Abstract
Background
The objective of this research is an artificial pancreas (AP) that performs automatic regulation of blood glucose levels in people with type 1 diabetes mellitus. This article describes a control strategy that performs algorithmic insulin dosing for maintaining safe blood glucose levels over prolonged, overnight periods of time and furthermore was designed with outpatient, multiday deployment in mind. Of particular concern is the prevention of nocturnal hypoglycemia, because during sleep, subjects cannot monitor themselves and may not respond to alarms. An AP intended for prolonged and unsupervised outpatient deployment must strategically reduce the risk of hypoglycemia during times of sleep, without requiring user interaction.
Methods
A diurnal insulin delivery strategy based on predictive control methods is proposed. The so-called “periodic-zone model predictive control” (PZMPC) strategy employs periodically time-dependent blood glucose output target zones and furthermore enforces periodically time-dependent insulin input constraints to modulate its behavior based on the time of day.
Results
The proposed strategy was evaluated through an extensive simulation-based study and a preliminary clinical trial. Results indicate that the proposed method delivers insulin more conservatively during nighttime than during daytime while maintaining safe blood glucose levels at all times. In clinical trials, the proposed strategy delivered 77% of the amount of insulin delivered by a time-invariant control strategy; specifically, it delivered on average 1.23 U below, compared with 0.31 U above, the nominal basal rate overnight while maintaining comparable, and safe, blood glucose values.
Conclusions
The proposed PZMPC algorithm strategically prevents nocturnal hypoglycemia and is considered a significant step toward deploying APs into outpatient environments for extended periods of time in full closed-loop operation.
Keywords: artificial pancreas, automated insulin delivery, automatic control, model predictive control, outpatient care, periodic control
Introduction
The overall goal of this work is an artificial pancreas (AP) for the automated delivery of insulin to people with type 1 diabetes mellitus (T1DM).1–4 A crucial element of any fully automated AP is a feedback control law that performs algorithmic insulin dosing that is effective and safe. A variety of such glycemia controllers have been proposed, e.g., based on model predictive control (MPC),5–10 proportional-integral-derivative control,11,12 fuzzy logic,13 and adaptive neural networks.14 The authors’ group has been focusing increasingly on developing MPC strategies.15 One advantage of MPC is the large degree of flexibility in formulating the control objective, and this flexibility was exploited in the authors’ development of glycemia controllers based on zone-MPC,7,16,17 whereby the blood glucose levels are controlled with respect to the inclusion within a safety set rather than to track a singular set point. The zone-MPC strategy of Grosman and coauthors7 and van Heusden and coauthors17 has successfully been employed in multiple clinical trials as well as undergone extensive in silico testing. The reason it has proven effective in real-life operation of the AP is twofold. First, there is generally a significant plant–model mismatch due to the large intersubject and intrasubject variability of human physiology. Second is that the feedback signals, an estimate of the blood glucose level provided every 5 min by a continuous glucose monitor (CGM),18 suffers large errors and delays, both of which have time-varying properties and have proven difficult to model and correct for. The use of zone-MPC provides robustness against excessively responding to plant–model mismatches and noise in the state estimate when the blood glucose level is estimated to be within the safe zone. The work presented in this article is an extension of the zone-MPC strategy presented previously.7,17
Rigorous testing of an AP requires, first, operating the controller for prolonged, all-day and multiday periods of time and, second, moving trials from the clinic to an outpatient environment. A major concern is nocturnal hypoglycemic events. The motivation for this article is to address this issue. While the user is awake, it is desirable to keep blood glucose levels toward the lower end of the safe range, at the risk of a higher probability of experiencing a hypoglycemic event. As the AP user may be more involved with her/his glucose control she/he either will become aware of her/his state or will be made aware of it by a threshold-based, or predictive, hypoglycemia alarm system19–21 and correct appropriately. However, this cannot be relied upon at night, and thus the controller must be designed to decrease the likelihood of hypoglycemia from the level of risk permitted during the day and not rely on alarms, glucose supplements, or subject intervention. The primary contribution of this article is the development of a zone-MPC law that strategically reduces the risk of hypoglycemia during the night—assumed to be the time of sleep. The novelty over the time-invariant zone-MPC strategy of Grosman and coauthors7 and van Heusden and coauthors17 is that the proposal is periodically time dependent with respect to the time of day. Specifically, during the night, the blood glucose target zone is raised and the bound on the maximum insulin infusion rate is reduced from the values employed during the day. The motivation for the former is to induce a rise of blood glucose levels at night. The latter is enforced as a further safety mechanism and reduces the chance of controller-induced hypoglycemia. The proposed strategy is referred to in this article as periodic-zone model predictive control (PZMPC).
The concept of dynamically modulating the control objective, and the accompanying constraints against which it must be achieved, is not limited to defending against nocturnal hypoglycemia but is envisaged to be useful in more general contexts too. The focus of this article is nocturnal hypoglycemia, because this particular scenario was subject to a clinical trial (see In-Clinic Evaluation). The strategy described in this article is time dependent based on the time of day, where it was assumed that people sleep during the night. The assumption was “correct” in the trials performed, because sleep was stipulated to occur at night by means of the clinical test protocol. In a true outpatient environment, subject behavior cannot be prescribed, and therefore the zone-MPC strategy may have to modulate its target zones and input constraints based on, e.g., user input or physiologic feedback signals provided by sleep sensors and motion detectors. Furthermore, accommodating time-dependent control objectives in an AP may permit longer-term adjustments of blood glucose levels tailored to subjects’ habits, physiological cycles, exercise routines, or work schedules, e.g., because a subject’s employment requires the use of a vehicle on certain days, for which she prefers a minimum blood glucose value higher than she would typically choose when not driving. Thus the work presented in this article may be a first step toward flexible, adaptive control laws that facilitate the semipermanent deployment of an AP in true outpatient environments, individualized to subjects and their lifestyles.
Methods: Periodic-Zone Model Predictive Control
Insulin–Glucose Model
The insulin–glucose model of van Heusden and coauthors17 is employed in this study and is summarized as follows. The model is a discrete-time linear time-invariant (LTI) system with sample period TS min. The time-step index is denoted by i. The scalar plant input is the administered insulin bolus uIN,i ( U/ TS), and the scalar plant output is the subject’s blood glucose value yBG,i (mg/dl). The plant is linearized around a steady state that is assumed to be achieved by applying the subject-specific and time-dependent basal input rate uBASAL,i (U/h) and is assumed to result in a steady state blood glucose output ySS = 110 mg/dl. Let the scalar input ui and output yi of the LTI model be defined as
We denote by z–1 the backward shift operator, by Y(z–1) and U(z–1) the z-transform of the time-domain signals of input ui and output yi, respectively. The transfer characteristics from u to y are described by
with poles p1 = 0.98 and p2 = 0.965, a so-called safety factor F = 1.5 (unitless; can be tuned to the subject but is fixed to 1.5 throughout this article), the subject-specific total daily insulin amount uTDI (U; positive scalar), and where the scalar constant
is employed to set the correct gain and for unit conversion. The constant 1800 stems from the “1800 rule” for estimating blood glucose decrease with respect to the delivery of rapid-acting insulin.
The state-space representation of this single-input, single-output LTI system is given by
with three-dimensional state x, input u, and output y, and with
Periodic Daily Blood Glucose Target Zone
The main novelty and contribution of the proposed PZMPC strategy over previous strategies,7,17 with respect to glycemia control, is the use of periodically time-dependent output target zones. It is desired that output y satisfy
| (1) |
where y̱ and yˉ denote time-dependent lower and upper bounds of the output target zone, respectively. The output objective of Equation (1) is a soft constraint throughout this article, i.e., the bounds may be violated.
During the day, the zones are selected equal to those employed previously:7,17 y̱ = 80 mg/dl, yˉ = 140 mg/dl. This choice provides a good combination of the controller striving to maintain a blood glucose level that is healthy semipermanently, while not excessively responding to disturbances and sensor errors with a non-basal insulin delivery.
During the night, the following bounds are selected: y̱ = 110 mg/dl, yˉ = 220 mg/dl (see Parameter Choices). Thus the blood glucose target zone is both elevated and widened during the night compared with the day. The elevated lower bound implies that the controller reduces the insulin input rate to below the basal rate at higher blood glucose values during the night than during the day. The highly elevated upper bound implies that the controller administers an insulin input rate exceeding the basal rate only at blood glucose levels that are high enough to pose a serious and near-term health risk. It furthermore implies that during the night, the controller makes no attempt to lower any blood glucose level less than 220 mg/dl, even though a level of 220 mg/dl would pose a considerable health risk if maintained indefinitely. This trade-off appears, at present, to be necessary in order to reduce the likelihood of immediately life-threatening nocturnal hypoglycemic events.
The daytime zone is employed from 7:00 am to 10:00 pm, the nighttime zone is from 12:00 pm to 5:00 am, and there are two 2 h periods in between where the controller smoothly transitions the target zone bounds based on a cosine function. The target zone bounds are plotted over the course of one day in Figure 1. A formal definition of the transition function is omitted for brevity.
Figure 1.
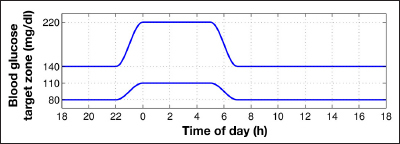
Daily periodic blood glucose (yBG) target zone boundaries (milligrams per deciliter). Daytime, 7:00 AM–10:00 PM; nighttime, 12:00 PM–5:00 AM; daytime zone, 80–140 mg/dl; nighttime zone, 110–220 mg/dl; smooth transition of 2 h duration (5:00 AM–7:00 AM, 10:00 PM–12:00 PM) based on the cosine function.
Periodic Daily Insulin Input Constraints
As a further safeguard against insulin overdosing during sleep, the proposed PZMPC strategy enforces daily periodically time-dependent insulin input constraints. The control input ui is required to satisfy
| (2) |
where u̱ and uˉ denote time-dependent lower and upper bounds, respectively. Throughout this article, Equation (2) is considered a hard constraint, i.e., it is rigorously enforced.
During daytime, the input is bounded from above only by the pump’s maximum achievable flow rate and is thus hardware dependent. Note that a typical pump’s maximum input rate is high enough to facilitate delivering very large boluses over short time intervals, and thus this maximum input rate is unlikely to ever be commanded by the controller. During nighttime, the input is limited from above to 1.5 uBASAL,i, i.e., 50% in excess of the subject’s time-dependent basal rate (see Parameter Choices). The insulin input rate’s lower bound is zero at all times.
Daytime is defined to be the interval 5:00 am to 10:00 pm. All other times are nighttime—there is no transition period. The start of daytime and nighttime coincides with the start of the output target zones’ transition periods. The insulin bounds are plotted over the course of one day in Figure 2.
Figure 2.
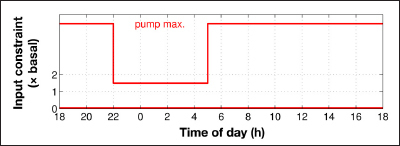
Daily periodic constraints on the insulin input uIN. Daytime, 5:00 AM–10:00 PM; nighttime, 10:00 PM–5:00 AM; daytime upper-bound is pump maximum, hardware dependent; nighttime upper bound is 1.5 uBASAL,i, subject specific; lower bound is 0 U at all times.
Periodic-Zone Model Predictive Control Problem
For all time steps i, let the zone excursion be denoted by
with zone-excursion function Z(·) defined as follows:
We denote by positive integer P the so-called prediction horizon; by positive integer M, M ≤ P, the so-called control horizon; and further denote a positive, scalar weighting factor for the input u by R. The parameters P, M, and R are design parameters and assumed to be given (see Parameter Choices).
The PZMPC strategy performs closed-loop control action of the plant by applying at each time step i the first control input u0* of the predicted optimal control input trajectory given by the solution of the PZMPC problem. The reader interested in the background and details of MPC is referred elsewhere.15
The PZMPC problem is as follows: Determine
subject to
| (3) |
| (4) |
| (5) |
where Njl denotes the set of consecutive integers {j, ···, l}, and ∀k ∈ Njl means the condition must hold for all values of k in the set Njl.
With sample-period TS = 5 min, the periodic bounds are defined by sequences , and of period length p = 24h/TS = 288. These sequences are known entirely at each time step i, and thus the output target zone boundaries and input constraints employed in Equations (4) and (5) are time-dependent with respect to the prediction time step k. This permits the PZMPC strategy to act upon future changes in output target zone that occur within the prediction horizon length PTS min.
State Estimator
A state estimate is required for initialization of the predicted state trajectory in Equation (3). A linear state estimator (sometimes referred to as a Luenberger observer) is employed (see, e.g., The Control Handbook22). The state estimator is based on the same plant model of Insulin–Glucose Model employed for prediction in the PZMPC problem and is implemented as
where the scalar y~i denotes the measured blood glucose level as per CGM, the superscript T denotes the transpose of a matrix, and positive definite weighting matrix Q is a design parameter and assumed to be given (see Parameter Choices).
The estimator state and model state are denoted by the same variable x because the model state can only be estimated. In contrast, the variable x employed in the PZMPC problem denotes predicted states.
Parameter Choices
The PZMPC problem is implemented employing control horizon M = 5, prediction horizon P = 9, and input weighting matrix R = 15. The linear state estimator described in State Estmator is implemented using Q = 1000 I3 where I3 denotes the identity matrix of dimension 3 × 3. These choices give good performance over the spectrum of in silico subjects of the University of Padova/Virginia Food and Drug Administration-accepted metabolic simulator.23 In this study, version 2 of the simulator is employed.
The choices of zone boundaries y̲, and y̅ and the upper bound u̅ on the insulin input during the night were chosen based on clinical and regulatory considerations. The values stated in the previous sections are the nominal values employed in the clinical trials described in In-Clinic Evaluation. Note that the parameter values are flexible and subject to adjustment depending on the results of clinical trials. Recall, however, that the upper bound in insulin delivery during the night as described in Periodic Daily Input Constraints is as a multiplier of the subjects’ basal rate and thus subject specific.
Results
In Silico Experiment
The proposed PZMPC strategy was tested using version 2 of the University of Padova/Virginia Food and Drug Administration-accepted metabolic simulator23 with 100 in silico adult subjects. The PZMPC strategy was compared with two alternative control strategies. The first alternative was the zone-MPC strategy described previously,7,17 employing the same blood glucose target zone (equal to the PZMPC daytime zone) at all times of day. This strategy is referred to here as invariant-zone-MPC. The second alternative employs the invariant-zone-MPC strategy only during the day (5:00 am–10:00 pm) and delivers the subject-specific basal insulin input rate during the night (10:00 pm–5:00 am). This strategy is referred to as the nighttime-basal strategy. The nighttime-basal strategy is included in the in silico tests for pedagogic purposes, to elucidate differences, and can be considered a realistic worst case of subjects’ regular control. While human subjects may frequently awake to take corrective action, no such intervention is included in the in silico trials, because the target audience of the proposed PZMPC strategy are subjects suffering hypoglycemia unawareness and subjects who are unable to take preventative action.
Note that the purpose of the experiment is to demonstrate increased safety margins during the night when using the proposed PZMPC algorithm. The purpose of the experiment is neither to demonstrate superiority of PZMPC over the other two control strategies in a general setting nor to participate in the debate on what, overall, is the best control strategy to employ for use in an AP. Nevertheless, for the in silico tests, some all-day results are provided to allow a comparison. All-day results could not be provided for the clinical trial results presented in In-Clinic Evaluation because they were not available.
Simulation Scenario
The simulations start at 1:00 pm and end at 6:00 pm the following day (simulated time). The controllers operate in closed loop from 4:00 pm on the first day until the end of the simulation. An unannounced 50 g carbohydrate (gCHO) dinner, 40 gCHO breakfast, and 15 gCHO snack is provided at 6:00 pm, 7:00 am (next day), and 2:00 pm (next day), respectively. Results prior to 6:00 Pm on the first day are ignored to reduce the effects of initial conditions. Simulations were performed employing the raw control law without the auxiliary systems present in the University of California, Santa Barbara/Sansum Diabetes Research Institute Artificial Pancreas System (APS),24 e.g., the Health Monitoring System20 that monitors for hypoglycemia and provides alarms if necessary. Note that the clinical trials described in In-Clinic Evaluation employed the full APS, and hypoglycemia alerts were followed by a 16 gCHO treatment.
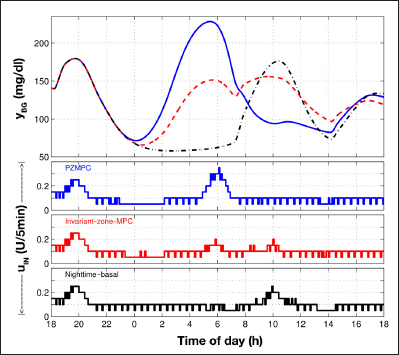
The Typical Case
The simulation result for an in silico subject that displays very typical behavior is depicted in Figure 3. The main response difference, as desired and expected, is an elevated blood glucose level during the night when using PZMPC. This is achieved by imposing a prolonged reduction in insulin input rate during the transition from daytime zone to nighttime zone starting at about 10:00 pm. The prolonged pump suspension in the case of PZMPC results from the lower zone boundary rising and neither demonstrates the need to correct a prior mistake nor is evidence of a malfunction. Rather, it is a design feature of the PZMPC strategy. The three control strategies produce the same output response until shortly before 11:00 pm, and a very similar output response after approximately 9:00 am (next day). All three control strategies produce the same input response until shortly prior to 10:00 pm and a very similar input response after 8:00 am (next day). Note that the MPC strategies can respond to zone changes in a seemingly non-causal manner, because the PZMPC problem contains the periodically time-dependent zones over the PTS = 45 min prediction horizon. Note further that the PZMPC strategy delivers more insulin in response to the 7:00 am breakfast than the other two strategies. Some statistics are tabulated in Table 1. To summarize, the PZMPC, invariant-zone-MPC, and nighttime-basal strategies are ordered here according to increasing insulin delivery and decreasing average blood glucose levels, both for the whole day and only nighttime.
Figure 3.
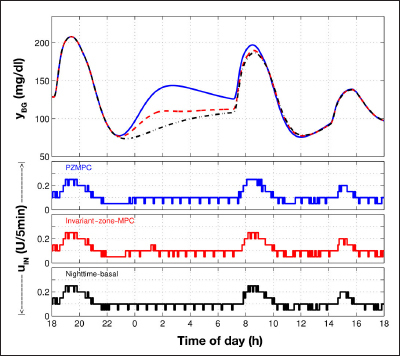
Simulation result. Top plot is blood glucose (yBG mg/ dl): PZMPC (blue, solid), invariant-zone-MPC (red, dashed), and nighttime-basal (black, dash–dotted). Lower three plots are insulin input (uIN U/5 min): PZMPC (blue, top), invariant-zone-MPC (red, middle), and nighttime-basal (black, bottom). This in silico subject results in trajectories with typical characteristics. (See The Typical Case and Table 1.)
Table 1.
Results for 2 of the 100 In Silico Adult Subjectsa
| Control strategy | Insulin delivery | Blood glucose levels | |||
| All day | Nighttime | All day | Nighttime | ||
| PZMPC | =1 | =1 | =1 | =1 | |
| Subject of Figure 3 | |||||
| Invariant-zone-MPC | 1.027 | 1.117 | 0.938 | 0.837 | |
| Nighttime-basal | 1.047 | 1.193 | 0.905 | 0.749 | |
| Subject of Figure 5 | |||||
| Invariant-zone-MPC | 0.993 | 0.856 | 0.968 | 0.738 | |
| Nighttime-basal | 1.019 | 0.921 | 0.825 | 0.457 | |
Ratio of per-subject summed insulin delivery and average blood glucose levels using invariant-zone-MPC and nighttime-basal versus those of PZMPC. Whole day, 6:00 pm-6:00pm; nighttime, 10:00 pm-7:00 am. See Figures 3 and 5 for trajectories.
100 In Silico Subjects
Plotted in Figure 4 are the trajectories of mean blood glucose values over all 100 in silico adult subjects. The three control strategies produce very similar mean responses until midnight and after 9:00 am, with the PZMPC, invariant-zone-MPC, and nighttime-basal strategies producing successively lower mean glucose responses during the night and early morning.
Figure 4.
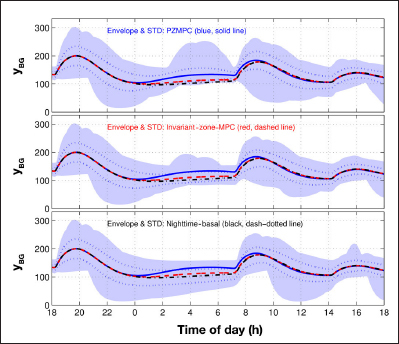
Blood glucose (yBG mg/dl) mean trajectories, mean ± standard deviation, and minimum–maximum envelopes over 100 in silico adult subjects. Mean trajectories identical on each subplot: PZMPC (blue, solid), invariant-zone-MPC (red, dashed), and nighttime-basal (black, dash–dotted). Envelopes (blue area) and standard deviation (blue, dotted): PZMPC (top), invariant-zone-MPC (middle), and nighttime-basal (bottom). STD, standard deviation.
Also plotted in Figure 4 are the minimum–maximum envelopes of the blood glucose responses for the three contrasted control strategies. Again, before midnight and after approximately 9:00 am, the envelopes are very similar. However, the PZMPC, invariant-zone-MPC, and nighttime-basal strategies result in significantly different nighttime envelope boundaries. Of particular interest for the purpose of increased nocturnal safety margins is that with the PZMPC approach, the nighttime lower bound of the envelope spends much time near (partly above) 100 mg/dl.
Further plotted in Figure 4 are the ±1 standard deviations from the means. Analogously to the minimum–maximum envelopes, these indicate that during the night, the glucose levels tend to be elevated for the PZMPC strategy but increasingly reduced for the invariant-zone and nighttime-basal strategies.
Statistics on the average, over 100 in silico adult subjects, insulin delivery, and blood glucose values are tabulated in Table 2. Overnight, the proposed PZMPC strategy delivered 92.7% and 91.6% the amount of insulin the invariant-zone-MPC and nighttime-basal strategies delivered, respectively, while maintaining safe blood glucose levels. The summary conclusion is the same as that stated in Clinical Protocol and Setup for the typical subject response of Figure 3: the PZMPC, invariant-zone-MPC, and nighttime-basal strategies are ordered here according to increasing insulin delivery and decreasing average blood glucose levels, both for the whole day and only nighttime.
Table 2.
Results for 100 In Silico Adult Subjectsa
| Control strategy | PZMPC | Invariant-zone-MPC | Nighttime-basal |
| Insulin delivered (U) | 9.81 ± 2.91 | 10.58 ± 2.92 | 10.70 ± 2.73 |
| 33.62 ± 7.51 | 34.27 ± 7.55 | 34.43 ± 7.36 | |
| Insulin above basal (U) | -0.82 ± 0.94 | -0.05 ± 0.80 | 0.07 ± 0.30 |
| 5.27 ± 2.62 | 5.92 ± 2.67 | 6.09 ± 2.61 | |
| Mean blood glucose (mg/dl) | 122 ± 13 | 110 ± 17 | 105 ± 25 |
| 138 ± 14 | 133 ± 17 | 131 ± 20 | |
| Breakfast (7:00 am) blood glucose (mg/dl) | 131 ± 12 | 115 ± 14 | 110 ± 19 |
| Blood glucose time in range 80-140 mg/dl (%) | 76 ± 28 | 84 ± 20 | 74 ± 32 |
| 55 ± 19 | 59 ± 18 | 55 ± 20 | |
| Blood glucose time in range 70-180 mg/dl (%) | 95 ± 13 | 95 ± 11 | 89 ± 25 |
| 85 ± 13 | 85 ± 12 | 83 ± 16 |
The top row (shaded) of double-row entries corresponds to nighttime (10:00 pm–7:00 am) and the bottom row to the whole day (6:00 pm–6:00 pm). Note that the nighttime basal strategy delivers basal from 10:00 pm to 5:00 am, therefore the nighttime “insulin above basal” from 10:00 pm-7:00 am is not exactly 0 ± 0.
Individual in silico subject data are not provided here due to space constraints. However, the ratio of mean blood glucose level achieved with invariant-zone-MPC versus the mean blood glucose level achieved with PZMPC is less than unity for each in silico subject, both for the whole day and only nighttime. The ratio of total insulin delivery with invariant-zone-MPC versus the total insulin delivery with PZMPC is greater than unity for each in silico subject except one. The one exception is described in more detail in An Atypical Case (see also Figure 5).
Figure 5.
Simulation result. Top plot is blood glucose (yBG mg/dl): PZMPC (blue, solid), invariant-zone-MPC (red, dashed), and nighttime-basal (black, dash–dotted). Lower three plots are insulin input (uIN U/5 min): PZMPC (blue, top), invariant-zone-MPC (red, middle), and nighttime-basal (black, bottom). This in silico subject resulted in atypically large deviations between the contrasted control laws, and PZMPC resulted in higher total insulin delivery than invariant-zone-MPC and nighttime-basal strategies. (See AN ATYPICAL CASE and Table 1.)
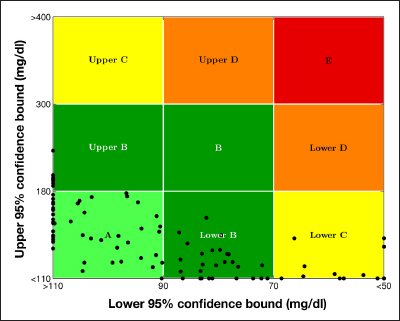
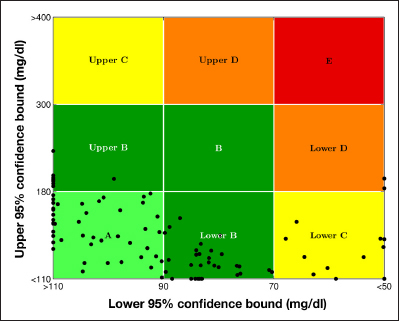
The control variability grid analysis (CVGA)25 plots for the PZMPC, invariant-zone-MPC, and nighttime-basal strategies are depicted in Figures 6–8, respectively. The CVGA statistics are tabulated in Table 3. Both CVGA plots and the statistics table cover only nighttime: 10:00 pm–7:00 am. The horizontal positions are comparable in the three plots, whereas the vertical position is clearly highest for PZMPC and lowest for the nighttime-basal strategy.
Figure 6.
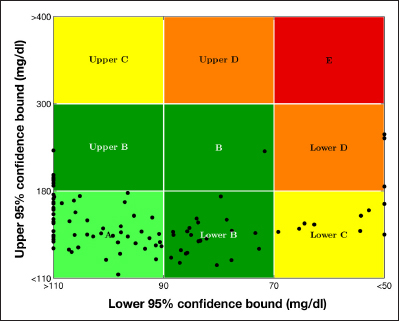
A CVGA plot for 100 in silico adult subjects and PZMPC over nighttime (10:00 pm–7:00 am). For detailed CVGA statistics, consult Table 3.
Figure 8.
A CVGA plot for 100 in silico adult subjects and nighttime-basal strategy over nighttime (10:00 PM–7:00 AM). For detailed CVGA statistics, consult Table 3.
Table 3.
Control Variability Grid Analysis Statistics for 100 In Silico Adult Subjects over Nighttime (10:00 pm–7:00 am)a
| Control strategy | CVGA zone inclusion (%) | ||||
| A | B | C | D | E | |
| PZMPC | 55 | 33 | 9 | 3 | 0 |
| Invariant-zone-MPC | 45 | 41 | 12 | 2 | 0 |
| Nighttime-basal | 46 | 38 | 16 | 0 | 0 |
See Figures 6-8 for CVGA plots.
Figure 7.
A CVGA plot for 100 in silico adu lt subjec ts a nd invar iant-zone-MPC over nighttime (10:00 pm–7:00 am). For detailed CVGA statistics, consult Table 3.
An Atypical Case
With one in silico subject, the total amount of insulin when using PZMPC exceeded the total amount of insulin delivered by the invariant-zone-MPC strategy. The three control strategies’ responses are plotted in Figure 5. Insulin delivery and glucose statistics are provided in Table 1. The blood glucose responses are significantly different after approximately midnight, with very elevated blood glucose levels resulting from the use of PZMPC. The reason why PZMPC results in a higher total insulin delivery is due to the high input rates commanded from shortly before 5:00 am until 7:00 am, when the nighttime zone (110–220 mg/dl) transitions to the daytime zone (80–140 mg/dl). The behavior is not surprising and conforms to the response that can be expected from the PZMPC proposal. It is important to remind the reader that one of the purposes of the University of Padova/Virginia simulator is to facilitate the testing of glycemia controllers on virtual subjects who have physiological parameters over a wide spectrum.
In-Clinic Evaluation
Clinical Protocol and Setup
A preliminary clinical trial was performed in order to test the feasibility of the proposed PZMPC strategy. In this trial, the PZMPC strategy was evaluated on four adult subjects in an in-clinic environment, and the results were compared with the results obtained in previous trials on the same four subjects (each subject served as her/his control) but using the invariant-zone-MPC strategy. The nighttime-basal strategy was not tested in any clinical trial.
Each trial lasted 24 h, starting at 4:00 pm, with an unannounced 50 gCHO dinner at 6:30 pm, an unannounced 40 gCHO breakfast at 7:00 am the next day, and 30 min of exercise.
The clinical trials were performed using the Dexcom Seven Plus CGM, the Animas OneTouch Ping system, and the APS operational, including auxiliary systems, e.g., the Health Monitoring System that monitors for hypoglycemia and provides alarms as necessary. During clinical trials, such hypoglycemia alarms were followed by a 16 gCHO treatment.
Subject information is listed in Table 4. The subjects’ total daily insulin delivery uTDI was employed in the model gain, and the subjects’ time-dependent basal profile uBASAL,i was employed during controller operation. No further subject data were employed.
Table 4.
Clinical Trial Statistics for Nighttime (10:00 pm-7:00 am)a
| Subject | 3 | 8 | 10 | 11 | Mean ± standard deviation |
| Age (years) | 56 | 28 | 44 | 55 | |
| Gender | Male | Female | Female | Female | |
| Years with T1DM | 43 | 7 | 34 | 17 | |
| Weight (kg) | 95.5 | 66.9 | 75.9 | 61.4 | |
| 97.7 | 66.5 | 75.9 | 61.4 | ||
| Total daily insulin uTDI (U) | 41.2 | 36.6 | 32 | 26.1 | |
| 45.1 | 34.4 | 31 | 31.6 | ||
| Insulin delivered (U) | 8.4 | 4.8 | 3.6 | 4 | 5.20 ± 2.2 |
| 9.55 | 6.6 | 4.45 | 6.45 | 6.76 ± 2.1 | |
| Insulin above basal (U) | -1 | -1.03 | -0.7 | -2.2 | -1.23 ± 0.7 |
| 0.15 | 0.55 | 0.57 | -0.05 | 0.31 ± 0.3 | |
| Mean CGM (mg/dl) | 125 | 149 | 131 | 109 | 129 ± 17 |
| 148 | 147 | 137 | 119 | 138 ± 14 | |
| Mean YSI (mg/dl) | 117 | 146 | 149 | 103 | 129 ± 22 |
| 150 | 127 | 143 | 128 | 137 ± 11 | |
| Breakfast (7:00 am) blood glucose (mg/dl) | 93 | 154 | 121 | 118 | 121 ± 25 |
| 84 | 116 | 129 | 138 | 117 ± 24 | |
| Hypoglycemia alarms with 16 gCHO treatments | 3 | 2 | 0 | 2 | |
| 3 | 0 | 1 | 2 | ||
| CGM time in range 80–140 mg/dl (%) | 81 | 29 | 39 | 79 | 56.8 ± 26.8 |
| 47 | 46 | 42 | 85 | 55.0 ± 20.1 | |
| CGM time in range 70–80 mg/dl (%) | 100 | 81 | 100 | 87 | 91.9 ± 9.6 |
| 64 | 86 | 100 | 100 | 87.6 ± 16.8 |
Here PZMPC is contrasted with invariant-zone-MPC. There are no clinical results for the nighttime-basal strategy. The top rows (shaded) of double–row entries correspond to PZMPC and the bottom row to invariant-zone-MPC.
Clinical Results and Discussion
The blood glucose and insulin delivery trajectories for the four subjects are depicted in Figures 9–12. Individual and summary statistics are tabulated in Table 4. The statistics are for the nighttime period 10:00 pm–7:00 am only. On average, over the four subjects, over the entire nighttime, the PZMPC strategy delivered a total of 1.23 ± 0.7 U less than nominal basal, in contrast to the invariant-zone-MPC strategy that, on average, over the four subjects, delivered 0.31 ± 0.3 U in excess of the nominal basal delivery. Recall that the PZMPC strategy enforces nighttime insulin upper bounds that are in excess of the basal rate (specifically, 1.5 uBASAL,i; see Periodic Daily Insulin Input Constraints). Thus the reduction in insulin delivery from the basal rate performed by the PZMPC strategy is not brought about simply by the low upper bound but is a consequence of modulating the blood glucose output target zone. Note that the reduction in nighttime insulin delivery is performed while maintaining practically equivalent, and equally safe, mean blood glucose values, similar breakfast blood glucose values, and analogous mean times in range.
Figure 9.
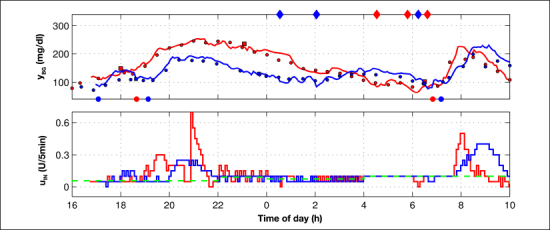
Clinical trial result for subject 3: PZMPC (blue) versus invariant-zone-MPC (red). There are no results for the nighttime-basal control strategy. Continuous glucose monitor, solid line; YSI, filled circles; finger stick, filled squares. Filled diamonds at the top of the yBG plot indicate a hypoglycemia alarm with 16 gCHO treatment. Filled circles at the bottom of the yBG plot indicate meals and one unscheduled, non-rescue snack at 17:05. The green dashed line depicts the basal profiles employed during both the PZMPC and invariant-zone-MPC trial. The PZMPC strategy demonstrates a reduced insulin delivery compared with the invariant-zone strategy after 10:00 pm, with the blood glucose level rising during the approach to breakfast at 7:00 am.
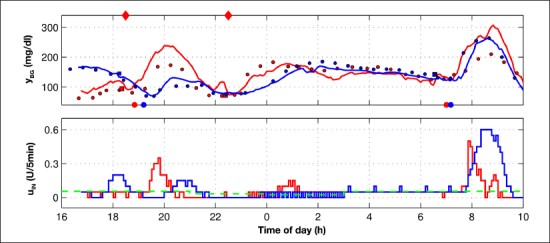
Figure 12.
Clinical trial result for subject 11: PZMPC (blue) versus invariant-zone-MPC (red). There are no results for the nighttime-basal control strategy. Continuous glucose monitor, solid line; YSI, filled circles; finger stick, filled squares. Filled diamonds at the top of the yBG plot indicate a hypoglycemia alarm with 16 gCHO treatment. Filled circles at the bottom of the yBG plot indicate meals. The green dashed line depicts the basal profile during the PZMPC trial. The basal profile during the invariant-zone-MPC trial was slightly different and not plotted. The PZMPC strategy performs a 2 h 45 min (22:01–00:46) pump suspension from the start of the transition from the daytime zone to the nighttime zone and allows the blood glucose level to rise steadily throughout the night. Note, however, that the blood glucose trajectory for the PZMPC case is beneath the daytime zone during the period (22:58–00:32), and thus the invariant-zone-MPC strategy would be expected to perform an extended pump suspension in that case also.
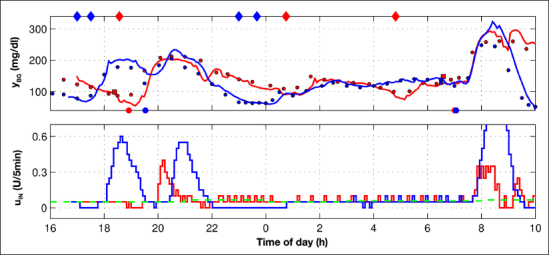
Figure 11.
Clinical trial result for subject 10: PZMPC (blue) versus invariant-zone-MPC (red). There are no results for the nighttime-basal control strategy. Continuous glucose monitor, solid line; YSI, filled circles; finger stick, filled squares. Filled diamonds at the top of the yBG plot indicate a hypoglycemia alarm with 16 gCHO treatment. Filled circles at the bottom of the yBG plot indicate meals. The green dashed line depicts the basal profile during the PZMPC trial. The basal profile during the invariant-zone-MPC trial was slightly different and not plotted. The PZMPC strategy performs a 2 h (21:45–23:45) pump suspension, starting at the start of the transition from the daytime zone to the nighttime zone, and permits the blood glucose level to rise steadily. The invariant-zone-MPC strategy also performs a prolonged pump suspension in the late evening (20:46–23:17, except one controller step at 22:21) but as a result of overdelivery after dinner. The invariant-zone-MPC strategy furthermore administers insulin exceeding the basal rate around 1:00 AM, whereas the PZMPC strategy administers only the basal rate at comparable blood glucose levels during nighttime.
While limited in scope and complicated by differing initial conditions, the preliminary clinical trials indicate the PZMPC strategy’s tendency to reduce insulin delivery during the night, starting before 10:00 pm, and allowing the blood glucose level to rise overnight during times of sleep. This demonstrates that the PZMPC strategy achieves its design objective.
A Comment on Controller Tuning
The two sets of clinical trials, one with PZMPC, the other with invariant-zone-MPC, were not conducted for the purpose of elucidating differences in the respective control strategies. The PZMPC trials were conducted as a proof-of-concept study, and the earlier invariant-zone-MPC trails were part of an independent study. It is important to note that there were differences in both the control algorithm and also the APS platform.
One crucial point is that the PZMPC and invariant-zone-MPC strategy were tuned differently. Specifically, R = 15 for the PZMPC trials, whereas the value of R was higher for the invariant-zone-MPC trials. The change was made for clinical considerations. Unfortunately, this tuning resulted in the PZMPC strategy administering insulin too aggressively, in particular, in response to unannounced meals. This behavior is clearly discernible in Figures 10–12. This aggressive tuning is considered inappropriate, and the parameter R has been adjusted to a higher value for future trials. Despite the unfortunate tuning, the PZMPC strategy administered insulin more conservatively during the night, thus strengthening the above conclusion that the PZMPC strategy achieves its design objective by enforcing safe nocturnal insulin delivery.
Figure 10.
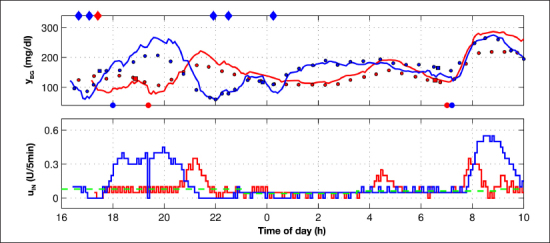
Clinical trial result for subject 8: PZMPC (blue) versus invariant-zone-MPC (red). There are no results for the nighttime-basal control strategy. Continuous glucose monitor, solid line; YSI, filled circles; finger stick, filled squares. Filled diamonds at the top of the yBG plot indicate a hypoglycemia alarm with 16 gCHO treatment. Filled circles at the bottom of the yBG plot indicate meals. The green dashed line depicts the basal profile during the PZMPC trial. The basal profile during the invariant-zone-MPC trial was slightly different and not plotted. The PZMPC strategy performs a 1 h 21 min (21:21–22:42) pump suspension at the end of daytime, starting shortly before the transition to the nighttime zone. This suspension is in response to overdelivery after dinner. The PZMPC strategy further performs a 40 min (00:16–00:56) pump suspension in response to a sudden drop in blood glucose value. Note that the blood glucose level during the drop is within the daytime zone 80–140 mg/dl. With PZMPC, the blood glucose level is allowed to rise during the night. In contrast, the invariant-zone-MPC strategy performs corrective action in the period 4:00 am–5:00 am.
Conclusions
An MPC strategy employing daily periodic blood glucose target zones and daily periodic insulin input constraints was proposed in order to operate glycemia controllers safely for overnight periods when the subject is asleep. The development of an AP that operates safely without requiring subject, or expert, supervision is essential for the deployment of APs that operate for prolonged, multiday periods. Both in silico and clinical testing confirmed that the proposed PZMPC strategy achieves the goal of reducing the threat of hypoglycemia during nighttime. The tradeoff may be slightly elevated glucose levels overnight, yet still in the acceptable near-normal range and without excessive hyperglycemia. Nevertheless, the proposed strategy remains in closed loop at all times of day and strives to correct blood glucose levels that are low, or very high. Thus the proposed strategy is a stepping stone to advancing the control of an AP without switching to delivering the basal rate in open loop during nighttime, as is currently common. The success of the tests and trials conducted thus far lead the authors to believe that time-dependent controller operation is a crucial element for the safe deployment of APs, and it is envisaged that the proposed control strategy— or one similar to it—will be indispensable for the testing, verification, and operation of an AP for the treatment of T1DM.
Acknowledgments
The authors thank the entire T1DM team at the University of California, Santa Barbara, and the clinical research team at the Sansum Diabetes Research Institute for efforts that have supported this research, in particular, Justin J. Lee (University of California, Santa Barbara) for technical assistance with the zone-MPC controllers, Dr. Rebecca A. Harvey (University of California, Santa Barbara) for technical assistance with the Health Monitoring System, and Dr. Wendy C. Bevier (Sansum Diabetes Research Institute) for coordinating the clinical trials. The authors thank the anonymous reviewers for their diligent reading and constructive comments and gratefully acknowledge product support from Animas Corp., Dexcom Inc., and LifeScan Inc.
Glossary
- (AP)
artificial pancreas
- (APS)
artificial pancreas system
- (CGM)
continuous glucose monitor
- (CVGA)
control variability grid analysis
- (gCHO)
gram carbohydrates
- (LTI)
linear time-invariant
- (MPC)
model predictive control
- (PZMPC)
periodic-zone model predictive control
- (T1DM)
type 1 diabetes mellitus
Funding
This work was supported by National Institutes of Health Grants DP3DK094331 and R01DK085628.
Disclosures
Howard C. Zisser is affiliated with or maintains professional relationships with the following companies: Animas Corp. (West Chester, PA; advisory panel), Dexcom Inc. (San Diego, CA; research support), Roche Diagnostics Corp. (Basel, Switzerland; consultant), Eli Lilly and Company (Indianapolis, IN; research support), Insulet Corp. (Bedford, MA; research support/consultant), LifeScan Inc., a Johnson & Johnson Company (Milpitas, CA; research support), MannKind Corp. (Valencia, CA; advisory panel), Medtronic Inc. (Fridley, MN; research support), and Novo Nordisk Inc. (Bagsværd, Denmark; research support).
References
- 1.Cobelli C, Dalla Man C, Sparacino G, Magni L, De Nicolao G, Kovatchev BP. Diabetes: models, signals, and control. IEEE Rev Biomed Eng. 2009;2:54–96. doi: 10.1109/RBME.2009.2036073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harvey RA, Wang Y, Grosman B, Percival MW, Bevier W, Finan DA, Zisser H, Seborg DE, Jovanovič L, Doyle III FJ, Dassau E. Quest for the artificial pancreas: combining technology with treatment. IEEE Eng Med Biol Mag. 2010;29(2):53–62. doi: 10.1109/MEMB.2009.935711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cobelli C, Renard E, Kovatchev B. artificial pancreas: past, present, future. Diabetes. 2011;60(11):2672–2682. doi: 10.2337/db11-0654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zisser H. Clinical hurdles and possible solutions in the implementation of closed-loop control in type 1 diabetes mellitus. J Diabetes Sci Tech nol. 2011;5(5):1283–1286. doi: 10.1177/193229681100500537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parker RS, Doyle III FJ, Peppas NA. A model-based algorithm for blood glucose control in type i diabetic patients. IEEE Trans Biomed Eng. 1999;46(2):148–157. doi: 10.1109/10.740877. [DOI] [PubMed] [Google Scholar]
- 6.Magni L, Raimondo DM, Dalla Man C, De Nicolao G, Kovatchev B, Cobelli C. Model predictive control of glucose concentration in type I diabetic patients: an in silico trial. Biomed Signal Process. 2009;4(4):338–346. [Google Scholar]
- 7.Grosman B, Dassau E, Zisser HC, Jovanovič L, Doyle III FJ. Zone model predictive control: a strategy to minimize hyper- and hypoglycemic events. J Diabetes Sci Technol. 2010;4(4):961–975. doi: 10.1177/193229681000400428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breton M, Farret A, Bruttomesso D, Anderson S, Magni L, Patek S, Dalla Man C, Place J, Demartini S, Del Favero S, Tofanin C, Hughes-Karvetski C, Dassau E, Zisser H, Doyle III FJ, De Nicolao G, Avogaro A, Cobelli C, Renard E, Kovatchev B. International artificial Pancreas Study Group. Fully integrated artificial pancreas in type 1 diabetes: modular closed-loop glucose control maintains near normoglycemia. Diabetes. 2012;61(9):2230–2237. doi: 10.2337/db11-1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elleri D, Allen JM, Kumareswaran K, Leelarathna L, Nodale M, Caldwell K, Cheng P, Kollman C, Haidar A, Murphy HR, Wilinska ME, Acerini CL, Dunger DB, Hovorka R. Closed-loop basal insulin delivery over 36 hours in adolescents with type 1 diabetes. Diabetes Care. 2013;36(4):838–844. doi: 10.2337/dc12-0816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turksoy K, Bayrak ES, Quinn L, Littlejohn E, Cinar A. Multivariable adaptive closed-loop control of an artificial pancreas without meal and activity announcement. Diabetes Technol Ther. 2013;15(5):386–400. doi: 10.1089/dia.2012.0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steil GM, Rebrin K, Darwin C, Hariri F, Saad MF. Feasibility of automating insulin delivery for the treatment of type 1 diabetes. Diabetes. 2006;55(12):3344–3350. doi: 10.2337/db06-0419. [DOI] [PubMed] [Google Scholar]
- 12.Marchetti G, Barolo M, Jovanovič L, Zisser H, Seborg DE. A feedforward-feedback glucose control strategy for type 1 diabetes mellitus. J Process Control. 2008;18(2):149–162. doi: 10.1016/j.jprocont.2007.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phillip M, Battelino T, Atlas E, Kordonouri O, Bratina N, Miller S, Biester T, Stefanija MA, Muller I, Nimri R, Danne T. Nocturnal glucose control with an artificial pancreas at a diabetes camp. N Engl J Med. 2013;368(9):824–833. doi: 10.1056/NEJMoa1206881. [DOI] [PubMed] [Google Scholar]
- 14.Leon BS, Alanis AY, Sanchez EN, Ornelas-Tellez F, Ruiz-Velazquez E. Inverse optimal neural control of blood glucose level for type 1 diabetes mellitus patients. J Franklin Institute Eng Appl Math. 2012;349(5):1851–1870. [Google Scholar]
- 15.Maciejowski JM. Harlow: Pearson; 2002. Predictive control with constraints. [Google Scholar]
- 16.Grosman B, Dassau E, Zisser HC, Jovanovič L, Doyle III FJ. Italy: Milan; 2011. Multi-zone-MPC: clinical inspired control algorithm for the artificial pancreas. Presented at the IFAC World Congress; pp. 7120–7125. [Google Scholar]
- 17.van Heusden K, Dassau E, Zisser HC, Seborg DE, Doyle III FJ. Control-relevant models for glucose control using a priori patient characteristics. IEEE Trans Biomed Eng. 2012;59(7):1839–1849. doi: 10.1109/TBME.2011.2176939. [DOI] [PubMed] [Google Scholar]
- 18.Hovorka R. Continuous glucose monitoring and closed-loop systems. Diabet Med. 2006;23(1):1–12. doi: 10.1111/j.1464-5491.2005.01672.x. [DOI] [PubMed] [Google Scholar]
- 19.Hughes CS, Patek SD, Breton MD, Kovatchev BP. Hypoglycemia prevention via pump attenuation and red-yellow-green “traffic” lights using continuous glucose monitoring and insulin pump data. J Diabetes Sci Technol. 2010;4(5):1146–1155. doi: 10.1177/193229681000400513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harvey RA, Dassau E, Zisser H, Seborg DE, Jovanovič L, Doyle III FJ. Design of the health monitoring system for the artificial pancreas: low glucose prediction module. J Diabetes Sci Technol. 2012;6(6):1345–1354. doi: 10.1177/193229681200600613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turksoy K, Bayrak ES, Quinn L, Littlejohn E, Rollins D, Cinar A. Hypoglycemia early alarm systems based on multivariable models. Ind Eng Chem Res. 2013;52(35):12329–12336. doi: 10.1021/ie3034015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levine WS. 2nd ed. Boca Raton: CRC Press; 2011. The control handbook. [Google Scholar]
- 23.Kovatchev BP, Breton M, Dalla Man C, Cobelli C. In silico preclinical trials: a proof of concept in closed-loop control of type 1 diabetes. J Diabetes Sci Technol. 2009;3(1):44–55. doi: 10.1177/193229680900300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dassau E, Zisser H, Palerm CC, Buckingham BA, Jovanovič L, Doyle III FJ. Modular artificial beta-cell system: a prototype for clinical research. J Diabetes Sci Technol. 2008;2(5):863–872. doi: 10.1177/193229680800200518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Magni L, Raimondo DM, Dalla Man C, Breton M, Patek S, De Nicolao G, Cobelli C, Kovatchev BP. Evaluating the efficacy of closed-loop glucose regulation via control-variability grid analysis. J Diabetes Sci Technol. 2008;2(4):630–635. doi: 10.1177/193229680800200414. [DOI] [PMC free article] [PubMed] [Google Scholar]


