close Relationships-Revised instrument administered at Wave 1 to create two measures of relationship style.32 Questions on the anxious subscale measured anxiety in close relationships (e.g., “I worry a lot about my relationships”). Questions on the avoidant subscale measured avoidance of intimacy in close relationships (e.g., “I find it difficult to allow myself to depend on others”). Cronbach's alphas were 0.86 and 0.77, respectively. Items on each scale were coded such that a higher score correlated with more anxiety or avoidance, and were then averaged. Scores on both measures were standardized (z-scored) for the main analyses.
STI-related outcomes
We created dichotomous (Y/N) variables for Waves 2-5 for each STI-related outcome. A small proportion of youth reported never having had intercourse at each outcome wave (13%, 5%, 5%, and 4% at Waves 2, 3, 4, and 5, respectively); these youth were coded as “No” for all outcomes at a given wave.
Inconsistent Condom Use at Any Wave (Y/N)
Participants were coded as having engaged in inconsistent condom use if they reported anything but “all of the time” to a question about the frequency of condom use in the past year (none/some/half/most/all of the time) and/or reported that they had not used a condom the last time they had sexual intercourse (Y/N) at any wave. Youth who reported no sexual partners in the past year were coded as “No”.
Five or More Partners in the Past Year at Any Wave (Y/N)
At each wave, participants reported the total number of sexual partners they had had in the past year. Participants were coded as ”Yes” for this variable if they had had 5 or more partners at any wave. Youth reporting no sexual partners in the past year were coded as “No”.
Sex for Money in Past Year at Any Wave (Y/N)
At each wave, participants reported whether they had ever had sex “with someone who paid you to do so” and whether they had done so in the past 12 months. Participants were coded as “Yes” if they reported having had sex for money in the past year at any wave.
Diagnosis of STI in Partner or Self (Y/N)
At Waves 2-5, all participants with at least one sexual partner in the past year were asked to report whether any of these partners had had an STI. At Wave 5 participants were also asked if they had ever been told by a doctor, nurse, or other health professional that they had any of the following: Chlamydia, gonorrhea, syphilis, genital herpes, genital warts, Human Papilloma Virus, pelvic inflammatory disease, cervicitis or mucopurulent cervicitis, urethritis, HIV Infection or AIDS, or “any other sexually transmitted disease”. Participants were coded as “Yes” if they reported having had a partner with an STI at any wave (with youth who reported having no sexual partners in the past year coded as “No” for a given wave) or if they had been personally diagnosed with an STI.
Covariates
Covariates included gender and race (African American versus other).
Analyses
The data were analyzed using Stata SE, version 12.33 We computed means and standard deviations for each variable using the whole sample, and after stratifying by gender and race. We also performed bivariate regression to assess associations between study variables and each covariate. We then computed unadjusted pairwise correlations among study variables. For our main analysis, we performed path analysis, a form of Structural Equation Modeling (SEM) using robust standard errors and the “MLMV” (maximum likelihood with missing values) approach.34,35 We included covariates as well as an inverse probability weight reflecting the number of follow-up waves of participation, as this has been shown to improve the accuracy of point estimates in longitudinal studies.36 We computed model fit statistics including the “Standardized Root Mean Squared Residual” (SRMR) index and the Coefficient of Determination (CD) in order to test the overall goodness of fit the conceptual model in Figure 1; other fit statistics were not available due to statistical package limitations when an MLMV approach is used. We also assessed significance of individual paths leading to STI risk. As exploratory analyses, we performed moderation analyses comparing models with path coefficients constrained and unconstrained by gender. We used the Chi-square difference test (excluding weights due to statistical software limitations) to test moderation by gender of the overall model.37 We then assessed differences in specific paths in the male and female-only models (with weights included). Finally, we performed several supplemental analyses to test the sensitivity of our results to decisions regarding certain study variable definitions. For example, in our main analyses we were not able to restrict our abuse variable to include only physical abuse events perpetrated by foster caregivers prior to age 17 (though we were able to do this for sexual abuse events and physical abuse events perpetrated by biological family members); thus it is theoretically possible that some youth who were coded as “Yes” for the dichotomized abuse variable may have their first and only physical abuse event occur after the mediator variables were collected. We therefore completed sensitivity analyses in which the abuse variable was restricted to include only events reported at Wave 1, but which did not include physical abuse events perpetrated by foster caregivers (see Results section).
RESULTS
Just over half of the study participants reported having experienced physical and/or sexual abuse. Most reported multiple placement changes (with a maximum of over 40 reported placements), and the majority reported having been in group care and also in kinship care at least once (Table 1). Over half reported having a “very close” relationship with their current caregiver. Twenty-two percent (22%) to 33% reported symptoms of depression, PTSD, and/or a substance use disorder. In terms of outcomes, 79% reported inconsistent condom use, 21% reported having had 5 or more partners, 9% reported having had sex for money, and 30% reported having had a partner with an STI in the past year at one or more waves or having ever received an STI diagnosis. All study variables were associated with gender and/or race (covariates), except closeness to current caregiver and avoidant attachment. Table 2 includes a matrix of unadjusted “pairwise” correlations evaluated between study variables.
Table 1.
Descriptive Statistics and Bivariate Associations with Gender and Race for All Study Variables
| Characteristic | Na | Whole Sample | Females | Males | pb | African American | Other Race | pc |
|---|---|---|---|---|---|---|---|---|
| MALTREATMENT & FOSTER CARE EXPERIENCES | ||||||||
| -Physical or Sexual Abuse (%) | 731 | 54 | 64 | 44 | .000 | 46 | 65 | .000 |
| - Total Placements (0−42; mean (SD)) | 727 | 5.8 (5.9) | 5.3 (5.4) | 6.4 (6.4) | .013 | 5.2 (5.2) | 6.7 (6.7) | .001 |
| -Group Placements (0−21; mean (SD)) | 729 | 1.7 (2.8) | 1.5 (2.8) | 2.1 (2.8) | .004 | 1.4 (2.3) | 2.2 (3.5) | .000 |
| -Close to Foster/Kin/Group Caregiver (%) | 617 | 58 | 58 | 58 | .875 | 57 | 59 | .518 |
| -Kinship Care (%) | 731 | 57 | 61 | 52 | .017 | 73 | 34 | .000 |
| -Extended Care (%) | 603 | 47 | 50 | 43 | .085 | 61 | 27 | .000 |
| HYPOTHESIZED MEDIATORS | ||||||||
| - ≥5 Depression Symptoms (%) | 593 | 22 | 30 | 15 | .000 | 18 | 28 | .004 |
| - ≥1 PTSD Symptom(s) (%) | 716 | 23 | 29 | 16 | .000 | 21 | 25 | .210 |
| - ≥1 Substance-Related Symptom(s) (%) | 715 | 33 | 28 | 39 | .003 | 28 | 41 | .000 |
| -Oppositional/Delinquent Scale (0−45; mean (SD)) | 730 | 7.7 (6.7) | 6.5 (5.6) | 8.9 (7.5) | .000 | 7.1 (6.2) | 8.5 (7.2) | .003 |
| -Anxious Attachment Scale (1−7; mean (SD)) | 730 | 3.2 (1.2) | 3.3 (1.3) | 3.1 (1.1) | .006 | 3.2 (1.2) | 3.3 (1.2) | .096 |
| -Avoidant Attachment Scale (1−7; mean (SD)) | 730 | 3.6 (1.0) | 3.5 (1.1) | 3.6 (1.0) | .615 | 3.6 (1.0) | 3.5 (1.0) | .148 |
| OUTCOMES | ||||||||
| -Inconsistent Condom Use-Any Wave (%) | 697 | 79 | 85 | 73 | .000 | 77 | 83 | .051 |
| -Five or More Partners-Any Wave (%) | 690 | 21 | 11 | 33 | .000 | 24 | 18 | .071 |
| Sex for Money-Any Wave (%) | 711 | 9 | 8 | 10 | .215 | 13 | 4 | .000 |
| STI Diagnosis-Partner or Self (%) | 696 | 30 | 40 | 20 | .000 | 34 | 26 | .036 |
Totals for each variable differ due to missing data
p-value for association with gender
p-value for association with race (African-American)
Table 2.
Pairwise Correlation Matrix for All Study Variables
| Pairwise Correlation Coefficient | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
| 1 | Physical/Sexual Abuse | 1 | |||||||||||||||
| 2 | Total Placements | .23*** | 1 | ||||||||||||||
| 3 | Group Homes | .17*** | .64*** | 1 | |||||||||||||
| 4 | Close to Foster Caregiver | −.11** | −.22*** | −.20*** | 1 | ||||||||||||
| 5 | Kinship Care | −.13*** | −.18*** | −.25*** | .10** | 1 | |||||||||||
| 6 | Extended Care Past Age 18 | −.04 | .04 | −.00 | −.07 | .19 | 1 | ||||||||||
| 7 | Depression Symptoms | .22*** | .09* | .05 | −.06 | −.07† | −.03 | 1 | |||||||||
| 8 | PTSD Symptoms | .26*** | .11** | .08* | −.10* | −.09* | −.08† | .20*** | 1 | ||||||||
| 9 | Substance Use Symptoms | .11** | .17*** | .19*** | −.05 | −.06 | −.09* | .07† | .11** | 1 | |||||||
| 10 | Opp/Delinquent Behaviors | .18*** | .26*** | .32*** | −.20*** | −.12** | −.10* | .18*** | .12** | .41*** | 1 | ||||||
| 11 | Anxious Attachment | .13*** | .14*** | .12** | −.16*** | −.06 | −.07 | .35*** | .17*** | .03 | .18*** | 1 | |||||
| 12 | Avoidant Attachment | .10** | .17*** | .16*** | −.28*** | −.04 | .01 | .13** | .11** | .11** | .19*** | .40*** | 1 | ||||
| 13 | Inconsistent Condom Use | .06 | .02 | −.04 | .03 | −.07† | −.09* | −.01 | .10* | .08* | .10* | .02 | −.03 | 1 | |||
| 14 | 5 or More Partners | −.08* | .06 | .05 | −.05 | .01 | −.04 | −.07 | −.01 | .13*** | .17*** | −.03 | −.04 | .09* | 1 | ||
| 15 | Sex for Money | −.02 | .10** | .13*** | −.03 | .05 | .07 | −.04 | .03 | .09* | .08* | .03 | .04 | .04 | .17*** | 1 | |
| 16 | STI in Partner/Self | .13*** | .03 | −.02 | −.05 | .04 | −.02 | .07† | .09* | .05 | .10** | .14*** | .10* | .27*** | .15*** | .14*** | 1 |
p<0.10
p<0.05
p<0.01
p<0.001
A total of 713 youth were included in the final path model. Overall fit of our main model was good (SRMR = 0.026). The coefficient of determination (R2) for the entire model was 0.501, indicating that 50.1% of the variance in the model was accounted for by study variables or covariates. Figure 2 shows all significant paths; coefficients for individual associations are standardized for ease of comparison. In evaluating specific pathways to risk, we found that history of physical and/or sexual abuse was the key exposure variable associated with STI risk in our model (after controlling for gender and race). Specifically, abuse exposure was positively associated with all proposed mental health and relational mediators except substance use symptoms and avoidant attachment. Having been in group care was also associated with increased oppositional/delinquent behaviors. Score on the oppositional/delinquent behavior scale, in turn, was significantly related to inconsistent condom use, though this relationship was relatively modest in size, and had a borderline significant relationship with having greater than 5 partners (coefficient=0.12; p=0.09); no other proposed mediators emerged as significant contributors to the sexual risk behavior outcomes. Both inconsistent condom use and having greater than 5 partners was positively associated with having an STI diagnosis and/or having a partner with an STI; having had sex for money at any wave demonstrated a borderline significant relationship with this variable as well (coefficient=0.10; p=0.07).
Figure 2.
Final path model of abuse and foster care experiences, late adolescent psychosocial mediators, and STI risk in young adulthood for youth in foster care.a,b
 significant STI risk path
significant STI risk path
 significant STI protective path
significant STI protective path
 significant associations not involved in an STI risk or protective pathway
significant associations not involved in an STI risk or protective pathway
 significant covariance between two variables at same time point
significant covariance between two variables at same time point
Model fit statistics: SRMR=0.026; CD=0.501
P-values for standardized path coefficients: *p<0.05; **p<0.01; ***P<0.001.
aN=713; bgender, race, & inverse probability weight also included
With respect to protective factors, reporting a very close relationship with a current foster caregiver was negatively associated with (i.e., protective against) delinquent behaviors and avoidant attachment style; this variable also had a borderline significant relationship with anxious attachment style (coefficient=-0.12; p=0.06). Remaining in care was significantly protective against inconsistent condom use.
When evaluating moderation by gender, we found that that a model unconstrained by gender fit better than a constrained model (Chi-square difference of 283.0 with 74 degrees of freedom; p<0.000). However, analysis of individual path coefficients in the unconstrained, gender-specific models (with weights included) revealed only 2 differences in significant pathways between male-only and female-only models. One new path was significant in the model containing females only: having had sex for money in the past year at one or more waves was associated with an increased risk of reporting an STI diagnosis in partner or self (coefficient =0.20, p=0.000 in females and −0.01, p=0.948 in males). In addition, the coefficient for the association between abuse history and attachment anxiety was significantly larger in males than in females (0.23, p=0.01 in males and 0.05, p=0.56 in females). All other pathways were similar. Sensitivity analyses, including the model in which we restricted our abuse definition to include only physical abuse events which occurred prior to Wave 1, indicated similar path coefficients and significance levels to those presented above.
DISCUSSION
The objectives of this study were to inform intervention and policy work directed at decreasing STIs and related behaviors in foster youth, by testing a conceptual model and detecting important psychosocial pathways to STI risk as well as potential protective factors during the transition from adolescence to young adulthood. Our overall model fit well, and significant pathways suggest that a history of physical or sexual abuse and having been in group care likely influence STI risk, at least in part, via their associations with oppositional/delinquent behaviors and consequent inconsistent condom use. The pathway involving abuse history and increased oppositional/delinquent behaviors is consistent with the juvenile justice literature, which indicates that for many youth aggressive/delinquent behaviors during adolescence may have their roots in chronic and/or multiple trauma exposure.38 It is also consistent with the STI literature, indicating that youth involved in the juvenile justice system tend to have high STI rates.16
Among foster youth, experiencing a close relationship with a substitute caregiver may decrease STI risk via its influence on externalizing (i.e., oppositional/delinquent) behaviors. Remaining in foster care beyond age 18 was also associated with a decreased risk of inconsistent condom use in our model. Staying in care longer may confer financial or other benefits that affect condom use and consequent STI risk; in addition the extension of substitute caregiver support during this developmentally vulnerable period may allow youth to develop better relationship and health-related behavior patterns. It is also possible that youth who remain in care are in some way predisposed to have lower rates of sexual risk behaviors, however research on the transition from adolescence to adulthood in other populations supports the above hypotheses that increased adult support during emerging adulthood has the potential to decrease sexual and other risk behaviors.16,23
Several limitations should be acknowledged. First, although greater than 80% follow-up rates are considered excellent for a longitudinal study with a transient population such as former foster youth, missing data could have affected our results. However, when youth who participated in Wave 2 were compared with youth who were lost to follow up on demographic and socioeconomic variables, the only significant difference detected was that fewer males were present in the follow-up sample.3 We also included an inverse probability weight and used available data methodology to account for missing data, both of which have been shown to improve point and standard error estimates.35,36 Second, we used self-report data. Due to potential biases that self-report data can introduce, we may have failed to accurately identify, or could have overestimated, contributions of some pathways to STI risk. Third, it is possible that we detected some reverse causation between abuse and/or foster care variables and psychosocial mediators. A detailed examination of the reciprocal associations among abuse history, types and stability of placements, and behavioral or mental health problems is beyond the scope of this study. However, from a practical standpoint it is important to know that abuse history and group care placement are markers of participation in oppositional/delinquent behaviors, and that strategies addressing these behaviors are likely to impact STI risk in this population. Finally, we did not evaluate potential contributions of other adverse childhood experiences (e.g. neglect, parental substance abuse); future work may identify other significant pathways to STI risk for this population.
Overall, results suggest that trauma-informed interventions focusing on externalizing behaviors may be promising strategies for STI prevention among foster youth. As an example, Multidimensional Treatment Foster Care, an intervention designed to decrease delinquent behaviors, has been shown to decrease teen pregnancy among female juvenile offenders.39 Thus, it and similar interventions may also decrease STI risk. Skill-based approaches which emphasize emotion regulation and interpersonal skills to prevent or minimize the development of oppositional/delinquent behaviors may be useful, in combination with or instead of traditional behavioral STI curricula. Dialectical-behavioral therapy is an example of one such intervention, and evidence is mounting that it may effectively address adolescent delinquent behaviors.40 For young women in foster care, the inclusion of content related to the prevention of transactional sex behaviors is likely important. Finally, policy changes which promote placement stability, youth-caregiver relationship building, and/or which extend foster care beyond age 18 have the potential to decrease STI risk and related behaviors for both genders.
IMPLICATIONS AND CONTRIBUTION.
Findings suggest that among foster youth, abuse history is associated with increased oppositional/delinquent behaviors in adolescence, which are, in turn, associated with inconsistent condom use and STI risk in young adulthood. Trauma-informed interventions which address externalizing behaviors and promote stable, high quality caregiver relationships could decrease STI risk for foster youth.
Acknowledgements
Research reported in this publication was supported by: the National Institute of Mental Health of the National Institutes of Health under award number1K23MH09098, and a New Investigator Award from the University of Washington Center for AIDS Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The parent study, the Midwest Evaluation of the Adult Functioning of Former Foster Youth, is a collaborative research effort with cooperation and funding from the Illinois Department of Children and Family Services, the Wisconsin Department of Health and Family Services, and the Iowa Department of Human Services; the authors wish to thank these departments for their support. The original study was also supported by funding from the William T. Grant Foundation. The authors also wish to thank all members of the research team at Chapin Hall Center for Children, Kerryann DiLoreto and the interviewers at the University of Wisconsin Survey Center in Madison, WI, and the individuals who participated in the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None of the authors have conflicts of interest to disclose.
REFERENCES
- 1.Courtney ME, Dworsky A, Lee JS, et al. Midwest evaluation of the adult functioning of former foster youth: Outcomes at age 23 and 24. Chapin Hall at the University of Chicago; Chicago: 2009. [March 19, 2013]. Available at: www.chapinhall.org/research/report/midwest-evaluation-adult-functioning-former-foster-youth. [Google Scholar]
- 2.Courtney ME, Dworsky A, Ruth GR, et al. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 21. Chapin Hall at the University of Chicago; Chicago: 2007. [March 19, 2013]. Available at: www.chapinhall.org/research/report/midwest-evaluation-adult-functioning-former-foster-youth. [Google Scholar]
- 3.Courtney ME, Dworsky A, Ruth GR, et al. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 19. Chapin Hall at the University of Chicago; Chicago: 2007. [March 19, 2013]. Available at: www.chapinhall.org/research/report/midwest-evaluation-adult-functioning-former-foster-youth. [Google Scholar]
- 4.Courtney ME, Terao S, Bost N. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Conditions of Youth Preparing to Leave State Care. Chapin Hall at the University of Chicago; Chicago: 2004. [March 19, 2013]. Available at: www.chapinhall.org/research/report/midwest-evaluation-adult-functioning-former-foster-youth. [Google Scholar]
- 5.O'Connell ME, Boat T, KE W, editors. National Research Council and Institute of Medicine. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Committee on Prevention of Mental Disorders and Substance Abuse Among Children, Youth and Young Adults: Research Advances and Promising Interventions. Board on Children, Youth, and Families, Division of Behavioral and Social Sciences and Education. The National Academies Press; Washington, DC: 2009. [PubMed] [Google Scholar]
- 6.Ahrens KR, Richardson LP, Courtney ME, et al. Laboratory-diagnosed sexually transmitted infections in former foster youth compared with peers. Pediatrics. 2010;126:e97–e103. doi: 10.1542/peds.2009-2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carpenter SC, Clyman RB, Davidson AJ, et al. The association of foster care or kinship care with adolescent sexual behavior and first pregnancy. Pediatrics. 2001;108:E46. doi: 10.1542/peds.108.3.e46. [DOI] [PubMed] [Google Scholar]
- 8.Crocker AR, Carlin EM. Coitarche and care: Does experience of the ‘looked after’ system affect timing of a woman's sexual debut? Int J STD AIDS. 2002;13:812–814. doi: 10.1258/095646202321020062. [DOI] [PubMed] [Google Scholar]
- 9.Polit DF, Morton TD, White CM. Sex, contraception and pregnancy among adolescents in foster care. Fam Plann Perspect. 1989;21:203–208. [PubMed] [Google Scholar]
- 10.Committee on Prevention Control of Sexually Transmitted Diseases Institute of Medicine . The Hidden Epidemic:Confronting Sexually Transmitted Diseases. The National Academies Press; 1997. [PubMed] [Google Scholar]
- 11.Haydon AA, Hussey JM, Halpern CT. Childhood abuse and neglect and the risk of STDs in early adulthood. Perspect Sex Reprod Health. 2011;43:16–22. doi: 10.1363/4301611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oshri A, Tubman JG, Jaccard J. Psychiatric symptom typology in a sample of youth receiving substance abuse treatment services: associations with self-reported child maltreatment and sexual risk behaviors. AIDS Behav. 2011;15:1844–1856. doi: 10.1007/s10461-011-9890-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katsikas SL. Long-term effects of childhood maltreatment: An attachment theory perspective. US: Dissertation Abstracts International: Section B: The Sciences and Engineering. ProQuest Information & Learning; 1996. [Google Scholar]
- 14.Alexander PC. The differential effects of abuse characteristics and attachment in the prediction of long-term effects of sexual abuse. J Interpers Violence. 1993;8:346–362. [Google Scholar]
- 15.Ciesla JA, Roberts JE, Hewitt RG. Adult Attachment and High-Risk Sexual Behavior Among HIV-Positive Patients. J Appl Soc Psychol. 2004;34:108–124. [Google Scholar]
- 16.DiClemente RJ, Crittenden CP, Rose E, et al. Psychosocial predictors of HIV-associated sexual behaviors and the efficacy of prevention interventions in adolescents at-risk for HIV infection: what works and what doesn't work? Psychosom Med. 2008;70:598–605. doi: 10.1097/PSY.0b013e3181775edb. [DOI] [PubMed] [Google Scholar]
- 17.Kershaw TS, Milan S, Westdahl C, et al. Avoidance, anxiety, and sex: The influence of romantic attachment on HIV-risk among pregnant women. AIDS Behav. 2007;11:299–311. doi: 10.1007/s10461-006-9153-z. [DOI] [PubMed] [Google Scholar]
- 18.Ahrens K, DuBois D, Garrison M, et al. Qualitative exploration of relationships with important non-parental adults in the lives of youth in foster care. Child Youth Serv Rev. 2011;33:1012–1023. doi: 10.1016/j.childyouth.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gramkowski B, Kools S, Paul S, et al. N. Health risk behavior of youth in foster care. J Child Adolesc Psychiatr Nurs. 2009;22:77–85. doi: 10.1111/j.1744-6171.2009.00176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mekonnen R, Noonan K, Rubin D. Achieving better health care outcomes for children in foster care. Pediatr Clin North Am. 2009;56:405–415. doi: 10.1016/j.pcl.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 21.Ahrens K, DuBois D, Richardson L, et al. Youth in foster care with adult mentors during adolescence have improved adult outcomes. Pediatrics. 2008;121:e246–252. doi: 10.1542/peds.2007-0508. [DOI] [PubMed] [Google Scholar]
- 22.GovTrack.us. H.R. 6893--110th Congress [March 19, 2013];Fostering Connections to Success and Increasing Adoptions Act of 2008, GovTrack.us (database of federal legislation) 2008 Available at www.govtrack.us/congress/bills/110/hr6893.
- 23.Steinberg L. A social neuroscience perspective on adolescent risk-taking. Dev Rev. 2008;28:78–106. doi: 10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Becker MG, Barth RP. Power Through Choices: The Development of a Sexuality Education Curriculum for Youths in Out-of-Home Care. Child Welfare. 2000;79:269–82. [PubMed] [Google Scholar]
- 25.McGuinness TM, Mason M, Tolbert G, et al. Becoming responsible teens: Promoting the health of adolescents in foster care. J Ame Psychiatr Nurses Assoc. 2002;8:92–98. [Google Scholar]
- 26.Slonim-Nevo V, Auslander WF. The long-term impact of AIDS-preventive interventions for delinquent and abused adolescents. J Adolesc. 1996;31:409. [PubMed] [Google Scholar]
- 27.The Composite International Diagnostic Interview (CIDI) World Health Organization. Geneva, Switzerland: 1998. [Google Scholar]
- 28.Kilpatrick D, Saunders B. National Survey of Adolescents in the United States. ICPSR 2833. Inter-University Consortium For Political and Social Research; Ann Arbor, MI: 1995. [Google Scholar]
- 29.Valenzuela MJ, Sachdev P. Assessment of complex mental activity across the lifespan: development of the Lifetime of Experiences Questionnaire (LEQ). Psychol Med. 2007;37:1015–1025. doi: 10.1017/S003329170600938X. [DOI] [PubMed] [Google Scholar]
- 30.American Psychiatric Association . Task Force on D-I. Diagnostic and statistical manual of mental disorders : DSM-IV-TR. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 31.Harris K. The National Longitudinal Study of Adolescent Health (Add Health), Waves I & II, 1994-1996; Wave III, 2001-2002; Wave IV, 2007-2009 [machine-readable data file and documentation]. : Chapel Hill, NC: Carolina Population Center. University of North Carolina; Chapel Hill: 2009. [Google Scholar]
- 32.Fraley RC, Heffernan ME, Vicary AM, et al. The Experiences in Close Relationships-Relationship Structures questionnaire: a method for assessing attachment orientations across relationships. Psychol Assess. 2011;23:615–625. doi: 10.1037/a0022898. [DOI] [PubMed] [Google Scholar]
- 33.Stata Technical Support, Stata Statistical Sofware: Release 12. [computer program] Statcorp LP; College Station, TX: 2011. [Google Scholar]
- 34.Croy CD, Novins DK. Methods for addressing missing data in psychiatric and developmental research. J Am Acad Child Adolesc Psychiatry. 2005;44:1230–1240. doi: 10.1097/01.chi.0000181044.06337.6f. [DOI] [PubMed] [Google Scholar]
- 35.Kline RB. Principles and practice of structural equation modeling. 2nd ed. Guilford Press; New York, NY US: 2005. [Google Scholar]
- 36.Curtis LH, Hammill BG, Eisenstein EL, et al. Using inverse probability-weighted estimators in comparative effectiveness analyses with observational databases. Med Care. 2007;45:S103–107. doi: 10.1097/MLR.0b013e31806518ac. [DOI] [PubMed] [Google Scholar]
- 37.MacCallum RC, Browne MW, Cai L. Testing differences between nested covariance structure models: Power analysis and null hypotheses. Psychol Methods. 2006;11:19–35. doi: 10.1037/1082-989X.11.1.19. [DOI] [PubMed] [Google Scholar]
- 38.Silvern L, Griese B. Multiple Types of Child Maltreatment, Posttraumatic Stress, Dissociative Symptoms, and Reactive Aggression among Adolescent Criminal Offenders. J Child Adolesc Trauma. 2012;5:88–101. [Google Scholar]
- 39.Kerr DC, Leve LD, Chamberlain P. Pregnancy rates among juvenile justice girls in two randomized controlled trials of multidimensional treatment foster care. J Consult Clin Psychol. 2009;77:588–593. doi: 10.1037/a0015289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Quinn A, Shera W. Evidence-based practice in group work with incarcerated youth. Int J Law Psychiatry. 2009;32:288–293. doi: 10.1016/j.ijlp.2009.06.002. [DOI] [PubMed] [Google Scholar]