Abstract
Francisella philomiragia is a rare gram-negative, halophilic coccobacillus with bizarre spherical forms on primary isolation. A case of F. philomiragia bacteremia in a 24-year-old patient with chronic granulomatous disease is reported. Identification of F. philomiragia was problematic with conventional tests but was done correctly and rapidly by kit 16S ribosomal DNA sequencing.
CASE REPORT
The patient was a 24-year-old man with chronic granulomatous disease (CGD). At the age of 2.5 years he was operated on for a hepatic abscess with Staphylococcus aureus. Follow-up investigations on his granulocyte function showed a profound defect in the intracellular bactericidal activity against S. aureus (Koch 1973). Repeated studies of the respiratory burst function all showed nearly complete absence of activity. Nitroblue tetrazolium tests on several occasions demonstrated less than 7% nitroblue tetrazolium-positive cells. The patient was put on prophylactic treatment with trimethoprim-sulfamethoxazole and later dicloxacillin, on which he remained well without serious infections. One month prior to the admission he was treated successfully with penicillin for pneumonia.
During a vacation in Turkey, where he had gone swimming in the sea and taken mud baths, he developed a high fever. The fever continued after his return from vacation and was accompanied by cough and expectoration. Three days before admission to the hospital he had a fever of 39°C and treatment with cefuroxime was initiated. His general condition deteriorated rapidly and he was admitted in shock at the intensive care unit with bilateral interstitial pneumonia with pleural effusion and splenomegaly. Treatment with high doses of erythromycin, ciprofloxacin, and metronidazole was initiated. The next day when gram-negative coccobacilli grew in blood cultures, the treatment was supplemented with meropenem, interferon, and filgrastim (Neupogen). The patient developed multiorgan failure and disseminated intravascular coagulation and died after 4 days. An autopsy was not performed.
Bacteriology.
The microorganism was detected in four of five aerobic FAN blood culture bottles and two of five anaerobic bottles (BactAlert; Organon Teknika, Durham, N.C.) after 4.8 to 22.7 h and 8.1 to 28.6 h of incubation at 35°C, respectively. Upon wet-mount microscopy directly from the positive blood cultures, spherical bodies with diameters of 0.5 to 3.0 μm dominated, with extremely few rod-shaped bacteria interspersed. Gram stain revealed an amorphous gram-negative mass without distinct cell forms. Upon repeated isolations on 5% horse blood agar, the number of small coccobacilli increased progressively, until they dominated. Rod-shaped forms developed faster on MWY agar (modified Wadowsky Yee Oxoid agar containing cysteine) than on 5% horse blood agar.
At 24 h colonies on 5% horse blood agar and chocolate agar were about 0.5 mm in diameter, smooth, glossy, and greyish. Growth on infusion agar and MWY agar was slower, and no growth occurred on modified Conradi-Drigalski agar.
Results of phenotypic characterization are given in Table 1. The organism was resistant to penicillin, ampicillin, and piperacillin and susceptible to cefuroxime, ceftazidime, erythromycin, trimethoprim-sulfamethoxazole, gentamicin, and ciprofloxacin (Rosco NeoSensitabs and Oxoid disks) on Danish blood agar and Iso-Sensitest agar, respectively.
TABLE 1.
Phenotypic characterization of F. philomiragia
| Test performed | Reactiona |
|---|---|
| Motility | − |
| Growth in semisolid agar | |
| 2.5% NaCl | + |
| 5% NaCl | + |
| Oxidase (Kovács) | + |
| Catalase | + |
| Indole production (Neo-Clear) | 0 |
| Beta-galactosidase (ONPGb) production | 0 |
| Urease production | 0 |
| Gelatin hydrolysis (stab) | +7d |
| Nitrate reduction | 0 |
| Arginine decarboxylase (Møller) | 0 |
| Lysine decarboxylase (Møller) | 0 |
| Ornithine decarboxylase (Møller) | 0 |
| H2S (TSI) | +7d |
| H2S (lead acetate paper) | +4d |
| Acid from (Hugh & Leifson): | |
| Glucose | (+)7d |
| Xylose | 0 |
| Mannitol | 0 |
| Maltose | (+)7d |
| Sucrose | (+)7d |
Parentheses indicate a weak reaction. Reactions that occurred after 4 or 7 days are indicated by 4d or 7d subscripts, respectively.
ONPG, o-nitrophenyl-β-d-galactopyranoside.
16S rRNA gene sequencing.
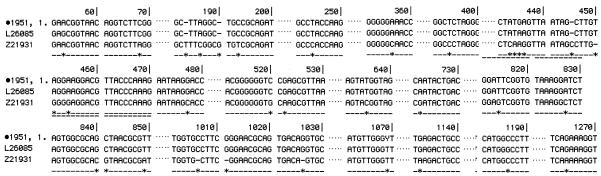
Species identification concurrent with conventional phenotypical characterization (6) was also obtained using the MicroSeq Full Gene 16S rDNA Bacterial Identification System (PE Applied Biosystems), with which 99.93% agreement was obtained with Francisella philomiragia ATCC 25015T, with a mismatch occurring in only 1 of 1,505 bp (MicroSeq Analysis Software, version 1.4.1). The MicroSeq database does not include Francisella species other than F. philomiragia. A BLAST search for sequences in GenBank gave 99.7% agreement with F. philomiragia ATCC 25015T, with a mismatch in 4 of 1,434 bp, and only 97% agreement with F. tularensis ATCC 6223T, the species with the second-best match (Fig. 1).
FIG. 1.
Alignment of the 16S rDNA sequences of F. philomiragia 1951 (GenBank AY496933), F. philomiragia ATCC 25015T (GenBank L26085), and F. tularensis ATCC 6223T (GenBank Z21931). Only regions with sequence variation are shown.
Discussion.
CGD is a group of inherited disorders characterized by defective oxidase function in the circulating phagocytes. The result is failure to produce superoxide anion and other oxygen metabolites, including H2O2, that are necessary for the killing of microorganisms in the phagocytic vacuoles. Microorganisms not producing catalase (e.g., streptococci and anaerobic bacteria) are killed normally, because their endogenous H2O2 accumulates in the phagocytic vacuoles and thereby substitutes for the lack of phagocytic H2O2 production. On the other hand, catalase-producing microorganisms (e.g.,Staphylococcus aureus, Pseudomonas aeruginosa, enteric bacilli, and Aspergillus spp.) cause infections, because they metabolize H2O2 with their own catalase, consequently impairing intraphagocytic killing (7). Several molecular defects are known to cause CGD. The most common and clinically severe type has an X-linked mode of inheritance, while other forms are inherited in an autosomal recessive manner. Variant forms with only partial lack of the oxidase activity have also been described (2).
Prophylactic treatment with trimethoprim-sulfamethoxazole plus dicloxacillin has greatly improved the prognosis of CGD patients, since it suppresses infections with most catalase-producing bacteria. This antibiotic prophylaxis is, however, not always protective, as seen in this case report.
F. philomiragia caused septic shock with multiorgan failure despite the administration of antibiotics to which the organism was sensitive (cefuroxime, ciprofloxacin, erythromycin, and meropenem) plus interferon and filgrastim.
Identification of the organism as F. philomiragia at our laboratories was difficult, i.e., due to the organism's exceptional microscopic morphology on primary isolation. This is in accordance with the original description of the bacterium (4), which states that individual cells could not be clearly distinguished by Gram staining of cultures due to production of a mucoid material but that washing with a 0.85% NaCl solution revealed coccoid organisms with a considerable number of bizarre forms and few decided rod forms. Like us, they also found that repeated isolations on solid media made the organisms more easily visible with Gram stains, revealing their small coccobacillary morphology. Another difficulty in conventional identification of the isolate was its relatively fastidious nature with slow growth giving weak and delayed reactions. Demonstration of the halophilicity would have been an almost diagnostic characteristic in this fastidious organism, but this was not demonstrated until after the identification was established by other conventional characteristics and 16S ribosomal DNA (rDNA) sequencing. Acid production from glucose, maltose and sucrose in Hugh & Leifson OF medium was very weak and not enhanced by 14 days of incubation. This is presumably due to a low NaCl content in the Hugh & Leifson formulations compared to the Difco formulations used by the Centers for Disease Control for this organism (3).
Infection with this organism was first described in 1982 (9) and has so far been reported only for a single series of 14 patients, of whom 5 suffered from CGD and the remaining from near-drowning and myeloproliferative disease (11), and in two episodes involving distinct isolates of F. philomiragia in a sixth CGD patient (8, 10).
The combination of finding fastidious growth and bizarre spherical forms with few rod shapes on wet-mount microscopy from sterile fluids from immunocompromised or near-drowning patients is probably the best clue to identification. Correct identification is presumably established most rapidly by 16S rDNA sequencing (1, 5) but can also be done by conventional characterization. With regard to the latter, the combination of halophilicity and production of oxidase and gelatinase is highly leading.
Nucleotide sequence accession number.
The 16S rRNA gene sequence of the isolate has been deposited in the GenBank sequence database under the accession number AY496933.
REFERENCES
- 1.Forsman, M., G. Sandström, and A. Sjöstedt. 1994. Analysis of 16S ribosomal DNA sequences of Francisella strains and utilization for determination of the phylogeny of the genus and for identification of strains by PCR. Int. J. Syst. Bacteriol. 44:38-46. [DOI] [PubMed] [Google Scholar]
- 2.Goldblatt, D., and A. J. Thrasher. 2000. Chronic granulomatous disease. Clin. Exp. Immunol. 122:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollis, D. G., R. E. Weaver, A. G. Steigerwalt, J. D. Wenger, C. W. Moss, and D. J. Brenner. 1989. Francisella philomiragia comb. nov. (formerly Yersinia philomiragia) and Francisella tularensis biogroup novicida (formerly Francisella novicida) associated with human disease. J. Clin. Microbiol. 27:1601-1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jensen, W. J., C. R. Owen, and W. L. Jellison. 1969. Yersinia philomiragia sp. n., a new member of the Pasteurella group of bacteria, naturally pathogenic for the muskrat (Ondatra zibethica). J. Bacteriol. 100:1237-1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johansson, A., A. Ibrahim, I. Göransson, U. Eriksson, D. Gurycova, J. E. Clarridge III, and A. Sjöstedt. 2000. Evaluation of PCR-based methods for discrimination of Francisella species and subspecies and development of a specific PCR that distinguishes the two major subspecies of Francisella tularensis. J. Clin. Microbiol. 38:4180-4185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nano, F. E. 2000. Francisella, p. 1347-1350. In L. Collier, A. Balows, and M. Sussman (ed.), Topley and Wilsons microbiology and microbial infections, 9th ed. Arnold, London, United Kingdom.
- 7.Nauseef, W. M., and R. A. Clark. 2000. Granulocytic phagocytes, p. 89-112. In G. L. Mandell, J. E. Bennett, and R. Dolun (ed.), Mandell, Douglas and Bennett's principles and practice of infectious diseases, 5th ed. Churchill Livingstone, Philadelphia, Pa.
- 8.Polack, F. P., S. M. Harrington, J. A. Winkelstein, W. G. Merz, and R. E. Willoughby. 1998. Recurrent Francisella philomiragia sepsis in chronic granulomatous disease. Pediatr. Infect. Dis. J. 17:442-443. [DOI] [PubMed] [Google Scholar]
- 9.Seger, R. A., D. G. Hollis, R. E. Weaver, and W. H. Hitzig. 1982. Chronic granulomatous disease: fatal septicemia caused by an unnamed gram-negative bacterium. J. Clin. Microbiol. 16:821-825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sicherer, S. H., E. J. Asturias, J. A. Winkelstein, J. D. Dick, R. E. Willoughby. 1997. Francisella philomiragia sepsis in chronic granulomatous disease. Pediatr. Infect. Dis. J. 16:420-422. [DOI] [PubMed] [Google Scholar]
- 11.Wenger, J. D., D. G. Hollis, R. E. Weaver, C. N. Baker, G. R. Brown, D. J. Brenner, and C. V. Broome. 1989. Infection caused by Francisella philomiragia (formerly Yersinia philomiragia). Ann. Intern. Med. 110:888-892. [DOI] [PubMed] [Google Scholar]