Abstract
The clinical value of Serum alpha-fetoprotein (AFP) to detect early hepatocellular carcinoma (HCC) has been questioned due to its low sensitivity and specificity found in recent years. Other than AFP, several new serum biomarkers including the circulating AFP isoform AFP-L3, des-gamma-carboxy prothrombin (DCP) and Golgi protein-73 (GP73) have been identified as useful HCC markers. In this investigation, we review the current knowledge about these HCC-related biomarkers, and sum up the results of our meta-analysis on studies that have addressed the utility of these biomarkers in early detection and prognostic prediction of HCC. A systematic search in PubMed, Web of Science, and the Cochrane Library was performed for articles published in English from 1999 to 2012, focusing on serum biomarkers for HCC detection. Data on sensitivity and specificity of tests were extracted from 40 articles that met the inclusion criteria, and the summary receiver operating characteristic curve (sROC) was obtained. A meta-analysis was carried out in which the area under the curve (AUC) for each biomarker or biomarker combinations (AFP, DCP, GP73, AFP-L3, AFP + DCP, AFP + AFP-L3, and AFP + GP73) was used to compare the diagnostic accuracy of different biomarker tests. The AUC of AFP, DCP, GP73, AFP-L3, AFP + DCP, AFP + AFP-L3, and AFP + GP73 are 0.835, 0.797, 0.914, 0.710, 0.874, 0.748, and 0.932 respectively. A combination of AFP + GP73 is superior to AFP in detecting HCC and differentiating HCC patients from non-HCC patients, and may prove to be a useful marker in the diagnosis and screening of HCC. In addition, the AUC of GP73, AFP + DCP and AFP + GP73 are better than that of AFP. The clinical value of GP73, AFP + DCP, or AFP + GP73 as serological markers for HCC diagnosis needs to be addressed further in future studies.
Keywords: hepatocellular carcinoma, biomarkers, detection, diagnosis
1. Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death worldwide. The incidence and mortality rates of HCC are almost equal because most HCC patients are diagnosed at an advanced stage. Therefore, the prognosis of HCC patients is generally poor, with a five-year survival rate lower than 5%. Alpha-fetoprotein (AFP) is the most commonly used serological biomarker in clinical practice. AFP, along with hepatic ultrasonography, is employed in the detection of HCC in high-risk patients with cirrhosis [1]. However, the clinical diagnostic accuracy of AFP is unsatisfactory due to low sensitivity and specificity. Therefore, there is an urgent need for developing better HCC-specific biomarkers [2,3]. Recent studies have identified other potential biomarkers for early detection of HCC, including the circulating AFP isoform AFP-L3, des-gamma-carboxy prothrombin (DCP), and Golgi protein-73 (GP73), although these biomarkers have been used in the clinic [4–6], the practical value of these markers has yet to be fully evaluated. So, it is meaningful to assess the value of these markers individually or for combined application in the clinic.
2. Results and Discussion
2.1. Results
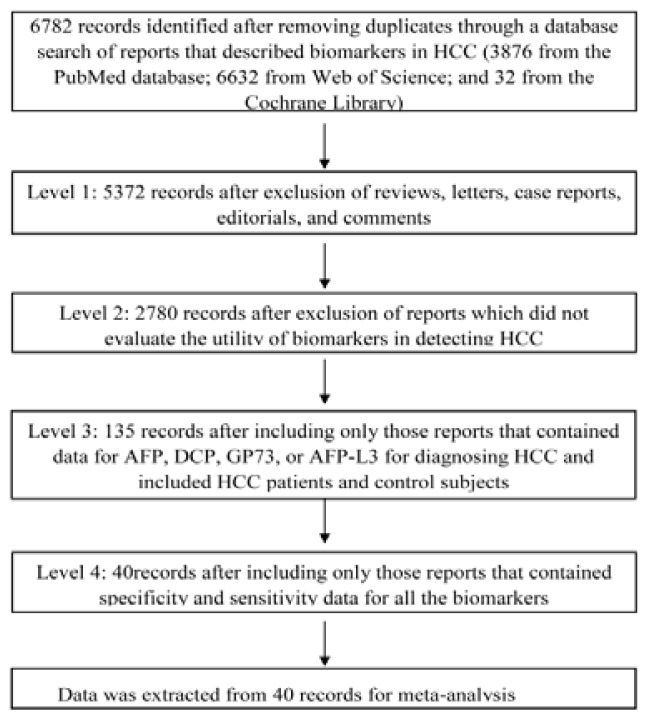
A total of 40 studies [7] were included in the meta-analysis, 35 for AFP (biomarker 1), 15 for DCP (biomarker 2), nine for GP73 (biomarker 3), 15 for AFP-L3 (biomarker 4), eight for AFP+DCP (biomarker 5), three for AFP+AFP-L3 (biomarker 6), and two for AFP+GP73 (biomarker 7). The literature search strategy is depicted below (Table 1). Literature screening was performed at four levels (Figure 1). We extracted data from the selected papers on authors, country, year of publication, journal, number of patients, test methods and results, sensitivity, specificity, and cut-off points for the biomarkers (Table 2).
Table 1.
Literature search strategy.
| Database | Search criteria | Filters/Limits |
|---|---|---|
| PubMed | Search ((hepatocellular carcinoma [MeSH Terms]) and biological markers [MeSH Terms]) and (“1999” [Date—Publication]: “2012” [Date—Publication]) | Humans; English |
| Web of Science | (hepatoma * or liver cell neoplasm * or hepatocellular neoplasm * or liver cell cancer * or hepatocellular cancer * or liver cell tumo * or hepatocellular tumo * or liver cell carcinom * or hepatocellular carcinom *) and (Biomarker * or Biological Marker * or Biologic Marker * or Biochemical Marker * or Serum Marker * or Clinical Marker *) | Publication date: 1999–present and language: English |
| Cochrane Library | #1 MeSH descriptor: [Carcinoma, Hepatocellular] explode all trees #2 MeSH descriptor: [Biological Markers] explode all trees |
Dates: from 1999–2012 |
A comprehensive literature search of original research articles published between January 1999 and July 2012 (cut-off date 1 July) assessing biomarkers for hepatocellular carcinoma (HCC) was conducted using the PubMed database, Web of Science, and Cochrane Library.
Figure 1.
Literature screening was performed at four levels. Level 1, reviews, letters, case reports, editorials, and comments were excluded from the papers identified using the above search strategy. Level 2, articles in which biomarkers were not evaluated for their utility in detecting hepatocellular carcinoma (HCC) were excluded. The full texts of reports that met the above criteria were obtained with duplicate articles excluded. Level 3, the content of the articles was analyzed to ensure that the serum biomarkers in the study included Alpha-fetoprotein (AFP), des-gamma-carboxy prothrombin (DCP), Golgi protein-73 (GP73), or circulating AFP isoform AFP-L3, and that these biomarkers were used just for diagnosing HCC. The data pertaining to other biomarkers were excluded from further analysis. Articles were further screened to ensure that the studies included data pertaining to patients with HCC and appropriate control populations. At Level 4, only reports with sensitivity and specificity data for the biomarkers were selected. A total of 40 reports met the inclusion criteria and were selected for meta-analysis.
Table 2.
Data from the selected papers.
| Study | Country/District | Publication Year | Number | Biomarker | Test Methods | Sensitivity | Specificity | Cutoff | Journal |
|---|---|---|---|---|---|---|---|---|---|
| Leerapun [8] | USA | 2007 | 52 | AFP-L3 | LiBASys | 0.710 | 0.630 | 10% | Clin. Gastroenterol. Hepatol. |
| 0.330 | 1.000 | 35% | |||||||
|
| |||||||||
| Cedrone [9] | Italy | 2000 | 74 | AFP | ELISA | 0.200 | 0.990 | 200 ug/L | Hepato Gastroenterol. |
| 0.550 | 0.880 | 20 ug/L | |||||||
|
| |||||||||
| Wang [10] | Taiwan, China | 2005 | 61 | AFP | ELISA | 0.590 | 0.770 | 20 ng/mL | World J. Gastroenterol. |
| DCP | EIA | 0.770 | 0.860 | 40 mAU/mL | |||||
| AFP + DCP | ELISA + EIA | 0.836 | 0.682 | 20 ng/mL/40 mAU/mL | |||||
|
| |||||||||
| Durazo [11] | USA | 2008 | 144 | AFP | IAUEC | 0.690 | 0.870 | 25 ng/mL | J. Gastroenterol. Hepatol. |
| DCP | ELISA | 0.870 | 0.850 | 84 mAU/mL | |||||
| AFP-L3 | LAEC | 0.560 | 0.900 | 10% | |||||
|
| |||||||||
| Gianluigi [12] | Italy | 2007 | 499 | AFP | ELISA | 0.410 | 0.940 | 18.8 ng/mL/20.5 IU/mL | Clin. Chim. Acta |
|
| |||||||||
| Giannelli [13] | Italy | 2005 | 120 | AFP | ELISA | 0.450 | 0.870 | 12.6 ng/mL/13.7 IU/mL | Int. J. Cancer |
|
| |||||||||
| Toyoda [14] | Japan | 2011 | 270 | AFP-L3 | μTAS | 0.394 | 0.770 | 7% | Cancer Sci. |
|
| |||||||||
| Okuda [15] | Japan | 1999 | 60 | DCP | EIA | 0.617 | 0.821 | 30 mAU/mL | Cancer |
| 0.600 | 0.863 | 35 mAU/mL | |||||||
| 0.600 | 0.923 | 40 mAU/mL | |||||||
| 0.583 | 0.949 | 45 mAU/mL | |||||||
| 0.567 | 0.966 | 50 mAU/mL | |||||||
| 0.567 | 0.966 | 55 mAU/mL | |||||||
| 0.533 | 0.974 | 60 mAU/mL | |||||||
|
| |||||||||
| Hsia [16] | Taiwan, China | 2007 | 26 | AFP | ELISA | 0.620 | 0.880 | 20 ng/mL | Eur. J. Surg. Oncol. |
|
| |||||||||
| Hu [17] | China | 2010 | 31 | AFP | ELISA | 0.480 | 0.970 | 36 ug/L | Med. Oncol. |
| AFP + GP73 | ELISA/western blotting | 0.770 | 0.840 | 7.4 RU | |||||
|
| |||||||||
| Hussein [18] | Egypt | 2008 | 49 | AFP | ELISA | 0.900 | 0.930 | 7.7 ng/mL | Indian J. Cancer |
|
| |||||||||
| Ikoma [19] | Japan | 2002 | 63 | AFP | ELISA | 0.510 | 0.830 | 20 ng/mL | Hepato Gastroenterol. |
| DCP | ELISA | 0.390 | 0.960 | 16 mAU/mL | |||||
| AFP + DCP | ELISA/ELISA | 0.830 | 0.840 | 20/16 | |||||
|
| |||||||||
| Ertle [20] | Germany | 2011 | 170 | AFP | ELISA | 0.310 | 0.960 | 200 ng/mL | J. Hepatol. |
| DCP | LiBASys | 0.600 | 0.940 | 7.5 ng/mL | |||||
| AFP-L3 | LiBASys | 0.410 | 0.990 | 10% | |||||
|
| |||||||||
| Yamamoto [21] | Japan | 2009 | 714 | AFP | immunometric assay | 0.649 | 0.829 | 11 ng/mL | Ann. Surg. Oncol. |
| 0.608 | 0.861 | 13 ng/mL | |||||||
| 0.513 | 0.908 | 20 ng/mL | |||||||
| 0.304 | 0.986 | 100 ng/mL | |||||||
| 0.247 | 0.990 | 200 ng/mL | |||||||
| DCP | two-step enzyme immunoassay | 0.734 | 0.947 | 20 mAU/mL | |||||
| 0.628 | 0.994 | 30 mAU/mL | |||||||
| 0.559 | 0.998 | 40 mAU/mL | |||||||
| 0.419 | 1.000 | 100 mAU/mL | |||||||
| 0.391 | 1.000 | 125 mAU/mL | |||||||
|
| |||||||||
| Volk [22] | USA | 2007 | 84 | AFP | IAUEC | 0.860 | 0.930 | 150 mAU/mL | Cancer Biomark. |
| 0.690 | 0.910 | 23 ng/mL | |||||||
| AFP-L3 | IAUEC | 0.570 | 0.880 | 3% | |||||
| AFP + DCP | IAUEC/ELISA | 0.880 | 0.890 | 23 ng/mL/150 mAU/mL | |||||
|
| |||||||||
| Mao [23] | China | 2010 | 789 | AFP + GP73 | ELISA/Immunoblot | 0.892 | 0.852 | 35 ng/mL/8.5 RU | Gut |
| GP73 | Immunoblot | 0.750 | 0.970 | 8.5 RU | |||||
| AFP | ELISA/Immunoblot | 0.580 | 0.850 | 35 ug/L | |||||
|
| |||||||||
| Yamamoto [24] | Japan | 2010 | 96 | AFP | ELISA | 0.400 | 0.830 | 15 ng/mL | J. Gastroenterol. |
| 0.390 | 0.870 | 20 ng/mL | |||||||
| 0.280 | 0.960 | 124 ng/mL | |||||||
| 0.220 | 0.960 | 200 ng/mL | |||||||
| DCP | Immunoblot | 0.770 | 0.580 | 20 mAU/mL | |||||
| 0.590 | 0.810 | 30 mAU/mL | |||||||
| 0.550 | 0.910 | 40 mAU/mL | |||||||
| 0.520 | 0.960 | 60 mAU/mL | |||||||
| AFP-L3 | IAUEC | 0.240 | 0.920 | 5% | |||||
| 0.220 | 0.960 | 10% | |||||||
| 0.170 | 0.970 | 15% | |||||||
| 0.150 | 0.970 | 20% | |||||||
| AFP + DCP | Immunoblot | 0.690 | 0.790 | 20 ng/mL/40 mAU/mL | |||||
| 0.680 | 0.830 | 20 ng/mL/60 mAU/mL | |||||||
| 0.590 | 0.900 | 400 ng/mL/40 mAU/mL | |||||||
| 0.570 | 0.950 | 400 ng/mL/60 mAU/mL | |||||||
| AFP + AFP-L3 | Immunoblot/IAUEC | 0.400 | 0.870 | 20 ng/mL/irrespective | |||||
| 0.260 | 0.960 | 20–400 ng/mL/10% | |||||||
| 0.260 | 0.970 | 20–400 ng/mL/15% | |||||||
| 0.180 | 0.990 | 400 ng/mL/irrespective | |||||||
|
| |||||||||
| Marrero [25] | USA | 2003 | 55 | AFP | IAUEC | 0.770 | 0.790 | 11 ng/mL | Hepatology |
| 0.680 | 0.860 | 20 ng/mL | |||||||
| 0.470 | 0.980 | 100 ng/mL | |||||||
| 0.340 | 1.000 | 400 ng/mL | |||||||
| DCP | ELISA | 0.890 | 0.950 | 125 mAU/mL | |||||
| 0.870 | 0.970 | 150 mAU/mL | |||||||
| AFP + DCP | IAUEC/ELISA | 0.880 | 0.950 | logAFP + 4.6 * logDCP | |||||
|
| |||||||||
| Colombo [26] | Italy | 2001 | 55 | AFP | ELISA | 0.390 | 0.760 | 20 ng/ml | Clin. Liver Dis. |
| 0.130 | 0.970 | 100 ng/mL | |||||||
|
| |||||||||
| Nguyen [27] | USA | 2002 | 163 | AFP | ELISA | 0.784 | 0.611 | 10 ng/mL | Hepatology |
| 0.630 | 0.799 | 20 ng/mL | |||||||
| 0.506 | 0.893 | 50 ng/mL | |||||||
| 0.414 | 0.973 | 100 ng/mL | |||||||
| 0.321 | 1.000 | 200 ng/mL | |||||||
|
| |||||||||
| Marrero [28] | USA | 2009 | 419 | AFP | LiBASys | 0.590 | 0.900 | 20 ng/mL | Gastroenterology |
| DCP | ELISA | 0.740 | 0.700 | 150 mAU/mL | |||||
| AFP-L3 | LiBASys | 0.420 | 0.970 | 10% | |||||
| AFP + DCP | ELISA + LiBASys | 0.860 | 0.630 | 20 ng/mL/150 mAU/mL | |||||
|
| |||||||||
| Shafie [29] | Egypt | 2012 | 31 | AFP | ELISA | 0.810 | 0.850 | 32.64 ng/mL | Life Sci. J. |
| 0.770 | 0.600 | 28.51 ng/mL | |||||||
| AFP + GP73 | ELISA | 0.870 | 0.950 | 32.64 ng/mL/7.62 ng/mL | |||||
| 0.900 | 0.900 | 28.51 ng/mL/7.62 ng/mL | |||||||
|
| |||||||||
| Morota [30] | Japan | 2011 | UN | AFP | ELISA | 0.630 | 0.920 | 15.3 ug/L | Clin. Chem. Lab. Med. |
| AFP + GP73 | ELISA | 0.890 | 0.620 | 94.7 ug/L | |||||
|
| |||||||||
| Marrero [31] | USA | 2005 | 144 | AFP | ELISA | 0.300 | 0.960 | 99 ug/L | J. Hepatol. |
| AFP + GP73 | ELISA/Immunoblot | 0.690 | 0.750 | 10.0 RU | |||||
|
| |||||||||
| Tong [32] | USA | 2001 | 31 | AFP | ELISA | 0.410 | 0.950 | 24 ng/mL | J. Gastroenterol. Hepatol. |
| 0.410 | 0.940 | 21 ng/mL | |||||||
| 0.450 | 0.940 | 19 ng/mL | |||||||
| 0.550 | 0.930 | 16 ng/mL | |||||||
| 0.590 | 0.910 | 13 ng/mL | |||||||
| 0.860 | 0.890 | 11 ng/mL | |||||||
| 0.860 | 0.850 | 8 ng/mL | |||||||
|
| |||||||||
| Nomura [33] | Japan | 1999 | 36 | AFP | ELISA | 0.590 | 0.760 | 20 ng/mL | Am. J. Gastroenterol. |
| DCP | Immunoblot | 0.280 | 0.960 | 40 mAU/mL | |||||
| AFP-L3 | ECLIA | 0.220 | 0.940 | 10% | |||||
|
| |||||||||
| Oka [34] | Japan | 2001 | 388 | AFP | ELISA | 0.550 | 0.490 | 20 ng/mL | J. Gastroenterol. Hepatol. |
| AFP-L3 | LAEC | 0.280 | 0.930 | 10% | |||||
| 0.210 | 0.990 | 15% | |||||||
|
| |||||||||
| Ozkan [35] | Turkey | 2011 | 75 | AFP | ELISA | 0.820 | 0.950 | 4.36 ug/L | Digestion |
| 0.690 | 0.950 | 13 ng/mL | |||||||
| 0.760 | 0.950 | 8.46 ng/mL | |||||||
| 0.600 | 0.980 | 20 ng/mL | |||||||
| 0.460 | 1.000 | 100 ng/mL | |||||||
| 0.390 | 1.000 | 200 ng/mL | |||||||
| AFP + GP73 | ELISA | 0.070 | 0.950 | 20 ng/mL/2.36 ug/L | |||||
| 0.820 | 0.090 | 20 ng/mL/0.078 ng/mL | |||||||
| 0.000 | 0.950 | 20 ng/mL/24.43 ng/mL | |||||||
|
| |||||||||
| Peng [36] | Taiwan, China | 1999 | 205 | AFP | ELISA | 0.450 | 1.000 | 200 ug/L | Hepato Gastroenterol. |
| 0.650 | 0.870 | 20 ug/L | |||||||
|
| |||||||||
| Porta [37] | Italy | 2008 | 30 | AFP | ELISA | 0.630 | 0.880 | 12.8 ng/mL | Ann. Oncol. |
|
| |||||||||
| Romeo [38] | Italy | 2010 | 86 | AFP | μ TAS | 0.465 | 0.868 | 20 ng/mL | J. Clin. Oncol. |
| DCP | μ TAS | 0.663 | 0.842 | 0.5 ng/mL | |||||
| 0.558 | 0.921 | 0.75 ng/mL | |||||||
| 0.209 | 1.000 | 2.5 ng/mL | |||||||
| 0.151 | 1.000 | 7.5 ng/mL | |||||||
| AFP-L3 | μ TAS | 0.779 | 0.526 | 5 ng/ml | |||||
| 0.558 | 0.789 | 7 ng/mL | |||||||
| 0.314 | 0.895 | 10 ng/mL | |||||||
| AFP + DCP | μ TAS | 0.698 | 0.789 | 20 ng/mL + 0.75 ng/mL | |||||
| AFP + AFP-L3 | μ TAS | 0.651 | 0.711 | 20 ng/mL + 10 ng/mL | |||||
| 0.791 | 0.684 | 20 ng/mL + 1010 ng/mL | |||||||
|
| |||||||||
| Sassa [39] | Japan | 1999 | 61 | AFP | ELISA | 0.080 | 1.000 | 200 ng/mL | Eur. J. Gastroenterol. Hepatol. |
| DCP | immunoassay | 0.440 | 0.950 | 40 mAU/mL | |||||
| AFP-L3 | LAEC | 0.230 | 0.990 | 10% | |||||
| AFP + DCP | ELISA/immunoassay | 0.480 | 0.990 | 200ng/mL/40 mAU/mL | |||||
| AFP + AFP-L3 | ELISA/LAEC | 0.250 | 0.990 | 200 ng/mL/10% | |||||
|
| |||||||||
| Shi [40] | China | 2011 | 73 | AFP | ELISA | 0.750 | 0.750 | 400 ug/L | Technol. Cancer Res. Treat |
| AFP + GP73 | ELISA | 0.980 | 0.950 | 400 ug/L/100.0 ug/L | |||||
|
| |||||||||
| Shimauch [41] | Japan | 1999 | 21 | AFP-L3 | Immunoblot | 0.330 | 0.930 | 10% | Oncol. Rep. |
| DCP | Immunoblot | 0.430 | 0.970 | 40mAU/mL | |||||
|
| |||||||||
| Sterling [42] | USA | 2009 | 74 | AFP | LiBASys | 0.990 | 0.200 | 200 ng/mL | Clin. Gastroenterol. Hepatol. |
| 0.608 | 0.711 | 20 ng/mL | |||||||
| DCP | LiBASys | 0.760 | 0.580 | 40 mAU/mL | |||||
| LiBASys | 0.390 | 0.900 | 7.5 ng/mL | ||||||
| AFP+DCP | LiBASys | 0.703 | 0.634 | 20 ng/mL/7.5 ng/mL | |||||
| AFP + AFP-L3 | LiBASys | 0.689 | 0.664 | 20 ng/mL/10 | |||||
| AFP-L3 | LiBASys | 0.365 | 0.916 | 10% | |||||
|
| |||||||||
| Sun [43] | China | 2009 | 79 | AFP-L3 | ACSC method | 0.848 | 0.925 | 10 | J. Gastroenterol. Hepatol. |
|
| |||||||||
| Tian [44] | China | 2010 | 153 | AFP | ELISA | 0.950 | 0.470 | 13.6 ug/L | Int. J. Cancer |
| AFP + GP73 | ELISA | 0.750 | 0.520 | 113.8 ug/L | |||||
|
| |||||||||
| Trevisani [45] | Italy | 2001 | 170 | AFP | ELISA | 0.600 | 0.906 | 20 ug/L | J. Hepatol. |
| 0.624 | 0.894 | 16 ug/L | |||||||
| 0.312 | 0.988 | 100 ug/L | |||||||
| 0.224 | 0.994 | 200 ug/L | |||||||
| 0.171 | 0.994 | 400 ug/L | |||||||
|
| |||||||||
| Wang [46] | USA | 2009 | 164 | AFP | ELISA | 0.950 | 0.210 | NK | Cancer Epidemiol. Biomark. Prev. |
| 0.500 | 0.980 | NK | |||||||
| 0.750 | 0.640 | NK | |||||||
| 0.900 | 0.360 | NK | |||||||
| 0.950 | 0.210 | NK | |||||||
| 1.000 | 0.040 | NK | |||||||
|
| |||||||||
| GP73 | Immunoblot | 0.500 | 0.970 | NK | |||||
| 0.750 | 0.860 | NK | |||||||
| 0.900 | 0.540 | NK | |||||||
| 0.950 | 0.350 | NK | |||||||
| 1.000 | 0.250 | NK | |||||||
|
| |||||||||
| AFP + GP73 | ELISA/Immunoblot | 0.500 | 0.990 | NK | |||||
| 0.750 | 0.870 | NK | |||||||
| 0.900 | 0.680 | NK | |||||||
| 0.950 | 0.550 | NK | |||||||
| 1.000 | 0.130 | NK | |||||||
|
| |||||||||
| LI [47] | China | 2009 | 50 | AFP | ELISA | 0.250 | 0.970 | 11.23 ng/mL | Hepatology |
| AFP + GP73 | Immunoblot | 0.620 | 0.880 | 14.37 RU | |||||
AFP: alpha-fetoprotein; DCP: des-gamma-carboxy prothrombin; GP73: Golgi protein-73; AFP-L3: Alpha-fetoprotein L3 isoform, ELISA: enzyme-linked immunosorbent assay; ACSC: Lens culinaris agglutinin (LCA)-coupled spin column; EIA: conventional enzyme immunoassay; μTAS: micro-total analysis system; IAUEC: immunometric assays utilizing enhanced chemiluminescence; ECLIA: immunoassay using the electrochemiluminescence detection system; LiBASys: LiBASys automated immunologic analyzer; LAEC: lecithin-affinity electrophoresis coupled with antibody-affinity blotting; NK: not known.
: Multiply.
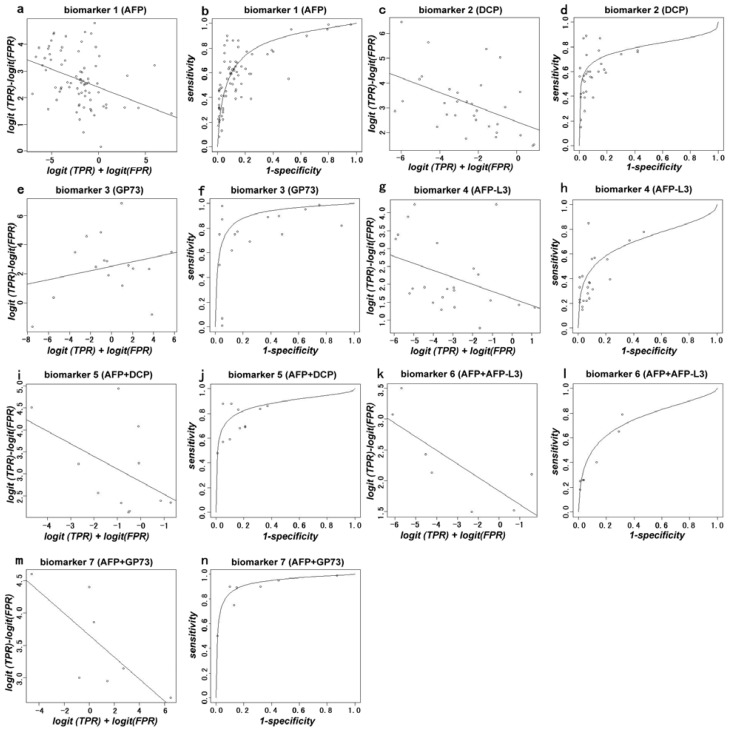
In this meta-analysis, AFP was considered to be the reference biomarker. The area under the curve (AUC) and S-values were the major indicators. The AUC for 1, 2, 3, 4, 5, 6 and 7 biomarkers or the associated compounds were 0.835, 0.797, 0.914, 0.710, 0.874, 0.748, and 0.932 respectively. It was found that the AUC of biomarkers 3, 5 and 7 were superior to that of the reference biomarker 1, while the AUC of biomarkers 2, 4 and 6 were inferior to that of the reference biomarker 1 (Table 3). The S-value represents the positive rate of the biomarkers for detecting HCC. Using biomarker 1 as a reference marker, the S-values of biomarkers 2, 3, 4, 5 and 6 were not significantly different from that of AFP (p > 0.05). The S-value of biomarker 7 was significantly different as compared with AFP (p < 0.05) (Table 4). The plots for calculating the pooled AUC, and the S- and D-values for each biomarker are shown in (Figure 2).
Table 3.
The area under the curve (AUC) for each marker in the meta-analysis.
| Biomarker | Number of Studies | AUC |
|---|---|---|
| 1 (AFP) | 35 | 0.835 |
| 2 (DCP) | 15 | 0.797 |
| 3 (GP73) | 9 | 0.914 |
| 4 (AFP-L3) | 15 | 0.710 |
| 5 (AFP+DCP) | 8 | 0.874 |
| 6 (AFP+AFP-L3) | 3 | 0.748 |
| 7 (AFP+GP73) | 3 | 0.932 |
AFP: alpha-fetoprotein; DCP: des-gamma-carboxy (abnormal) prothrombin; GP73: golgi protein-73; AFP-L3: Alpha-fetoprotein L3 isoform.
Table 4.
The S-values of the biomarkers in the meta-analysis.
| Estimate | Std. Error | t Value | Pr (>|t|) | |
|---|---|---|---|---|
| (Intercept) | 2.39257 | 0.15197 | 15.744 | <2 × 10−16 |
| S.Biomarker.1 | 0.13594 | 0.04532 | 2.999 | 0.00314 |
| S.Biomarker.2 | 0.29219 | 0.10222 | 2.859 | 0.00483 |
| S.Biomarker.3 | 0.15326 | 0.08245 | 1.859 | 0.06492 |
| S.Biomarker.4 | −0.19643 | 0.12226 | −1.607 | 0.11012 |
| S.Biomarker.5 | −0.28662 | 0.20797 | −1.378 | 0.17009 |
| S.Biomarker.6 | 0.21913 | 0.17122 | 1.280 | 0.20250 |
| S.Biomarker.7 | −0.16597 | 0.13200 | 1.257 | 0.21050 |
| Biomarker.2 | 0.08054 | 0.36171 | 0.223 | 0.82409 |
| Biomarker.3 | 0.13195 | 0.31404 | 0.420 | 0.67494 |
| Biomarker.4 | −0.78803 | 0.47604 | −1.655 | 0.09983 |
| Biomarker.5 | 0.43157 | 0.40973 | 1.053 | 0.29381 |
| Biomarker.6 | 0.77644 | 0.70680 | 1.099 | 0.27364 |
| Biomarker.7 | 1.21688 | 0.48657 | 2.501 | 0.01341 |
The statistical significance level was set to p < 0.05. The S-value, which represents the positive rate of the biomarker for detecting HCC, was calculated as follows: S = logit (TPR) + logit (FPR), where TPR is the true positive rate (sensitivity) and FPR is the false positive rate (1-specificity).
Figure 2.
Plots for calculating the area under the curve (AUC) and D (log odds ratio) against S (implicit threshold) for biomarker 1 to biomarker 7. The S-value represents the positive rate of the biomarker for detecting HCC. S = logit (TPR) + logit (FPR), where TPR is the true positive rate (sensitivity) and FPR is the false positive rate (1-specificity) for AFP. D represents the ability of distinguishing HCC and the control. D = logit (TPR) − logit (FPR) (a, c, e, g, i, k, m). The AUC of biomarkers 1 to biomarker 7 are 0.835, 0.797, 0.914, 0.710, 0.874, 0.748, 0.932 respectively (b, d, f, h, j, l, n).
2.2. Discussion
HCC remains one of the most common malignant tumors. Early diagnosis and early surgical extraction are imperative for improving the survival of HCC patients [1,4,5]. AFP, a specific glycoprotein produced primarily by the fetal liver has been the most practical and widely used serum biomarker for HCC diagnosis. However, its sensitivity and specificity varied significantly ranging from 40%–65% and 76%–96%, respectively [45,48,49]. The AFP value is often elevated at a milder level in patients with chronic hepatitis C infection in the absence of HCC [27]. An AFP value >400 ng/mL is considered ideal for diagnosing HCC [27]. Even though normal AFP levels can be seen in approximately one-third of patients with HCC [49], a large number of HCC patients have AFP values <400 ng/mL, making them very difficult to undergo detection and prognosis of HCC [49]. Other conventional clinical tumor associated biomarkers such as CEA, CA199, CA724 etc. are not practical in the clinic because of their poor sensitivity and specificity. The present situation requires an urgent need to explore new markers to overcome these drawbacks in liver cancer diagnosis.
An ideal serum biomarker should be both sensitive and specific for HCC detection at an early stage, and be easy to test, reproduce, as well as be non-invasive [50]. With the latest developments in molecular techniques, several new HCC-specific biomarkers including AFP-L3, DCP and GP73 have been discovered [51,52]. These new markers have been investigated for their diagnostic accuracy and potential for HCC detection [53,54]. However, the clinical usefulness of these biomarkers needs to be carefully evaluated and validated. Thus, we aimed to evaluate the utility of the biomarkers individually, as well as their combined application in the early detection of HCC and for their usefulness in therapeutic decision-making.
AFP-L3, one of the AFP isoforms, has a high binding affinity to lectin Lens culinaris agglutinin. It has been reported that AFP-L3 is a more valuable index than total AFP for early diagnosis of HCC [24,51]. The proportion of AFP-L3 over the total AFP concentration has been used as a marker for early diagnosis and assessment of the therapeutic effect as well as prognosis of HCC [51]. AFP-L3 was found to be associated with liver dysfunction, poor differentiation, and other biologically malignant characteristics [48]. If total AFP concentration is below 10 ng/mL, the absolute value of AFP-L3 would be hard to be detected. However, AFP-L3 instead of AFP can be detected in the serum of some patients with tumors smaller than two centimeters in size. Generally, AFP-L3 has been detected in approximately one-third of HCC patients with cutoff values of 10%–15% (percentage of AFP-L3 over AFP) [2,55]. Therefore, percentage of AFP-L3 is often used when AFP concentration is above 10 ng/mL, especially within levels between 10–200 ng/mL [8]. In the clinic, it is a diagnostic dilemma for patients with total AFP values of 10–200 ng/mL [8]. For these cases, AFP-L3 may be a better complement index for diagnosing HCC when combined with AFP. However, because its sensitivity and specificity range from 36%–96%, and 89%–94%, respectively [34,48,49,53,56,57], drawing a conclusion requires caution. For example, Nouso K et al. found that the sensitivity of AFP-L3 in patients of HCC with low AFP (under 20 ng/mL) was 51.5%, 13.3%, and 8.7% at cutoff levels of 5%, 10%, and 15%, respectively [58]. Leerapun, A. et al. found that in patients with total AFP values of 10–200 ng/mL, the AFP-L3 was greater than 10% and had a sensitivity of 71% and a specificity of 63% for diagnosing HCC [8]. With an AFP-L3 greater than 35%, the specificity for HCC diagnosis reached 100% while reducing sensitivity to 33% [8]. Nonetheless, the combination of AFP-L3% and AFP significantly improved the specificity (100%) of diagnosis of HCC [8]. Thus, they proposed that the AFP-L3% should be taken as a potential marker for AFP in the diagnosis of HCC, although no prognostic significance for AFP-L3% was observed after adjustment for total AFP [8]. Our meta-analysis result showed that AFP-L3 alone or combined with AFP was not superior to AFP (AUC: 0.710, 0.748 vs. 0.835) (Table 3). However, significant variations for interpreting the present studies arose due to different assay methods, cutoff values, and study populations.
As a new serum biomarker in patients with HCC, DCP, or prothrombin, induced by vitamin K absence-II (PIVKA-II) was first described by Liebman et al. [59]. DCP is an abnormal protein that is increased in the serum of patients with HCC. With a cutoff value of 40 mAU/mL, the sensitivity and specificity of DCP for diagnosing HCC ranges from 28%–89%, and 87%–96% respectively [19,25,33,60–65]. DCP at a 125 mAU/mL had a high sensitivity (89%) and specificity (95%) for differential diagnosis of HCC from cirrhosis and chronic hepatitis [25]. The areas under the ROC curve for DCP (125 mAU/mL) and AFP (11 ng/mL) were 0.928 vs. 0.810, respectively [25]. Another case-controlled study comparing the AFP value of diagnosing HCC with DCP showed that a cutoff value of 60 mAU/mL for DCP had a higher sensitivity than AFP (with a cutoff value 20 ng/mL) (75.5% vs. 68.4%) [60]. Therefore, DCP is considered as a valuable complement prognostic predictor for HCC [66,67]. Nevertheless, just as our meta-analysis showed, DCP was not statistically better than AFP (AUC: 0.797 vs. 0.835), albeit combined measurement of DCP and AFP was superior to AFP alone (AUC: 0.874 vs. 0.835) (Table 3). As a biomarker of HCC, more appropriate and accurate evaluations of DCP are expected in future studies.
GP73, also called Golgi phosphoprotein 2 (GOLPH2), is a resident Golgi transmembrane glycoprotein with 400 amino acids and the 73kDa molecular weight was found up-regulated in expression in virus-infected hepatocyte [52]. Several recent studies indicate that GP73 is one of the most promising serum markers for HCC. Although there are studies reporting that the sensitivity of GP73 was higher than that of AFP in the diagnosis of early HCC (62% vs. 25%), the potential clinical value of GP73 as a better serum biomarker than AFP remains controversial [7,17,31,54,68]. A large cohort study of HCC by Mao et al. showed that GP73 was a valuable tumor biomarker for HCC and was superior to AFP with respect to sensitivity and specificity after comparing the adjusted factors such as the likelihood ratio and predictive value, which are independent of the age and gender of the subjects [23]. They also found that combined measurement of GP73 and AFP could further increase the sensitivity for the detection of HCC. Using 8.5 relative units as the cut-off value, the sensitivity and specificity of serum GP73 for HCC were 74.6% (95% confidence interval (CI), 71.5%–77.6%) and 97.4% (95% CI, 96.8%–98.3%) [23]. Combined measurement of GP73 and AFP increased the sensitivity for HCC to 89.2% (95% CI, 86.7%–91.5%), with a specificity of 85.2% (95% CI, 83.4%–86.4%) [23], which indicated that serum GP73 was dramatically elevated in patients with HCC and that the sensitivity and specificity of GP73 for HCC might be superior to that of AFP [23]. Another meta-analysis by Zhou et al. found that, as an independent marker for diagnosis of HCC, GP73 is comparable to AFP [69]. In our study, the result showed that GP73 and AFP combined were dramatically superior to AFP (AUC: 0.914, 0.932 vs. 0.835), which was similar to the results above (Table 3). However, there were several drawbacks in our study. For instance, the data extracted from the paper was not enough to conclude for certain that GP73 and AFP were more effective when applied together. Moreover, the assay methods and the cutoff values varied in these studies.
The results of this meta-analysis showed that the AUC of biomarkers 3, 5 and 7 were superior to that of the reference biomarker AFP, while the AUC of biomarkers 2, 4, and 6 were inferior to that of the reference biomarker AFP. Based on our tendency to conclude that GP73, together with DCP + AFP, with the combined measurement of GP73 + AFP could increase detection of HCC, this may be superior to AFP for diagnosis and screening in the early stages of HCC. Using biomarker 1 (AFP) as the reference marker, there is no significant difference in the S-value between biomarkers 2, 3, 4, 5 and 6 (p > 0.05), while the S-value of biomarker 7 (AFP + GP73) was significantly different (p < 0.05), suggesting that biomarker 7 may be more valuable and useful in clinical practice, although the compound value of AFP + GP73 still calls for further research and evaluation.
The clinical value of a biomarker depends not only on the high sensitivity and specificity but also on the universality and availability for practice. Technologies of testing assays for these biomarkers vary, including: ELISA, LiBASys, μTAS, IAUEC, ECLIA, EIA, LAEC, and immunoblot. Some may not been used worldwide and their costs differ significantly. However, with the optimization and improvement of technology, such problems are expected to be resolved. The costs of these technologies could not be extracted from the original citation papers, which suggests that in future studies, financial factors should be taken into consideration. According to the inclusion criteria, although the obtained reports of each biomarker may bring potential bias, they do not affect statistical analysis with Empower Stats software package (Empower Stats, X & Y Solutions, Boston, MA, USA). Therefore, more caution needs to be taken with the results.
3. Experimental Section
3.1. Identification of Studies
To assess biomarkers for HCC, a comprehensive literature search of original research articles published between January 1999 and July 2012 (cut-off date 1 July) was conducted using the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed), Web of Science (http://www.isiknowledge.com), and Cochrane Library (http://www.thecochranelibrary.com).
3.2. Literature Screening
Literature screening was performed at four levels. At level 1, we excluded reviews, letters, case reports, editorials, and comments. At level 2, we excluded the articles in which biomarkers were not evaluated for their utility in detecting HCC and content duplicated articles. At level 3, we ensured the articles included serum biomarkers: AFP, DCP, GP73, or AFP-L3 for diagnosing HCC in their studies. The data pertaining to other biomarkers were excluded from further analysis. Articles were further screened to ensure that the data in those studies pertained to patients with HCC and appropriate control populations. At level 4, only reports with sensitivity and specificity data for the biomarkers were selected. A total of 40 reports met the inclusion criteria for meta-analysis.
3.3. Data Extraction
Data extracted from the selected papers included authors, country, year of publication, journal, number of patients, test methods and results, sensitivity, specificity, and cut-off points for the biomarkers.
3.4. Statistical Analysis
Data from disparate reports were summarized by the method described by Littenberg and Moses using a logistic transformation and linear regression we generated a summary receiver operating characteristic (sROC) curve [70]. The ROC curve has been demonstrated to be useful for summarizing the diagnostic accuracy of multiple reports, comparing technologies, detecting outliers, and identifying the optimum operating point of the test.
The sensitivity and specificity of the biomarkers from the included studies were logistically transformed, and then a linear regression line was fitted through the data points. This line was back-transformed to obtain the sROC curve [7], which is a compact description of the accuracy of the diagnostic test in many populations [48,70]. We did not extrapolate the curve beyond the range of the logistically transformed data.
The AUC, as one of the serum biomarkers, was obtained from the included studies. For each biomarker, the pooled AUC was calculated with the inverse standard errors as weights. The pooled AUC, together with similarly pooled standard errors, was used to compare the accuracy of these diagnostic tests [7].
Two parameters were used to describe the meta-analysis data S, a sum of the two transforms, is related to the frequency when the test is positive, which depends on the test threshold D, the difference between the two transforms, is a measure of the successful degree of the test to discriminate between the populations of healthy subjects and HCC [70].
AFP was taken as the reference marker for performing comparisons with other biomarkers. Student’s t-test was used to compare the pooled AUC of AFP and the pooled AUC of each new biomarker. Statistical analysis was performed using the Empower Stats software package (Empower Stats, X & Y Solutions, Boston, MA, USA). Differences were considered statistically significant at a p < 0.05.
4. Conclusions
The results of our meta-analysis suggested that AFP+GP73 is superior to AFP alone in diagnosing HCC and differentiating HCC patients from non-HCC patients, therefore, it might be a useful compound marker in the diagnosis and screening of potential HCC patients. In addition, the values of GP73, AFP + DCP and AFP + GP73 are also better than that of AFP alone. The clinical value of GP73, AFP + DCP, or AFP + GP73 as serological markers for early diagnosis of HCC needs to be evaluated further in future studies using stricter criteria.
Acknowledgments
Statistical analysis was performed using the Empower Stats software package (Empower Stats, X & Y Solutions, Boston, MA, USA), which was supported and directed by Changzhong Chen in the Department of Biostatistics of Harvard University.
We are very grateful to the authors of the primary studies included in our meta-analysis; due to their contributions, this work could be carried out successfully.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Stefaniuk P., Cianciara J., Wiercinska-Drapalo A. Present and future possibilities for early diagnosis of hepatocellular carcinoma. World J. Gastroenterol. 2010;16:418–424. doi: 10.3748/wjg.v16.i4.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oka H., Tamori A., Kuroki T., Kobayashi K., Yamamoto S. Prospective study of alpha-fetoprotein in cirrhotic patients monitored for development of hepatocellular carcinoma. Hepatology. 1994;19:61–66. [PubMed] [Google Scholar]
- 3.Zoli M., Magalotti D., Bianchi G., Gueli C., Marchesini G., Pisi E. Efficacy of a surveillance program for early detection of hepatocellular carcinoma. Cancer. 1996;78:977–985. doi: 10.1002/(SICI)1097-0142(19960901)78:5<977::AID-CNCR6>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 4.Behne T., Copur M.S. Biomarkers for hepatocellular carcinoma. Int. J. Hepatol. 2012 doi: 10.1155/2012/859076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masuzaki R., Karp S.J., Omata M. New serum markers of hepatocellular carcinoma. Semin. Oncol. 2012;39:434–439. doi: 10.1053/j.seminoncol.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Ba M.C., Long H., Tang Y.Q., Cui S.Z. GP73 expression and its significance in the diagnosis of hepatocellular carcinoma: A review. Int. J. Clin. Exp. Pathol. 2012;5:874–881. [PMC free article] [PubMed] [Google Scholar]
- 7.Norton P.A., Comunale M.A., Krakover J., Rodemich L., Pirog N., D’Amelio A., Philip R., Mehta A.S., Block T.M. N-linked glycosylation of the liver cancer biomarker GP73. J. Cell. Biochem. 2008;104:136–149. doi: 10.1002/jcb.21610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leerapun A., Suravarapu S.V., Bida J.P., Clark R.J., Sanders E.L., Mettler T.A., Stadheim L.M., Aderca I., Moser C.D., Nagorney D.M., et al. The utility of Lens culinaris agglutinin-reactive alpha-fetoprotein in the diagnosis of hepatocellular carcinoma: Evaluation in a United States referral population. Clin. Gastroenterol. Hepatol. 2007;5:394–402. doi: 10.1016/j.cgh.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cedrone A., Covino M., Caturelli E., Pompili M., Lorenzelli G., Villani M.R., Valle D., Sperandeo M., Rapaccini G.L., Gasbarrini G. Utility of alpha-fetoprotein (AFP) in the screening of patients with virus-related chronic liver disease: Does different viral etiology influence AFP levels in HCC? A study in 350 western patients. Hepato Gastroenterol. 2000;47:1654–1658. [PubMed] [Google Scholar]
- 10.Wang C.S., Lin C.L., Lee H.C., Chen K.Y., Chiang M.F., Chen H.S., Lin T.J., Liao L.Y. Usefulness of serum des-gamma-carboxy prothrombin in detection of hepatocellular carcinoma. World J. Gastroenterol. 2005;11:6115–6119. doi: 10.3748/wjg.v11.i39.6115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Durazo F.A., Blatt L.M., Corey W.G., Lin J.H., Han S., Saab S., Busuttil R.W., Tong M.J. Des-gamma-carboxyprothrombin, alpha-fetoprotein and AFP-L3 in patients with chronic hepatitis, cirrhosis and hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2008;23:1541–1548. doi: 10.1111/j.1440-1746.2008.05395.x. [DOI] [PubMed] [Google Scholar]
- 12.Giannelli G., Fransvea E., Trerotoli P., Beaugrand M., Marinosci F., Lupo L., Nkontchou G., Dentico P., Antonaci S. Clinical validation of combined serological biomarkers for improved hepatocellular carcinoma diagnosis in 961 patients. Clin. Chim. Acta. 2007;383:147–152. doi: 10.1016/j.cca.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 13.Giannelli G., Marinosci F., Trerotoli P., Volpe A., Quaranta M., Dentico P., Antonaci S. SCCA antigen combined with alpha-fetoprotein as serologic markers of HCC. Int. J. Cancer. 2005;117:506–509. doi: 10.1002/ijc.21189. [DOI] [PubMed] [Google Scholar]
- 14.Toyoda H., Kumada T., Tada T., Kaneoka Y., Maeda A., Kanke F., Satomura S. Clinical utility of highly sensitive Lens culinaris agglutinin-reactive alpha-fetoprotein in hepatocellular carcinoma patients with alpha-fetoprotein <20 ng/mL. Cancer Sci. 2011;102:1025–1031. doi: 10.1111/j.1349-7006.2011.01875.x. [DOI] [PubMed] [Google Scholar]
- 15.Okuda H., Nakanishi T., Takatsu K., Saito A., Hayashi N., Watanabe K., Magario N., Yokoo T., Naraki T. Measurement of serum levels of des-gamma-carboxy prothrombin in patients with hepatocellular carcinoma by a revised enzyme immunoassay kit with increased sensitivity. Cancer. 1999;85:812–818. [PubMed] [Google Scholar]
- 16.Hsia C.Y., Huo T.I., Chiang S.Y., Lu M.F., Sun C.L., Wu J.C., Lee P.C., Chi C.W., Lui W.Y., Lee S.D. Evaluation of interleukin-6, interleukin-10 and human hepatocyte growth factor as tumor markers for hepatocellular carcinoma. Eur. J. Surg. Oncol. 2007;33:208–212. doi: 10.1016/j.ejso.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 17.Hu J.S., Wu D.W., Liang S., Miao X.Y. GP73, a resident Golgi glycoprotein, is sensibility and specificity for hepatocellular carcinoma of diagnosis in a hepatitis B-endemic Asian population. Med. Oncol. 2010;27:339–345. doi: 10.1007/s12032-009-9215-y. [DOI] [PubMed] [Google Scholar]
- 18.Hussein M., Ibrahim A., Abdella H., Montasser I., Hassan M. Evaluation of serum squamous cell carcinoma antigen as a novel biomarker for diagnosis of hepatocellular carcinoma in Egyptian patients. Indian J. Cancer. 2008;45:167–172. doi: 10.4103/0019-509x.44666. [DOI] [PubMed] [Google Scholar]
- 19.Ikoma J., Kaito M., Ishihara T., Nakagawa N., Kamei A., Fujita N., Iwasa M., Tamaki S., Watanabe S., Adachi Y. Early diagnosis of hepatocellular carcinoma using a sensitive assay for serum des-gamma-carboxy prothrombin: A prospective study. Hepato Gastroenterol. 2002;49:235–238. [PubMed] [Google Scholar]
- 20.Ertle J.M., Wiehert M., Küper R., Hilgard P., Gerken G., Schlaak J. 965 Sensitivity and specificity of Alpha-Feto Protein (Afp), Lens culinaris agglutinin-reactive Afp (Afp-L3) and des-gamma-carboxyprothrombin (Dcp) as tumor markers in patients with hepatocellular carcinoma (Hcc) J. Hepatol. 2011;54:S385. [Google Scholar]
- 21.Yamamoto K., Imamura H., Matsuyama Y., Hasegawa K., Beck Y., Sugawara Y., Makuuchi M., Kokudo N. Significance of alpha-fetoprotein and des-gamma-carboxy prothrombin in patients with hepatocellular carcinoma undergoing hepatectomy. Ann. Surg. Oncol. 2009;16:2795–2804. doi: 10.1245/s10434-009-0618-y. [DOI] [PubMed] [Google Scholar]
- 22.Volk M.L., Hernandez J.C., Su G.L., Lok A.S., Marrero J.A. Risk factors for hepatocellular carcinoma may impair the performance of biomarkers: A comparison of AFP, DCP, and AFP-L3. Cancer Biomark. 2007;3:79–87. doi: 10.3233/cbm-2007-3202. [DOI] [PubMed] [Google Scholar]
- 23.Mao Y., Yang H., Xu H., Lu X., Sang X., Du S., Zhao H., Chen W., Xu Y., Chi T., et al. Golgi protein 73 (GOLPH2) is a valuable serum marker for hepatocellular carcinoma. Gut. 2010;59:1687–1693. doi: 10.1136/gut.2010.214916. [DOI] [PubMed] [Google Scholar]
- 24.Yamamoto K., Imamura H., Matsuyama Y., Kume Y., Ikeda H., Norman G.L., Shums Z., Aoki T., Hasegawa K., Beck Y., et al. AFP, AFP-L3, DCP, and GP73 as markers for monitoring treatment response and recurrence and as surrogate markers of clinicopathological variables of HCC. J. Gastroenterol. 2010;45:1272–1282. doi: 10.1007/s00535-010-0278-5. [DOI] [PubMed] [Google Scholar]
- 25.Marrero J.A., Su G.L., Wei W., Emick D., Conjeevaram H.S., Fontana R.J., Lok A.S. Des-gamma carboxyprothrombin can differentiate hepatocellular carcinoma from nonmalignant chronic liver disease in american patients. Hepatology. 2003;37:1114–1121. doi: 10.1053/jhep.2003.50195. [DOI] [PubMed] [Google Scholar]
- 26.Colombo M. Screening for cancer in viral hepatitis. Clin. Liver Dis. 2001;5:109–122. doi: 10.1016/s1089-3261(05)70156-2. [DOI] [PubMed] [Google Scholar]
- 27.Nguyen M.H., Garcia R.T., Simpson P.W., Wright T.L., Keeffe E.B. Racial differences in effectiveness of alpha-fetoprotein for diagnosis of hepatocellular carcinoma in hepatitis C virus cirrhosis. Hepatology. 2002;36:410–417. doi: 10.1053/jhep.2002.34744. [DOI] [PubMed] [Google Scholar]
- 28.Marrero J.A., Feng Z., Wang Y., Nguyen M.H., Befeler A.S., Roberts L.R., Reddy K.R., Harnois D., Llovet J.M., Normolle D., et al. Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology. 2009;137:110–118. doi: 10.1053/j.gastro.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.El Shafie M.A., Fawzy A.M., Al Monem E.A., Abbass S., Zakaria D.M., El Baz S. Golgi Protein 73 (GP73) as a novel serum marker for early detection of hepatocellular carcinoma in egyptian patients. Life Sci. J. 2012;9:823. [Google Scholar]
- 30.Morota K., Nakagawa M., Sekiya R., Hemken P.M., Sokoll L.J., Elliott D., Chan D.W., Dowell B.L. A comparative evaluation of Golgi protein-73, fucosylated hemopexin, α-fetoprotein, and PIVKA-II in the serum of patients with chronic hepatitis, cirrhosis, and hepatocellular carcinoma. Clin. Chem. Lab. Med. 2011;49:711–718. doi: 10.1515/CCLM.2011.097. [DOI] [PubMed] [Google Scholar]
- 31.Marrero J.A., Romano P.R., Nikolaeva O., Steel L., Mehta A., Fimmel C.J., Comunale M.A., D’Amelio A., Lok A.S., Block T.M. GP73, a resident Golgi glycoprotein, is a novel serum marker for hepatocellular carcinoma. J. Hepatol. 2005;43:1007–1012. doi: 10.1016/j.jhep.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 32.Tong M.J., Blatt L.M., Kao V.W. Surveillance for hepatocellular carcinoma in patients with chronic viral hepatitis in the United States of America. J. Gastroenterol. Hepatol. 2001;16:553–559. doi: 10.1046/j.1440-1746.2001.02470.x. [DOI] [PubMed] [Google Scholar]
- 33.Nomura F., Ishijima M., Kuwa K., Tanaka N., Nakai T., Ohnishi K. Serum des-gamma-carboxy prothrombin levels determined by a new generation of sensitive immunoassays in patients with small-sized hepatocellular carcinoma. Am. J. Gastroenterol. 1999;94:650–654. doi: 10.1111/j.1572-0241.1999.00930.x. [DOI] [PubMed] [Google Scholar]
- 34.Oka H., Saito A., Ito K., Kumada T., Satomura S., Kasugai H., Osaki Y., Seki T., Kudo M., Tanaka M. Multicenter prospective analysis of newly diagnosed hepatocellular carcinoma with respect to the percentage of Lens culinaris agglutinin-reactive alpha-fetoprotein. J. Gastroenterol. Hepatol. 2001;16:1378–1383. doi: 10.1046/j.1440-1746.2001.02643.x. [DOI] [PubMed] [Google Scholar]
- 35.Ozkan H., Erdal H., Tutkak H., Karaeren Z., Yakut M., Yuksel O., Koklu S. Diagnostic and prognostic validity of Golgi protein 73 in hepatocellular carcinoma. Digestion. 2011;83:83–88. doi: 10.1159/000320379. [DOI] [PubMed] [Google Scholar]
- 36.Peng Y.C., Chan C.S., Chen G.H. The effectiveness of serum alpha-fetoprotein level in anti-HCV positive patients for screening hepatocellular carcinoma. Hepato Gastroenterol. 1999;46:3208–3211. [PubMed] [Google Scholar]
- 37.Porta C., de Amici M., Quaglini S., Paglino C., Tagliani F., Boncimino A., Moratti R., Corazza G.R. Circulating interleukin-6 as a tumor marker for hepatocellular carcinoma. Ann. Oncol. 2008;19:353–358. doi: 10.1093/annonc/mdm448. [DOI] [PubMed] [Google Scholar]
- 38.Romeo R., Sangiovanni A., Iavarone M., Vavassori S., Della Corte C., Colombo M. Diagnostic value of Lens culinaris agglutinin isoform 3 fraction (AFP-L3%) and des-gamma-carboxy prothrombin (DCP) for the diagnosis of hepatocellular carcinoma in cirrhotic patients. J. Clin. Oncol. 2010;28:4119. [Google Scholar]
- 39.Sassa T., Kumada T., Nakano S., Uematsu T. Clinical utility of simultaneous measurement of serum high-sensitivity des-(gamma)-carboxy prothrombin and Lens culinaris agglutinin A-reactive a-fetoprotein in patients with small hepatocellular carcinoma. Eur. J. Gastroenterol. Hepatol. 1999;11:1387–1392. doi: 10.1097/00042737-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Shi Y., Chen J., Li L., Sun Z., Zen L., Xu S., Zhang Y., Zhang L. A study of diagnostic value of Golgi protein GP73 and its genetic assay in primary hepatic carcinoma. Technol. Cancer Res. Treat. 2011;10:287–294. doi: 10.7785/tcrt.2012.500205. [DOI] [PubMed] [Google Scholar]
- 41.Shimauchi Y., Tanaka M., Kuromatsu R., Ogata R., Tateishi Y., Itano S., Ono N., Yutani S., Nagamatsu H., Matsugaki S. A simultaneous monitoring of Lens culinaris agglutinin A-reactive alpha-fetoprotein and des-gamma-carboxy prothrombin as an early diagnosis of hepatocellular carcinoma in the follow-up of cirrhotic patients. Oncol. Rep. 2000;7:249–256. doi: 10.3892/or.7.2.249. [DOI] [PubMed] [Google Scholar]
- 42.Sterling R.K., Jeffers L., Gordon F., Venook A.P., Reddy K.R., Satomura S., Kanke F., Schwartz M.E., Sherman M. Utility of Lens culinaris agglutinin-reactive fraction of alpha-fetoprotein and des-gamma-carboxy prothrombin, alone or in combination, as biomarkers for hepatocellular carcinoma. Clin. Gastroenterol. Hepatol. 2009;7:104–113. doi: 10.1016/j.cgh.2008.08.041. [DOI] [PubMed] [Google Scholar]
- 43.Sun Y., Yang H., Mao Y., Xu H., Zhang J., Li G., Lu X., Sang X., Zhao H., Zhong S., et al. Increased Golgi protein 73 expression in hepatocellular carcinoma tissue correlates with tumor aggression but not survival. J. Gastroenterol. Hepatol. 2011;26:1207–1212. doi: 10.1111/j.1440-1746.2011.06733.x. [DOI] [PubMed] [Google Scholar]
- 44.Tian L., Wang Y., Xu D., Gui J., Jia X., Tong H., Wen X., Dong Z., Tian Y. Serological AFP/Golgi protein 73 could be a new diagnostic parameter of hepatic diseases. Int. J. Cancer. 2011;129:1923–1931. doi: 10.1002/ijc.25838. [DOI] [PubMed] [Google Scholar]
- 45.Trevisani F., D’Intino P.E., Morselli-Labate A.M., Mazzella G., Accogli E., Caraceni P., Domenicali M., de Notariis S., Roda E., Bernardi M. Serum alpha-fetoprotein for diagnosis of hepatocellular carcinoma in patients with chronic liver disease: Influence of HBsAg and anti-HCV status. J. Hepatol. 2001;34:570–575. doi: 10.1016/s0168-8278(00)00053-2. [DOI] [PubMed] [Google Scholar]
- 46.Wang M., Long R.E., Comunale M.A., Junaidi O., Marrero J., di Bisceglie A.M., Block T.M., Mehta A.S. Novel fucosylated biomarkers for the early detection of hepatocellular carcinoma. Cancer Epidemiol. Biomark. Prev. 2009;18:1914–1921. doi: 10.1158/1055-9965.EPI-08-0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li X., Wu K., Fan D. Serum Golgi Phosphoprotein 2 level: A better marker than alpha-fetoprotein for diagnosing early hepatocellular carcinoma. Hepatology. 2009;50:325–325. doi: 10.1002/hep.23028. [DOI] [PubMed] [Google Scholar]
- 48.Khien V.V., Mao H.V., Chinh T.T., Ha P.T., Bang M.H., Lac B.V., Hop T.V., Tuan N.A., Don L.V., Taketa K., et al. Clinical evaluation of lentil lectin-reactive alpha-fetoprotein-L3 in histology-proven hepatocellular carcinoma. Int. J. Biol. Markers. 2001;16:105–111. doi: 10.1177/172460080101600204. [DOI] [PubMed] [Google Scholar]
- 49.Yoshida S., Kurokohchi K., Arima K., Masaki T., Hosomi N., Funaki T., Murota M., Kita Y., Watanabe S., Kuriyama S. Clinical significance of Lens culinaris agglutinin-reactive fraction of serum alpha-fetoprotein in patients with hepatocellular carcinoma. Int. J. Oncol. 2002;20:305–309. [PubMed] [Google Scholar]
- 50.Srivastava S., Gopal-Srivastava R. Biomarkers in cancer screening: A public health perspective. J. Nutr. 2002;132:2471S–2475S. doi: 10.1093/jn/132.8.2471S. [DOI] [PubMed] [Google Scholar]
- 51.Li D., Mallory T., Satomura S. AFP-L3: A new generation of tumor marker for hepatocellular carcinoma. Clin. Chim. Acta. 2001;313:15–19. doi: 10.1016/s0009-8981(01)00644-1. [DOI] [PubMed] [Google Scholar]
- 52.Kladney R.D., Bulla G.A., Guo L., Mason A.L., Tollefson A.E., Simon D.J., Koutoubi Z., Fimmel C.J. GP73, a novel Golgi-localized protein upregulated by viral infection. Gene. 2000;249:53–65. doi: 10.1016/S0378-1119(00)00136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taketa K., Okada S., Win N., Hlaing N.K., Wind K.M. Evaluation of tumor markers for the detection of hepatocellular carcinoma in Yangon General Hospital, Myanmar. Acta Med. Okayama. 2002;56:317–320. doi: 10.18926/AMO/31689. [DOI] [PubMed] [Google Scholar]
- 54.Block T.M., Marrero J., Gish R.G., Sherman M., London W.T., Srivastava S., Wagner P.D. The degree of readiness of selected biomarkers for the early detection of hepatocellular carcinoma: Notes from a recent workshop. Cancer Biomark. 2008;4:19–33. doi: 10.3233/cbm-2008-4103. [DOI] [PubMed] [Google Scholar]
- 55.Taketa K., Sekiya C., Namiki M., Akamatsu K., Ohta Y., Endo Y., Kosaka K. Lectin-reactive profiles of alpha-fetoprotein characterizing hepatocellular carcinoma and related conditions. Gastroenterology. 1990;99:508–518. doi: 10.1016/0016-5085(90)91034-4. [DOI] [PubMed] [Google Scholar]
- 56.Wang S.S., Lu R.H., Lee F.Y., Chao Y., Huang Y.S., Chen C.C., Lee S.D. Utility of lentil lectin affinity of alpha-fetoprotein in the diagnosis of hepatocellular carcinoma. J. Hepatol. 1996;25:166–171. doi: 10.1016/s0168-8278(96)80069-9. [DOI] [PubMed] [Google Scholar]
- 57.Sato Y., Nakata K., Kato Y., Shima M., Ishii N., Koji T., Taketa K., Endo Y., Nagataki S. Early recognition of hepatocellular carcinoma based on altered profiles of alpha-fetoprotein. N. Engl. J. Med. 1993;328:1802–1806. doi: 10.1056/NEJM199306243282502. [DOI] [PubMed] [Google Scholar]
- 58.Nouso K., Kobayashi Y., Nakamura S., Kobayashi S., Takayama H., Toshimori J., Kuwaki K., Hagihara H., Onishi H., Miyake Y., et al. Prognostic importance of fucosylated alpha-fetoprotein in hepatocellular carcinoma patients with low alpha-fetoprotein. J. Gastroenterol. Hepatol. 2011;26:1195–1200. doi: 10.1111/j.1440-1746.2011.06720.x. [DOI] [PubMed] [Google Scholar]
- 59.Liebman H.A., Furie B.C., Tong M.J., Blanchard R.A., Lo K.J., Lee S.D., Coleman M.S., Furie B. Des-gamma-carboxy (abnormal) prothrombin as a serum marker of primary hepatocellular carcinoma. N. Engl. J. Med. 1984;310:1427–1431. doi: 10.1056/NEJM198405313102204. [DOI] [PubMed] [Google Scholar]
- 60.Ishii M., Gama H., Chida N., Ueno Y., Shinzawa H., Takagi T., Toyota T., Takahashi T., Kasukawa R. Simultaneous measurements of serum alpha-fetoprotein and protein induced by vitamin K absence for detecting hepatocellular carcinoma. South Tohoku District Study Group. Am. J. Gastroenterol. 2000;95:1036–1040. doi: 10.1111/j.1572-0241.2000.01978.x. [DOI] [PubMed] [Google Scholar]
- 61.Lamerz R., Runge M., Stieber P., Meissner E. Use of serum PIVKA-II (DCP) determination for differentiation between benign and malignant liver diseases. Anticancer Res. 1999;19:2489–2493. [PubMed] [Google Scholar]
- 62.Mita Y., Aoyagi Y., Yanagi M., Suda T., Suzuki Y., Asakura H. The usefulness of determining des-gamma-carboxy prothrombin by sensitive enzyme immunoassay in the early diagnosis of patients with hepatocellular carcinoma. Cancer. 1998;82:1643–1648. doi: 10.1002/(sici)1097-0142(19980501)82:9<1643::aid-cncr8>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 63.Aoyagi Y., Oguro M., Yanagi M., Mita Y., Suda T., Suzuki Y., Hata K., Ichii K., Asakura H. Clinical significance of simultaneous determinations of alpha-fetoprotein and des-gamma-carboxy prothrombin in monitoring recurrence in patients with hepatocellular carcinoma. Cancer. 1996;77:1781–1786. doi: 10.1002/(SICI)1097-0142(19960501)77:9<1781::AID-CNCR4>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 64.Izuno K., Fujiyama S., Yamasaki K., Sato M., Sato T. Early detection of hepatocellular carcinoma associated with cirrhosis by combined assay of des-gamma-carboxy prothrombin and alpha-fetoprotein: A prospective study. Hepato Gastroenterol. 1995;42:387–393. [PubMed] [Google Scholar]
- 65.Grazi G.L., Mazziotti A., Legnani C., Jovine E., Miniero R., Gallucci A., Palareti G., Gozzetti G. The role of tumor markers in the diagnosis of hepatocellular carcinoma, with special reference to the des-gamma-carboxy prothrombin. Liver Transplant. Surg. 1995;1:249–255. doi: 10.1002/lt.500010410. [DOI] [PubMed] [Google Scholar]
- 66.Okuda H., Nakanishi T., Takatsu K., Saito A., Hayashi N., Yamamoto M., Takasaki K., Nakano M. Comparison of clinicopathological features of patients with hepatocellular carcinoma seropositive for alpha-fetoprotein alone and those seropositive for des-gamma-carboxy prothrombin alone. J. Gastroenterol. Hepatol. 2001;16:1290–1296. doi: 10.1046/j.1440-1746.2001.02610.x. [DOI] [PubMed] [Google Scholar]
- 67.Hamamura K., Shiratori Y., Shiina S., Imamura M., Obi S., Sato S., Yoshida H., Omata M. Unique clinical characteristics of patients with hepatocellular carcinoma who present with high plasma des-gamma-carboxy prothrombin and low serum alpha-fetoprotein. Cancer. 2000;88:1557–1564. doi: 10.1002/(sici)1097-0142(20000401)88:7<1557::aid-cncr9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 68.Willyard C. Researchers look for “sweet” method to diagnose cancer. Nat. Med. 2007;13:1107–1267. doi: 10.1038/nm1107-1267. [DOI] [PubMed] [Google Scholar]
- 69.Zhou Y., Yin X., Ying J., Zhang B. Golgi protein 73 versus alpha-fetoprotein as a biomarker for hepatocellular carcinoma: A diagnostic meta-analysis. BMC Cancer. 2012;12 doi: 10.1186/1471-2407-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Littenberg B., Moses L.E. Estimating diagnostic accuracy from multiple conflicting reports: A new meta-analytic method. Med Decis Making. 1993;13:313–321. doi: 10.1177/0272989X9301300408. [DOI] [PubMed] [Google Scholar]