Abstract
The homing of mesenchymal stem cells to injured tissue, which is important for the correction of conditions such as ischemia-reperfusion injury (IRI) and immunolesions, has been performed previously, but with poor efficiency. Substantial improvements in engraftment are required to derive clinical benefits from MSC transplantation. Chemokines are the most important factors that control cellular migration. Stromal derived factor-1 (SDF-1) is up-regulated during tissue/organ ischemia damage, and its cognate receptor, chemokine receptor 4 (CXCR4), is involved in stem cell migration. The aim of our study was to investigate CXCR4 expression in MSCs and to validate both its role in mediating migration to transplanted kidneys and its immunoregulatory effects in renal protection. Specifically, the present study was designed to investigate the short-term tissue homing of MSCs carrying genetically modified CXCR4 in a rat renal transplantation model. We tested the hypothesis that MSCs with CXCR4 over-expression can more efficiently regulate immunological reactions. Lentiviral vectors were used to over-express CXCR4 or to introduce a short hairpin ribonucleic acid (shRNA) construct targeting endogenous CXCR4 in rat MSCs. MSCs were labeled with enhanced green fluorescent protein (eGFP). After cell sorting, recipient kidneys were regionally perfused; recipient animals were injected with transduced MSCs, native MSCs, or PBS via tail vein following renal transplantation; and the effects of MSC injection were observed.
Introduction
Mesenchymal stem cells (MSCs) have great potential for the treatment of various diseases, especially those involving tissue damage due to immune reactions and ischemia reperfusion injury (IRI) [1]–[3]. Acute/chronic renal failure, particularly renal allograft dysfunction, is associated with high morbidity and mortality [4]–[6]. An increasing number of studies have focused on endogenous and exogenous methods to protect renal function after renal transplantation [7], and MSC-based therapeutic approaches for organ transplantation are promising. Studies show that MSCs can prevent or attenuate ischemic tissue injury in primary transplantation [4], [8]–[11]. MSCs are specially characterized by their low immunogenicity and immunoregulatory abilities [12]–[17]. These MSC characteristics are ideal for their use in a renal transplantation model. Some studies have demonstrated that stem cells are capable of forming functional components of kidney [18], [19].
However, in vivo strategies with MSCs rely upon efficient localization and retention within the appropriate tissue(s). Current evidence suggests that in the absence of tissue damage, systemically administered MSCs only seed target tissues or organs at low levels [20]–[26]. Furthermore, due to localized hypoxia, oxidative stress and inflammation in the targeted tissue, the homing of transplanted cells is very also low and transient, reducing the therapeutic effects [26]–[28]. Thus, it is crucial to identify techniques that can enhance the chemotaxis and retention of implanted MSCs to maximize the effectiveness of MSC-based therapy. It is also important to elucidate MSC immunoregulatory mechanisms in transplanted kidneys. Many studies have demonstrated that stem cell migration and organ-specific homing are regulated by chemokines and their receptors [29], [30]. SDF-1 plays a major role in the homing and engraftment of stem cells and progenitor cells to bone marrow and other injured tissues [23], [29], [31]–[33]. Its receptor, CXCR4, is highly expressed in MSCs within the bone marrow, but this expression is largely reduced during ex vivo expansion of MSCs [34]. Previous studies have shown that the SDF-1/CXCR4 axis may play an important role in the homing and survival of MSCs [29], [33], [35]–[38]. However, the therapeutic effects of the SDF-1/CXCR4 axis in renal transplantation have not been clearly evaluated, and its detailed mechanism of action is unknown.
The aim of our study was to modulate CXCR4 expression in MSCs and to observe the effects both on secretory action and MSC viability in vitro and on migration and immunoregulation in transplanted kidneys in vivo. The surface expression of CXCR4 was either up-regulated or knocked down in rat MSCs with lentiviral vectors. A rat renal transplantation model was utilized, and the homing, renal protection and paracrine/autocrine functions of these cells were assessed.
Results
Cells isolated from rat bone marrow samples exhibited the properties of MSCs
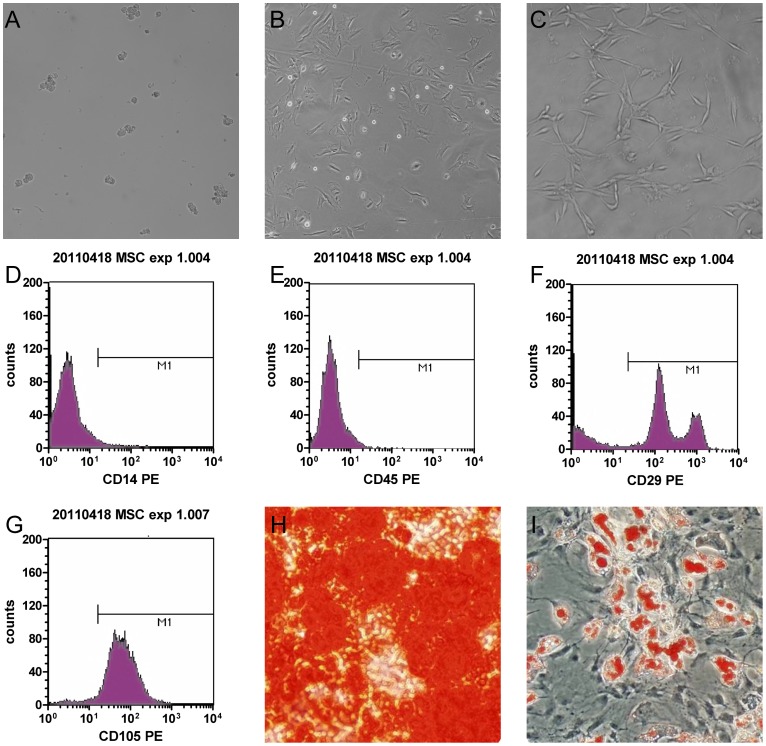
Primary adherent cells were small and round in the first few days following isolation (Fig. 1A), but later they became larger and polygonal (Fig. 1B). The cells were expanded under normal culture conditions and had a fusiform shape or uniform morphology after several passages (Fig. 1C). Rat MSCs expressed typical markers and differentiation profiles. They strongly expressed CD29 and CD105 but were negative for CD14 and CD45, as shown by flow cytometry analysis (Fig. 1D, E, F, and G). This surface marker pattern was comparable to previous studies and guidelines for MSCs [3], [39], [40]. Culture-expanded MSCs were also tested for their multi-lineage differentiation potential. In vitro tests using the appropriate inductive culture conditions promoted osteogenic or adipogenic MSC differentiation (Fig. 1H and I). Thus, the isolated cells met MSC standards mostly [40].
Figure 1. Characterization of rat bone marrow MSCs (α-MEM).
(A) Isolated MSCs were round and small at 2 days after isolation. (B) After three passages, MSCs became larger and multiangular. (C) Before use, MSCs were mostly found in the clostridial form. (D, E, F, G) Fluorescent immunocytostaining showed that cultivated cells expressed CD29, strongly expressed CD105 and did not express CD14 and CD45. (H) Osteocyte lineage differentiation potential was determined by Alizarin Red S staining. (I) Oil Red O staining indicated the accumulation of oil droplets in cells that differentiated to adipocytes.
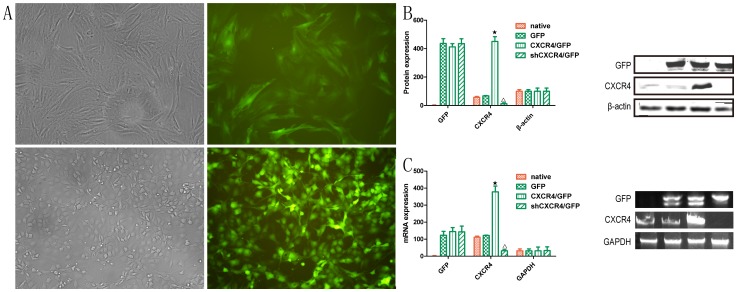
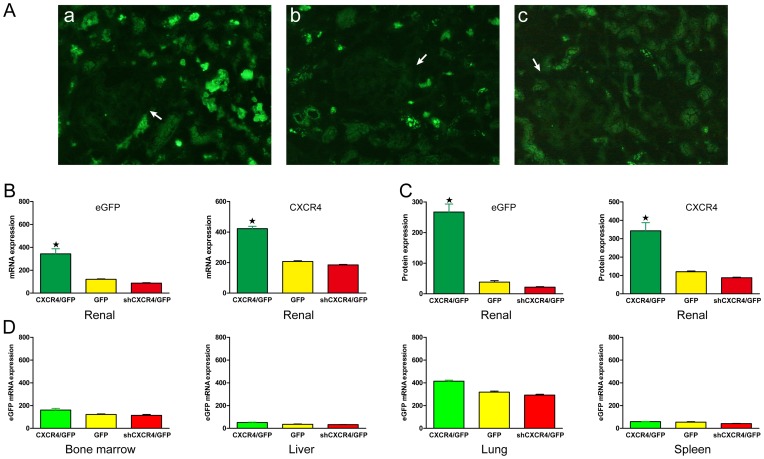
Analysis of transfection efficiency
MSCs were transfected with the sense-strand lentiviral vectors pLV-null-eGFP, pLV-shRNA-CXCR4-eGPF or pLV-CXCR4-eGFP. To confirm the transfection efficiency, MSCs were observed with fluorescence microscopy. Green fluorescent MSCsGFP, MSCsCXCR4 /GFP and MSCsshCXCR4/GFP could be observed (Fig. 2A). The expression of CXCR4 and GFP by MSCs was examined at both the mRNA and protein levels. Expression of the CXCR4 protein was higher in MSCsCXCR4 /GFP compared to cells from the control groups (MSCsnative and MSCsGFP) and MSCsshCXCR4/GFP, as determined by Western blot (Fig. 2B). Semi-quantitative RT-PCR was performed and revealed that CXCR4 expression was significantly higher in MSCsCXCR4 /GFP than in the control groups and was lowest in MSCsshCXCR4/GFP (Fig. 2C). Furthermore, analysis of eGFP expression at the mRNA and protein levels confirmed the transfection efficiency.
Figure 2. Transfection efficiency in MSCs.
(A) Staining for fluorescence microscopy showed that MSCs expressed eGFP (original magnification 400× and 200×). (B) Western blot analysis was performed to detect CXCR4 protein expression. β-actin was used as protein loading control. Analysis of CXCR4 levels by histogram indicated that protein expression was up-regulated in MSCsCXCR4 /GFP(★P<0.05 vs MSCsnative) and down-regulated in MSCsshCXCR4/GFP (▵P<0.05 vs. MSCsnative). (C) Semi-quantitative RT-PCR was used to analyze CXCR4 mRNA levels in MSCs. GAPDH was used as RNA loading control. (★▵P<0.05 vs. MSCsnative).
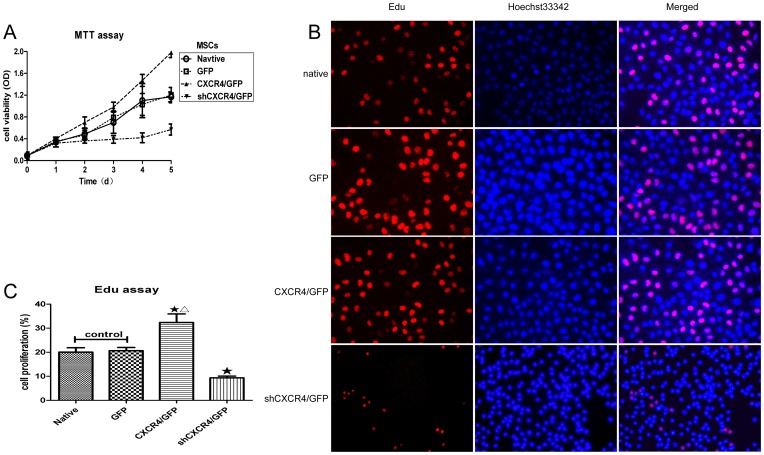
Effects of CXCR4 expression on the cellular proliferation of MSCs
In order to investigate the proliferation and cytotoxicity, a standard proliferation and cytotoxicity test, the MTT assay, was adopted to assess mitochondrial viability, and a 5-ethynyl-2′-deoxyuridine (EdU) incorporation assay was used to investigate DNA synthesis in MSCs infected with either a CXCR4 or shRNA-CXCR4 lentiviral vector for CXCR4 up-regulation or down-regulation, respectively. As shown in Fig. 3, knockdown of CXCR4 resulted in significant reductions in MSC viability. (Fig. 3A). EdU incorporation dramatically increased from 28.2% to 42.3% in MSCsCXCR4 /GFP (Fig. 3B) and decreased from 11.3% to 7.9% in MSCsshCXCR4/GFP (Fig. 3C). This result indicated that cell proliferation was inhibited with reduced CXCR4 expression and that CXCR4 up-regulation facilitated cell proliferation. Comparison of MSCsGFP and MSCsnative showed no difference, demonstrating that the viral vector and eGFP expression did not affect cell proliferation.
Figure 3. Regulation of CXCR4 expression affects the proliferation of MSCs in vitro.
(A) Viability was decreased in MSCsshCXCR4/GFP and increased in MSCsCXCR4 /GFP compared to MSCsGFP or MSCsnative (control), as measured by the MTT assay (Mean ± SD; n = 6; P<0.05 from NO. 4 to 5 time point). (B) All cell nuclei exhibited blue fluorescent Hoechst 33342 staining, and EdU labeling indicated replicating cells. In MSCsCXCR4, an increased number of cells exhibited red fluorescent EdU labeling following CXCR4 overexpression. In MSCsshCXCR4/GFP, fewer cells exhibited red fluorescence, indicating that EdU labeling decreased with CXCR4 knockdown. (C) The percentages of red fluorescent cells for different MSC groups are indicated in the histogram. There were more replicating cells for MSCsCXCR4 /GFP than the control group. ★P<0.05 vs. control, and ▵P<0.01 vs. MSCsshCXCR4/GFP.
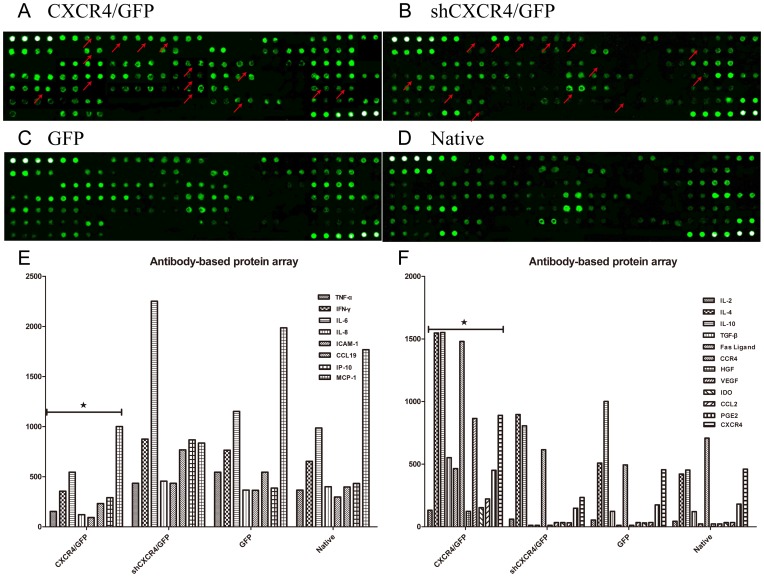
Effects of CXCR4 regulation on MSC secretion
We used a rat cytokine antibody array that enabled us to detect the expression of 90 different rat target proteins, including cytokines, chemokines, adipokines, growth factors, angiogenic factors, proteases, soluble receptors, soluble adhesion molecules and other proteins, in cell culture supernatants to investigate these factors in MSCs with and without modification. In contrast to MSCsGFP and MSCsshCXCR4/GFP, up-regulated factors in MSCsCXCR4 /GFP included interleukins2, -4, -10 (IL-2, -4, -10), TGF-β, Fas Ligand, CCR4, HGF, VEGF, indoleamine 2,3-dioxygenase (IDO), CCL2, and prostaglandin E2 (PGE2), and down-regulated factors included TNF-α, IFN-γ, IL-6, IL-8, ICAM-1, CCL19, etc. (Fig. 4).
Figure 4. Antibody-based protein array system.
Positive controls are located in the upper left-hand corner (four spots) and lower right-hand corner (two spots) of each membrane. (A) MSCsCXCR4 /GFP. (B) MSCsshCXCR4 /GFP. (C) MSCsGFP. (D) MSCsnative. Down-regulated or up-regulated proteins are indicated with arrowheads. Histogram shows protein array results. (E) down-regulated proteins. (F) up-regulated proteins. ★P<0.05 vs. MSCsGFP.
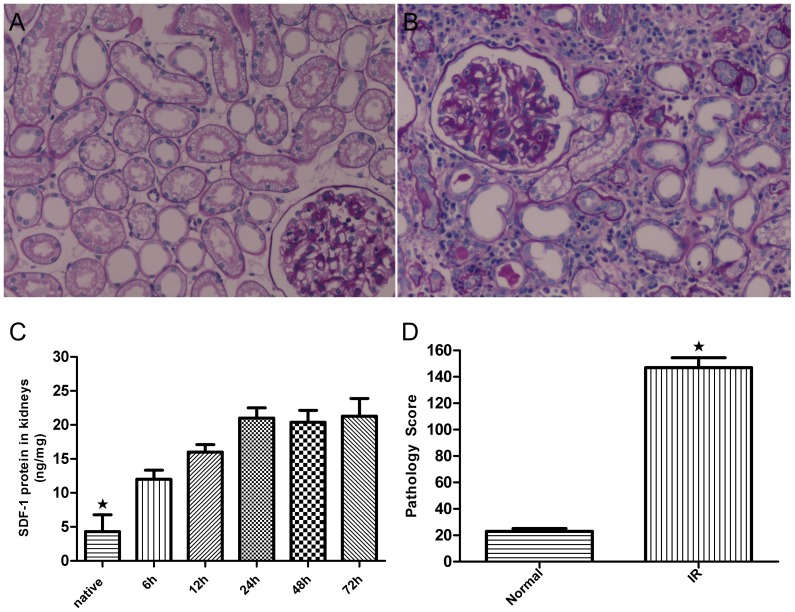
SDF-1 expression is up-regulated in transplanted kidneys
In this study, we demonstrated that SDF-1 was up-regulated in an IRI renal model (Fig. 5 A, B). TheSDF-1 protein levels in transplanted kidneys were observed by enzyme-linked immunosorbent assay (ELISA) at 6 h, 24 h, 48 h, and 72 h after surgery. The results showed that the IRI caused a time-dependent increase in SDF-1 protein levels (Fig. 5C). SDF-1 appeared to increase within the first 6 h after transplant surgery, peaked at 24 h and remained at high levels at 48 h until day 3 after surgery, compared to the levels observed in control kidneys. Pathology score analysis showed a apparently higher injury score in transplanted kidney (Fig. 5 D).
Figure 5. Injury in transplanted organs.
(A, B) Morphology analysis showed apparent injury in transplanted organs. (C) SDF-1 protein was up-regulated in transplanted kidneys. The kidney tissue lysates from recipient rats were analyzed by ELISA to determine SDF-1 protein expression at 5 time points after transplant surgery. The histogram indicates that SDF-1 expression was up-regulated in transplanted kidneys at different time points post-surgery time. ★P<0.05 vs. normal kidney. (D) Pathology score analysis showed a disparity. Normal kidneys were used as controls (methods not shown). ★P<0.05 vs. control.
Short-term homing of transplanted MSCs to transplanted kidneys in vivo
To validate the homing of MSCs to target tissue, we looked for eGFP-labeled MSCs 48 h after MSC infusion. Transplanted MSCs could be detected via their eGFP expression by fluorescent microscopy. The migration and distribution of infected MSCs were observed 3 days after the operation. Many eGFP+ cells could be found in the transplanted kidneys (Fig. 6Aa, b, c). The vast majority of eGFP+ MSCs were located within the tubules. Some eGFP+ MSCs were also found around the lumens of blood vessels. Furthermore, CXCR4 and eGFP expression were examined by quantifying mRNA and protein levels in the kidney via RT-PCR and Western blot, respectively (Fig. 6B and C). MSCsCXCR4 /GFP demonstrated significantly higher levels of CXCR4 and eGFP compared with MSCsGFP and MSCsshCXCR4/GFP.
Figure 6. The role of the SDF-1-CXCR4 pathway in the homing of MSCs.
(A) Kidney uptake of eGFP-labeled MSCs was measured by fluorescence microscopy 48 h after systemic administration (a: MSCsCXCR4 /GFP, b: MSCsGFP, c: MSCsshCXCR4/GFP). Labeled cells were detected surrounding the glomerulus (arrows). (B and C) Chemotaxis into transplanted kidneys was measured by RT-PCR andWestern blot. Recipients treated with MSCsGFP were used as control. ★P<0.05 vs. control. (D) The expression of eGFP in different organs from recipient rats was measured 48 h after infusion.
Infused MSCs redistributed not only to the kidneys but also to other organs, including the lungs, spleen and bone marrow. We also detected eGFP expression by measuring mRNA levels via real-time fluorescent quantitation PCR in the lungs, spleen, liver and bone marrow of kidney recipients (Fig. 6D). It appears that CXCR4 over-expression magnified the rate of homing to transplanted kidneys.
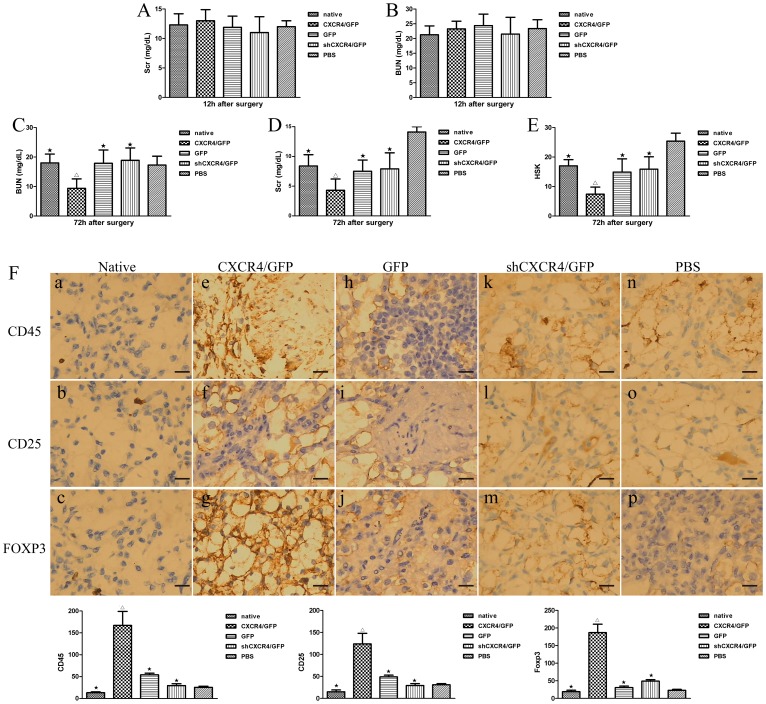
Transplantation of MSCs ameliorate transplanted renal failure
Twelve hours after renal surgery, renal function was dissimilarly aggravated in animals receiving MSCsCXCR4 /GFP, MSCsshCXCR4/GFP, MSCsGFP, MSCsnative, and PBS treatment, as assessed by blood urea nitrogen (BUN) and serum creatinine (Scr) levels (Fig. 7A and B). The administration of all MSCs improved renal function assessed by Scr in animals at day 3 after transplantation compared to renal function in PBS-treated animals. However, MSCsCXCR4 /GFP-treated animals had significantly lower BUN and Scr levels at 48 h after infusion compared with MSCsnative-, MSCsGFP-, and MSCsshCXCR4/GFP-treated animals. Renal function was restored to normal levels at 3 days after transplantation in MSC-treated groups (Fig. 7C and D). BUN levels were also restored to normal levels at 3 days after transplantation in PBS-treated groups. But Scr levels did not. To further substantiate these results, histological scores of kidneys (HSK) were evaluated. As expected, kidneys from MSC-treated rats had significantly reduced HSK compared with control PBS-treated kidneys (Fig. 7E). Assessment of kidney function and structure showed that the transplantation of different MSC types, in particular MSCsCXCR4/ GFP, had greater therapeutic effects than the administration of PBS alone.
Figure 7. Transplantation of MSCs was renoprotective.
The effects of the SDF-1-CXCR4 pathway on the therapeutic efficacy of MSCs for the treatment of injury in transplanted kidneys was evaluated by measuring serum urea, serum creatinine, pathology scores, and immunohistochemisty staining. BUN and Scr levels were measured in recipients that received MSCs or PBS 12 h and 72 h after the surgery. There were no difference between each group 12 h after the surgery (A and B), but there were significant diversity 72 h after the surgery (C and D). ★P<0.05 vs. MSCsCXCR4/GFP; ▵P<0.05 vs. PBS. (E) HSK in transplanted kidneys that received different MSCs or PBS were calculated 72 h after the surgery (n = 8 per group). ★P<0.05 vs.MSCsCXCR4 /GFP ; ▵P<0.05 vs. PBS. (F) Expression of CD25, FOXP3, or CD45 in the renal interstitium of native renal tissues or at different MSCs-treated groups after renal transplantation by immunohistochemistry. a, b, c: Paraffin-embedded sections of normal renal tissues showing weaker expression of CD25, or FOXP3, or CD45 [diaminobenzidine (DAB), original magnification 200×]. P<0.05 vs. transplanted kidney. d∼p: Paraffin-embedded sections of transplanted kidney exhibiting positive expression of CD25, or FOXP3, or CD45 in the renal interstitium (DAB, original magnification 200×). The expression of CD45,CD25 and FOXP3 were hyper in MSCsCXCR4 /GFP-treated group.★ P<0.05 vs. MSCsCXCR4 /GFP-treated group. ▵P<0.05 vs. PBS-treated group. Scale bars represent 50 µm.
Immunohistochemisty staining showed that, within kidney interstitium, CD25 or Foxp3 immunoreactivity was detected in cells interspersed among the intertitium of renal tubules. In contrast with PBS-, or MSCsshCXCR4/GFP-, or MSCsGFP-treated group, in MSCsCXCR4 /GFP-treated group, more percentage of CD25+ and Foxp3+ cells were present in the different zones of renal interstitium (Figures 7 F). But there were no different of CD45+ cells between the four groups (Figures 7 F e, h, k, n).
Discussion
Renal transplantation is an effective approach for end-stage renal disease. To prevent rejection reactions, organ recipients must take steroids and immune-suppressing drugs for life after surgery. However, many serious side effects of these drugs, such as infection and tumors, impact recipient survival rates and quality of life. MSCs are characterized by their low immunogenicity, abundant tissue sources, easy accessibility, and immunoregulation abilities, and therefore, they have become a good option for organ transplantation. Professor Tan has achieved good therapeutic effects in clinical treatment [41].
This study investigated the effects of CXCR4 expression modulation in MSCs on the role of MSCs in a renal transplantation model. The results showed that (i) the proportion of transplanted cells localizing into the kidneys increased with CXCR4 overexpression; and the secretory action of MSCs was critically influenced by CXCR4 gene modification.
Importantly, our observations confirmed a potential role for CXCR4 in the short-term homing behavior of topically and systemically administered MSCs. We demonstrated that induced surface expression of CXCR4 by lentiviral gene transfer was able to enhance in vivo short-term homing and to enhance cell proliferation and immunosuppressive soluble factors in vitro.
Site-directed administration of MSCs is only practical for a limited number of applications, and thus, the localization of MSCs is crucial for successful therapy. Current evidence suggests that in the absence of tissue damage, systemically administered MSCs only seed the target organ at low levels [21], [42], with large numbers of MSCs lodging in the pulmonary vascular bed [20]–[25], [43], [44]. The chemokine SDF-1, together with its receptor, CXCR4, plays a major role in the homing and engraftment of MSCs to target organs. Numerous studies have demonstrated that the SDF-1/CXCR4 axis is essential for MSC homing in humans and rats [45], [46]. CXCR4 and SDF-1 levels are both up-regulated in stressed or injured tissues [11], [47]–[49]. Inflammation leads to activation of the endothelium, increased impermeability and the expression of various adhesion molecules. IRI-related acute inflammation causes acute organ damage and, more importantly, strengthens the host immune response by enhancing graft immunogenicity through activation of intragraft antigen-presenting cells and supporting infiltration by immune cells via up-regulation of major histocompatibility complex (MHC) class II (MHC II) antigens, intracellular adhesion molecule-1 (ICAM-1), and P- and E-selectin [50]. Therefore, IRI-induced intragraft inflammation is a key factor in renal allograft immunogenicity and explains poor outcomes [51]. MSCs, with their broad immunomodulatory and tissue-protective properties, might be ideal candidates for conditioning the environment in the recipient to combat IRI in transplanted organs [11], [49]. Reports on the homing and engraftment of MSCs are limited and controversial. Recent results showed that MSCs could migrate to damaged kidneys and participate in functional and structural recovery or regeneration [52]–[54]. However, subsequent studies have demonstrated that only a few MSCs engraft injured tubules, and their overall contribution to renal repair is negligible [26], [55]. Overall, in wild-type MSCs, CXCR4 expression is limited [33]. MSCs can only home and engraft into IRI kidneys to a very restricted degree. Substantial improvements are necessary to enable greater clinical benefits. CXCR4 expression is dynamic and can be regulated by cytokines, adhesion molecules, ligand-binding and proteolytic enzymes [56]. Previous studies demonstrated that such variability may be related to differences in culture conditions [30], [36], [57].
In the present study, we used a lentiviral system to stably over-express or knock down a functional CXCR4 gene in rat MSCs, and we examined the effects in vivo. Based on Western blot and quantitative PCR data, as well as fluorescent microscopy, acceptable transgene expression levels were achieved. We did not determine whether other chemokines and their receptors also participated in the regulation of MSC homing in this study. However, we found that the neutralization of CXCR4 could not completely abolish MSC homing and engraftment. This finding suggests that there are other factors that affect homing, which has also been suggested by other studies [58], [59]. Cooperative and compensatory mediators are involved in migration and homing, and these mediators can partially and flexibly substitute when CXCR4 expression is lost. The cytokine milieu and the source of MSCs most likely both determine the main pathway that operates in cell migration [60]. Therefore, we examined changes to cytokines in this study.
We analyzed the cytokines present in MSC cultivation supernatant and determined that many interesting changes to protein levels occurred when CXCR4 was modulated. Numerous in vitro studies have shown that MSCs have low immunogenicity [61] and poorly express or do not express HLA-I [13] or the transplantation immunity factors CD80,CD86,CD40,and CD40L [16]. In addition, MSCs have been shown to secrete cytokines and growth factors, which not only decrease IRI but also suppress immune cell functions [10], [17], [62]. MSCs inhibit the proliferation and cytotoxic effects of antigen-specific CTLs [63]. MSCs can also suppress T cell proliferation and activation [64]. In animal studies [65] and clinical trials [15], MSCs have been shown to exhibit immuno-depression and reduce inflammation. Their immunomodulation efficacy has also been shown in vivo during solid organ transplantation [41], [66]. However, the exact MSC immunomodulatory mode of action still remains unclear. Some reports have demonstrated that the immunomodulatory properties of MSCs are associated with direct cell-cell contact with T cells [67], whereas others have shown that MSCs can regulate immune functions by secreting a variety of cytokines and chemokines, such as interleukin IL-10, nitric oxide (NO), TGF-β, PGE2, HGF, and IDO [14], [17], [68]. These results are compatible with our study. The up-regulation of TGF-β and IL-10 is important for the differentiation and proliferation of regulatory T cells (Treg cells) [69]–[71]. Treg cells have very important immunoregulatory effects and play a significant role in the induction of immunotolerance or the maintenance of immunosuppressive activity [72]–[74]. Furthermore, up-regulation of many factors can enhance these immunoregulatory effects of MSCs, including CCL2 [75], PGE2 [76], [77],iNOS [78], VACM-1 and ICAM-1 [79], IL-4 [80], CD45 [81], and IDO [82], [83]. MSCs secrete soluble factors to regulate immunity. Our findings indicate the decreased immunogenicity of transplanted kidneys and the inhibited migration of activated T cells or possibly regulatory T cells that are necessary to mediate immunomodulatory functions [8]. It is well known that IFN-α induces MHC II expression and can also be amplified by TNF-α produced by other cells [84]. ICAM-1 expression could be affected by TNF-α and IFN-γ production, and it has also been reported that MSCs induce the down-regulation of ICAM-1 on co-cultured fibroblasts [85]. IL-2 and TGF-β can induce CD4+C25− T cells to express Foxp3, converting them to CD4+CD25+ Treg cells [86]. Following the down-regulation of pro-inflammatory cytokines, both MHC II expression and subsequent injurious cell migration into injured kidneys might be suppressed by the administration of MSCs.
Another unique property of MSCs is their tissue repair potential, which is attributed to their migration and differentiation capacity and their ability to secrete various growth factors [21]–[23]. Although numerous IRI-related studies describe protective effects in kidney injury or transplantation models [9], [87]–[91], few groups have focused on the relationship between changes in the paracrine action of MSCs and the induction of immunotolerance. In our study, many factors relevant to immunosuppression were up-regulated when CXCR4 was overexpressed.
Analysis of the effects of MSC application within an early time frame demonstrated CXCR4-related effects on three processes: (i) the down-regulation of pro-inflammatory cytokines (TNF-α, IFN-γ, IL-6); (ii) the inhibition of adhesion molecules (ICAM-1), resulting in diminished infiltration by macrophages and CD3+ T cells, particularly activated CD25+ cells; and (iii) the prevention of IRI-induced release of DC-attracting chemokines (CCL19), resulting in diminished infiltration by DCs. MSCs, through direct contact [92] or through the secretion of IL-6 or PEG2, inhibit the migration abilities of DCs, enhance the conversion of DCs into immature or tolerant cell types, or affect cell activity [68], [93]–[95]. Furthermore, we found that the over-expression of CXCR4 could enhance these secretory actions. These data reveal a correlation between CXCR4 expression in MSCs and intragraft immune activation that leads to acute rejection and compromised long-term graft function.
The secondary findings in our studies were the beneficial effects of CXCR4 on cell proliferation and survival, which are very important in a therapeutic context. The longer that transplanted MSCs retain their special characteristics, the more transplanted MSCs can cycle and accumulate in ischemic kidneys, and the more recipient MSCs can be incorporated among renal cells, facilitating differentiation into renal stem cells or terminal cells and ultimately participating in the repair of kidney function. MSCs form nested capillaries that might be helpful in supplying more oxygen and providing secondary protection against injury tubular [96].
Some limitations of the current study are the relatively small sample size and a failure to study the ability of MSCs to induce tolerance and long-term graft survival in our model. In our next study, we will examine whether the up-regulation of CXCR4 can also enhance the long-term residency of MSCs in transplanted kidneys. Several aspects of our study distinguish it from previous studies [97], [98]. These discrepancies may be explained by differences in experimental design, such as the cell transplantation protocol, the animal strain, and the type and severity of gene mismatch.
In conclusion, we have demonstrated that MSC therapy ameliorates the negative effects of IRI in a very strong, clinically relevant model of rat kidney transplantation at early time points. CXCR4 plays a critical role not only in the process of homing but also in the pathogenesis of acute rejection and chronic allograft nephropathy, in which both immune- and non-immune-mediated mechanisms are involved. CXCR4 is a clinically useful parameter for the identification of subjects with a high risk of acute rejection, chronic allograft nephropathy, and graft failure. The pretreatment to MSCs, such as using some cytokines or anoxia to up-regulate CXCR4, may facilitate the migration of infused MSCs to the site of injury and promote tissue repair [30]. Increased CXCR4 expression can improve the homing of MSCs to transplanted kidneys, inhibit rejection reactions and accelerate the recovery of renal function in vivo. This simple method could contribute to the prevention of IRI and acute/chronic rejections and to the individualization of immunosuppressive therapies after renal transplant.
Materials and Methods
All experimental procedures were conducted in accordance with the Detailed Rules for the Administration of Animal Experiments for Medical Research Purposes, issued by the Ministry of Health of China, and had received ethical approval by the Animal Experiment Administration Committee of the FMMU and the General Hospital of Shenyang Military Region (Shenyang, China). All efforts were made to minimize animal suffering and to reduce the number of animals used.
Animals
Animals were purchased from the Animal Center of the Fourth Military Medical University (FMMU) (Xi'an, China) and the General Hospital of Shenyang Military Region (Shenyang, China), housed individually in cages with a 12 hour light-dark cycle and given free access to water and standard rat chow throughout the study. Eleven-week-old Wistar rats (200–220 g; Laboratory Animal Center of the FMMU, Xi'an, China) were used as donors, and 7-week-old Sprague-Dawley (SD) rats (200–250 g; Laboratory Animal Center of the FMMU, Xi'an, China) were used as recipients. Two-week-old SD rats (100–120 g; Laboratory Animal Center of the FMMU, Xi'an, China, and the General Hospital of Shenyang Military Region, Shenyang, China) were used as MSC donors. Animals were anesthetized with inhaled isoflurane (2% to 3%).
Isolation of MSCs
Two-week-old SD rats were killed by cervical dislocation. Bone marrow cells from femurs and tibiae were collected using a syringe with a 26-gauge needle, and freshly isolated cells were centrifuged at 2,000 rpm for 5 min. The marrow was washed in phosphate-buffered saline (PBS), centrifuged at 1,000 rpm for 10 min, and then re-suspended into α-modified Eagle's medium (α-MEM; Gibco®, Life Tech, USA) supplemented with 10% fetal bovine serum (FBS, Invitrogen™,Life Tech, USA) and 1% penicillin-streptomycin (Gibco®, Life Tech, USA) in a humidified atmosphere of 5% CO2 at 37°C. After culture for 48 hours, non-adherent cells were removed via media replacement twice per week. When cultures reached 80–90% confluence, adherent cells were trypsinized (1% Trypsin–EDTA, Gibco®, Life Tech, USA). Cells were collected and replated at concentrations ranging between 0.05 and 0.15×105 cells/ml of medium for several passages. MSCs from passages 4–8 were used for all experiments.
Identification and differentiation of MSCs
To confirm the identity of the isolated cells as MSCs, the expression of some surface markers was examined by flow cytometry. Surface marker expression was measured by FACS analysis using specific mouse monoclonal antibodies for the rat surface markers CD14, CD45, CD29, and CD105, followed by staining with a PE-labeled anti-mouse-IgG specific antibody (all antibodies: BD Biosciences Pharmingen, USA).
The differentiation of rat MSCs (passage 4) into osteocytes and adipocytes was evaluated as described previously [3]. Briefly, to induce osteogenic differentiation, cells (6×103/cm2) were seeded and cultured for 3 weeks in Dulbecco's Modified Eagle Medium (DMEM; Gibco®, Life Tech, USA) with 10% FBS and the osteogenic supplements 50 µM L-ascorbic acid-2-phosphate, 100 nM dexamethasone and 10 mM β-glycerophosphate (Sigma, USA). Bone mineralization was confirmed with Alizarin red staining. Adipocytes were identified by Oil red O staining (Sigma, USA) after treatment with induction medium, consisting of high-glucose DMEM with 10% FBS, 1 µM dexamethasone, 0.2 mM indomethacin, 0.5 mM 3-isobutyl-1-methylxanthine (Sigma, USA), and 10 µg/ml insulin (Novo Nordisk®), and maintenance medium, consisting of DMEM, FBS, antibiotics and insulin, for 3 weeks.
MTT and EdU Assays
To determine whether CXCR4 was involved in cellular proliferation, we infected MSCs with either a CXCR4 or shRNA-CXCR4 lentiviral vector for CXCR4 up-regulation or down-regulation, respectively. The effects of genetic regulation on MSC proliferation were measured with a 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide assay and a 5-ethynyl-2′-deoxyuridine (EdU, Ruibo Biotech, China) incorporation assay using an MTT cell proliferation and cytotoxicity assay kit (Beyotime, China) and an EdU assay kit (RiboBio, China), respectively, according to the manufacturer instructions. OD values at 570 nm were measured with a Sunrise microplate reader (Tecan, Groedig, Austria). EdU-labeled cells were manually counted in ten fields of view that were randomly selected in each well, and percentages were calculated.
Viral vector construction and transduction of MSCs
The lentiviral three-plasmid expression system (kindly provided by Prof. Jian Zhang, FMMU, Xi'an, China) was used to generate the recombinant vector. A rat CXCR4 plasmid (kindly provided by Prof. ChaoJun Song, FMMU, Xi'an, China) was subcloned into the transfer vector pLV-IRES-GFP to generate the pLV-CXCR4-IRES-GFP plasmid, which contained the enhanced green fluorescence protein (eGFP) expression cassette, and insertion was confirmed by sequencing. Stable down-regulation of CXCR4 was achieved by transduction of a lentiviral vector with short hairpin RNA (shRNA) for CXCR4 (shRNA-CXCR4), generated by GenePharma (GenePharma, Shanghai, China), to knock down the expression of CXCR4. Complementary DNA oligonucleotides were then subcloned into the pLV-IRES-GFP backbone to generate the pLV-shRNA-CXCR4-IRES-GFP construct. This resulting transfer plasmid, a packaging plasmid (psPAX2), and an enveloping plasmid (pMD2.G) were co-transfected into 293T cells using Lipofectamine 2000 (Invitrogen™, Life Tech). The cells were transfected for 6 h, and the medium was subsequently replaced. The viral particles were harvested at 48 h or 72 h after transfection, filtered through a 0.45-µm cellulose acetate filter, and concentrated by centrifugation at 50,000 rpm (4°C) for 2 h. The titer was determined via transduction of 293T cells with serial dilutions of the vector and eGFP expression assessment by flow cytometry after 72–96 h. Infection with diluted pLV resulted in less than 40% eGFP+ cells, and this value was used to calculate the transducing units.
MSCs were transduced with pLV-IRES-GFP (encoding eGFP), pLV-CXCR4-IRES-GFP (encoding CXCR4 and eGFP), or pLV-shRNA-CXCR4-IRES-GFP (encoding shRNA-CXCR4 and eGFP, separated) lentiviral vectors at a multiplicity of infection of 30 in the presence of 5 mg/ml Polybrene (Sigma), followed by a second transduction after 48 h. MSCs transduced with pLV-CXCR4-IRES-GFP, pLV-shRNA-CXCR4-IRES-GFP, or pLV-IRES-GFP were referred to as MSCsCXCR4 /GFP, MSCsshCXCR4/GFP, or MSCsGFP, respectively. In this study, MSCsGFP and untransduced MSCs (MSCsnative) were controls.
RNA preparation and RT-PCR analysis
After humanely sacrificing the animals, organs were removed and kept in liquid nitrogen until analysis. Tissues were placed in lysis buffer and then homogenized with a tissue homogenizer using TRIZOL reagent (Invitrogen™,Life Tech, USA), and total RNA was isolated. Total RNA was isolated from MSCs using TRIZOL reagent as well. Reverse transcription-polymerase chain reaction (RT-PCR) was performed with equal amounts of RNA using a reverse transcriptase kit (Takara, Japan) according to the manufacturer's instructions. RT was performed in a 25 µl polymerase chain reaction reaction mixture that contained 10 nM 5′ and 3′ oligomers and Taq DNA polymerase (Takara, Japan). Real time-PCR experiments were performed using SYBR Green (Takara, Japan) and an ABI machine. Samples were normalized based on GAPDH values. The presence and levels of CXCR4 or eGFP were determined with SYBR Premix Ex Taq kit (Takara, Japan) and a Rotor Gene 6000 Real-Time PCR Machine. The primers used for this study are available upon request. Gene sequences were searched in MEDLINE and re-validated. The temperature profile consisted of an initial step at 95°C for 10 min followed by 40 cycles of 95°C for 15 s and 60°C for 1 min. Melting curve analysis and agarose gel electrophoresis were performed after amplification. All of the results represent the average density of the positive bands obtained from three independent experiments using Quantity One software (Bio-Rad).
Western-blot analysis
Kidney samples were homogenized, and the lysates were sonicated for 10 s and centrifuged at 12,000 rpm for 15 min. Protein concentrations were determined using a bicinchoninic acid (BCA) protein assay kit (Thermo Scientific). Fifty micrograms of protein was loaded onto a 10% SDS-polyacrylamide gel, and after electrophoresis, proteins were transferred to nitrocellulose filters. The filters were blocked with TBS-T buffer containing 5% nonfat milk and were then incubated with primary anti-CXCR4 rabbit polyclonal antibodies (Santa Cruz, CA) or anti-eGFP rabbit polyclonal antibodies (Santa Cruz, CA). Equal loading of all lanes was confirmed by reprobing the membrane with anti-β-actin mouse monoclonal antibodies (Santa Cruz, CA) overnight at 4°C. Horseradish peroxidase (HRP)-conjugated secondary antibodies were obtained from Jackson ImmunoResearch Laboratories (West Grove, PA). Densitometric analysis was performed using Kodak Digital Science 1D software (Kodak, New Haven, CT). The experiments were repeated two more times with different tissues or pooled cells. The results were then statistically analyzed.
Antibody-based protein array system
Cell-free supernatants were removed from the conditioned serum-free media of 4-day cultured MSCsGFP, MSCsCXCR4/GFP, MSCsshCXCR4/GFP, or MSCsnative and then analyzed with the RayBio Rat Cytokine Array V kit, which was purchased from RayBiotech (RayBio, Guangzhou, China). The array membranes can detect 90 different growth factors/cytokines at once. The layout of the membrane is depicted in Fig. 4. The assay protocol was followed precisely as stated in the directions from the manufacturer. In brief, each membrane was placed into the provided eight-well tray, 2 ml blocking buffer was added, and the membranes were incubated at room temperature for 30 min. The blocking buffer was decanted from each container, and the membranes were then incubated with 1 ml of conditioned medium at room temperature for 2 h. The samples were decanted from each container, and the membranes were washed three times with 2 ml of wash buffer I at room temperature with shaking for 5 min, followed by two washes with 2 ml of wash buffer II at room temperature with shaking for 5 min. One milliliter of 250-fold diluted biotin-conjugated antibodies was added to each membrane and incubated at room temperature for 2 h. After washing two times, 2 ml of 1000-fold diluted HRP-conjugated streptavidin was added to each membrane and incubated at room temperature for 30 min, followed again by 2 washes. The membranes were placed in detection buffer and incubated at room temperature for 5 min. Excess detection reagent was drained off, and the membrane was wrapped with PE wrap. The membrane was then exposed to Hyperfilm (Amersham Bioscience). Detectable spots were scanned by a densitometer. Positive controls, provided by the manufacturer, were normalized to 1-fold, and the densities of the unknown samples were calculated and normalized to the control spots.
ELISA
The production of SDF-1 in the kidney cortex was determined by ELISA using a commercially available ELISA kit (R&D Systems, USA) according to the manufacturer's recommendations. Tissue lysates were obtained by mincing, sonicating, and lysing with RIPA buffer. Protein content was quantified with the BCA protein assay (Thermo Scientific). All samples and standards were measured in duplicate.
Animal model of kidney transplantation
After humane animal sacrifice, kidneys from male Wistar rats were harvested, perfused with Histidine Tryptophan Ketoglutarate solution (HTK, CUSTODIOL®, Germany) to remove blood from the vascular beds and maintained at 4°C. Approximatelyone hour later, kidney grafts were transplanted into male SD recipient rats, and blood flow was restored using standard microsurgical techniques. Contralateral kidneys were removed immediately after implantation of the left kidney graft. The animals were kept in a specific pathogen-free facility with drinking water containing Cyclosporine A (CsA, 1.5 mg/kg/day, Sandimmun Neoral; Novartis) and were injected with 1 ml PBS with or without 2.0×106 MSCs via the tail vein 24 h after the operation (n = 8 per group). Amoxicillin (1 mg/ml) was given each day to prevent infection. Three days after transplantation, the rats were euthanized, and grafts and some original organs were harvested for Western blot, RT-PCR and histological analysis (n = 8 per group). Operated animals appeared healthy until just before graft harvest without surgical complications during the observation period.
Cell transplantation procedures
To mimic the stem cell transplant protocol utilized in clinical renal transplant patients, SD recipient rats received lentiviral-transduced MSCs or native MSCs (2×106) diluted in 1 ml PBS or 1 ml PBS alone as a control via straight perfusion and caudal vein injections. Straight perfusions were performed when draining blood from donor kidneys, and injections were performed 24 h after renal transplants.
Animals were randomly divided into five groups: the MSCsCXCR4 /GFP-treated group (n = 8), the MSCsGFP-treated control group (n = 8), the MSCsshCXCR4/GFP-treated group (n = 8), the MSCsnative-treated control group (n = 8), and the PBS-treated group (n = 8).
Histopathological and biochemical analysis
To assess the therapeutic effects of native and genetically engineered MSC populations, blood was harvested 12 h and 72 h after renal transplantation, and tissue samples were harvested 72 h after transplantation. Biochemical and histopathological analyses were then performed (n = 8 per group). Briefly, random fields were analyzed using a 40× objective. The excised kidneys were fixed in phosphate-buffered 10% formalin, sectioned, and then stained with hematoxylin and eosin. HSK evaluation was performed in a blind manner by two separate pathologists. HSK was graded on a 4-point scale [99]: 0 = normal histology; 1 = mild damage [less than one-third of nuclear loss (necrosis) per tubular cross section]; 2 = moderate damage [greater than one-third and less than two-thirds of tubular cross section showing nuclear loss (necrosis)]; and 3 = severe damage [greater than two-thirds of tubular cross section shows nuclear loss (necrosis)]. The total score per kidney section was calculated by adding all 10 scores with a maximum possible injury score of 30. Quantification of Scr in serum samples was performed via an enzymatic method on a Cobas Integra analyzer (Roche, Indianapolis, IN). BUN quantification was performed manually via the diacetyl monoxime method.
Immunohistochemical staining
To assess CD25, FOXP3, and CD45 expression in transplanted kidneys of four groups and normal renal tissues (Paraffin-embedded sections), The Paraffin-embedded sections were fixed in freshly prepared 10% paraformaldehyde for 5 min. After blocking the endogenous peroxidase activity with 0.3% hydrogen peroxide in TBS for 15 min, the serial sections (5-µm thick) were immersed in horse serum diluted 1∶10 in TBS for 30 min to reduce nonspecific binding, and then were incubated with antibodies against CD25, or FOXP3, or CD45 (Abcam, diluted 1 : 100,United States) overnight at after washing in TBS. Next, the sections were incubated in biotinylated IgG for 30 min, and avidin-biotin-peroxidase complex for 30 min. After each step of the staining procedure, the sections were given three 5-min washes in TBS. Immunoreactivity (IR) was visualized using 1 mg/mL diaminobenzidine as chromogen and 0.01% hydrogen peroxide as substrate. The peroxidase reaction was stopped after 5 min with distilled water, and the sections were counter-stained with Toluidine blue, dehydrated, and then mounted with Entellan. Slides were evaluated under a light microscope (original magnification200×). For digital image analysis, the software Imagepro-Plus was used. Results were scored by two independent investigators as hadro-positive (+++), positive (++), weakly positive (+), heterogeneous (+−), or negative (−). The two scores were averaged.
Fluorescence microscopy for analysis of eGFP-positive cells
To determine whether overexpression of CXCR4 enhances the chemotaxis of MSCs into transplanted kidneys, the presence of eGFP was used to distinguish resident MSCs from injected MSCs. For the in vivo migration assay with donor MSCs, the kidneys of euthanized rats were removed 3 days after transplantation, as previously described, and cryosectioned into 6-µm sections. The sections were observed under a fluorescence microscope (Olympus) to identify eGFP+ MSCs. Ten random fields were analyzed using a 40× objective. The number of labeled MSCs per visual field was estimated by Image J software.
Statistical analysis
The results were statistically analyzed using SigmaStat (SPSS) version 11.0 software. All of the values were expressed as the mean ± SD. A one-way analysis of variance (ANOVA) or paired t-test was used for multiple or two-group comparisons. All of the tests were two-tailed, and a p-value of <0.05 was considered statistically significant.
Acknowledgments
The authors are grateful to Dr. Yan Jin (Fourth Military Medical University, Xi'an, China) for technical advice regarding the development of MSCs and to Dr. Bo-quan Jin (FMMU, Xi'an, China) for his wise comments on experimental design. We also appreciate the assistance of Dr. Ming Liang, Dr. Jie Tao and Dr. Dewei Zhang (General Hospital of Shenyang Military Region, Shenyang, China) in this study.
Funding Statement
This study was supported by the grants from National Natural Science Foundation of China (NSFC)(No. 30872583 to Yuan) and the Shanxi Social Development Project of Science and Technology (No. 2009K01-60-03 and No. 2012k16-08-02 to Yuan). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Xu G, Zhang L, Ren G, Yuan Z, Zhang Y, et al. (2007) Immunosuppressive properties of cloned bone marrow mesenchymal stem cells. Cell Res 17: 240–248. [DOI] [PubMed] [Google Scholar]
- 2. Bryan CF, Luger AM, Martinez J, Muruve N, Nelson PW, et al. (2001) Cold ischemia time: an independent predictor of increased HLA class I antibody production after rejection of a primary cadaveric renal allograft. Transplantation 71: 875–879. [DOI] [PubMed] [Google Scholar]
- 3. Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, et al. (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284: 143–147. [DOI] [PubMed] [Google Scholar]
- 4. Hoogduijn MJ, Popp FC, Grohnert A, Crop MJ, van RM, et al. (2010) Advancement of mesenchymal stem cell therapy in solid organ transplantation (MISOT). Transplantation 90: 124–126. [DOI] [PubMed] [Google Scholar]
- 5. Reinders ME, Fibbe WE, Rabelink TJ (2010) Multipotent mesenchymal stromal cell therapy in renal disease and kidney transplantation. Nephrol Dial Transplant 25: 17–24. [DOI] [PubMed] [Google Scholar]
- 6. Kosieradzki M, Rowinski W (2008) Ischemia/reperfusion injury in kidney transplantation: mechanisms and prevention. Transplant Proc 40: 3279–3288. [DOI] [PubMed] [Google Scholar]
- 7. Vatazin AV, Astakhov PV, Zul'karnaev AB, Kantariia RO, Artemov DV (2012) [Cellular factors of ischemia/reperfusion injury pathogenesis in the renal transplantation]. Ross Fiziol Zh Im I M Sechenova 98: 906–914. [PubMed] [Google Scholar]
- 8. Ge W, Jiang J, Arp J, Liu W, Garcia B, et al. (2010) Regulatory T-cell generation and kidney allograft tolerance induced by mesenchymal stem cells associated with indoleamine 2,3-dioxygenase expression. Transplantation 90: 1312–1320. [DOI] [PubMed] [Google Scholar]
- 9. De Martino M, Zonta S, Rampino T, Gregorini M, Frassoni F, et al. (2010) Mesenchymal stem cells infusion prevents acute cellular rejection in rat kidney transplantation. Transplant Proc 42: 1331–1335. [DOI] [PubMed] [Google Scholar]
- 10. Yoo KH, Jang IK, Lee MW, Kim HE, Yang MS, et al. (2009) Comparison of immunomodulatory properties of mesenchymal stem cells derived from adult human tissues. Cell Immunol 259: 150–156. [DOI] [PubMed] [Google Scholar]
- 11. Kale S, Karihaloo A, Clark PR, Kashgarian M, Krause DS, et al. (2003) Bone marrow stem cells contribute to repair of the ischemically injured renal tubule. J Clin Invest 112: 42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Le BK, Tammik C, Rosendahl K, Zetterberg E, Ringden O (2003) HLA expression and immunologic properties of differentiated and undifferentiated mesenchymal stem cells. Exp Hematol 31: 890–896. [DOI] [PubMed] [Google Scholar]
- 13. Lu LL, Liu YJ, Yang SG, Zhao QJ, Wang X, et al. (2006) Isolation and characterization of human umbilical cord mesenchymal stem cells with hematopoiesis-supportive function and other potentials. Haematologica 91: 1017–1026. [PubMed] [Google Scholar]
- 14. Munn DH, Sharma MD, Lee JR, Jhaver KG, Johnson TS, et al. (2002) Potential regulatory function of human dendritic cells expressing indoleamine 2,3-dioxygenase. Science 297: 1867–1870. [DOI] [PubMed] [Google Scholar]
- 15. Le BK, Rasmusson I, Sundberg B, Gotherstrom C, Hassan M, et al. (2004) Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet 363: 1439–1441. [DOI] [PubMed] [Google Scholar]
- 16. Deans RJ, Moseley AB (2000) Mesenchymal stem cells: biology and potential clinical uses. Exp Hematol 28: 875–884. [DOI] [PubMed] [Google Scholar]
- 17. Nauta AJ, Fibbe WE (2007) Immunomodulatory properties of mesenchymal stromal cells. Blood 110: 3499–3506. [DOI] [PubMed] [Google Scholar]
- 18. Poulsom R, Forbes SJ, Hodivala-Dilke K, Ryan E, Wyles S, et al. (2001) Bone marrow contributes to renal parenchymal turnover and regeneration. J Pathol 195: 229–235. [DOI] [PubMed] [Google Scholar]
- 19. Lin F, Cordes K, Li L, Hood L, Couser WG, et al. (2003) Hematopoietic stem cells contribute to the regeneration of renal tubules after renal ischemia-reperfusion injury in mice. J Am Soc Nephrol 14: 1188–1199. [DOI] [PubMed] [Google Scholar]
- 20. Riella LV, Chandraker A (2012) Stem cell therapy in kidney transplantation. JAMA 308: 130 author reply 130–131. [DOI] [PubMed] [Google Scholar]
- 21. Togel F, Hu Z, Weiss K, Isaac J, Lange C, et al. (2005) Administered mesenchymal stem cells protect against ischemic acute renal failure through differentiation-independent mechanisms. Am J Physiol Renal Physiol 289: F31–F42. [DOI] [PubMed] [Google Scholar]
- 22. Shyu WC, Lee YJ, Liu DD, Lin SZ, Li H (2006) Homing genes, cell therapy and stroke. Front Biosci 11: 899–907. [DOI] [PubMed] [Google Scholar]
- 23. Chavakis E, Urbich C, Dimmeler S (2008) Homing and engraftment of progenitor cells: a prerequisite for cell therapy. J Mol Cell Cardiol 45: 514–522. [DOI] [PubMed] [Google Scholar]
- 24. Sordi V (2009) Mesenchymal stem cell homing capacity. Transplantation 87: S42–S45. [DOI] [PubMed] [Google Scholar]
- 25. Zonta S, De Martino M, Bedino G, Piotti G, Rampino T, et al. (2010) Which is the most suitable and effective route of administration for mesenchymal stem cell-based immunomodulation therapy in experimental kidney transplantation: endovenous or arterial. Transplant Proc 42: 1336–1340. [DOI] [PubMed] [Google Scholar]
- 26. Duffield JS, Park KM, Hsiao LL, Kelley VR, Scadden DT, et al. (2005) Restoration of tubular epithelial cells during repair of the postischemic kidney occurs independently of bone marrow-derived stem cells. J Clin Invest 115: 1743–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fan VH, Tamama K, Au A, Littrell R, Richardson LB, et al. (2007) Tethered epidermal growth factor provides a survival advantage to mesenchymal stem cells. Stem Cells 25: 1241–1251. [DOI] [PubMed] [Google Scholar]
- 28. Mylotte LA, Duffy AM, Murphy M, O'Brien T, Samali A, et al. (2008) Metabolic flexibility permits mesenchymal stem cell survival in an ischemic environment. Stem Cells 26: 1325–1336. [DOI] [PubMed] [Google Scholar]
- 29. Schantz JT, Chim H, Whiteman M (2007) Cell guidance in tissue engineering: SDF-1 mediates site-directed homing of mesenchymal stem cells within three-dimensional polycaprolactone scaffolds. Tissue Eng 13: 2615–2624. [DOI] [PubMed] [Google Scholar]
- 30. Shi M, Li J, Liao L, Chen B, Li B, et al. (2007) Regulation of CXCR4 expression in human mesenchymal stem cells by cytokine treatment: role in homing efficiency in NOD/SCID mice. Haematologica 92: 897–904. [DOI] [PubMed] [Google Scholar]
- 31. Zhuang Y, Chen X, Xu M, Zhang LY, Xiang F (2009) Chemokine stromal cell-derived factor 1/CXCL12 increases homing of mesenchymal stem cells to injured myocardium and neovascularization following myocardial infarction. Chin Med J (Engl) 122: 183–187. [DOI] [PubMed] [Google Scholar]
- 32. Belema-Bedada F, Uchida S, Martire A, Kostin S, Braun T (2008) Efficient homing of multipotent adult mesenchymal stem cells depends on FROUNT-mediated clustering of CCR2. Cell Stem Cell 2: 566–575. [DOI] [PubMed] [Google Scholar]
- 33. Son BR, Marquez-Curtis LA, Kucia M, Wysoczynski M, Turner AR, et al. (2006) Migration of bone marrow and cord blood mesenchymal stem cells in vitro is regulated by stromal-derived factor-1-CXCR4 and hepatocyte growth factor-c-met axes and involves matrix metalloproteinases. Stem Cells 24: 1254–1264. [DOI] [PubMed] [Google Scholar]
- 34. Kyriakou C, Rabin N, Pizzey A, Nathwani A, Yong K (2008) Factors that influence short-term homing of human bone marrow-derived mesenchymal stem cells in a xenogeneic animal model. Haematologica 93: 1457–1465. [DOI] [PubMed] [Google Scholar]
- 35. Pasha Z, Wang Y, Sheikh R, Zhang D, Zhao T, et al. (2008) Preconditioning enhances cell survival and differentiation of stem cells during transplantation in infarcted myocardium. Cardiovasc Res 77: 134–142. [DOI] [PubMed] [Google Scholar]
- 36. Liu H, Liu S, Li Y, Wang X, Xue W, et al. (2012) The role of SDF-1-CXCR4/CXCR7 axis in the therapeutic effects of hypoxia-preconditioned mesenchymal stem cells for renal ischemia/reperfusion injury. PLoS One 7: e34608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kortesidis A, Zannettino A, Isenmann S, Shi S, Lapidot T, et al. (2005) Stromal-derived factor-1 promotes the growth, survival, and development of human bone marrow stromal stem cells. Blood 105: 3793–3801. [DOI] [PubMed] [Google Scholar]
- 38. Otsuru S, Tamai K, Yamazaki T, Yoshikawa H, Kaneda Y (2008) Circulating bone marrow-derived osteoblast progenitor cells are recruited to the bone-forming site by the CXCR4/stromal cell-derived factor-1 pathway. Stem Cells 26: 223–234. [DOI] [PubMed] [Google Scholar]
- 39. Djouad F, Plence P, Bony C, Tropel P, Apparailly F, et al. (2003) Immunosuppressive effect of mesenchymal stem cells favors tumor growth in allogeneic animals. Blood 102: 3837–3844. [DOI] [PubMed] [Google Scholar]
- 40. Dominici M, Le BK, Mueller I, Slaper-Cortenbach I, Marini F, et al. (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8: 315–317. [DOI] [PubMed] [Google Scholar]
- 41. Tan J, Wu W, Xu X, Liao L, Zheng F, et al. (2012) Induction therapy with autologous mesenchymal stem cells in living-related kidney transplants: a randomized controlled trial. JAMA 307: 1169–1177. [DOI] [PubMed] [Google Scholar]
- 42. Bi B, Schmitt R, Israilova M, Nishio H, Cantley LG (2007) Stromal cells protect against acute tubular injury via an endocrine effect. J Am Soc Nephrol 18: 2486–2496. [DOI] [PubMed] [Google Scholar]
- 43. Devine SM, Cobbs C, Jennings M, Bartholomew A, Hoffman R (2003) Mesenchymal stem cells distribute to a wide range of tissues following systemic infusion into nonhuman primates. Blood 101: 2999–3001. [DOI] [PubMed] [Google Scholar]
- 44. Lee RH, Pulin AA, Seo MJ, Kota DJ, Ylostalo J, et al. (2009) Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell 5: 54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sordi V, Malosio ML, Marchesi F, Mercalli A, Melzi R, et al. (2005) Bone marrow mesenchymal stem cells express a restricted set of functionally active chemokine receptors capable of promoting migration to pancreatic islets. Blood 106: 419–427. [DOI] [PubMed] [Google Scholar]
- 46. Ji JF, He BP, Dheen ST, Tay SS (2004) Interactions of chemokines and chemokine receptors mediate the migration of mesenchymal stem cells to the impaired site in the brain after hypoglossal nerve injury. Stem Cells 22: 415–427. [DOI] [PubMed] [Google Scholar]
- 47. Schioppa T, Uranchimeg B, Saccani A, Biswas SK, Doni A, et al. (2003) Regulation of the chemokine receptor CXCR4 by hypoxia. J Exp Med 198: 1391–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Askari AT, Unzek S, Popovic ZB, Goldman CK, Forudi F, et al. (2003) Effect of stromal-cell-derived factor 1 on stem-cell homing and tissue regeneration in ischaemic cardiomyopathy. Lancet 362: 697–703. [DOI] [PubMed] [Google Scholar]
- 49. Kim K, Lee KM, Han DJ, Yu E, Cho YM (2008) Adult stem cell-like tubular cells reside in the corticomedullary junction of the kidney. Int J Clin Exp Pathol 1: 232–241. [PMC free article] [PubMed] [Google Scholar]
- 50. Wood KJ (2003) Passenger leukocytes and microchimerism: what role in tolerance induction. Transplantation 75: 17S–20S. [DOI] [PubMed] [Google Scholar]
- 51. van der Woude FJ, Schnuelle P, Yard BA (2004) Preconditioning strategies to limit graft immunogenicity and cold ischemic organ injury. J Investig Med 52: 323–329. [DOI] [PubMed] [Google Scholar]
- 52. Li B, Cohen A, Hudson TE, Motlagh D, Amrani DL, et al. (2010) Mobilized human hematopoietic stem/progenitor cells promote kidney repair after ischemia/reperfusion injury. Circulation 121: 2211–2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Masereeuw R (2009) Contribution of bone marrow-derived cells in renal repair after acute kidney injury. Minerva Urol Nefrol 61: 373–384. [PubMed] [Google Scholar]
- 54. Morigi M, Introna M, Imberti B, Corna D, Abbate M, et al. (2008) Human bone marrow mesenchymal stem cells accelerate recovery of acute renal injury and prolong survival in mice. Stem Cells 26: 2075–2082. [DOI] [PubMed] [Google Scholar]
- 55. Szczypka MS, Westover AJ, Clouthier SG, Ferrara JL, Humes HD (2005) Rare incorporation of bone marrow-derived cells into kidney after folic acid-induced injury. Stem Cells 23: 44–54. [DOI] [PubMed] [Google Scholar]
- 56. Kucia M, Reca R, Miekus K, Wanzeck J, Wojakowski W, et al. (2005) Trafficking of normal stem cells and metastasis of cancer stem cells involve similar mechanisms: pivotal role of the SDF-1-CXCR4 axis. Stem Cells 23: 879–894. [DOI] [PubMed] [Google Scholar]
- 57. Ruster B, Gottig S, Ludwig RJ, Bistrian R, Muller S, et al. (2006) Mesenchymal stem cells display coordinated rolling and adhesion behavior on endothelial cells. Blood 108: 3938–3944. [DOI] [PubMed] [Google Scholar]
- 58. Ip JE, Wu Y, Huang J, Zhang L, Pratt RE, Dzau VJ (2007) Mesenchymal stem cells use integrin beta1 not CXC chemokine receptor 4 for myocardial migration and engraftment. Mol Biol Cell 18: 2873–2882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Annabi B, Lee YT, Turcotte S, Naud E, Desrosiers RR, et al. (2003) Hypoxia promotes murine bone-marrow-derived stromal cell migration and tube formation. Stem Cells 21: 337–347. [DOI] [PubMed] [Google Scholar]
- 60. Bonig H, Priestley GV, Papayannopoulou T (2006) Hierarchy of molecular-pathway usage in bone marrow homing and its shift by cytokines. Blood 107: 79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Liechty KW, MacKenzie TC, Shaaban AF, Radu A, Moseley AM, et al. (2000) Human mesenchymal stem cells engraft and demonstrate site-specific differentiation after in utero transplantation in sheep. Nat Med 6: 1282–1286. [DOI] [PubMed] [Google Scholar]
- 62. Bochev I, Elmadjian G, Kyurkchiev D, Tzvetanov L, Altankova I, et al. (2008) Mesenchymal stem cells from human bone marrow or adipose tissue differently modulate mitogen-stimulated B-cell immunoglobulin production in vitro. Cell Biol Int 32: 384–393. [DOI] [PubMed] [Google Scholar]
- 63. Karlsson H, Samarasinghe S, Ball LM, Sundberg B, Lankester AC, et al. (2008) Mesenchymal stem cells exert differential effects on alloantigen and virus-specific T-cell responses. Blood 112: 532–541. [DOI] [PubMed] [Google Scholar]
- 64. Stagg J, Pommey S, Eliopoulos N, Galipeau J (2006) Interferon-gamma-stimulated marrow stromal cells: a new type of nonhematopoietic antigen-presenting cell. Blood 107: 2570–2577. [DOI] [PubMed] [Google Scholar]
- 65. Karussis D, Kassis I, Kurkalli BG, Slavin S (2008) Immunomodulation and neuroprotection with mesenchymal bone marrow stem cells (MSCs): a proposed treatment for multiple sclerosis and other neuroimmunological/neurodegenerative diseases. J Neurol Sci 265: 131–135. [DOI] [PubMed] [Google Scholar]
- 66. Chabannes D, Hill M, Merieau E, Rossignol J, Brion R, et al. (2007) A role for heme oxygenase-1 in the immunosuppressive effect of adult rat and human mesenchymal stem cells. Blood 110: 3691–3694. [DOI] [PubMed] [Google Scholar]
- 67. Krampera M, Glennie S, Dyson J, Scott D, Laylor R, et al. (2003) Bone marrow mesenchymal stem cells inhibit the response of naive and memory antigen-specific T cells to their cognate peptide. Blood 101: 3722–3729. [DOI] [PubMed] [Google Scholar]
- 68. Shi Y, Hu G, Su J, Li W, Chen Q, et al. (2010) Mesenchymal stem cells: a new strategy for immunosuppression and tissue repair. Cell Res 20: 510–518. [DOI] [PubMed] [Google Scholar]
- 69. Patel SA, Meyer JR, Greco SJ, Corcoran KE, Bryan M, et al. (2010) Mesenchymal stem cells protect breast cancer cells through regulatory T cells: role of mesenchymal stem cell-derived TGF-beta. J Immunol 184: 5885–5894. [DOI] [PubMed] [Google Scholar]
- 70. English K, Ryan JM, Tobin L, Murphy MJ, Barry FP, et al. (2009) Cell contact, prostaglandin E(2) and transforming growth factor beta 1 play non-redundant roles in human mesenchymal stem cell induction of CD4+CD25(High) forkhead box P3+ regulatory T cells. Clin Exp Immunol 156: 149–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Selmani Z, Naji A, Zidi I, Favier B, Gaiffe E, et al. (2008) Human leukocyte antigen-G5 secretion by human mesenchymal stem cells is required to suppress T lymphocyte and natural killer function and to induce CD4+CD25highFOXP3+ regulatory T cells. Stem Cells 26: 212–222. [DOI] [PubMed] [Google Scholar]
- 72. Goodnow CC, Sprent J, de St Groth B F, Vinuesa CG (2005) Cellular and genetic mechanisms of self tolerance and autoimmunity. Nature 435: 590–597. [DOI] [PubMed] [Google Scholar]
- 73. Di IM, Del PB, De Ioanni M, Moretti L, Bonifacio E, et al. (2008) Mesenchymal cells recruit and regulate T regulatory cells. Exp Hematol 36: 309–318. [DOI] [PubMed] [Google Scholar]
- 74. Sun L, Akiyama K, Zhang H, Yamaza T, Hou Y, et al. (2009) Mesenchymal stem cell transplantation reverses multiorgan dysfunction in systemic lupus erythematosus mice and humans. Stem Cells 27: 1421–1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Rafei M, Hsieh J, Fortier S, Li M, Yuan S, et al. (2008) Mesenchymal stromal cell-derived CCL2 suppresses plasma cell immunoglobulin production via STAT3 inactivation and PAX5 induction. Blood 112: 4991–4998. [DOI] [PubMed] [Google Scholar]
- 76. Aggarwal S, Pittenger MF (2005) Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood 105: 1815–1822. [DOI] [PubMed] [Google Scholar]
- 77. Martinet L, Fleury-Cappellesso S, Gadelorge M, Dietrich G, Bourin P, et al. (2009) A regulatory cross-talk between Vgamma9Vdelta2 T lymphocytes and mesenchymal stem cells. Eur J Immunol 39: 752–762. [DOI] [PubMed] [Google Scholar]
- 78. Ren G, Zhang L, Zhao X, Xu G, Zhang Y, et al. (2008) Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell 2: 141–150. [DOI] [PubMed] [Google Scholar]
- 79. Ren G, Zhao X, Zhang L, Zhang J, L'Huillier A, et al. (2010) Inflammatory cytokine-induced intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 in mesenchymal stem cells are critical for immunosuppression. J Immunol 184: 2321–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Nemeth K, Keane-Myers A, Brown JM, Metcalfe DD, Gorham JD, et al. (2010) Bone marrow stromal cells use TGF-beta to suppress allergic responses in a mouse model of ragweed-induced asthma. Proc Natl Acad Sci U S A 107: 5652–5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Ghannam S, Pene J, Torcy-Moquet G, Jorgensen C, Yssel H (2010) Mesenchymal stem cells inhibit human Th17 cell differentiation and function and induce a T regulatory cell phenotype. J Immunol 185: 302–312. [DOI] [PubMed] [Google Scholar]
- 82. English K, Barry FP, Field-Corbett CP, Mahon BP (2007) IFN-gamma and TNF-alpha differentially regulate immunomodulation by murine mesenchymal stem cells. Immunol Lett 110: 91–100. [DOI] [PubMed] [Google Scholar]
- 83. Yagi H, Soto-Gutierrez A, Parekkadan B, Kitagawa Y, Tompkins RG, et al. (2010) Mesenchymal stem cells: mechanisms of immunomodulation and homing. Cell Transplant 19: 667–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Larrick JW, Graham D, Toy K, Lin LS, Senyk G, et al. (1987) Recombinant tumor necrosis factor causes activation of human granulocytes. Blood 69: 640–644. [PubMed] [Google Scholar]
- 85. Smith AN, Willis E, Chan VT, Muffley LA, Isik FF, et al. (2010) Mesenchymal stem cells induce dermal fibroblast responses to injury. Exp Cell Res 316: 48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Fontenot JD, Rudensky AY (2005) A well adapted regulatory contrivance: regulatory T cell development and the forkhead family transcription factor Foxp3. Nat Immunol 6: 331–337. [DOI] [PubMed] [Google Scholar]
- 87. Lange C, Togel F, Ittrich H, Clayton F, Nolte-Ernsting C, et al. (2005) Administered mesenchymal stem cells enhance recovery from ischemia/reperfusion-induced acute renal failure in rats. Kidney Int 68: 1613–1617. [DOI] [PubMed] [Google Scholar]
- 88. Choi S, Park M, Kim J, Hwang S, Park S, Lee Y (2009) The role of mesenchymal stem cells in the functional improvement of chronic renal failure. Stem Cells Dev 18: 521–529. [DOI] [PubMed] [Google Scholar]
- 89. Hara Y, Stolk M, Ringe J, Dehne T, Ladhoff J, et al. (2011) In vivo effect of bone marrow-derived mesenchymal stem cells in a rat kidney transplantation model with prolonged cold ischemia. Transpl Int 24: 1112–1123. [DOI] [PubMed] [Google Scholar]
- 90. Togel F, Weiss K, Yang Y, Hu Z, Zhang P, et al. (2007) Vasculotropic, paracrine actions of infused mesenchymal stem cells are important to the recovery from acute kidney injury. Am J Physiol Renal Physiol 292: F1626–F1635. [DOI] [PubMed] [Google Scholar]
- 91. Pino CJ, Humes HD (2010) Stem cell technology for the treatment of acute and chronic renal failure. Transl Res 156: 161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Aldinucci A, Rizzetto L, Pieri L, Nosi D, Romagnoli P, et al. (2010) Inhibition of immune synapse by altered dendritic cell actin distribution: a new pathway of mesenchymal stem cell immune regulation. J Immunol 185: 5102–5110. [DOI] [PubMed] [Google Scholar]
- 93. English K, Barry FP, Mahon BP (2008) Murine mesenchymal stem cells suppress dendritic cell migration, maturation and antigen presentation. Immunol Lett 115: 50–58. [DOI] [PubMed] [Google Scholar]
- 94. Jiang XX, Zhang Y, Liu B, Zhang SX, Wu Y, et al. (2005) Human mesenchymal stem cells inhibit differentiation and function of monocyte-derived dendritic cells. Blood 105: 4120–4126. [DOI] [PubMed] [Google Scholar]
- 95. Nauta AJ, Kruisselbrink AB, Lurvink E, Willemze R, Fibbe WE (2006) Mesenchymal stem cells inhibit generation and function of both CD34+-derived and monocyte-derived dendritic cells. J Immunol 177: 2080–2087. [DOI] [PubMed] [Google Scholar]
- 96. Lee PT, Lin HH, Jiang ST, Lu PJ, Chou KJ, et al. (2010) Mouse kidney progenitor cells accelerate renal regeneration and prolong survival after ischemic injury. Stem Cells 28: 573–584. [DOI] [PubMed] [Google Scholar]
- 97. Inoue S, Popp FC, Koehl GE, Piso P, Schlitt HJ, et al. (2006) Immunomodulatory effects of mesenchymal stem cells in a rat organ transplant model. Transplantation 81: 1589–1595. [DOI] [PubMed] [Google Scholar]
- 98. Gheisari Y, Azadmanesh K, Ahmadbeigi N, Nassiri SM, Golestaneh AF, et al. (2012) Genetic modification of mesenchymal stem cells to overexpress CXCR4 and CXCR7 does not improve the homing and therapeutic potentials of these cells in experimental acute kidney injury. Stem Cells Dev 21: 2969–2980. [DOI] [PubMed] [Google Scholar]
- 99. Gupta S, Li S, Abedin MJ, Wang L, Schneider E, et al. (2010) Effect of Notch activation on the regenerative response to acute renal failure. Am J Physiol Renal Physiol 298: F209–F215. [DOI] [PubMed] [Google Scholar]