Abstract
Background
A recent review concluded that general health checks fail to reduce mortality in adults.
Aim
This review focuses on general practice-based health checks and their effects on both surrogate and final outcomes.
Design and setting
Systematic search of PubMed, Embase, and the Cochrane Central Register of Controlled Trials.
Method
Relevant data were extracted from randomised trials comparing the health outcomes of general practice-based health checks versus usual care in middle-aged populations.
Results
Six trials were included. The end-point differences between the intervention and control arms in total cholesterol (TC), systolic and diastolic blood pressure (SBP, DBP), and body mass index (BMI) were −0.13 mmol/l (95% confidence interval [CI] = −0.19 to −0.07), −3.65 mmHg (95% CI = −6.50 to −0.81), −1.79 mmHg (95% CI = −2.93 to −0.64), and −0.45 kg/m2 (95% CI = −0.66 to −0.24), respectively. The odds of a patient remaining at ‘high risk’ with elevated TC, SBP, DBP, BMI or continuing smoking were 0.63 (95% CI = 0.50 to 0.79), 0.59 (95% CI = 0.28 to 1.23), 0.63 (95% CI = 0.53 to 0.74), 0.89 (95% CI = 0.81 to 0.98), and 0.91 (95% CI = 0.82 to 1.02), respectively. There was little evidence of a difference in total mortality (OR 1.03, 95% CI = 0.90 to 1.18). Higher CVD mortality was observed in the intervention group (OR 1.30, 95% CI = 1.02 to 1.66).
Conclusion
General practice-based health checks are associated with statistically significant, albeit clinically small, improvements in surrogate outcome control, especially among high-risk patients. Most studies were not originally designed to assess mortality.
Keywords: general practice, health check, mortality, primary health care, risk factors, systematic review
INTRODUCTION
As medicine has adopted the principles of prevention,1 screening for preventable disease has become more common. A ‘health check’ can be defined as a comprehensive assessment to detect and manage risk factors and chronic disease, most of which are cardiovascular disease-related. It is biologically plausible that chronic disease could be prevented or at least delayed via early detection and management of biomedical and lifestyle risk factors, and there is some evidence that periodic health evaluations can improve the delivery of some recommended preventive services.2 General practice-based health checks refer to those conducted in general practice or its equivalent and managed by either practice staff or trained personnel.
A recently published systematic review by Krogsbøll and colleagues concluded that general health checks failed to improve total and disease-specific mortality; and there was no strong evidence suggesting these checks would reduce either morbidity or subsequent medical service use.3 Their systematic review found 16 eligible trials, nine of which were included in the meta-analysis. Year of publication ranged from the 1960s to the 2000s, and the included studies were conducted in different settings. To interpret the results, it is important to understand the differences between studies conducted in different eras. Generally, studies conducted in the 1960s focused solely on detection; few considered subsequent interventions and most used mortality, morbidity, and medical service use as primary outcomes. In the 1970s, studies started to consider how to manage detected risk factors. From the 1980s onwards, the focus shifted from screening to screening plus intervention. These changes would potentially enhance the effects of the health checks.
In Krogsbøll’s systematic review five trials were practice-based, 10 were conducted in the community, and one was workplace-based. However, none of the subgroup analyses differentiated the study setting. Nor did the review examine surrogate outcomes (for example, total cholesterol levels, blood pressure, body mass index and smoking status). The authors argued that surrogate outcomes have unreliable effects on morbidity and mortality and their use might conceal harmful effects of the health check. Furthermore, the sustainability of surrogate outcome changes was questionable.3
Although it is true that there are disadvantages with the use of surrogate outcomes as mentioned above, especially when they are used as sole measures in clinical trials,4 most identified surrogate outcomes used in health check studies are validated risk factors for chronic disease.5 Lifestyle and pharmaceutically managing such risk factors should reduce the risk of developing a chronic disease or its complications. Moreover, as health checks target common risk factors, such as blood pressure, serum lipids, and lifestyles, the risk of adverse outcomes from the check itself is fairly low. In addition, evidence suggests no short- or long-term adverse psychological effects on patients after their health check.6–8
How this fits in
The value of a general health check has been questioned following the publication of a systematic review by Krogsbøll et al. However, they did not differentiate between health checks conducted in general practice and those undertaken in other community settings or the workplace. The present authors consider that general practice, by offering comprehensive and ongoing care, could improve health check outcomes, particularly for established chronic disease risk factors. Using standard meta-analysis it was found that general practice-based health check studies report slightly better results for surrogate outcomes than do non-practice based studies. However, when meta-regression was used the differences were non-significant; this may be because there were only a small number of studies. No differences were found in total mortality, but all the general practice-based studies were not originally designed to assess this outcome.
The present authors consider that the cumulative death rate alone is not sufficient to fully capture the impact of a health check on patients. Morbidity and quality of life should also be assessed. So far, there is limited evidence for morbidity outcomes in health check studies because of the requirement for large sample sizes and longer follow-up periods. On the other hand, surrogate outcomes can easily be measured and compared. Therefore, they are widely used in routine medical practice and clinical research to predict a patient’s prognosis and as indicators of quality health care.9 Given the established associations between surrogate outcomes and morbidity, they should be considered to be good substitute indicators for morbidity.
New health check programmes have been proposed or initiated in the Netherlands, UK, and Australia in recent years. Even though all target the middle-aged, there exists considerable variation in recruitment strategies and the interval between checks. For instance, whereas the Dutch chose to target ‘high-risk’ patients, programmes in the UK and Australia are less selective. There is a 5-year interval between checks in the UK, whereas in Australia there is a one-off 45–49-year-old check. Clearly these programmes need to be evaluated and research undertaken to determine if such differences affect outcomes.
There is also evidence that the impact of a health check could be improved and be more sustainable if provided in conjunction with the patient’s routine health care.6,10 Healthcare providers, such as GPs, who have ongoing relationships with patients may be in a better position to deliver preventive health services, as they tend to have a strong influence on patient’s health perceptions and be better able to encourage compliance.11
Therefore, the present systematic review focuses on the health benefits (surrogate and final outcomes) of health checks conducted within general practice. Supplementary analyses were performed to compare the effects of study settings.
METHOD
Literature search
Systematic literature searches of PubMed, Embase, and the Cochrane Central Register of Controlled Trials were performed in March 2012 (updated in October 2012). Single citation search of relevant publications was performed using SCOPUS and Google Scholar. Only articles in English were included. No time period restriction was applied to the search.
Study selection
The pre-specified inclusion criteria were:
Types of study: randomised controlled trials (RCT), cluster RCTs, or pseudo-RCTs.
Participants: middle-aged populations with a mean age of 35–65 years.
Intervention: general health checks with/without subsequent intervention protocols; general practice was involved in the entire process.
Comparison: no health screening or usual care.
Outcomes: total mortality, cardiovascular disease (CVD) mortality, blood pressure, total cholesterol, body mass index (BMI), and smoking status.
The titles and abstracts of all records were reviewed. Full texts were retrieved for potentially relevant records. Further eliminations were made if the study objective was to investigate an intervention strategy rather than a health check or if the study did not report relevant outcomes. Important characteristics of relevant studies were summarised by one author and independently reviewed by two other authors.
Data abstraction
Relevant data were extracted using a self-developed form. For continuous outcomes, the mean and variance were collected. For categorical outcomes, either the number of events/total in both groups or the corresponding relative risks with confidence intervals (CIs) were extracted. From the cluster RCT, only data that had been adjusted for clustering effects were used in this meta-analysis. Published and unpublished data were collected from relevant systematic reviews.3,12
Data analysis
Study quality was assessed using the Cochrane risk of bias tool.13 Studies were assessed for the following potential biases: selection, performance, detection, attrition, reporting, and other potential bias. Each and every included study was marked with high, low, or unclear risk of all potential bias categories. Data synthesis was performed using the Review Manager 5 software. Continuous outcomes were analysed using the inverse variance approach. The mean difference between two groups with the 95% CI was calculated. Dichotomous outcomes were synthesised using the generic inverse variance model. Odds ratio (OR) with 95% CI were calculated. A random effects model was applied to all analyses.14 Statistical heterogeneity was tested using χ2 tests and quantified using I2 statistics.15 Substantial heterogeneity is defined when I2 >85%. Pre-specified subgroup analyses were applied to explain the potential heterogeneous results from meta-analyses. Different recruitment strategies and the length of follow-up period were chosen as potential subgroups, because they were considered as potential determinants of health check effects. Publication bias was evaluated using funnel plots.
Supplementary analysis
To compare the effects of study settings, non-practice-based studies were identified from the reference list of Krogsbøll’s systematic review. Relevant data were extracted from these studies to allow for the comparison of study settings: practice-based versus non-practice-based studies. Random effects meta-regression was applied to test if the health check effects were statistically different between the practice- and non-practice-based studies.
RESULTS
Study identification
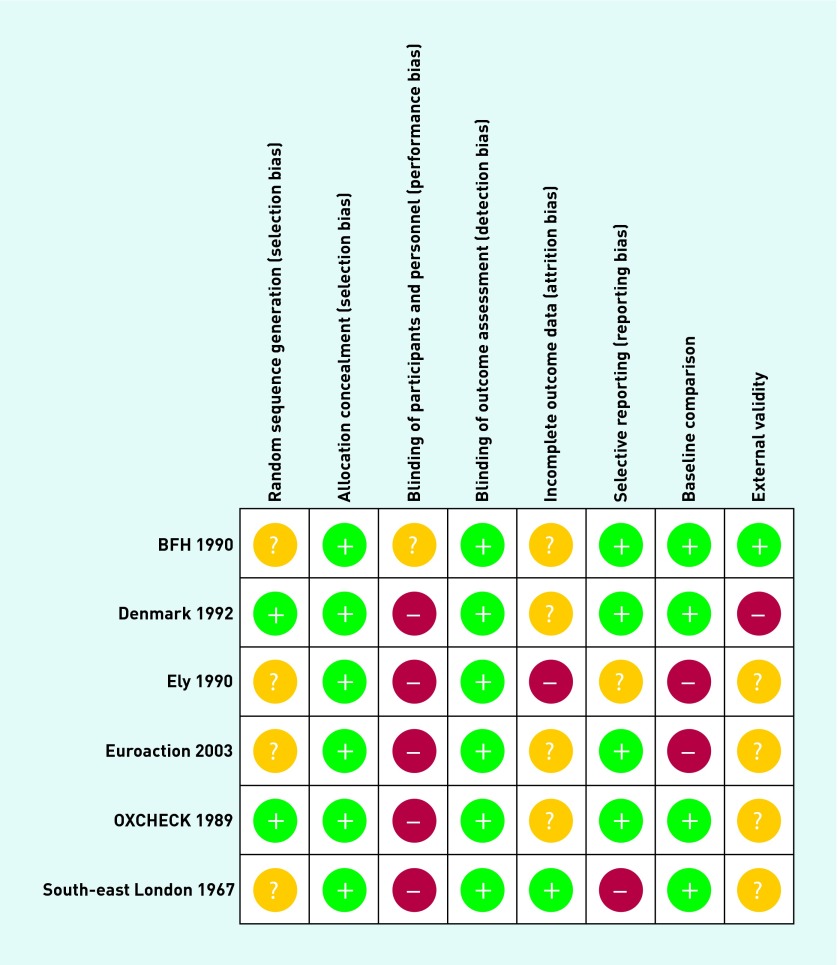
Six general practice-based trials were identified from the search (Figure 1), two of which were not included in Krogsbøll’s review.16,17 The latter two studies met the inclusion criteria. The Euroaction study was a cluster RCT investigating the effectiveness of primary prevention of CVD in general practice patients aged 50–80 years.16 The Ely study was primarily a diabetes risk screening study, but a multiple risk factor screening strategy was adopted.17
Figure 1.
Study flow diagram.
A supplementary search of the reference list of Krogsbøll’s review yielded 11 non-practice-based trials. Three of these studies reported at least one surrogate outcome.18–20 Six reported total and CVD mortality.19–24
Study characteristics
Five of the practice-based studies were RCTs.25–28 The other was a cluster RCT randomised at the general practice level.15 Health checks were performed either by practice staff or trained personnel. Four of the six trials targeted general populations.26–29 The other two recruited high-risk patients and their partners.16,30 Different interventions were implemented after the health check. The follow-up period ranged from 1 to 10 years.
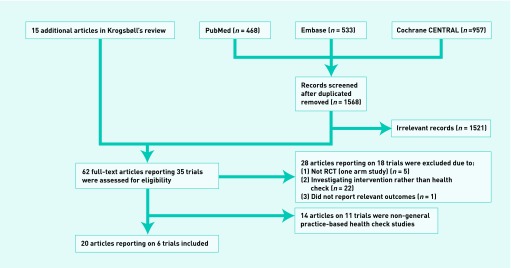
Quality assessment
The risk of bias varied between the included trials (Figure 2). Important issues were lack of blinding and loss to follow-up. Blinding of patients and practice staff was impossible; however, potential performance bias could affect the results in either direction. Loss to follow-up was the main limitation of studies assessing surrogate outcome differences. However, comparisons of patients who returned for the final check with those who did not return suggested no significant differences between most investigated outcomes at the initial assessment.31 Therefore, the direction and magnitude of any attrition bias remains uncertain. Finally, even though studies were conducted among patients who had agreed to participate, patients who refused to participate did not appear to be significantly different from those participants in terms of general health status and health awareness.32,33
Figure 2.
Summary of bias in included studies.
All four studies reporting mortality demonstrated a bias towards the null caused by early interventions to the control group prior to data collection (for example, health check to the control group prior to mortality data collection)17,26–28 or the merging of study groups (for example, in the OXCHECK study, the initial health check was conducted in 3 consecutive years in the intervention group).29
Effectiveness of intervention
Meta-analyses on total cholesterol (TC), systolic blood pressure (SBP), diastolic blood pressure (DBP), and BMI consistently favoured the health check group, with results as summarised in Table 1. The analyses for SBP and DBP were subject to substantial heterogeneity. However, within each outcome analysis, the results consistently favoured the intervention group. Subgroup analyses based on recruitment strategies reduced the magnitude of the heterogeneity of SBP and DBP differences, and the length of follow-up could explain the heterogeneity of TC differences. However, meta-regression was not applicable because of the small number of included studies.
Table 1.
Meta-analysis of surrogate outcomes
| Outcomes | Studies, n | Mean difference (95% CI) |
Heterogeneity
|
|
|---|---|---|---|---|
| P-value | I2, % | |||
| General practice-based studies | ||||
| TC17,26,29,31 | 4 | −0.13 (−0.19 to −0.07) | 0.08 | 52 |
| SBP17,26,29,31 | 4 | −3.65 (−6.50 to −0.81) | <0.001 | 94 |
| DBP17,26,29,31 | 4 | −1.79 (−2.93 to −0.64) | <0.001 | 88 |
| BMI17,26,29 | 3 | −0.45 (−0.66 to −0.24) | 0.79 | 0 |
|
| ||||
| Non-practice-based studies | ||||
| TC18–20 | 3 | −0.01 (−0.07 to 0.04) | 0.21 | 35 |
| SBP18–20 | 3 | −0.95 (−1.98 to 0.08) | 0.21 | 37 |
| DBP18–20 | 3 | −0.72 (−1.36 to −0.08) | 0.16 | 46 |
| BMI18 | 1 | −0.10 (−0.69 to 0.49) | N/A | |
BMI = body mass index. DBP = diastolic blood pressure. SBP = systolic blood pressure. TC = total cholesterol.
In addition to the absolute changes, ORs were used to compare the odds of patients at high risk in both groups at the end of the study period. The thresholds of high risk are listed in Table 2. Meta-analyses suggested that practice-based health checks significantly reduced the odds of patients remaining at high risk (high levels of TC, DBP, and BMI) compared with usual care (Table 3). The analysis of high SBP was heterogeneous because only two studies were included. No significant difference was found for smoking status between the intervention and control groups.
Table 2.
Risk categories
| Studies | SBP, mmHg | DBP, mmHg | TC, mmol/l | BMI, kg/m2 |
|---|---|---|---|---|
| OXCHECK, 1989 199229 | N/A | 100 | 8 | 30 |
| BFH, 1990 199131 | N/A | 100 | 8 | 30 |
| Denmark, 1992 199726 | 140 | 90 | 6 | 27.5 |
| Euroaction, 2003 200616 | 140 | 100 | 6 | 30 |
BMI = body mass index. DBP = diastolic blood pressure. SBP = systolic blood pressure. TC = total cholesterol.
Table 3.
Meta-analysis of the odds of patients remaining at high risk
| Outcomes | Studies, n | OR (95% CI) |
Heterogeneity
|
|
|---|---|---|---|---|
| P-value | I2, % | |||
| General practice-based studies | ||||
| TC17,26,29,31 | 4 | 0.63 (0.50 to 0.79) | 0.09 | 50 |
| SBP16,26 | 2 | 0.59 (0.28 to 1.23) | 0.01 | 84 |
| DBP16,26,29,31 | 4 | 0.63 (0.53 to 0.74) | 0.25 | 26 |
| BMI16,26,29,31 | 4 | 0.89 (0.81 to 0.98) | 0.59 | 0 |
| Smoking16,26,27,29,31 | 5 | 0.91 (0.82 to 1.02) | 0.04 | 58 |
| Total mortality26–29 | 4 | 1.03 (0.90 to 1.18) | 0.36 | 7 |
| CVD mortality27–29 | 3 | 1.30 (1.02 to 1.66) | 0.34 | 7 |
|
| ||||
| Non-practice-based studies | ||||
| Smoking18–20 | 3 | 0.94 (0.87 to 1.03) | 0.34 | 7 |
| Total mortality19–24 | 6 | 1.00 (0.93 to 1.08) | 0.05 | 54 |
| CVD mortality19–24 | 6 | 1.02 (0.92 to 1.13) | 0.11 | 44 |
BMI = body mass index. CVD = cardiovascular disease. DBP = diastolic blood pressure. SBP = systolic blood pressure. TC = total cholesterol.
Meta-analyses on total mortality suggested no differences between intervention and control groups. However, the CVD death rate was significantly higher in the intervention group (Table 3). This result contradicted the previous analysis of surrogate outcome changes. However, the forest plot suggests that this result was dominated by the inclusion of the SouthEast London study27 (OR 1.54, 95% CI = 1.09 to 2.16). This study, conducted in the 1960s, did not report on surrogate outcome changes.
Funnel plots of all invested outcomes suggested no publication bias.
Full details of the search strategies, the characteristics of included studies, and their quality assessments, together with forest plots of the sub-group analyses and the funnel plots, are available from the authors on request.
Comparison with non-practice-based studies
Meta-analyses were performed using data from the non-practice-based studies. Except for the differences in mean DBP, no statistically significant differences were found in the analyses (Tables 1 and 3). Meta-regressions were used to test the statistical differences of health check outcomes between the practice- and non-practice-based studies. Besides a borderline significant difference in mean TC changes (P = 0.06) favouring the practice-based studies, no other differences were found between the two sub-groups with regards to the changes in mean SBP (P = 0.21), mean DBP (P = 0.28), mean BMI (P = 0.39), smoking rates (P = 0.94), total mortality (P = 0.71), and CVD death rates (P = 0.09) between the intervention and control groups (Table 4).
Table 4.
Meta-regression with practice and non-practice-based studies
| Outcome |
Studies, n
|
P-value | Coefficient (95% CI) | |
|---|---|---|---|---|
| Practice-baseda | Non-practice-based | |||
| TC | 417,26,29,31 | 318–20 | 0.056 | 0.108 (−0.004 to 0.220) |
| SBP | 417,26,29,31 | 318–20 | 0.213 | 2.719 (−2.052 to 7.490) |
| DBP | 417,26,29,31 | 318–20 | 0.282 | 0.968 (−1.035 to 2.971) |
| BMI | 317,26,29 | 118 | 0.386 | 0.350 (−1.019 to 1.719) |
|
| ||||
| OR (95% CI) | ||||
| Smoking | 516,26,27,29,31 | 318–20 | 0.941 | 1.006 (0.830 to 1.221) |
| Total mortality | 426–29 | 619–24 | 0.712 | 0.967 (0.790 to 1.184) |
| CVD mortality | 327–29 | 619–24 | 0.087 | 0.738 (0.513 to 1.062) |
BMI = body mass index. CVD = cardiovascular disease. DBP = diastolic blood pressure. SBP = systolic blood pressure. TC = total cholesterol.
Base case.
DISCUSSION
Summary
The meta-analyses demonstrate that practice-based health checks are associated with statistically significant improvements in surrogate outcomes and significantly reduced the proportion of patients remaining at high risk. However, the only study (Ely study) with long term follow-up (10 years) did not report any significant differences in surrogate outcomes. Since this study had several limitations, further long-term data are required.17 As to the final outcomes, the comparisons yield an equivalent total mortality and a higher CVD mortality rate in the health check group compared to usual care.
For the supplementary analysis, none of the meta-regressions on surrogate or final outcomes (that is, TC, SBP, DBP, BMI smoking status and mortality) showed significant differences between the practice and non-practice based studies. It is possible that the regressions did not have sufficient statistical power because only a limited number of studies were included in the analyses (Table 4).
Strengths and limitations
A problem with the design of RCTs for practice-based health checks is the impracticality of blinding both participants and health personnel, which inevitably raises the possibility of performance and detection bias (especially for self-reported outcomes). Second, there are methodological difficulties in the investigation of surrogate outcomes.4 The interpretation of outcome changes should be made with caution considering the loss to follow-up. Third, heterogeneity could have increased the difficulties with data interpretation. However, the direction of study outcomes consistently favoured the health check. In addition, much of the heterogeneity could be explained by the subgroup analyses of recruitment strategy and length of follow-up. Finally, as only small numbers of studies were included, the meta-regression may not have had sufficient statistical power.
It has also been argued that the degree of blood pressure change is compatible with acclimatisation to measurement.31,38 However, as all health checks were conducted at the patient’s regular general practice where they received most of their healthcare services, the acclimatisation to measurement’ effect should be minimised. Finally, most included trials were conducted around the early 1990s, when the population prevalence of risk factors, the thresholds for treatment used in clinical guidelines and the availability of effective pharmacotherapy were different from those available now.
Comparison with existing literature
The improvements in surrogate outcomes for the GP studies may reflect the comprehensive and continuous health care available in this setting. Arguably general practice is an ideal setting to bridge the gap between detection and management allowing intervention strategies to be implemented by physicians or practice nurses, to target biomedical risk factors.34–37
Consistent with relevant systematic reviews, 3, 12 no differences in total mortality are found in the review. However, mortality was not the primary outcome for the majority of the practice-based studies. All studies were subject to a bias towards the null because of contamination of the control group and the merging of study groups.16, 26, 29, 31 In addition, the statistical power of the practice-based studies investigating mortality, especially disease-specific mortality, is questionable considering the generally short follow-up period and the healthy baseline status of the participants. Other reasons for this finding may include: 1) The possibility that the effects on surrogate outcomes might not be sustainable, especially when several studies attributed surrogate outcome changes to lifestyle modification; and 2) the statistically significant changes in surrogate outcomes may not be clinically relevant in altering mortality outcomes for individuals. Evidence about changes in mortality among high risk patients is required. However, neither the British Family Heart nor the Euroaction study included mortality as study outcomes.16, 31
In contrast to the previous review, a significant increase in CVD mortality was found in the health check group. Given that the analysis suggested no significant differences in total mortality, potential bias in the coding of cause of death could not be excluded. In the health check group, mortality may have been more likely coded as CVD-related, because of the increased diagnosis of CVD and relevant risk factors. Furthermore, the definitions of CVD death in the three included studies were different. While the South-east London study used the 1957 version of the ICD to identify CVD mortality, the OXCHECK study only reported ‘coronary heart disease’ death and the Ely study used the term ‘cardiovascular causes mortality’. Therefore caution should be applied to the interpretation of these results.
Implications for research and practice
Overall, the findings of this study not only demonstrate the positive effects of practice-based health checks on surrogate risk factor control, but also differentiate them from studies performed in other settings. Although the direction of effects was consistent across studies and outcomes, the underlying magnitude of the changes remains uncertain given the limited number of existing studies, the divergent study designs, and differences in the conduct of the health checks.
Therefore, more evidence is required before it is possible to determine the degree of effectiveness of health checks in general practice and the Ely study17 used the term ‘cardiovascular causes mortality’. Therefore, caution should be applied to the interpretation of these results.
Acknowledgments
We thank the members of the School thesis writing group for their valuable comments.
Funding
Si Si was sponsored by the China Scholarship Council. This funder had no role in study design or data collection, analysis, or interpretation.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: www.bjgp.org/letters
REFERENCES
- 1.Department of Health . Healthy lives, Healthy People: Our strategy for public health in England. London: England; 2010. [Google Scholar]
- 2.Boulware L, Marinopoulos S, Phillips K, et al. Systematic review: the value of the periodic health evaluation. Ann Intern Med. 2007;146(4):289. doi: 10.7326/0003-4819-146-4-200702200-00008. [DOI] [PubMed] [Google Scholar]
- 3.Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ. 2012;345:7191. doi: 10.1136/bmj.e7191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fleming TR, DeMets DL. Surrogate end points in clinical trials: are we being misled? Ann Intern Med. 1996;125:605–613. doi: 10.7326/0003-4819-125-7-199610010-00011. [DOI] [PubMed] [Google Scholar]
- 5.Psaty BM, Weiss NS, Furberg CD, et al. Surrogate end points, health outcomes, and the drug-approval process for the treatment of risk factors for cardiovascular disease. JAMA. 1999;282(8):786–790. doi: 10.1001/jama.282.8.786. [DOI] [PubMed] [Google Scholar]
- 6.Meland E, Laerum E, Maeland JG. Life style intervention in general practice: effects on psychological well-being and patient satisfaction. Qual Life Res. 1996;5(3):348–354. doi: 10.1007/BF00433919. [DOI] [PubMed] [Google Scholar]
- 7.Christensen B. Psychological reactions to information about risk of ischaemic heart disease in general practice. Scand J of Prim Health. 1995;13(3):164–167. doi: 10.3109/02813439508996756. [DOI] [PubMed] [Google Scholar]
- 8.Christensen B, Engberg M, Lauritzen T. No long-term psychological reaction to information about increased risk of coronary heart disease in general practice. Eur J Cardiovasc Prev Rehabil. 2004;11(3):239–243. doi: 10.1097/01.hjr.0000129739.30593.23. [DOI] [PubMed] [Google Scholar]
- 9.NHS Health Check Programme . Putting Prevention First – NHS Health Check: vascular risk assessment and management best practice guidance. London: Department of Health; 2009. [Google Scholar]
- 10.Royal College of General Practitioners . Prevention of Arterial Disease in General Practice. London: RCGP; 1981. [Google Scholar]
- 11.Devroey D, Coigniez P, Vandevoorde J, et al. Prevention and follow-up of cardiovascular disease among patients without a personal GP. Fam Pract. 2003;20(4):420–424. doi: 10.1093/fampra/cmg415. Epub 2003/07/24. [DOI] [PubMed] [Google Scholar]
- 12.Ebrahim S, Beswick A, Burke M, et al. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev. 2006;4:CD001561. doi: 10.1002/14651858.CD001561.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. http://handbook.cochrane.org/ (accessed 9 Dec 2013).
- 14.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 15.Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 16.Wood D, Kotseva K, Connolly S, et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet. 2008;371(9629):1999–2012. doi: 10.1016/S0140-6736(08)60868-5. [DOI] [PubMed] [Google Scholar]
- 17.Rahman M, Simmons R, Hennings S, et al. Effect of screening for Type 2 diabetes on population-level self-rated health outcomes and measures of cardiovascular risk: 13-year follow-up of the Ely cohort. Diabetic Med. 2012;29(7):886–892. doi: 10.1111/j.1464-5491.2012.03570.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murray DM, Luepker RV, Pirie PL, et al. Systematic risk factor screening and education: a community-wide approach to prevention of coronary heart disease. Prev Med. 1986;15(6):661–672. doi: 10.1016/0091-7435(86)90071-x. [DOI] [PubMed] [Google Scholar]
- 19.Wilhelmsen L, Ljungberg S, Wedel H, Werko L. A comparison between participants and non-participants in a primary preventive trial. J Chron Dis. 1976;29(5):331–339. doi: 10.1016/0021-9681(76)90093-x. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization European Collaborative Group Multifactorial trial in the prevention of coronary heart disease: 2. Risk factor changes at two and four years. Eur Heart J. 1982;3:184–190. [PubMed] [Google Scholar]
- 21.Lannerstad O, Sternby NH, Isacsson SO, et al. Effects of a health screening on mortality and causes of death in middle-aged men. A prospective study from 1970 to 1974 of mean in Malmo, born 1914. Scand J Soc Med. 1977;5(3):137–140. doi: 10.1177/140349487700500305. [DOI] [PubMed] [Google Scholar]
- 22.Dales L, Friedman G, Ramcharan S, et al. Multiphasic checkup evaluation study. 3. Outpatient clinic utilization, hospitalization, and mortality experience after seven years. Prev Med. 1973;2(2):221. doi: 10.1016/0091-7435(73)90066-2. [DOI] [PubMed] [Google Scholar]
- 23.Tibblin G, Welin L, Larsson B, et al. The influence of repeated health examinations on mortality in a prospective cohort study, with a comment on the autopsy frequence: the study of men born in 1913. Scand J Public Health. 1982;10(1):27. doi: 10.1177/140349488201000106. [DOI] [PubMed] [Google Scholar]
- 24.Theobald H, Bygren LO, Carstensen J, et al. Effects of an assessment of needs for medical and social services on long-term mortality: a randomised controlled study. Int J Epidemiol. 1998;27(2):194–198. doi: 10.1093/ije/27.2.194. [DOI] [PubMed] [Google Scholar]
- 25.OXCHECK Study Group Prevalence of risk factors for heart disease in OXCHECK trial: implications for screening in primary care. BMJ. 1991;302(6784):1057–1060. doi: 10.1136/bmj.302.6784.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Engberg M, Christensen B, Karlsmose B, et al. General health screenings to improve cardiovascular risk profiles: a randomised controlled trial in general practice with 5-year follow-up. J Fam Pract. 2002;51(6):546–552. [PubMed] [Google Scholar]
- 27.Holland W, Creese A, D’Souza M, et al. A controlled trial of multiphasic screening in middle-age: results of the South-East London Screening Study. Int J Epidemiol. 1977;6(4):357–363. doi: 10.1093/ije/6.4.357. [DOI] [PubMed] [Google Scholar]
- 28.Simmons R, Rahman M, Jakes R, et al. Effect of population screening for type 2 diabetes on mortality: long-term follow-up of the Ely cohort. Diabetologia. 2011;54(2):312–319. doi: 10.1007/s00125-010-1949-8. [DOI] [PubMed] [Google Scholar]
- 29.OXCHECK Study Group Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. BMJ. 1995;310(6987):1099–1104. [PMC free article] [PubMed] [Google Scholar]
- 30.Wood D, Kinmonth A, Davies G, et al. British family heart study: Its design and method, and prevalence of cardiovascular risk factors. Br J Gen Pract. 1994;44(379):62–67. [PMC free article] [PubMed] [Google Scholar]
- 31.Wood D, Kinmonth A, Davies G, et al. Randomised controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of British family heart study. BMJ. 1994;308(6924):313. [PMC free article] [PubMed] [Google Scholar]
- 32.Nielsen KDB, Dyhr L, Lauritzen T, Malterud K. ‘You can’t prevent everything anyway’: A qualitative study of beliefs and attitudes about refusing health screening in general practice. Fam Pract. 2004;21(1):28–32. doi: 10.1093/fampra/cmh107. [DOI] [PubMed] [Google Scholar]
- 33.Davies G, Pyke S, Kinmonth AL. Effect of non-attenders on the potential of a primary care programme to reduce cardiovascular risk in the population. Family Heart Study Group. BMJ. 1994;309(6968):1553–1556. doi: 10.1136/bmj.309.6968.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stewart S, Carrington MJ, Swemmer CH, et al. Effect of intensive structured care on individual blood pressure targets in primary care: multicentre randomised controlled trial. BMJ. 2012;345 doi: 10.1136/bmj.e7156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benner J, Erhardt L, Flammer M, et al. A novel programme to evaluate and communicate 10 year risk of CHD reduces predicted risk and improves patients’ modifiable risk factor profile. Int J Clin Pract. 2008;62(10):1484–1498. doi: 10.1111/j.1742-1241.2008.01872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brett T, Arnold-Reed D, Phan C, et al. The fremantle primary prevention study: a multicentre randomised trial of absolute cardiovascular risk reduction. BrJ Gen Pract. 2012;62(594):e22–e28. doi: 10.3399/bjgp12X616337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tiessen AH, Smit AJ, Broer J, et al. Randomised controlled trial on cardiovascular risk management by practice nurses supported by self-monitoring in primary care. BMC Fam Pract. 2012;13(1):90. doi: 10.1186/1471-2296-13-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.OXCHECK Study Group Effectiveness of health checks conducted by nurses in primary care: results of the OXCHECK study after one year. BMJ. 1994;308(6924):308–312. [PMC free article] [PubMed] [Google Scholar]