Abstract
A 15-year-old female with a prior history of aborted cardiac death and surgical correction of anomalous origin of the right coronary artery (RCA) presented with polymorphic ventricular tachycardia. Her electrocardiogram after defibrillation was suggestive of congenital long QT syndrome (LQTS). The patient was treated with a β-blocker and remained free from ventricular arrhythmia during the follow-up of more than 6 months. Here, we present the case of a young female with repeated aborted cardiac death accompanied by anomalous origin of the RCA and congenital LQTS for the first time.
Keywords: Long QT syndrome; Tachycardia, ventricular; Coronary vessel anomalies
Introduction
Both anomalous origin of the right coronary artery (RCA) from the left coronary cusp or congenital long QT syndrome (LQTS) are an important cause of sudden cardiac death, especially in young and healthy individuals. However, sudden cardiac death in a patient with these two disease entities has not yet been reported. Here, we report the case of a young female with repeated aborted cardiac death accompanied by anomalous origin of the RCA and congenital LQTS.
Case
A 15-year-old female with a prior history of aborted cardiac death and surgical correction of anomalous origin of the RCA was referred to the cardiology department due to repeated aborted sudden cardiac death after physical exertion with boxing. The initial electrocardiogram (ECG) showed polymorphic ventricular tachycardia (Fig. 1). Biphasic 200 joules defibrillation restored the heart to sinus rhythm and cardiopulmonary function recovered without neurologic sequelae. Two years prior to this event, she experienced chest discomfort followed by aborted sudden cardiac death after heavy exercise for the first time. Initial ECG at the emergency room showed pulseless electrical activity. She was successfully resuscitated after basic life support maneuvers and fully recovered with hypothermic treatment after being admitted to the emergency department. Her family history of structural heart disease, syncope or sudden cardiac death was unremarkable. Several cardiac examinations were performed at that time. Echocardiography demonstrated no structural heart disease with a normal left ventricular ejection fraction. Cardiac computed tomography revealed anomalous origin of the RCA from the left coronary cusp coursing between the pulmonary artery and the aorta (Fig. 2). Her follow-up ECGs after stabilization showed a sinus rhythm with an inverted T wave and a prolonged QT interval which was suggestive of congenital LQTS (Fig. 3). She was not taking any medications which can prolong the QT interval and laboratory findings did not show electrolyte abnormalities. But this finding was overlooked and anomalous origin of the RCA was provisionally considered as the cause of the aborted cardiac arrest. She underwent surgery to re-implant the anomalous RCA from the left to the right sinus of Valsalva. After receiving surgical correction of anomalous origin of the RCA, she had been doing well before the second event of aborted cardiac death developed. Coronary angiogram with a provocation test using ergonovine was done after the second event, and it revealed no significant abnormalities and the re-implantation site of the RCA ostium was intact. An electrophysiologic study was performed to rule out possible causes of other arrhythmias leading to cardiac arrest. However no other arrhythmia was induced and also polylmorphic ventricular tachycardia was not inducible with programmed stimulation. The ECG after restoring the heart to sinus rhythm showed still significant prolongation of the QT interval, resulting in the diagnosis of LQTS, probably type I, regarding her clinical presentation, even though the ECG pattern showed a prolonged QT interval and a notched T wave suggesting LQTS type 2. Gene studies were recommended, but declined by her family. ECGs of her parents showed no significant QT prolongation. Medication with a β-blocker (atenolol) was started and the dose was titrated up to 1.3 mg/kg (50 mg bid, regarding her body weight; 78 kg). A follow-up exercise tolerance test revealed blunting of the heart rate response during maximal exertion and she was instructed to avoid heavy exercise. She remained free from ventricular arrhythmias while she was on a β-blocker medication during the follow-up of more than 6 months. Her serial follow-up ECGs showed significant QTc prolongation of >500 ms consistently.
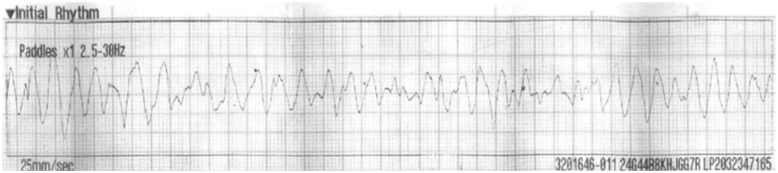
Fig. 1.
A 15-year-old female was referred to the cardiology department due to repeated aborted sudden cardiac death. Initial electrocardiogram showed polymorphic ventricular tachycardia.
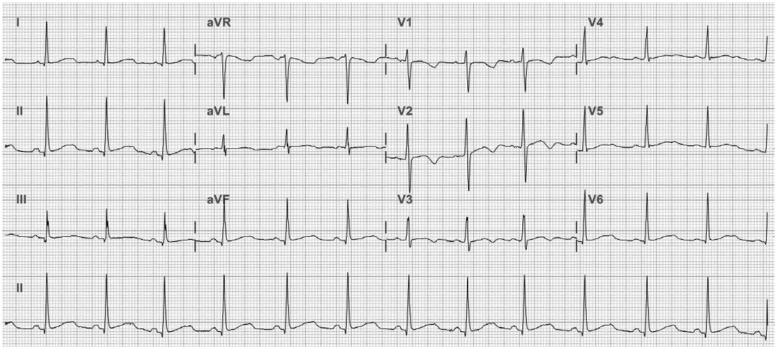
Fig. 2.
Cardiac computed tomography revealed anomalous origin of the RCA from the left coronary cusp coursing between the pulmonary artery and the aorta (white arrows). Ao: aorta, RCA: right coronary artery, PA: pulmonary artery.
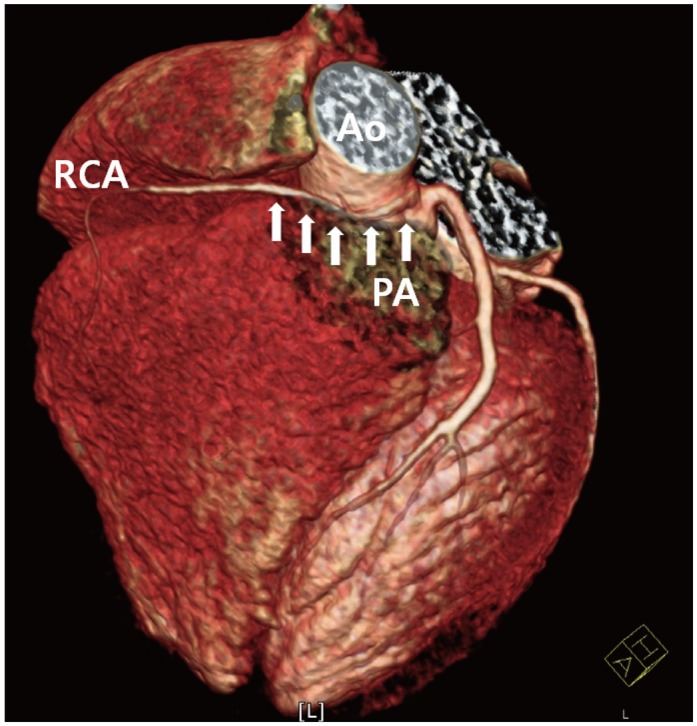
Fig. 3.
Her follow-up electrocardiogram after stabilization showed a sinus rhythm with an inverted T wave and a prolonged QT interval: 470 ms, and QTc: 531 ms, which was suggestive of congenital long QT syndrome.
Discussion
We report the case of a young female with repeated cardiac arrest accompanied by anomalous origin of the RCA and congenital LQTS. Surgical correction of the coronary anomaly was performed and the diagnosis of LQTS was made after the second episode of aborted cardiac death. The patient was treated with a β-blocker.
Congenital LQTS is a genetic disorder characterized by a prolonged QT interval and polymorphic ventricular tachycardia. Prolongation of the repolarization phase acts as a primary step for the generation of early after depolarizations (EADs) and prolonged repolarization is associated with increased spatial dispersion of repolarization in the LQTS. The focal EAD-induced triggered beats can infringe on the underlying substrate of inhomogeneous repolarization to initiate polymorphic reentrant ventricular arrhythmia.1) The features of QT prolongation on ECG can be difficult to recognize or sometimes overlooked. Although genetic testing may provide additional information, the rationale is often debatable and the diagnosis of LQTS remains a challenge. The Schwartz scoring system is widely used in clinical practice and the high probability of a clinical diagnosis gives the yield of positive genetic testing in 72%.2) We could not confirm the genotype in this patient; however, the scoring system was suggestive of a high probability of LQTS.
Coronary artery anomalies of ectopic RCA originating from the left sinus were found in approximately 0.92% in a recent prospective study.3) Anomalous origin of the RCA from the left coronary cusp which courses between the pulmonary artery and aorta can cause a malignant arrhythmia due to the potential for RCA ischemia, particularly during exertion or stress. Surgical correction of the RCA can be a definitive treatment for this condition.
Physical exertion can precipitate a ventricular arrhythmia in both conditions, even though the mechanisms are different. Also, it is possible that both conditions can interact with each other to increase the susceptibility to develop a ventricular arrhythmia. Recent studies have shown that only a long QT interval is not sufficient to provoke polymorphic ventricular tachycardia.4) Heterogeneity of repolarization throughout the transmural regions of the ventricle, which results in transmural dispersion of repolarization, is a marker of electrical instability. This enhanced transmural dispersion of repolarization allows for the propagation of multiple waves of reentry, which is responsible for polymorphic ventricular tachycardia by serving as a functional underlying reentrant substrate.5) As previously reported, the QT interval can be prolonged during the early post-infarction period.6) Furthermore, the QT interval was significantly more prolonged in patients with extensive transmural infarction.7) Thus, significant myocardial ischemia due to extrinsic compression or spasm of the RCA might exacerbate transmural dispersion of repolarization and play a role in triggering ventricular arrhythmia during the first episode of aborted sudden cardiac death in our patient with QT prolongation. However, LQTS might be solely responsible for the second episode of polymorphic ventricular tachycardia because she received definite treatment for the coronary anomaly.
Implantation of a defibrillator was considered because of repeated aborted cardiac death; however, treatment for LQTS had not been attempted before. β-blocker is relatively effective in congenital LQTS type I; therefore, a defibrillator was not placed in the patient and sympathetic denervation was not performed in this patient, who was carefully monitored instead. In conclusion, both anomalous origin of the RCA from the left coronary cusp and LQTS can coexist and interact to induce a ventricular arrhythmia. We should not overlook QT prolongation even in a patient with a diagnosis of anomalous origin of the RCA from the left coronary cusp.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.El-Sherif N, Chinushi M, Caref EB, Restivo M. Electrophysiological mechanism of the characteristic electrocardiographic morphology of torsade de pointes tachyarrhythmias in the long-QT syndrome: detailed analysis of ventricular tridimensional activation patterns. Circulation. 1997;96:4392–4399. doi: 10.1161/01.cir.96.12.4392. [DOI] [PubMed] [Google Scholar]
- 2.Tester DJ, Will ML, Haglund CM, Ackerman MJ. Effect of clinical phenotype on yield of long QT syndrome genetic testing. J Am Coll Cardiol. 2006;47:764–768. doi: 10.1016/j.jacc.2005.09.056. [DOI] [PubMed] [Google Scholar]
- 3.Angelini P. Coronary artery anomalies--current clinical issues: definitions, classification, incidence, clinical relevance, and treatment guidelines. Tex Heart Inst J. 2002;29:271–278. [PMC free article] [PubMed] [Google Scholar]
- 4.Shimizu W, Antzelevitch C. Sodium channel block with mexiletine is effective in reducing dispersion of repolarization and preventing torsade des pointes in LQT2 and LQT3 models of the long-QT syndrome. Circulation. 1997;96:2038–2047. doi: 10.1161/01.cir.96.6.2038. [DOI] [PubMed] [Google Scholar]
- 5.Kawabata M, Hirao K, Takeshi S, et al. Torsades de pointes related to transient marked QT prolongation following successful emergent percutaneous coronary intervention for acute coronary syndrome. J Electrocardiol. 2008;41:117–122. doi: 10.1016/j.jelectrocard.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Moreno FL, Villanueva T, Karagounis LA, Anderson JL TEAM-2 Study Investigators. Reduction in QT interval dispersion by successful thrombolytic therapy in acute myocardial infarction. Circulation. 1994;90:94–100. doi: 10.1161/01.cir.90.1.94. [DOI] [PubMed] [Google Scholar]
- 7.Chauhan VS, Tang AS. Dynamic changes of QT interval and QT dispersion in non-Q-wave and Q-wave myocardial infarction. J Electrocardiol. 2001;34:109–117. doi: 10.1054/jelc.2001.23116. [DOI] [PubMed] [Google Scholar]