Abstract
Background
Elevated blood pressure (BP) levels in childhood have been associated with subsequent atherosclerosis. However, it is uncertain whether this risk is attenuated in individuals who acquire normal BP by adulthood. The present study examined the effect of child and adult BP levels on carotid artery intima-media thickness (cIMT) in adulthood.
Methods and Results
The cohort consisted of 4,210 participants from four prospective studies (mean follow-up 23 years). Childhood elevated BP was defined according to the tables from the National High Blood Pressure Education Program. In adulthood BP was classified as elevated for individuals with systolic BP ≥120mmHg, diastolic BP ≥80mmHg or with self-reported use of antihypertensive medications. cIMT was measured in the left common carotid artery. High IMT was defined as an IMT ≥age-, sex-, race-, and cohort-specific 90th percentile. Individuals with persistently elevated BP and individuals with normal childhood BP, but elevated adult BP had increased risk of high cIMT (RR[95%CI]) 1.82[1.47-2.38] and 1.57[1.22-2.02], respectively) when compared to individuals with normal child and adult BP. In contrast, individuals with elevated BP as children but not as adults did not have significantly increased risk (1.24[0.92-1.67]). In addition, these individuals had lower risk of increased cIMT (0.66[0.50-0.88]) when compared to those with persistently elevated BP. The results were consistent when controlling for age, sex, adiposity and when different BP definitions were applied.
Conclusions
Individuals with persistently elevated BP from childhood to adulthood had increased risk of carotid atherosclerosis. This risk was reduced if elevated BP during childhood resolved by adulthood.
Keywords: risk factors, atherosclerosis, blood pressure, hypertension, epidemiology
INTRODUCTION
Hypertension is a major modifiable risk factor for atherosclerosis1. It was estimated that about 50% of stroke and ischemic heart disease worldwide and a total of 7.6 million deaths in 2001 were attributable to high blood pressure (BP)2. The atherosclerotic process begins in childhood. In autopsy studies, elevated childhood BP has been associated with atherosclerotic lesions3, 4. Childhood BP levels also predict increased occurrence of subclinical atherosclerosis5-9. Indeed, expert panel guidelines recommend that BP should be measured annually from the age of 3 years10. Prior reports have shown that based on multivariable models taking into account adult BP levels, childhood BP levels are significantly associated with subclinical atherosclerosis in adulthood7, 9. However, it is not precisely known if the effects of elevated BP during childhood on atherosclerotic markers are permanent or reversible should the individual acquire normal BP levels by adulthood.
Ultrasound measurement of common carotid intima-media thickness (cIMT) serves as an early marker of structural atherosclerosis. High cIMT has been shown to associate with cardiovascular risk factors and the risk of cardiovascular and cerebrovascular events11-13. Within an international consortium of cardiovascular risk factor studies initiated in childhood known as the International Childhood Cardiovascular Cohort (i3C) Consortium14, we examined data for 4,210 individuals from four cohorts to determine the combined effects of child and adult elevated BP on cIMT. The main aim was to test a hypothesis whether a change from elevated BP status in childhood to normal BP in adulthood is associated with an attenuated risk of developing increased cIMT.
METHODS
Study Cohorts
Data from four prospective cohort studies conducted in the United States (Bogalusa Heart Study, Muscatine Study), Finland (Cardiovascular Risk in Young Finns Study), and Australia (Childhood Determinants of Adult Health (CDAH) Study) were analyzed. In all cohorts, analyses included participants who had a baseline evaluation during childhood and who also attended a follow-up examination as an adult. In cohorts that conducted several childhood examinations, data from the earliest examination were used. In adulthood, data from the latest available exam were utilized in Bogalusa, Young Finns and CDAH, whereas in Muscatine the first adult study with IMT measures was used to provide as similar follow-up period as possible.
Descriptions of these cohorts, including attrition analyses, have been previously been published3, 7, 14-19. All blood biochemical values were measured from fasting samples. Korotkoff’s first phase was used to define systolic and fifth phase to define diastolic BP. Height and weight were measured during field studies. Smoking habits were assessed with questionnaires in childhood and adulthood (Muscatine only in adulthood)20. Each study received ethical approval from the appropriate institutional review boards, and obtained informed consent from the study participants or parents.
The Muscatine Study
Study sample
For this analysis, 721 representative individuals who had previously participated in at least one childhood examination between 1970-198121, and in the 1996-99 adult follow-up (aged 33-45 years) when cIMT was measured were included.
Clinic measurements
Baseline BP was measured using standard mercury sphygmomanometers; follow-up measures were obtained using a Hawksley random-zero sphygmomanometer (GelmanHawksley Limited, Sussex, England). All measurements were taken on the right arm, before venipuncture, and after the participant had been seated for five minutes. The mean of three measurements was used for analysis.
Carotid artery ultrasound
Carotid ultrasound studies were performed by a single technician using the Biosound Phase 2 ultrasound machine and a 10-MHz transducer (Biosound Esaote Inc., Indianapolis, IN) 15. A 4.4% random sample underwent repeat carotid ultrasound studies during a second visit, a mean of 107 days later, to assess intra-individual reproducibility. The mean absolute difference for all cIMT segments was 0.06mm15.
The Bogalusa Heart Study
Study sample
For this analysis, 586 individuals who had BP measured in either the 1981-83, 1984-85, or 1987-88 youth surveys (when aged 4-17-years) and BP and cIMT measured in either the 2001-02 or 2003-07 adult surveys (then aged 23-42-years) were included.
Clinic measurements
BP measurements at baseline and follow-up were obtained on the right arm, after venipuncture with participants in a relaxed sitting position. Three BP readings were taken by each of two randomly assigned observers for a total of six measurements. The mean of the six replicate readings was used in the analyses. In childhood, those reporting smoking at least one cigarette per week were defined as regular smokers.
Carotid artery ultrasound
B-mode ultrasound examinations of the carotid arteries were performed at the 2001-02 and 2003-07 follow-ups using a Toshiba Sonolayer SSH160A ultrasound machine with a 7.5-MHz linear array transducer (Toshiba Medical, Tokyo, Japan) 16. Seventy-five participants underwent repeat ultrasound examinations 10-12 days after their initial visit to determine intra-individual reproducibility. The mean absolute difference and standard deviation (SD) between measurements for all cIMT segments was 0.05±0.03 mm.
The Cardiovascular Risk in Young Finns Study
Study Sample
For this analysis, 2,223 participants who were 6-18 years old at baseline in 1980 and who had BP measured in childhood and cIMT and BP measured in 2001 or 2007 (27-45 years) were included. Participants aged 3 years at baseline were not included because BP measures were collected using an ultrasound device.
Clinic measurements
BP was measured using a standard mercury sphygmomanometer at baseline and using a random zero sphygmomanometer (Hawksley&Sons Ltd, Lancin, UK) at follow-up. All measurements were taken on the right arm, before venipuncture (among adults after venipuncture) and after the participant had been seated for five minutes. Readings to the nearest even number of millimeters of mercury were performed at least three times on each participant. The mean of these three measurements was used in the analyses. Socioeconomic position in childhood was assessed by questionnaires20. Baseline pubertal status was assessed by Tanner staging and categorized as not started, on-going or finished. In childhood, those reporting smoking daily or weekly were defined as regular smokers.
Carotid Artery Ultrasound Studies
B-mode ultrasound studies of the left carotid artery were performed at both 2001 and 2007 follow-ups using an Acuson Sequoia 512 ultrasound machine with a 13-MHz linear-array transducer (Siemens Medical Solutions USA Inc., Mountainview, CA) 7. To assess intra-individual reproducibility of ultrasound measurements, 57 participants were re-examined 3 months after their initial visit. The average absolute difference and SD between measurements was 0.05±0.04 mm.
The Childhood Determinants of Adult Health (CDAH) Study
Study sample
For this analysis, data were included from 680 individuals who had BP measured in the 1985 baseline survey (when aged 9-15 years) and cIMT and BP measured in the 2004-06 adult follow-up survey (27-36-years).
Clinic measurements
BP measurements were obtained from the left brachial artery, before venipuncture, using a standard mercury sphygmomanometer at baseline. All measurements were taken after the participant had been seated for five minutes. This procedure was repeated after five minutes, and the mean of the two measurements was used in the analyses. At follow up, BP was measured from the right brachial artery, after venipuncture, using a digital automatic monitor (Omron Corporation, Kyoto, Japan). The mean of the three consecutive measurements separated by a one-minute interval was used in the analyses. Participants retrospectively reported the highest level of education completed by their guardian20. Smoking in childhood was assessed using a question: How long have you been smoking regularly?
Carotid artery ultrasound
B-mode ultrasound studies of the carotid artery were performed using a portable Acuson Cypress ultrasound machine with a 7.0-MHz linear-array transducer (Siemens Medical Solutions USA Inc., Mountainview, CA)22. Intra-individual reproducibility for replicate max cIMT measurements was assessed in a random sample of 30 participants. The average absolute difference and SD between measurements was 0.02±0.04 mm.
Classification of BP levels
Elevated BP in childhood was defined according to BP tables issued by the National High Blood Pressure Education Program (NHBPEP)23 and in adulthood according to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood pressure24. BP status in youth was classified as normal if systolic and diastolic BP (fifth phase) were <90th percentile for age, sex, and height using the NHBPEP tables, and elevated if systolic or diastolic BP were ≥90th percentile. BP status in adulthood was classified as normal if systolic BP<120mmHg and diastolic BP<80mmHg, and elevated if systolic BP≥120mmHg or diastolic BP≥80mmHg. In addition, adult BP status was considered elevated among those self-reporting use of antihypertensive medications.
Four groups based on childhood and adult BP levels were defined for comparison of outcomes: (1) Control group – participants who had a normal BP in childhood and normal BP as an adult; (2) Resolution group – participants who had elevated BP in childhood but not as an adult; (3) Incident group – participants with a normal BP in childhood who had elevated BP as an adult; and (4) Persistent group – participants who had elevated BP in childhood and as an adult.
Definition and classification of high cIMT in adulthood
The maximum cIMT measurement from the far wall of the left common carotid artery was chosen since it was the most consistent cIMT measurement across the cohorts25. Additional analyses performed using average cIMT values (CDAH and Young Finns cohorts) or data from the left and right carotid arteries (Muscatine and Bogalusa cohorts) gave essentially similar results (data not shown). In line with our previous reports, percentile points stratified by age, sex, race (Bogalusa) and cohort were first calculated and those with a maximum cIMT ≥90th percentile were classified as having high cIMT20, 25, 26. In individual cohorts, IMT cut-points in different age-, sex-, and race-groups varied as follows: Muscatine, 0.804-0.927 mm; Bogalusa, 0.796-1.110 mm; YF, 0.672-0.920 mm; CDAH, 0.660-0.825 mm.
Statistical Analyses
Comparisons of characteristics among the cohorts were conducted using chi-square tests or analysis of variance.
Relative risks (RR) and 95% confidence intervals (CI) were calculated using Poisson regression with robust standard errors to examine the associations between child-adult BP groups and adult high cIMT. All analyses were adjusted for length of follow-up, cohort and race (five cohort/race groups: Muscatine, Bogalusa whites, Bogalusa blacks, Young Finns, and CDAH), and adult body mass index (BMI, calculated as weight(kg)/[height(m)2]. Those analyses that were not stratified by age or sex were adjusted for these factors. Both data pooling and random-effects meta-analysis27, 28 techniques were used. In addition, a linear trend over BP groups was tested with a regression analysis. Cohort×BP, sex×BP, and age×BP group interaction effects on high cIMT were tested. There were no significant interaction effects.
Several sensitivity analyses were performed to examine the influence of different child and adult BP definitions, sex, age and adiposity status on the magnitude of the associations. In cohorts with relevant available data, pooled analyses were re-run after additional adjustment for smoking status (Bogalusa, Young Finns, and CDAH), socioeconomic status (Young Finns, CDAH) and pubertal status (Young Finns) in childhood.
In order to examine the influence of BMI on change in BP status between childhood and adulthood, we present mean (SD) change in BMI (adult minus child) of age-, sex-, cohort-, and race-specific (Bogalusa) z-scores for each BP group (control, resolution, incident, and persistent). Logistic regression analysis was used to examine differences between the control group and the remaining BP groups. The logistic regression models were adjusted for length of follow-up for analyses stratified by cohort and additionally adjusted for cohort in pooled analyses.
Statistical analyses were performed using STATA-10 and SAS 9.1.3. Statistical significance was inferred at a 2-tailed P-value <0.05, without adjustment for multiple comparisons.
RESULTS
Data for 4,210 participants (Table 1)29 with mean follow-up interval of 23 years were available. 1,632 (39%) participants in childhood and 2,078 (49%) participants in adulthood had elevated BP. Among children with normal or elevated BP, 42% and 60% respectively had elevated BP as adults (Supplemental Table 1). In all cohorts, significant tracking was observed between child and adult BP levels (Supplemental Table 2).
Table 1.
Child and adult characteristics of participants in the four cohorts.
| Muscatine | Bogalusa | Young Finns | CDAH | P-value* | |
|---|---|---|---|---|---|
| N (males/females) | 721 (345/376) | 586 (234/352) | 2,223 (1,004/1,219) | 680 (315/365) | 0.03 |
| Childhood | |||||
| Age, y | 14.6 (1.9) | 12.5 (3.4) | 12.0 (4.2) | 11.9 (2.4) | <0.001 |
| Age range, y | 8–18 | 4–18 | 6–18 | 9–15 | |
| Blacks, N(%) | - | 209 (35.7) | - | - | |
| Height, cm | 163.4 (10.2) | 153.3 (17.6) | 149.4 (20.2) | 151.3 (14.5) | <0.001 |
| Systolic BP, mm Hg | 116.9 (12.7) | 106.9 (10.8) | 114.1 (11.3) | 109.3 (12.9) | <0.001 |
| Diastolic BP, mm Hg | 68.8 (10.9) | 55.9 (11.6) | 68.7 (9.6) | 66.4 (11.8) | <0.001 |
| BP status, N(%) | |||||
| Normal | 437 (60.6) | 534 (91.1) | 1151 (51.8) | 456 (67.1) | |
| Elevated | 284 (39.4) | 52 (8.9) | 1072 (48.2) | 224 (32.9) | <0.001 |
| BMI, kg/m2 | 21.4 (3.4) | 19.9 (4.3) | 18.3 (3.1) | 18.6 (2.9) | <0.001 |
| BMI status, N(%) | |||||
| Normal | 573 (79.5) | 454 (77.7) | 2017 (90.8) | 603 (88.7) | |
| Overweight | 121 (16.8) | 88 (15.1) | 173 (7.8) | 62 (9.1) | |
| Obese | 27 (3.7) | 42 (7.2) | 31 (1.4) | 15 (2.2) | <0.001 |
| Regular smoking, N(%) | - | 55 (15.0) | 157 (12.5) | 71 (10.6) | 0.12 |
| Adulthood | |||||
| Age, y | 38.6 (2.9) | 33.9 (3.6) | 38.0 (4.8) | 31.8 (2.5) | <0.001 |
| Age range, y | 33–46 | 23–42 | 27–45 | 27–36 | |
| Systolic BP, mm Hg | 113.8 (11.8) | 115.7 (14.4) | 120.8 (14.3) | 118.2 (13.0) | <0.001 |
| Diastolic BP, mm Hg | 74.0 (9.7) | 77.8 (10.6) | 75.7 (11.4) | 72.7 (9.5) | 0.06 |
| BP status, N(%) | |||||
| Normal | 450 (62.4) | 322 (55.0) | 999 (44.9) | 361 (53.1) | |
| Elevated | 271 (37.6) | 264 (45.1) | 1224 (55.1) | 319 (46.9) | <0.001 |
| BMI, kg/m2 | 28.2 (5.8) | 30.2 (7.9) | 26.1 (4.8) | 25.8 (4.9) | <0.001 |
| BMI status, N(%) | |||||
| Normal | 235 (32.6) | 173 (29.5) | 1023 (46.2) | 328 (50.4) | |
| Overweight | 245 (34.0) | 161 (27.5) | 795 (35.9) | 221 (34.0) | |
| Obese | 241 (33.4) | 252 (43.0) | 395 (17.9) | 102 (15.7) | <0.001 |
| cIMT, mm | 0.71 (0.15) | 0.74 (0.16) | 0.67 (0.10) | 0.60 (0.10) | <0.001 |
| Length of follow-up, y | 24.0 (2.1) | 21.4 (1.5) | 26.0 (2.2) | 19.9 (0.6) | 0.009 |
Values are mean (SD) for continuous variables or N(%) for dichotomous variables unless stated otherwise. Abbreviations: BMI, body mass index; BP, blood pressure; CDAH, Childhood Determinants of Adult Health; cIMT, carotid intima-media thickness. In childhood, overweight and obesity were defined using international cut-points.29 In adulthood, a cut-point of 25 kg/m2 was used to define overweight and 30 kg/m2 for obesity. Child BP was classified as elevated if systolic or diastolic BP were ≥90th percentile using the NHBPEP tables for age, sex, and height. Adult BP was classified as elevated if systolic BP≥120mmHg, diastolic BP≥80mmHg or if individual self-reported use of antihypertensive medications.
P-values are for comparisons across cohorts, with the use of linear regression and χ2 tests
Influence of childhood and adult elevated BP on cIMT
Pooled Analyses
The risk of high cIMT among participants whose elevated BP resolved by adulthood was not significantly different from those in the control group (Table 2). Risks were higher among participants who had elevated BP in adulthood (incident and persistent groups) compared with the control group. Individuals in the resolution group had lower risk of increased cIMT (RR 0.66, 95% CI 0.50-0.88) when compared to those with persistently elevated BP. In linear regression analyses, a significant trend over BP groups was observed in age-stratified, sex-stratified and pooled data (P always <0.05).
Table 2.
Relative risks (RR) and 95% confidence intervals (95%CI) of high cIMT (≥90th percentile) according to blood pressure (BP) group* in childhood and adulthood (age 23-46 years, mean follow-up 23 years).
| Participants 4-11 years | Participants 12-18 years | Males | Females | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Child-adult BP group | n/N | RR | (95%CI) | P | n/N | RR | (95%CI) | P | n/N | RR | (95%CI) | P | n/N | RR | (95%CI) | P |
| Control | 35/457 | 1.00 | ref | ref | 74/983 | 1.00 | ref | ref | 31/471 | 1.00 | ref | ref | 78/969 | 1.00 | ref | ref |
| Resolution | 20/224 | 1.07 | (0.63–1.82) | 0.80 | 40/409 | 1.29 | (0.89–1.86) | 0.18 | 15/172 | 1.33 | (0.74–2.39) | 0.34 | 45/461 | 1.20 | (0.85–1.71) | 0.31 |
| Incident | 36/294 | 1.42 | (0.89–2.27) | 0.14 | 107/765 | 1.67 | (1.24–2.24) | 0.001 | 84/645 | 1.66 | (1.11–2.48) | 0.01 | 59/414 | 1.54 | (1.10–2.16) | 0.01 |
| Persistent | 46/300 | 1.63 | (1.08–2.48) | 0.02 | 109/669 | 1.96 | (1.45–2.63) | <0.001 | 91/573 | 1.99 | (1.34–2.96) | 0.001 | 64/396 | 1.79 | (1.29–2.47) | <0.001 |
All analyses adjusted for length of follow-up, cohort, race, and adult BMI. The age-stratified model additionally adjusted for sex; the sex-stratified model additionally adjusted for age; and the ‘All’ model additionally adjusted for both age and sex.
Child BP was classified as elevated if systolic or diastolic BP were ≥90thpercentile using the NHBPEP tables for age, sex, and height. Adult BP was classified as elevated if Systolic BP≥120mmHg or Diastolic BP≥80mmHg. In addition, adult BP status was considered elevated among those self-reporting use of antihypertensive medications. BP groups were: control group –normal BP in childhood and normal BP as adults; resolution group –elevated BP in childhood but not as adults; incident group –normal BP in childhood, but elevated BP as adults; and persistent group –elevated BP in childhood and as adults.
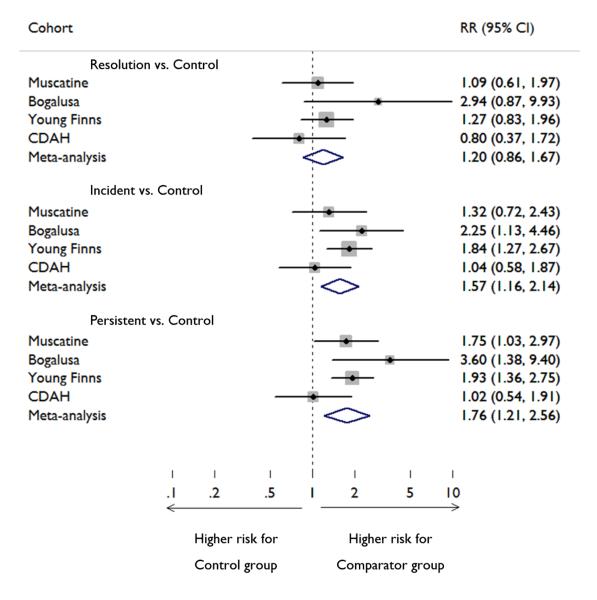
Meta-Analysis
The meta-analysis results are shown in Figure 1. The results were similar to those observed using pooled analyses. Although there were some between-cohort differences in effects, notably CDAH showing no difference between any of the comparator groups with the control group, heterogeneity was non-significant.
Figure 1.
Forest plots showing relative risk of high carotid intima media thickness (cIMT) in four cohorts. Data were analyzed from four studies — the Muscatine Study, the Bogalusa Heart Study, the Cardiovascular Risk in Young Finns Study, and the Childhood Determinants of Adult Health (CDAH) Study. In each individual study cohort and in a meta-analysis of all four cohorts, the risk of high cIMT (≥90th percentile for age-, sex-, race-, study-year–, and cohort-specific values) is shown. Child blood pressure (BP) was classified as elevated if systolic or diastolic BP were ≥90thpercentile using the NHBPEP tables for age, sex, and height. Adult BP was classified as elevated if Systolic BP≥120mmHg or Diastolic BP≥80mmHg. In addition, adult BP status was considered elevated among those self-reporting use of antihypertensive medications. Participants who had a normal blood pressure (BP) in childhood and had normal BP as adults (Control) were compared with participants who had elevated BP in childhood but not as adults (Resolution), participants with a normal BP in childhood who had elevated BP as adults (Incident), and participants who had elevated BP in childhood and as adults (Persistent). The size of each box is proportional to the weight of the cohort in the meta-analysis. The diamonds represent the relative risks estimated from the meta-analysis, with the lateral points indicating the 95% confidence intervals. The P values for heterogeneity among groups were 0.34 for the comparison of Resolution with Control, 0.27 for the comparison of Incident with Control, and 0.15 for the comparison of Persistent with Control, suggesting that there was no dissimilarity among cohorts
Sensitivity Analyses
Sensitivity analyses that used alternate BP status definitions were consistent with the observation that the risk of high cIMT among the resolution group was not significantly different from the risk among the control group (Supplemental Tables 3 and 4). For example, in analyses using more stringent BP cut-offs (≥95th percentile using the NHBPEP tables in childhood and ≥140/90 in adulthood), the RR (95% CI) values in comparisons with control group were 1.22 (0.96-1.54) for resolution group, 1.33 (1.04-1.71) for incident group and 1.94 (1.45-2.61) for persistent group.
Findings were consistent in analyses stratified by age, sex or adiposity status (Table 2, Supplemental Table 5). The results were not altered when analyzed without race-adjustment (data not shown) or using different IMT cut-points (Supplemental Table 6). Data from the Bogalusa, Young Finns, and CDAH cohorts allowed us to determine the independence of the observed effects after accounting for child smoking, SES and puberty. The findings were not altered after inclusion of these variables (data not shown). The analyses were also repeated after exclusion of those individuals using antihypertensive medication (N=254, 6.0% of the whole cohort) with essentially similar findings.
Interactions between adiposity and BP status
To assess the effect of BMI on BP values from childhood to adulthood, change in BMI z-score was calculated and examined across BP groups (Table 3). In pooled analyses, BMI z-score in the resolution group significantly decreased between childhood and adulthood compared to the control group. For the incident and persistent groups, BMI z-score significantly increased between childhood and adulthood. As illustrated in Supplemental Table 7, changes in adiposity status from childhood to adulthood paralleled BP status changes.
Table 3.
Change in BMI z-score between childhood (4–18 years) and adulthood (age 23–46 years, mean follow-up 23 years) according to blood pressure (BP) groups
| BP group | ||||||||
|---|---|---|---|---|---|---|---|---|
| Control | Resolution | Incident | Persistent | |||||
| Cohort | N | mean (SD) | N | mean (SD) | N | mean (SD) | N | mean (SD) |
| Muscatine | 307 | −0.04 (0.74) | 146 | −0.23 (0.82)* | 128 | 0.30 (1.04)† | 137 | 0.05 (0.97) |
| Bogalusa | 307 | −0.06 (0.73) | 22 | −0.18 (0.94) | 224 | 0.04 (0.90) | 28 | −0.01 (1.01) |
| Young Finns | 635 | −0.07 (0.86) | 401 | −0.21 (0.94)* | 513 | 0.28 (0.91)† | 670 | 0.05 (1.03)* |
| CDAH | 248 | 0.09 (0.83) | 97 | −0.18 (0.86)* | 193 | 0.20 (0.95) | 119 | 0.16 (0.90) |
| All | 1497 | −0.03 (0.81) | 666 | −0.21 (0.90)† | 1058 | 0.22 (0.93)† | 954 | 0.06 (1.01)* |
Child BP was classified as elevated if systolic or diastolic BP were ≥90thpercentile using the NHBPEP tables for age, sex, and height. Adult BP was classified as elevated if Systolic BP≥120mmHg or Diastolic BP≥80mmHg. In addition, adult BP status was considered elevated among those self-reporting use of antihypertensive medications. BP groups were: control group –normal BP in childhood and normal BP as adults; resolution group –elevated BP in childhood but not as adults; incident group –normal BP in childhood, but elevated BP as adults; and persistent group –elevated BP in childhood and as adults.
P<0.05
P<0.01for comparisons between control (reference group) and resolution, incident, and persistent groups using logistic regression adjusted for length of follow-up in cohort stratified analyses and additionally for cohort in pooled analyses
DISCUSSION
The main finding of the pooled analyses from four prospective cohort studies was that among individuals with elevated BP in childhood and normal BP in adulthood the risk of increased cIMT in adulthood was somewhat higher (RR 1.2), but not significantly increased compared to those with persistently normal BP. In contrast, adults with elevated BP, irrespective of their childhood BP status, had significantly increased risk of high cIMT. These results were consistently demonstrated in meta-analysis of the data, in both sexes, and across different age and adiposity groups.
In prior analyses in the Muscatine Study15, the Bogalusa Heart Study16 and the Young Finns Study7, childhood BP levels predicted increased adult cIMT. In the Young Finns Study7, 9, analyses using continuous BP data showed that in 12-18 year old individuals the association between childhood BP levels and adult cIMT or coronary calcification remained significant after adjustment for adult BP levels or BP change between childhood and adulthood. In addition, in other cohort studies elevated BP in childhood and adolescence has been linked with cardiovascular morbidity and premature death.30-32 In the present analyses conducted in four cohorts using categorically-defined BP levels, the risk of high cIMT was not significantly increased among adolescents aged 12-18 years with elevated BP only in childhood, even though the risk increase in this age group approached 30% and was higher than among children aged 4-9 years. These results suggest that the effects of elevated BP in childhood on early atherosclerosis can be mostly reversed if normal BP levels are achieved by adulthood. However, as the lower limit of the 95% confidence interval was close to 1 in some analyses comparing resolution and control groups, the independent effect of elevated childhood BP cannot be definitely ruled out. Concerning the reversibility of childhood risk factor effects, we20 previously reported that overweight or obese children who become non-obese adults have a mainly similar adult risk profile as those who were never obese. However, childhood adiposity had some residual effect on hypertension risk. Tirosh et al.33 observed among a cohort of over 37,000 apparently healthy males that BMI measured at a mean age of 17 years, independent of adult BMI, was associated with later risk of coronary heart disease, but not diabetes.
Our findings suggest that the effects of elevated childhood BP on cIMT are not completely permanent, as those individuals with resolution of increased BP did not have significantly increased adult cIMT. While it might be tempting to interpret these data by downplaying the importance of childhood elevated BP, it is necessary to consider that elevated child BP is the strongest predictor of adult hypertension34 and that once elevated BP is established it is difficult to reverse – as was highlighted in our results with only 40% of youth with elevated BP able to avoid having elevated BP as adults. We observed significant tracking of BP levels within all cohorts, and the risk of elevated adult BP was dependent on childhood BP status. Adiposity status is known to have a substantial effect on both BP levels and accelerated atherosclerosis. We previously observed that especially adult BMI levels are associated with elevated BP and increased carotid IMT20. Therefore, we conducted several analyses to take into account the effect of adiposity. First, the main analyses were adjusted for adult BMI levels. Second, analyses were performed separately in normal weight and overweight/obese participants with essentially similar results. These results support the view that the markedly reduced risk for high cIMT among the BP resolution group is independent of adiposity status. However, we found support for weight management by observing the most favorable changes in adiposity levels between childhood and adulthood among the BP resolution group. Clearly maintaining normal BMI and normal BP throughout life is preferred, and maintaining low or optimum risk status throughout life is associated with a very low lifetime risk of CVD35. However, these results suggest that when increased BMI or BP are detected in childhood or adolescence, interventions should be implemented to reduce risk of atherosclerosis development in adulthood, as persistence of these risk factors is associated with increased carotid IMT. These results are limited in that they do not demonstrate the optimum timing (age) of risk factor improvement or whether more aggressive treatment of elevated BP in childhood with medication would be beneficial. Future research should focus on these questions.
Using the NHBPEP tables, there were considerable differences in childhood prevalence of elevated BP. In the Muscatine, Young Finns, and CDAH cohorts (on the order of 33-49%) prevalence was far higher than what would be expected based on the definition coinciding with the 90th percentile within the NHANES data (on which the NHBPEP tables were based). Population, secular, and/or method differences (e.g., a different number of BP measurements to derive mean values) may have contributed to this disparity. For example, Muscatine, Young Finns, and CDAH participants are predominantly of white European descent whereas NHANES measured participants of all ethnicities represented in the USA. These findings should be considered while using the tables in the clinical setting. Sensitivity analyses using a definition for elevated childhood BP as diastolic or systolic BP ≥90th percentile according to age-, sex-, height-, and cohort-specific levels (Supplemental Table 3) which provided similar results suggests the validity of our main findings. Although there was no statistically significant heterogeneity among the cohorts, the findings from the CDAH study were somewhat different from others as the risk of high cIMT was not increased in the incident high BP or persistent high BP groups. In line, in our previous analyses concerning the link between childhood obesity and adult cIMT, the association was non-significant and weakest in the CDAH study20. The most likely explanation for this is that carotid imaging in CDAH was performed using a portable ultrasound equipment with lower resolution compared to other studies22.
Potential limitations of our study should be considered. First, as the cohorts were comprised of young adults at follow-up, we were not able to study associations with cardiovascular events. Instead we used cIMT as a surrogate end-point. Our main analyses were performed using a maximal measure of left common carotid artery, the most consistent cIMT measurement across the cohorts25. Ideally average measures of both carotid arteries would have been used in the analyses. Only Bogalusa and Muscatine studies had measures from both the left and right sides. Additional analyses using data from both sides in these cohorts showed essentially similar results compared to the main analyses. Concerning cardiovascular event prediction, Polak et al. 13 have shown that both common and internal carotid IMT measures predict cardiovascular outcomes, but only internal carotid data improves the classification of risk of cardiovascular disease. However, prior reports have shown that BP is more strongly related to the cIMT in the common segment than in other segments36 and the common segment rarely has any raised plaque37. Second, BP measurements were only taken from a single time-point in childhood and again in adulthood. However, in the Young Finns cohort we have previously shown that concerning the association between childhood BP and adult cIMT, single childhood measurements seem to be nearly as informative as repeated measurements7. Third, although the RRs indicated some residual effect of elevated child BP, the differences between resolution and control groups were not statistically significant among a total cohort of 4,210 participants. Therefore the possibility of limited power in our analyses has to be taken into account while interpreting these findings. Fourth, during the time of baseline examinations the prevalence of overweight or obesity was lower than contemporary children, and given the link between obesity and BP the results might not be completely generalized to today’s children. Finally, as study participants were predominantly Caucasian, the results should be generalized to other ethnicities with caution. The main strength is the opportunity to combine data from four longitudinal cohorts around the world. The pooled analyses allowed comparisons between different BP groups whereas in separate cohorts there would have been insufficient statistical power.
Conclusions
Our analyses from four longitudinal childhood cohort studies showed that the effect of elevated BP in childhood on carotid atherosclerosis as assessed by cIMT is markedly reduced if these individuals become normotensive adults.
Supplementary Material
Clinical Perspective.
Hypertension is a major modifiable risk factor for atherosclerosis. The atherosclerotic process begins in early life, and blood pressure (BP) levels in childhood predict increased occurrence of subclinical atherosclerosis. However, it is not precisely known if the effects of elevated BP during childhood on atherosclerotic markers are permanent or reversible should the individual acquire normal BP levels by adulthood. Within an international consortium of cardiovascular risk factor studies initiated in childhood known as the International Childhood Cardiovascular Cohort (i3C) Consortium, we examined data for 4,210 individuals from four cohorts to determine the combined effects of child and adult elevated BP on carotid intima-media thickness (cIMT, a preclinical marker of atherosclerosis). The main aim was to examine whether a change from elevated BP status in childhood to normal BP in adulthood is associated with an attenuated risk of developing increased cIMT. In pooled analyses of the cohorts, among individuals with elevated BP in childhood and normal BP in adulthood the risk of increased cIMT in adulthood was not significantly increased (RR=1.24, 95%CI=0.92-1.67) compared with those who had persistently normal BP. In contrast, adults with elevated BP, irrespective of their childhood BP status, had significantly increased risk of high cIMT with relative risks of 1.82 (95%CI=1.47-2.38) among those with persistently elevated BP and 1.57 (95%CI=1.22-2.02) among those with elevated BP only in adulthood. These results suggest that the effects of elevated BP in childhood on early atherosclerosis can be mostly reversed if normal BP levels are achieved by adulthood.
Acknowledgments
Funding Sources: These analyses were supported by funding from the individual studies. The Muscatine Study was supported by grants from the National Heart, Lung, and Blood Institute (HL-14230 and HL-54730), and the General Clinical Research Centers Program (RR-00059) of the NIH. The Bogalusa Heart Study is supported by grants AG-16592 from the National Institute on Aging and ES-021724 from National Institute of Environmental Health Science. The Cardiovascular Risk in Young Finns Study was supported by grants from the Academy of Finland (121584, 126925, 124282, 129378), the Social Insurance Institution of Finland, the Turku University Foundation, Special Federal Grants for University Hospitals, the JuhoVainio Foundation, PaavoNurmi Foundation, the Finnish Foundation of Cardiovascular Research, Orion-Farmos Research Foundation, the Ida Montin Foundation, and the Finnish Cultural Foundation. The Childhood Determinants of Adult Health study was supported at baseline by the Commonwealth Departments of Sport, Recreation and Tourism, and Health; the National Heart Foundation; and the Commonwealth Schools Commission and at follow-up by the National Health and Medical Research Council, the Heart Foundation, the Tasmanian Community Fund, and Veolia Environmental Services. Authors from the Murdoch Children’s Research Institute are supported by the Victorian Government Operational Infrastructure Support Program. CGM, AV and MAS are supported by fellowships from the National Health & Medical Research Council (Australia).
Footnotes
Conflicts of Interest Disclosures: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L, INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 2.Lawes CM, Vander HS, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 3.Berenson GS, Srinivasan SR, Bao W, Newman WP, III, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338:1650–6. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 4.McGill HC, Jr., McMahan CA, Zieske AW, Malcom GT, Tracy RE, Strong JP. Effects of nonlipid risk factors on atherosclerosis in youth with a favorable lipoprotein profile. Circulation. 2001;103:1546–50. doi: 10.1161/01.cir.103.11.1546. [DOI] [PubMed] [Google Scholar]
- 5.Sorof JM, Alexandrov AV, Garami Z, Turner JL, Grafe RE, Lai D, Portman DJ. Carotid ultrasonography for detection of vascular abnormalities in hypertensive children. Pediatr Nephrol. 2003;18:1020–4. doi: 10.1007/s00467-003-1187-0. [DOI] [PubMed] [Google Scholar]
- 6.Lande MB, Carson NL, Roy J, Meagher CC. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40–4. doi: 10.1161/01.HYP.0000227029.10536.e8. [DOI] [PubMed] [Google Scholar]
- 7.Raitakari OT, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N, Järvisalo MJ, Uhari M, Jokinen E, Rönnemaa T, Åkerblom HK, Viikari JSA. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood - The Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–83. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 8.Juonala M, Viikari JSA, Rönnemaa T, Helenius H, Taittonen L, Raitakari OT. Elevated blood pressure in adolescent boys predicts endothelial dysfunction: The Cardiovascular Risk in Young Finns Study. Hypertension. 2006;48:424–30. doi: 10.1161/01.HYP.0000237666.78217.47. [DOI] [PubMed] [Google Scholar]
- 9.Hartiala O, Magnussen CG, Kajander S, Knuuti J, Ukkonen H, Saraste A, Rinta-Kiikka I, Kainulainen S, Kähönen M, Hutri-Kähönen N, Laitinen T, Lehtimäki T, Viikari JS, Hartiala J, Juonala M, Raitakari OT. Adolescence risk factors are predictive of coronary artery calcification at middle age: the cardiovascular risk in young Finns study. J Am Coll Cardiol. 2012;60:1364–70. doi: 10.1016/j.jacc.2012.05.045. [DOI] [PubMed] [Google Scholar]
- 10.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: summary report. Pediatrics. 2011;128(suppl 5):S213–S256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 12.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic rreview and meta-analysis. Circulation. 2007;115:459–67. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 13.Polak JF, Pencina MJ, Pencina KM, O’Donnell CJ, Wolf PA, D’Agostino RBS. Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. 2011;365:213–21. doi: 10.1056/NEJMoa1012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dwyer T, Sun C, Magnussen CG, Raitakari OT, Schork NJ, Venn A, Burns TL, Juonala M, Steinberger J, Sinaiko AR, Prineas RJ, Davis PH, Woo JG, Morrison JA, Daniels SR, Chen W, Srinivasan SR, Viikari JS, Berenson GS. Cohort Profile: The International Childhood Cardiovascular Cohort (i3C) Consortium. Int J Epidemiol. 2013;42:86–96. doi: 10.1093/ije/dys004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation. 2001;104:2815–9. doi: 10.1161/hc4601.099486. [DOI] [PubMed] [Google Scholar]
- 16.Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, Berenson GS. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290:2271–6. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 17.Magnussen CG, Raitakari OT, Thomson R, Juonala M, Patel DA, Viikari JS, Marniemi J, Srinivasan SR, Berenson GS, Dwyer T, Venn A. Utility of currently recommended pediatric dyslipidemia classifications in predicting dyslipidemia in adulthood: evidence from the Childhood Determinants of Adult Health (CDAH) study, Cardiovascular Risk in Young Finns Study, and Bogalusa Heart Study. Circulation. 2008;117:32–42. doi: 10.1161/CIRCULATIONAHA.107.718981. [DOI] [PubMed] [Google Scholar]
- 18.Raitakari OT, Juonala M, Rönnemaa T, Keltikangas-Järvinen L, Räsänen L, Pietikäinen M, Hutri-Kähönen N, Taittonen L, Jokinen E, Marniemi J, Jula A, Telama R, Kähönen M, Lehtimäki T, Åkerblom HK, Viikari JS. Cohort Profile: The Cardiovascular Risk in Young Finns Study. Int J Epidemiol. 2008;37:1220–6. doi: 10.1093/ije/dym225. [DOI] [PubMed] [Google Scholar]
- 19.Cleland VJ, Ball K, Magnussen C, Dwyer T, Venn A. Socioeconomic position and the tracking of physical activity and cardiorespiratory fitness from childhood to adulthood. Am J Epidemiol. 2009;170:1069–77. doi: 10.1093/aje/kwp271. [DOI] [PubMed] [Google Scholar]
- 20.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JS, Dwyer T, Raitakari OT. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–85. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 21.Lauer RM, Clarke WR, Beaglehole R. Level, trend, and variability of blood pressure during childhood: the Muscatine study. Circulation. 1984;69:242–9. doi: 10.1161/01.cir.69.2.242. [DOI] [PubMed] [Google Scholar]
- 22.Magnussen CG, Fryer J, Venn A, Laakkonen M, Raitakari OT. Evaluating the use of a portable ultrasound machine to quantify intima-media thickness and flow-mediated dilation: agreement between measurements from two ultrasound machines. Ultrasound Med Biol. 2006;32:1323–9. doi: 10.1016/j.ultrasmedbio.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 23.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76. [PubMed] [Google Scholar]
- 24.Chobanian AV, Bakris GL, Black HR, Cushman WC, Grren LA, Izzo JLjr. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 25.Magnussen CG, Venn A, Thomson R, Juonala M, Srinivasan SR, Viikari JS, Berenson GS, Dwyer T, Raitakari OT. The Association of Pediatric LDL-cholesterol and HDL-cholesterol Dyslipidemia Classifications and Change in Dyslipidemia Status with Carotid Intima-Media Thickness in Adulthood: Evidence from the Cardiovascular Risk in Young Finns Study, the Bogalusa Heart Study, and the Childhood Determinants of Adult Health (CDAH) Study. J Am Coll Cardiol. 2009;53:860–9. doi: 10.1016/j.jacc.2008.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juonala M, Magnussen CG, Venn A, Dwyer T, Burns TL, Davis PH, Chen W, Srinivasan SR, Daniels SR, Kähönen M, Laitinen T, Taittonen L, Berenson GS, Viikari JSA, Raitakari OT. The influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood. The Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Bogalusa Heart Study and the Muscatine Study for the International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation. 2010;122:2514–20. doi: 10.1161/CIRCULATIONAHA.110.966465. [DOI] [PubMed] [Google Scholar]
- 27.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 28.Pettigrew HM, Gart JJ, Thomas DG. The bias and higher cumulants of the logarithm of a binomial variate. Biometrika. 1986;73:425–35. [Google Scholar]
- 29.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–93. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gray L, Lee IM, Sesso HD, Batty GD. Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard Alumni Health Study) J Am Coll Cardiol. 2011;58:2396–403. doi: 10.1016/j.jacc.2011.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sundström J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643. doi: 10.1136/bmj.d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B, Derazne E, Tzur D, Shamis A, Vinker S, Rudich A. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med. 2011;364:1315–25. doi: 10.1056/NEJMoa1006992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Juhola J, Oikonen M, Magnussen CG, Mikkilä V, Siitonen N, Jokinen E, Laitinen T, Würtz P, Gidding SS, Taittonen L, Seppälä I, Jula A, Kahonen M, Hutri-Kähönen N, Lehtimäki T, Viikari JS, Juonala M, Raitakari OT. Childhood physical, environmental, and genetic predictors of adult hypertension: the cardiovascular risk in young Finns study. Circulation. 2012;126:402–9. doi: 10.1161/CIRCULATIONAHA.111.085977. [DOI] [PubMed] [Google Scholar]
- 35.Lloyd-Jones DM. Improving the cardiovascular health of the US population. JAMA. 2012;307:1314–6. doi: 10.1001/jama.2012.361. [DOI] [PubMed] [Google Scholar]
- 36.Polak JF, Person SD, Wei GS, Godreau A, Jacobs DR, Jr., Harrington A, Sidney S, O’Leary DH. Segment-specific associations of carotid intima-media thickness with cardiovascular risk factors: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Stroke. 2010;41:9–15. doi: 10.1161/STROKEAHA.109.566596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zureik M, Ducimetiere P, Touboul PJ, Courbon D, Bonithon-Kopp C, Berr C, Magne C. Common carotid intima-media thickness predicts occurrence of carotid atherosclerotic plaques: longitudinal results from the Aging Vascular Study (EVA) study. Arterioscler Thromb Vasc Biol. 2000;20:1622–9. doi: 10.1161/01.atv.20.6.1622. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.