Abstract
Acrokeratosis Paraneoplastica or Bazex syndrome is a dermatologic manifestation usually associated with the diagnosis of squamous cell carcinoma of the upper aerodigestive tract. We report a case with exuberant clinical manifestations, exemplifying the typical cutaneous lesions in this rare syndrome, in a patient with squamous cell carcinoma of the esophagus.
Keywords: Paraneoplastic syndromes, Skin, Skin abnormalities, Skin diseases
Abstract
Acroceratose paraneoplásica ou síndrome de Bazex é uma manifestação cutânea paraneoplásica rara, geralmente associada a carcinoma de células escamosas do trato aerodigestivo superior. Relata-se um caso com manifestações clínicas exuberantes, ilustrativo quanto às lesões cutâneas típicas da síndrome, em paciente portadora de carcinoma de células escamosas do esôfago.
INTRODUCTION
Paraneoplastic syndromes are defined as clinical, biochemical, hormonal, hematological, neurological or dermatological disorders, associated to a neoplasm, but not directly caused by the primary tumor invasion or by its metastases.1 They occur in 1 to 7% of all cancers.2
Cutaneous alterations may be indicators of malignancy, thus helping on the diagnosis of a primary tumor by means of physical exam or biopsy.2
Bazex syndrome is a paraneoplastic syndrome more frequently associated to squamous cell carcinomas of the higher aerodigestive tract, and described for the first time by Bazex et al. in 1965. It affects primarily Caucasian males over 40 years of age, and it is characterized by a psoriasiform eruption of typical distribution, palmoplantar keratosis and symmetric onychodystrophy. Nose and ears are affected in 63% and 79% of patients respectively.3 One hundred and forty-five cases were already described, of which only twelve were women.4
We report the case of a female patient, with esophageal squamous cell carcinoma, associated to a typical and exuberant cutaneous manifestation, characterizing Bazex syndrome.
CASE REPORT
Seventy-three year-old female, dark-skinned, farm worker sought medical attention due to pruritus and the presence of skin lesions in hands and feet for the last 40 days. She presented with edema and a well-delimited violet coloration extending through the distal half of the dorsal area of the hands to the tips of the digits. The fingers were swollen and the nails presented a yellow hyperchromia and onychomadesis (Figure 1). Edema and violet coloration repeated the same pattern on the feet, appearing more pronounced at the distal half, and extending over the dorsal area of the toes. Onychomadesis and hyperchromia were also present on the feet.
FIGURE 1.

Lesions on the dorsal area of the hands and onychomadesis
The patient was reluctant, responding only vaguely to the questions on the anamnesis. She declared herself a former smoker and a former drinker. Physical examination did not show any alterations besides voluntary guarding during the abdominal palpation. The main hypothesis proposed was of acrokeratosis paraneoplastica with differential diagnoses of tinea or psoriasis. Laboratory exams showed discreet normocytic and normochromic anemia, kidney and liver functions were normal and fungal tests on skin scrapings were positive for dermatophytes on the dorsal area of the feet. Subsequently we ordered abdominal and pelvic ultrasounds, chest x-rays, upper digestive endoscopy and colonoscopy, and a course of ketoconazole was prescribed for systemic use.
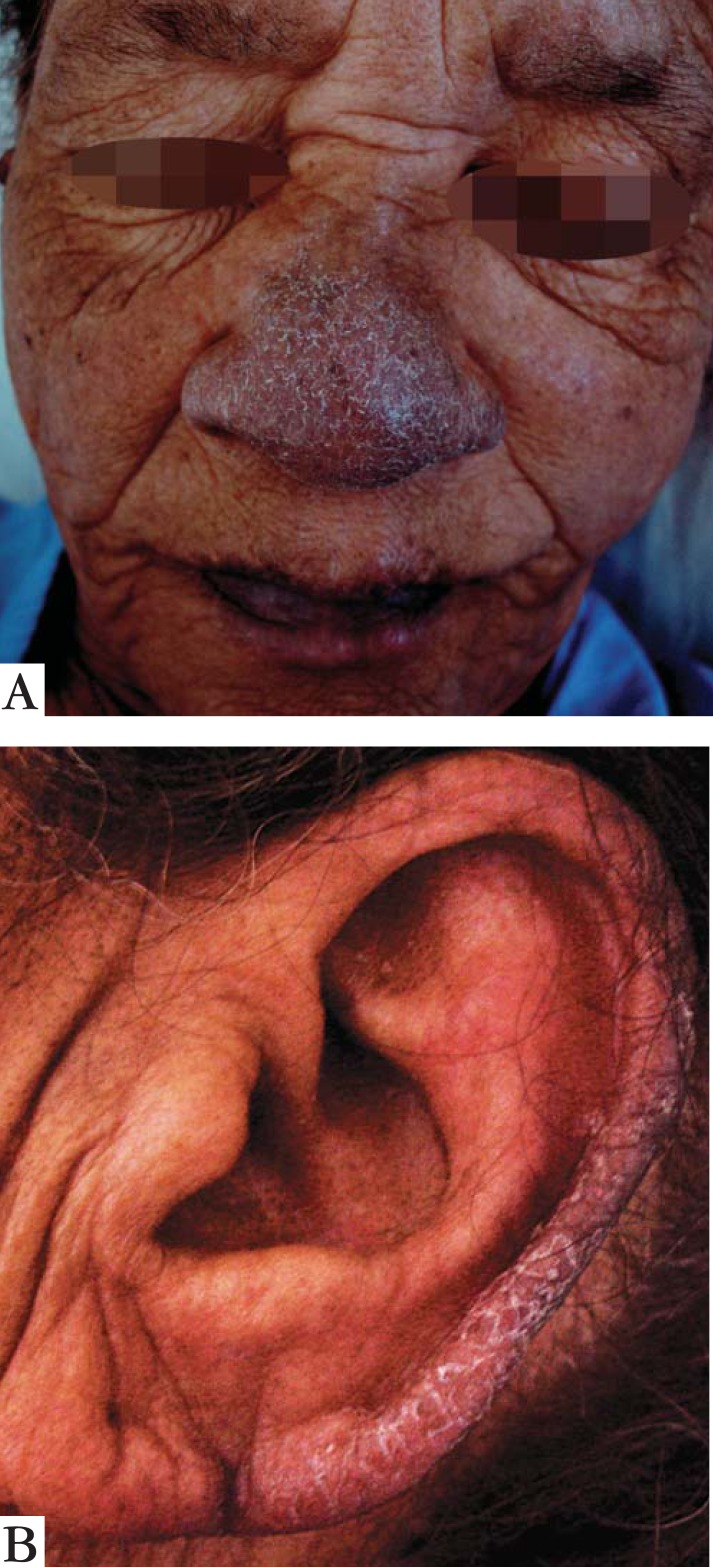
After thirty days, the patient returned, showing violet, slightly infiltrated, desquamative lesions, located on the nose, auricular pavilions, dorsal area of hands, feet and toes (Figure 2). Symmetric palmoplantar keratoderma, with lamellar desquamation was also present (Figure 3A). There was a worsening on hand and feet pruritus. Also noticeable were the rare blisters over the violet lesions on the dorsal areas of the hands and feet (Figure 3B). The patient's lips were also affected by the violet discoloration (Figure 2). Abdominal examination evidenced painful hepatomegaly; the liver border was located 10 cm from the right costal margin, with blunt and irregular edges. Abdominal ultrasound showed hepatic nodules and lymphadenomegaly. Pelvic ultrasound was normal. Anatomopathological examination of the skin on the dorsal area of the hand found discreet superficial psoriasiform chronic dermatitis, with pigmentary dispersion (Figure 4). Contrasted esophageal x-rays detected Zenker's diverticulum and distal esophageal stenosis. Upper digestive endoscopy demonstrated cancer of the esophagus and the biopsy confirmed a poorly differentiated esophageal squamous cell carcinoma. The patient died a few days after the diagnosis was completed.
FIGURE 2.
A: violet, infiltrative, desquamative erythematous plaque on the nose. B: similar lesion in the left auricular pavilion, also present on the right ear
FIGURE 3.
A: Plantar keratoderma. B: blister over the violet lesion on the medial side of the foot
FIGURE 4.
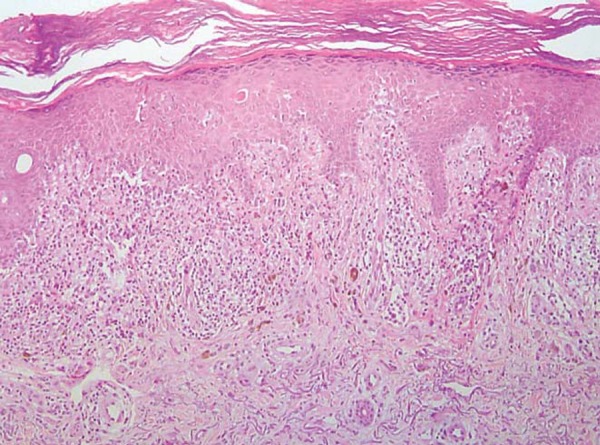
Anatomopathological exam of the skin on the dorsal area of the hand showing discreet, superficial, psoriasiform, chronic dermatitis, with pigmentary dispersion (enlarged 10x).
DISCUSSION
Bazex syndrome's physiopathology is still not well understood. Velez and Howard proposed, as a possible mechanism, the crossed reactions between tumor and skin antigens, the action of growth factors produced by the cancer cells and also zinc deficiency associated to the neoplasm.5 In 67% of cases reported on the medical literature, cutaneous manifestations precede in approximately one year, the diagnosis of cancer. Paraneoplastic acrokeratosis is highly specific for upper aerodigestive and lung neoplasms, however, rare reports point to the possibility of an association with bladder, prostate and breast cancer as well as liposarcoma.6,7,8 In 18% of patients, cutaneous lesions and cancer are diagnosed concomitantly and in 15% of the cases the diagnosis of cancer occurs first.7
All of the patients present with one or more of the following signs: desquamative erythematous lesions with a bluish or violet discoloration, onychodystrophy or keratoderma. Lesions are typically located on acral regions; they are symmetric and usually resistant to conventional treatments.8 The appearance of blisters in hands and feet is common in African-American patients.5 Pruritus is a rare manifestation.9
Bazex syndrome can progress in three stages: (1) cutaneous lesions in ears, fingers and nails; (2) palmoplantar keratosis; (3) involvement of knees, elbows and torso. The primary tumor tends to become symptomatic during the stage of palmoplantar keratosis6
Histological findings are unspecific, resulting in the description of one superficial psoriasiform dermatitis.1,3 Among the differential diagnoses are psoriasis, eczemas, pityriasis rubra pilaris, Reiter syndrome, tinea, acquired palmoplantar keratoderma, syphilis, porphyria cutanea tarda, and acquired epidermolysis bullosa.
The improvement of lesions is described in 91% of the cases after the primary tumor is treated. The cutaneous condition is refractory to topical treatment, which may be attempted with coal tar, salicylic acid, vitamin D analogues, corticoids and UVB radiation. Systemic treatment also presents inconsistent results in studies with etretinate, corticoids and antibiotics.7,10
Paraneoplastic syndromes may simulate other diseases, deferring the diagnosis of the primary tumor. The exuberance of the clinical manifestations described in this report illustrates the Bazex syndrome and draws the dermatologist attention to the possibility of this diagnosis. Our report is an exception to the rule, while describing a dark-skinned, female patient, with pruriginous lesions, an altogether unusual presentation of acrokeratosis paraneoplastica.
Footnotes
Work performed at Instituto Metropolitano de Ensino Superior (IMES) - Ipatinga (MG), Brazil.
Conflict of interest: None
Financial Support: None
REFERENCES
- 1.Ramos-E-Silva M, Carvalho JC, Carneiro SC. Cutaneous paraneoplasia. Clin Dermatol. 2011;29:541–547. doi: 10.1016/j.clindermatol.2010.09.022. [DOI] [PubMed] [Google Scholar]
- 2.Toro C, Rinaldo A, Silver CE, Politi M, Ferlito A. Paraneoplastic syndromes in patients with oral cancer. Oral Oncol. 2010;46:14–18. doi: 10.1016/j.oraloncology.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Poligone B, Christensen SR, Lazova R, Heald PW. Bazex syndrome (acrokeratosis paraneoplastica) Lancet. 2007;369:530. doi: 10.1016/S0140-6736(07)60240-2. [DOI] [PubMed] [Google Scholar]
- 4.Fasanmade A, Farrell K, Perkins CS. Bazex syndrome (acrokeratosis paraneoplastica): persistence of cutaneous lesions after successful treatment of an associates oropharyngeal neoplasm. Br J Oral Maxillofac Surg. 2009;47:138–139. doi: 10.1016/j.bjoms.2008.07.190. [DOI] [PubMed] [Google Scholar]
- 5.Abreu Velez AM, Howard MS. Diagnosis and treatment of cutaneous paraneoplastic disorders. Dermatol Ther. 2010;23:662–675. doi: 10.1111/j.1529-8019.2010.01371.x. [DOI] [PubMed] [Google Scholar]
- 6.Louvel G, Vauléon E, Boucher E, Raoul JL. Acrokeratosis Paraneoplastica (Bazex' Syndrome) Associated With Metastatic Squamous Cell Esophageal Carcinoma. J Clin Oncol. 2008;26:5128. doi: 10.1200/JCO.2008.16.8641. [DOI] [PubMed] [Google Scholar]
- 7.Abrou AE, Hope J, Jackson-Richards D, Lim HW, Ozog DM. Acrodermatitis paraneoplastica responding to topical PUVA treatment. Photodermatol Photoimmunol Photomed. 2007;23:37–38. doi: 10.1111/j.1600-0781.2007.00269.x. [DOI] [PubMed] [Google Scholar]
- 8.Chapireau D, Adlam D, Cameron M, Thompson M. Paraneoplastic syndromes in patients with primary oral cancersa systematic review. Br J Oral Maxillofac Surg. 2010;48:338–344. doi: 10.1016/j.bjoms.2009.08.025. [DOI] [PubMed] [Google Scholar]
- 9.Reis VMS, Pires MC, Martins SR, Criado PR, Pegas JRP, Müller H. Bazex's paraneoplastica acrokeratosisa case report. An Bras Dermatol. 1997;72:551–553. [Google Scholar]
- 10.Ferlito A, Rinaldo A. Paraneoplastic syndromes in patients with cancer of the larynx and hypopharynnx. Ann Otol Rhinol Laryngol. 2007;116:502–513. doi: 10.1177/000348940711600705. [DOI] [PubMed] [Google Scholar]