Abstract
Background
Infantile hemangiomas (IH) are common benign vascular tumors in children. Recognition and timely referral of high risk IH to specialized centers is important. This might be achieved by involving parents in the care for IH by means of an eHealth intervention.
Objective
The objective of our study was to evaluate parent compliance, acceptance, and usability of an open access, Web-based eHealth intervention (including e-learning and e-consult) designed to increase parents’ knowledge and (risk) evaluation of IH.
Methods
A cross-sectional study of parents who completed the eHealth intervention between October 2010 and November 2012 was carried out. All parents were sent a study questionnaire. Questions to evaluate compliance (to the advice given by a dermatologist during e-consultation) were asked. Acceptance and usability were evaluated by using the modified Technology Acceptance Model.
Results
A total of 224 parents completed the eHealth intervention and received the questionnaire, 135/224 parents responded (response rate was 60.3%). There were 128/135 questionnaires that were completed and included. A total of 110/128 (85.9%) parents were compliant to the advice of the dermatologist. There were 116.8/128 (91.3%) that perceived the eHealth intervention as useful and almost all parents (98.4%, 126/128) found the information in the e-learning clear. There were 29/128 (22.7%) that experienced technical problems. The majority of the parents (94.5%, 121/128) found the eHealth intervention reliable and most of them (98.4%, 126/128) would recommend the eHealth intervention to other parents. Noncompliant parents judged the eHealth intervention significantly less reliable compared to compliant parents (71%, 10/14 versus 97.3%, 107/110; P=.003).
Conclusions
Parents of children with an IH showed a high compliance (85.9%, 110/128) to the advice of the dermatologist given via our Web-based eHealth intervention. This high compliance might be positively influenced by the good acceptance and usability of the eHealth intervention and might result in timely presentation and treatment of children with high risk IH in specialized centers.
Keywords: eHealth, e-learning, Internet, compliance, acceptance, usability, dermatology, optimizing care, infantile hemangioma, child
Introduction
Infantile Hemangiomas
Infantile hemangiomas (IH) are common benign vascular tumors with a unique growth pattern [1-3]. Although most IH have an uncomplicated course, 24% of the patients experience complications, such as ulceration, bleeding, functional impairment, life-threatening risk, or cosmetic risk of which 38% need treatment [4]. Also, a segmental IH can be associated with congenital malformations and requires diagnostic evaluation [4]. Currently, complicated IH can be treated with beta blockers, like propranolol [5,6]. Correct initial diagnosis and timely referral of patients at risk of complications is important since early intervention may prevent complications [4,7].
Parents and E-Learning
In order to ensure timely referral of high-risk IH, it is imperative for parents and health care professionals to have knowledge about IH and risk factors for developing complications. e-learning is widely used to increase knowledge, including the field of dermatology [8-14]. Parents use the Internet as an information source for the disease of their child, and the use of an educational e-learning module to increase patients’ knowledge has also been reported [15-18].
To increase parents’ knowledge about IH and its complications, we have developed an open access Web-based eHealth intervention [19,20]. This eHealth intervention consisted of an e-learning module and an e-consult (including a teledermatology consultation). Advice on diagnosis, risk of complications, and need to be seen by a medical specialist was given. If parents follow this advice (compliance to the advice) it might contribute to timely referral of high-risk patients to a medical specialist.
Parent Compliance
Patient/parent-compliance (“the extent to which the parent’s behavior coincides with the advice of the dermatologist”) is essential for the success of this eHealth intervention. Compliance to medication has been extensively described in the literature. However, little is known about compliance to advice given via eHealth.
The goal of this study was to evaluate the compliance of the parents to the advice given by the dermatologist via the e-consult. Second, the acceptance and usability of this eHealth intervention were determined.
Methods
Design and Participants
A cross-sectional study was carried out after participation in the open access Web-based eHealth intervention [19], consisting of an e-learning module and e-consult (Figure 1 shows illustrative screenshots).
Figure 1.
Illustrative screenshots of the e-learning module (in Dutch). The top image shows general information about infantile hemangiomas. The bottom image shows a case scenario of an infantile hemangioma on the scalp (Case 2).
The Dutch patient support group for Hemangiomas and Vascular Anomalies (HEVAS) and the University Medical Center Utrecht (UMCU) supported the eHealth intervention, and their logos were displayed on the home page. Parents were referred to the eHealth intervention by a link on the home page of HEVAS [21], by their child’s youth or primary health care provider, or by surfing the Internet. Participation was voluntary and free of charge.
After registration on the website, parents received a password to start the e-learning module and e-consult. By using a password, safe uploading of personal information on the website was guaranteed. During the e-learning module parents were informed about IH and its complications and two illustrative cases were presented. During the e-consult parents were asked to provide one photograph of the skin lesion of their child and to give information regarding its growth pattern. A dermatologist of the Center for Congenital Vascular Anomalies Utrecht (CAVU) judged this photograph. In case the dermatologist was unable to make a proper diagnosis, due to lack of quality of the photograph, parents were asked for a new photograph or referred to their general practitioner (GP). Advice on diagnosis, risk of complications, and need to be seen by a medical specialist was given within 5 working days by email [20]. Parents were advised whether or not to go to a medical specialist and whether there was urgency. All parents of a child with a suspected IH, who fully went through the e-learning and e-consult between October 2010 and November 2012, were eligible for study participation and received a study questionnaire by email. The time between participation in the eHealth intervention and completing the questionnaire was variable. Demographic information of the parents was obtained. The ethics committee of the University Medical Center Utrecht approved the study.
Theoretical Framework and Study Questionnaire
Compliance, Acceptance, and Usability
A questionnaire was developed to evaluate the variables–compliance, acceptance, and usability of the eHealth intervention.
Compliance
Compliance was defined as the extent to which the parent’s behavior coincides with the advice of the dermatologist. By means of the e-consult, parents were given an advice about the diagnosis of the skin lesion of their child (IH/no IH/uncertain) and about the need to visit a medical specialist (no need/need/urgent need). In case of “need to visit a specialist,” parents were first referred to their GP because in the Netherlands a referral of the GP is required for visiting a medical specialist. In case of “no need to visit a specialist,” parents were only advised to go to their GP if the IH was growing rapidly or became ulcerated. In all cases of “no IH” or “uncertain diagnosis” (in which the dermatologist was unable to diagnose the skin abnormality using the provided information by the parents), parents were advised to go to their GP. In order to determine the compliance, questions regarding visits to GP/medical specialists, additional diagnostics, and initiated treatment were asked. The time between the advice and the actual appointment with a specialist was also evaluated by asking the parents.
Acceptance and Usability
The acceptance and usability of the eHealth intervention were evaluated by using a modified Technology Acceptance Model (TAM). The TAM is the most widely applied model to describe consumer acceptability [22,23]. Technology acceptance is defined as “an individual’s psychological state with regard to his or her voluntary or intended use of a particular technology” [24]. The TAM theorizes that an individual’s behavioral intention to use a technology is determined by two beliefs: (1) perceived usefulness (PU) and (2) perceived ease of use (PEU) [25]. It has proved to be suitable for different genders, age groups, cultures, levels of information technology competency, and in both obligatory and voluntary usage settings [26]. Health care professionals have tested the TAM for the prediction of adoption of telemedicine, and its reliability, robustness, and validity have been demonstrated [26-28]. To determine the acceptance and usability of our eHealth intervention, we have modified the TAM based on the Chau and Hu’s model of telemedicine acceptance [29]. We have added the dimension “attitude towards use” to the original TAM, because behavioral intention is also determined by attitude, which is influenced by PU and PEU [29,30]. Attitude can be defined as “the perception by an individual of the positive or negative consequences related to adopting the technology.” Questions to evaluate acceptance and usability were developed following the modified TAM.
Study Questionnaire
The study questionnaire consisted of 24 questions, grouped into three variables (demographic information, compliance, acceptance and usability) (Table 1). Acceptance and usability was subdivided using the three dimensions of the TAM (PU, PEU, and attitude). There were 12 questions that were rated on a three-point scale (agree, no agreement/no disagreement, disagree). There were 7 questions that could be answered with “yes” or “no,” and with the final question parents were asked to rate the eHealth intervention (including e-learning and e-consult) on a 0-10 scale (0=very bad, 10=excellent). At the end of the questionnaire there was an open field for comments and suggestions.
Table 1.
Questions used to evaluate compliance, acceptance, and usability.
| Variable | Dimension | Related questions | Example |
| Demographic information |
|
1-4 | Gender, age, relation to the patient, and education level |
| Compliance to advice |
|
5-15 | Did you visit your general practitioner after our advice? |
| Acceptance and usability | Perceived usefulness | 16a-16e, 19a-19d | The e-learning module is useful to determine if my child is at risk for complications |
|
|
Perceived ease of use | 17, 20, 21a-21d, 23 | The information of the e-learning is understandable |
|
|
Attitude | 8, 18, 22, 24 | I would recommend the e-learning module to other people |
Analyses
Only fully completed questionnaires were used for evaluation. Descriptive analyses were used to evaluate the compliance, acceptance, and usability.
Fisher’s exact tests were used to evaluate the difference in acceptance, usability, and attitude between compliant parents and noncompliant parents.
Results
The Parent Questionnaire
A total of 224 parents completed the eHealth intervention and received the questionnaire, 135/224 parents responded (response rate, 60.3%). There were 128/135 questionnaires completed and included in this study. Reasons for not responding on the questionnaire are unknown. Parent characteristics are shown in Table 2.
Table 2.
Characteristics of the parents (N=128).
| Characteristic | Frequency, n (%) | |
| Gender | ||
|
|
Men | 10 (7.8) |
|
|
Women | 118 (92.2) |
| Age | ||
|
|
< 20 years | 0 (0) |
|
|
20-29 years | 20 (15.6) |
|
|
30-39 years | 85 (66.4) |
|
|
> 40 years | 21 (16.4) |
|
|
Unknown | 2 (1.6) |
| Relation to the child | ||
|
|
Parent | 127 (99.2) |
|
|
Caretaker (grandparent) | 1 (0.8) |
| Highest educational level | ||
|
|
Low | 6 (4.7) |
|
|
Moderate | 32 (25.0) |
|
|
High | 88 (68.8) |
|
|
Unknown | 2 (1.6) |
| Previously received information a | ||
|
|
None | 4 (3.1) |
|
|
Internet | 66 (51.6) |
|
|
Primary health care provider | 58 (45.3) |
|
|
Specialist | 6 (4.7) |
|
|
Unknown | 32 (25.0) |
aSome parents previously received information from multiple sources.
Parent Compliance With Medical Advice
There were 119/128 (93.0%) skin lesions that were diagnosed as an IH of which 58/119 (48.7%) parents were advised not to visit the medical specialist, and 61/119 (51.3%) parents were advised to visit a medical specialist. In 9/119 cases (7.6%) the skin lesion was not an IH or the diagnosis was uncertain. A total of 110/128 (85.9%) parents followed the advice of the dermatologist. Figure 2 shows all patients who were advised not to visit a medical specialist. Figure 3 shows all patients, who were advised to visit a medical specialist. Figure 4 shows all patients with no IH or where it was not possible to make an accurate diagnosis.
Figure 2.
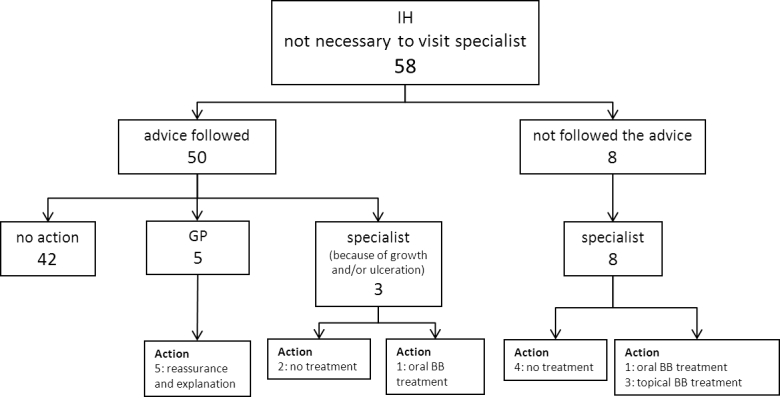
Flowchart of the compliance of the parents who were advised not to visit a medical specialist by the dermatologist via e-consultation. The flowchart shows which doctor the parents visited and to what actions (eg, diagnostic evaluation and/or treatment) it has led. The figures indicate the number of patients. Infantile hemangioma(s) (IH); general practitioner (GP); and beta blocker (BB).
Figure 3.
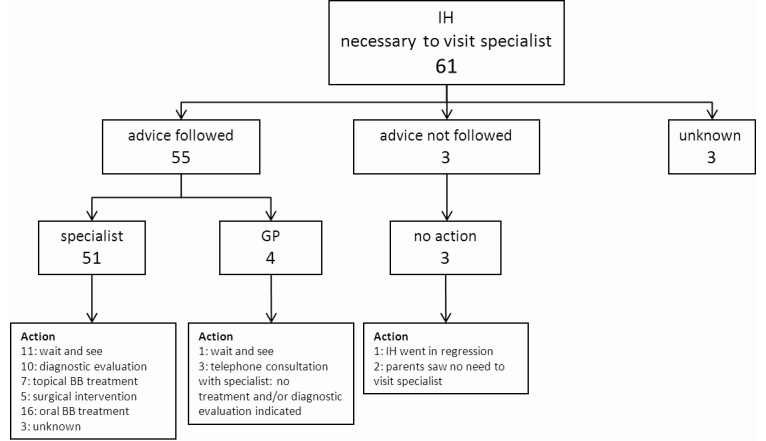
Flowchart of the compliance of the parents who were advised to visit a medical specialist by the dermatologist via e-consultation. The flowchart shows which doctor the parents visited and to what actions (eg, diagnostic evaluation and/or treatment) it has led. The figures indicate the number of patients. One patient, who followed the advice of the dermatologist and went to a specialist, underwent both diagnostic evaluation and topical beta blocker treatment was initiated. Infantile hemangioma(s) (IH); general practitioner (GP); and beta blocker (BB).
Figure 4.
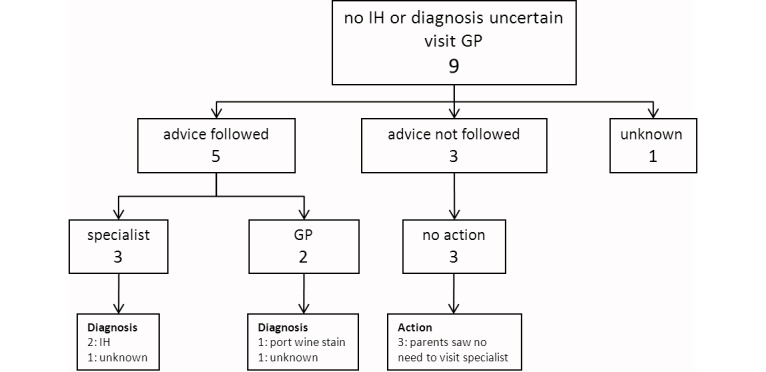
Flowchart of the compliance of the parents of a child with no Infantile hemangioma (IH) or where it was not possible to make an accurate diagnosis by the dermatologist via e-consultation. The flowchart shows which doctor the parents visited and to what actions (eg, diagnostic evaluation and/or treatment) it has led. The figures indicate the number of patients. General practitioner (GP).
There were 8/58 parents who were advised not to visit a specialist that did visit a medical specialist (for unknown reasons) (Figure 2). In four patients beta blocker treatment was initiated–one patient with a small, superficial, localized/nodular IH in the face was treated with oral propranolol; one patient with a superficial, localized/nodular IH on the lower arm was treated with topical timolol; and two patients with a small, superficial, localized/nodular IH in the face/neck area were treated with topical timolol. There were 3/61 parents who were advised to visit a specialist and did not–one small, superficial, localized/nodular IH close to the eye spontaneously went into regression; and two parents saw no need to visit a specialist (one patient with a big superficial IH on the arm, because of no functional impairment, and one patient with a small superficial IH on the tip of the nose whose parents did not want treatment). In three cases of “no IH/uncertain diagnosis” the advice of the dermatologist was not followed because the parents saw no need to visit a specialist (Figure 4).
The time between the advice and the actual appointment with a medical specialist, sorted by referral indication, are shown in Table 3. These data were available for 33/71 cases.
Table 3.
Compliance, time between the advice and the actual appointment with a specialist, and average age of the patient, sorted by referral indication.
| Referral indication | na | Compliance, n (%) | Average time to appointment in weeks, (SDb) | Average age of the child weeks, (SD) |
| (Imminent) functional impairment | 19 | 18 (94.7) | 2.6 (2.5) | 12.6 (9.1) |
| Ulceration | 19 | 18 (94.7) | 3.4 (2.6) | 13.5 (9.4) |
| Cosmetic impairment | 18 | 17 (94.4) | 3.9 (5.0) | 55.5 (143.4c) |
| Diagnostic | 15 | 14 (93.3) | 2.8 (3.1) | 9.3 (5.3) |
an=number of patients
bBased on available data in 33/71 cases.
cOne patient with cosmetic impairment was 12 years. Excluding this patient the average age was 22.1 SD 21.8 weeks.
Acceptance and Usability
On all questions concerning PU an average of 91.3% (116.8/128) (range 86.7%, 111/128-98.5%, 126/128) of the parents agreed. This means that the PU was high.
Almost all parents (98.4%, 126/128) found the information of the e-learning understandable and clear, and 92.2% (118/128) of them found the eHealth intervention easy to use. There were 3/128 parents (2.3%) that experienced technical problems with logging in, 3/128 (2.3%) with filling in the questionnaire, and 29/128 parents (22.6%) experienced technical problems with uploading the photograph of their child.
The majority of the parents (94.8%, 121/128) found the eHealth intervention reliable and most of them (98.4%, 126/128) would recommend the eHealth intervention to other parents. There were 97.7% (125/128) of them that think the time investment was worth the effort (average time of completing the e-learning module, excluding e-consult, was 12.54 minutes). The average rate parents gave the eHealth intervention on a 0-10 scale was 8.4 (SD 1.1).
Comments and suggestions were evaluated. Positive comments were given about the reassurance parents experienced, the added value of the e-learning module for primary health care providers, and timely and adequate care due to the eHealth intervention. Negative comments were given about “shocking” photographs used in the e-learning module and difficulties in uploading photographs from an iPad.
An evaluation of difference in acceptance, usability, and attitude between compliant parents and noncompliant parents showed that noncompliant parents judged the eHealth intervention significantly less reliable compared to the compliant parents (71.4%, 10/14 versus 97.3%, 107/110), P=.003). There was no statistically significant difference between the percentage of highly educated parents in the compliant group (68.2%, 75/110) and the noncompliant group (85.7%, 12/14) (P=.23). All parents with a low education level (n=6) found the eHealth intervention easy to use.
Discussion
Parent Compliance With Advice
This study shows that parents are highly compliant (85.9%, 110/128) to the advice of the dermatologist given via the described eHealth intervention for IH. Overall parents very positively judged the PU and PEU and they had a positive attitude towards the eHealth intervention.
The compliance rate is high compared to patient compliance with telephone triage recommendations in emergency care (62%), compliance to advice given via Web-based triage in primary care (57%), and family compliance to travel advice (≥80%) [31-33]. The high compliance of the eHealth intervention might have been positively influenced by its perceived reliability. Our eHealth intervention addresses the need of parents to get complementary information regarding diagnosis and treatment, to get a second opinion, to complement the information already provided by their doctor, or to confirm what they are already thinking [8,34]. It was developed in cooperation with the HEVAS and parents could find it by means of a link on their home page [21]. On the home page of the open access eHealth intervention the logos of HEVAS and UMCU were shown, as well as the names of the specialists of the CAVU team. All this might have contributed to the reliability of our eHealth intervention and might have increased the compliance of the parents. This is confirmed by the fact that noncompliant parents judged the eHealth intervention significantly less reliable.
Little is known about (non) compliance to advice given via eHealth. Compliance is a multifaceted process that is influenced by multiple factors (eg, social and economic circumstances, particularly health literacy, patient belief systems and patient education) [35,36]. Noncompliance to the advice may reflect ignorance or misunderstanding of the clinical situation and might result from the parents’ inability to cope emotionally with the stresses surrounding the advice [37]. The advice, given by e-consultation, might have been in conflict with previously obtained advice by the parents from, for example, other health care takers, family, friends, media sources and health-related websites. Parents who encountered conflicting information might have been less compliant to the advice [38]. Principles to improve compliance to medication have been described and mostly apply in the case of a face-to-face contact between doctor and patient/parent [35]. Therefore most of these principles do not apply to compliance to the advice given via our eHealth intervention. Further studies are necessary to evaluate the factors influencing (non) compliance to advice given via eHealth.
The advice given via the eHealth intervention was based on criteria used in the literature [4,39-41] and in line with a recently published consensus about the treatment of IH with propranolol [6]. However, treatment was initiated in four children who were advised not to visit a medical specialist (Figure 2) and in 15 children visiting a GP/medical specialist has not led to action (Figure 3). A possible explanation is that in some cases our advice was inadequate because of the lack of information given by the parents (eg, photograph of the IH did not reflect the real situation). Another explanation might be that not all GPs and medical specialists are familiar with the most recent recommendations for the management of IH.
Parental Education Levels and the Internet
In accordance with findings about parental Internet use for health-related information in the literature, the population of this study consisted of highly educated woman in the age group 30-35 [10,42,43]. This higher education is associated via higher eHealth literacy [9,44]. Possibly, low educated parents did not find the eHealth intervention on the Internet or dropped out of the e-learning module before finishing because they were not able to locate, evaluate, integrate, and apply the medical information (low eHealth literacy) [44], or had other needs and/or expectations. The small number of low educated parents in this study thought the eHealth intervention was easy to use and they were compliant to the advice. Our results show no significant difference in results between (the small number of) low educated and highly educated parents. Parents with a low socioeconomic status have access to the Internet and their Internet use is high [9,42,45]. The pressure to use the Internet to empower patients and exchange information is increasing and therefore the Internet might still provide an opportunity to reach low educated parents and may prompt them to consult their doctor [9,45]. Eventually this might contribute to timely presentation of high-risk IH, also for children of low educated parents.
Chang et al showed that the mean age of the first visit of IH patients to a specialist is 5 months [39]. The average age at the time of referral of IH leading to functional impairment (12.6 weeks) and the average time to appointment (2.6 weeks) suggest that this eHealth intervention might contribute to earlier presentation of patients with high-risk IH in specialized centers. More studies are necessary to confirm this.
eHealth Intervention Positively Judged by Parents
The parents positively judged the acceptance and usability of the eHealth intervention. A positive attitude leads to intentions to follow the advice [33], and this might have influenced the compliance to the advice in our study. Although 71.8% (92/128) of the parents (Table 2) previously received information via Internet and/or from their primary health care provider/medical specialist, this eHealth intervention seems to have added value. However, there is still progress to be made. Almost a quarter (22.7%, 29/128) of the parents experienced technical problems with uploading of the photograph. Mostly, because uploading via a tablet was not supported by our website. This problem was temporally solved by giving parents the opportunity to send the photograph via email and is now completely resolved. Furthermore, parents commented on the lack of knowledge among primary health care providers. Initially, we have developed the eHealth intervention for both parents and health care providers. Until now, mostly parents participated in the eHealth intervention. To stimulate usage among health care providers, the link to our eHealth intervention has been since 2013 included in the IH guideline for youth health care providers in the Netherlands. It might be interesting to investigate whether this will improve the usage by health care providers.
Conclusions
Parents of children with an IH show a high compliance (85.9, 110/128) to the advice (about risk of complications and need to be seen by a medical specialist) given by the dermatologist via the described Web-based eHealth intervention. This high compliance might be positively influenced by the good acceptance and usability of the eHealth intervention. Our results implicate that increasing parents’ knowledge and involving them in the care for IH might result in timely presentation and treatment of children with high-risk IH in specialized centers.
Acknowledgments
We would like to thank the Dutch patient support group HEVAS for their support in developing the e-learning module and for showing the link of our eHealth intervention on their home page.
Abbreviations
- CAVU
Center for Congenital Vascular Anomalies Utrecht
- GP
general practitioner
- HEVAS
Dutch patient support group for Hemangiomas and Vascular Anomalies
- IH
infantile hemangiomas
- PEU
perceived ease of use
- PU
perceived usefulness
- TAM
Technology Acceptance Model
- UMCU
University Medical Center Utrecht
Footnotes
Conflicts of Interest: None declared.
References
- 1.Kilcline C, Frieden IJ. Infantile hemangiomas: How common are they? A systematic review of the medical literature. Pediatr Dermatol. 2008;25(2):168–173. doi: 10.1111/j.1525-1470.2008.00626.x. [DOI] [PubMed] [Google Scholar]
- 2.Hoornweg MJ, Smeulders MJ, Ubbink DT, van der Horst CM. The prevalence and risk factors of infantile haemangiomas: A case-control study in the Dutch population. Paediatr Perinat Epidemiol. 2012 Mar;26(2):156–162. doi: 10.1111/j.1365-3016.2011.01214.x. [DOI] [PubMed] [Google Scholar]
- 3.Finn MC, Glowacki J, Mulliken JB. Congenital vascular lesions: Clinical application of a new classification. J Pediatr Surg. 1983 Dec;18(6):894–900. doi: 10.1016/s0022-3468(83)80043-8. [DOI] [PubMed] [Google Scholar]
- 4.Haggstrom AN, Drolet BA, Baselga E, Chamlin SL, Garzon MC, Horii KA, Lucky AW, Mancini AJ, Metry DW, Newell B, Nopper AJ, Frieden IJ. Prospective study of infantile hemangiomas: Clinical characteristics predicting complications and treatment. Pediatrics. 2006 Sep;118(3):882–887. doi: 10.1542/peds.2006-0413. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=16950977. [DOI] [PubMed] [Google Scholar]
- 5.Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, Boralevi F, Thambo JB, Taïeb A. Propranolol for severe hemangiomas of infancy. N Engl J Med. 2008 Jun 12;358(24):2649–2651. doi: 10.1056/NEJMc0708819. [DOI] [PubMed] [Google Scholar]
- 6.Drolet BA, Frommelt PC, Chamlin SL, Haggstrom A, Bauman NM, Chiu YE, Chun RH, Garzon MC, Holland KE, Liberman L, MacLellan-Tobert S, Mancini AJ, Metry D, Puttgen KB, Seefeldt M, Sidbury R, Ward KM, Blei F, Baselga E, Cassidy L, Darrow DH, Joachim S, Kwon EK, Martin K, Perkins J, Siegel DH, Boucek RJ, Frieden IJ. Initiation and use of propranolol for infantile hemangioma: Report of a consensus conference. Pediatrics. 2013 Jan;131(1):128–140. doi: 10.1542/peds.2012-1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacFie CC, Jeffery SL. Diagnosis of vascular skin lesions in children: An audit and review. Pediatr Dermatol. 2008;25(1):7–12. doi: 10.1111/j.1525-1470.2007.00573.x. [DOI] [PubMed] [Google Scholar]
- 8.Wutoh R, Boren SA, Balas EA. eLearning: A review of Internet-based continuing medical education. J Contin Educ Health Prof. 2004;24(1):20–30. doi: 10.1002/chp.1340240105. [DOI] [PubMed] [Google Scholar]
- 9.Cobb SC. Internet continuing education for health care professionals: An integrative review. J Contin Educ Health Prof. 2004;24(3):171–180. doi: 10.1002/chp.1340240308. [DOI] [PubMed] [Google Scholar]
- 10.Choules AP. The use of elearning in medical education: A review of the current situation. Postgrad Med J. 2007 Apr;83(978):212–216. doi: 10.1136/pgmj.2006.054189. http://europepmc.org/abstract/MED/17403945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kulier R, Gülmezoglu AM, Zamora J, Plana MN, Carroli G, Cecatti JG, Germar MJ, Pisake L, Mittal S, Pattinson R, Wolomby-Molondo JJ, Bergh AM, May W, Souza JP, Koppenhoefer S, Khan KS. Effectiveness of a clinically integrated e-learning course in evidence-based medicine for reproductive health training: A randomized trial. JAMA. 2012 Dec 5;308(21):2218–2225. doi: 10.1001/jama.2012.33640. [DOI] [PubMed] [Google Scholar]
- 12.Farrimond H, Dornan TL, Cockcroft A, Rhodes LE. Development and evaluation of an e-learning package for teaching skin examination. Action research. Br J Dermatol. 2006 Sep;155(3):592–599. doi: 10.1111/j.1365-2133.2006.07360.x. [DOI] [PubMed] [Google Scholar]
- 13.Jenkins S, Goel R, Morrell DS. Computer-assisted instruction versus traditional lecture for medical student teaching of dermatology morphology: A randomized control trial. J Am Acad Dermatol. 2008 Aug;59(2):255–259. doi: 10.1016/j.jaad.2008.04.026. [DOI] [PubMed] [Google Scholar]
- 14.Hanson AH, Krause LK, Simmons RN, Ellis JI, Gamble RG, Jensen JD, Noble MN, Orser ML, Suarez AL, Dellavalle RP. Dermatology education and the Internet: Traditional and cutting-edge resources. J Am Acad Dermatol. 2011 Oct;65(4):836–842. doi: 10.1016/j.jaad.2010.05.049. [DOI] [PubMed] [Google Scholar]
- 15.Bernhardt JM, Felter EM. Online pediatric information seeking among mothers of young children: Results from a qualitative study using focus groups. J Med Internet Res. 2004 Mar 1;6(1):e7. doi: 10.2196/jmir.6.1.e7. http://www.jmir.org/2004/1/e7/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knapp C, Madden V, Marcu M, Wang H, Curtis C, Sloyer P, Shenkman E. Information seeking behaviors of parents whose children have life-threatening illnesses. Pediatr Blood Cancer. 2011 May;56(5):805–811. doi: 10.1002/pbc.22674. [DOI] [PubMed] [Google Scholar]
- 17.Fox S, Jones S. Pew Internet. Washington, DC: Pew Internet and American Life Project; [2013-11-15]. The social life of health information http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information.aspx. [Google Scholar]
- 18.Mulders G, de Wee EM, Vahedi Nikbakht-Van de Sande MC, Kruip MJ, Elfrink EJ, Leebeek FW. E-learning improves knowledge and practical skills in haemophilia patients on home treatment: A randomized controlled trial. Haemophilia. 2012 Sep;18(5):693–698. doi: 10.1111/j.1365-2516.2012.02786.x. [DOI] [PubMed] [Google Scholar]
- 19.de Graaf M; Breugem CC; Pasmans SGMA Aardbeivlek.nl. [2013-11-16]. Is de afwijking van uw kind een Hemangioom? http://www.aardbeivlek.nl.
- 20.de Graaf M, Knol MJ, Totté JEE, van Os-Medendorp H, Breugem CC, Pasmans SGMA. E-learning enables parents to assess an infantile hemangioma. J Am Acad Dermatol. 2013 XX; doi: 10.1016/j.jaad.2013.10.040. (in press)(forthcoming)(forthcoming) [DOI] [PubMed] [Google Scholar]
- 21.HEVAS. 2005. Jun, [2013-08-21]. Patientenvereniging voor hemangiomen en vasculaire malformaties http://hevas.eu/
- 22.Davis FD. MIS Quarterly. 1989. [2013-11-17]. Perceived usefulness, perceived ease of use, and user acceptance of information technology http://iris.nyit.edu/~kkhoo/Spring2008/Topics/TAM/PercieveUsefulness_MIS.pdf.
- 23.Kim J, Park HA. Development of a health information technology acceptance model using consumers' health behavior intention. J Med Internet Res. 2012;14(5):e133. doi: 10.2196/jmir.2143. http://www.jmir.org/2012/5/e133/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gattiker UE. Managing computer-based office information technology: A process model for management. In: Hendrick HW, Brown OG, editors. Human factors in organizational design. The Netherlands: Elsevier Science; 1984. pp. 395–403. [Google Scholar]
- 25.Venkatesh V, Davis FD. Management Science. 2000. Feb, [2013-11-17]. A theoretical extension of the technology acceptance model: Four longitudinal field studies http://web.ebscohost.com/ehost/detail?sid=2720c481-0ae3-41c9-8cfb-34abb4cfd2f6%40sessionmgr111&vid=1&hid=121&bdata=JnNpdGU9ZWhvc3QtbGl2ZQ%3d%3d#db=bth&AN=2958359.
- 26.Yarbrough AK, Smith TB. Technology acceptance among physicians: A new take on TAM. Med Care Res Rev. 2007 Dec;64(6):650–672. doi: 10.1177/1077558707305942. [DOI] [PubMed] [Google Scholar]
- 27.Hu PJ, Chau PYK, Liu ORS, Yan TK. Journal of Management Information Systems. 1999. [2013-11-17]. Examining the technology acceptance model using physician acceptance of telemedicine technology http://www.academia.edu/3000650/Examining_the_technology_acceptance_model_using_physician_acceptance_of_telemedicine_technology.
- 28.Burton-Jones A, Hubona GS. Information and Management. 2006. Sep, [2013-11-18]. The mediation of external variables in the technology acceptance model http://pls-institute.org/uploads/Burton-Jones-Hubona-IandM-2006.pdf.
- 29.Chau PYK, Hu PJ. Journal of Management Information Systems. 2002. Dec, Examining a model of information technology acceptance by individual professionals: An exploratory study http://www.jstor.org/discover/10.2307/40398548?uid=3739920&uid=2129&uid=2&uid=70&uid=4&uid=3739256&sid=21103028863853.
- 30.Chau PY, Hu PJ. Investigating healthcare professionals’ decisions to accept telemedicine technology: An empirical test of competing theories. Information & Management. 2002 Jan;39(4):297–311. doi: 10.1016/S0378-7206(01)00098-2. [DOI] [Google Scholar]
- 31.Purc-Stephenson RJ, Thrasher C. Patient compliance with telephone triage recommendations: A meta-analytic review. Patient Educ Couns. 2012 May;87(2):135–142. doi: 10.1016/j.pec.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 32.Caillet-Gossot S, Laporte R, Noël G, Gautret P, Soula G, Delmont J, Faucher B, Parola P, Osei L, Minodier P. Family compliance with counseling for children traveling to the tropics. J Travel Med. 2013;20(3):171–176. doi: 10.1111/jtm.12016. [DOI] [PubMed] [Google Scholar]
- 33.Nijland N, Cranen K, Boer H, van Gemert-Pijnen JE, Seydel ER. Patient use and compliance with medical advice delivered by a web-based triage system in primary care. J Telemed Telecare. 2010;16(1):8–11. doi: 10.1258/jtt.2009.001004. [DOI] [PubMed] [Google Scholar]
- 34.O'Connor H, Madge C. 'My mum's thirty years out of date'. Community, Work & Family. 2004 Dec;7(3):351–369. doi: 10.1080/1366880042000295754. [DOI] [Google Scholar]
- 35.Winnick S, Lucas DO, Hartman AL, Toll D. How do you improve compliance? Pediatrics. 2005 Jun;115(6):e718–724. doi: 10.1542/peds.2004-1133. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=15930200. [DOI] [PubMed] [Google Scholar]
- 36.DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: A meta-analysis. Med Care. 2007 Jun;45(6):521–528. doi: 10.1097/MLR.0b013e318032937e. [DOI] [PubMed] [Google Scholar]
- 37.Menahem S, Halasz G. Parental non-compliance--A paediatric dilemma. A medical and psychodynamic perspective. Child Care Health Dev. 2000 Jan;26(1):61–72. doi: 10.1046/j.1365-2214.2000.00115.x. [DOI] [PubMed] [Google Scholar]
- 38.Carpenter DM, DeVellis RF, Fisher EB, DeVellis BM, Hogan SL, Jordan JM. The effect of conflicting medication information and physician support on medication adherence for chronically ill patients. Patient Educ Couns. 2010 Nov;81(2):169–176. doi: 10.1016/j.pec.2009.11.006. http://europepmc.org/abstract/MED/20044230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chang LC, Haggstrom AN, Drolet BA, Baselga E, Chamlin SL, Garzon MC, Horii KA, Lucky AW, Mancini AJ, Metry DW, Nopper AJ, Frieden IJ, Hemangioma Investigator Group Growth characteristics of infantile hemangiomas: Implications for management. Pediatrics. 2008 Aug;122(2):360–367. doi: 10.1542/peds.2007-2767. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=18676554. [DOI] [PubMed] [Google Scholar]
- 40.Maguiness SM, Frieden IJ. Semin Cutan Med Surg. 2010. Jun, Current management of infantile hemangiomas http://www.pediatricnews.com/fileadmin/content_pdf/san/scms_pdf/vol_29_i2_Infantile_Hemangiomas.pdf. [DOI] [PubMed]
- 41.Maguiness SM, Frieden IJ. Management of difficult infantile haemangiomas. Arch Dis Child. 2012 Mar;97(3):266–271. doi: 10.1136/archdischild-2011-300851. [DOI] [PubMed] [Google Scholar]
- 42.Plantin L, Daneback K. Parenthood, information and support on the internet. A literature review of research on parents and professionals online. BMC Fam Pract. 2009;10:34. doi: 10.1186/1471-2296-10-34. http://www.biomedcentral.com/1471-2296/10/34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sarkadi A, Bremberg S. Socially unbiased parenting support on the Internet: A cross-sectional study of users of a large Swedish parenting website. Child Care Health Dev. 2005 Jan;31(1):43–52. doi: 10.1111/j.1365-2214.2005.00475.x. [DOI] [PubMed] [Google Scholar]
- 44.Neter E, Brainin E. eHealth literacy: Extending the digital divide to the realm of health information. J Med Internet Res. 2012;14(1):e19. doi: 10.2196/jmir.1619. http://www.jmir.org/2012/1/e19/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Knapp C, Madden V, Wang H, Sloyer P, Shenkman E. Internet use and eHealth literacy of low-income parents whose children have special health care needs. J Med Internet Res. 2011;13(3):e75. doi: 10.2196/jmir.1697. http://www.jmir.org/2011/3/e75/ [DOI] [PMC free article] [PubMed] [Google Scholar]


