Abstract
Background
Simulation is widely used to teach medical procedures. Our goal was to develop and implement an innovative virtual model to teach resident physicians the cognitive skills of type 1 and type 2 diabetes management.
Methods
A diabetes educational activity was developed consisting of (a) a curriculum using 18 explicit virtual cases, (b) a web-based interactive interface, (c) a simulation model to calculate physiologic outcomes of resident actions, and (d) a library of programmed feedback to critique and guide resident actions between virtual encounters. Primary care residents in 10 U.S. residency programs received the educational activity. Satisfaction and changes in knowledge and confidence in managing diabetes were analyzed with mixed quantitative and qualitative methods.
Results
Pre- and post-education surveys were completed by 92/142 (65%) of residents. Likert scale (five-point) responses were favorably higher than neutral for general satisfaction (94%), recommending to colleagues (91%), training adequacy (91%), and navigation ease (92%). Finding time to complete cases was difficult for 50% of residents. Mean ratings of knowledge (on a five-point scale) posteducational activity improved by +0.5 (p < .01) for use of all available drug classes, +0.9 (p < .01) for how to start and adjust insulin, +0.8 (p < .01) for interpreting blood glucose values, +0.8 (p < .01) for individualizing treatment goals, and +0.7 (p < .01) for confidence in managing diabetes patients.
Conclusions
A virtual diabetes educational activity to teach cognitive skills to manage diabetes to primary care residents was successfully developed, implemented, and well liked. It significantly improved self-assessed knowledge and confidence in diabetes management.
Keywords: clinical competence, diabetes mellitus, medical education, patient simulation, primary care residents, virtual system
Background
The safety and quality of diabetes care in the United States is suboptimal, with only a modest percentage of patients with diabetes achieving all their optimal care targets for blood sugar, blood pressure (BP), and lipid control.1–3Many experts believe that inadequacies related to care delivery and health care professional knowledge contribute to clinical inertia (failure to initiate or intensify treatment in a timely manner for patients who are not achieving care goals) and poor patient outcomes.4–7 Clinical inertia rates are pronounced among resident physicians with medication intensification observed at only 21% of diabetes visits, particularly for insulin treatment.8,9 Consistent with these findings, most physicians today perceive their medical training for chronic illness care as inadequate, and many experts agree that health care professionals need better training to prepare them to treat the growing number of people with chronic conditions such as diabetes.10,11
Adult learning theory emphasizes a focus on interactivity and learner involvement in the process, rather than didactics.12 Compared with youth, adults have a greater need for the learning experience to be relevant to their own job situation, and they prefer to learn through a task or problem-centered orientation (e.g., on-the-job training).12Simulated educational designs incorporate adult learning principles by being case based, interactive, realistic, and self-directed. Web-based simulation technology also overcomes many other potential barriers to quality medical training, including the inconvenience of scheduled live meetings and webinars, the cost of teaching faculty resources, and the lack of consistency often observed when using local opinion leaders. Internet activities can reach large numbers of health care professionals, including those in rural locations, in a cost-effective manner.
Simulated learning designs are by definition dynamic and characterized by the ability of a participant to be immersed in tasks as if it were a real-world experience.13 Simulations are a proven method of providing training, experience, and improving safety in nonmedical industries such as military and aviation.14–16 In addition, simulation has become widely used to teach medical procedures, often with high-fidelity mannequins, to overcome worry over safety issues in real patients due to incomplete knowledge and experience.17–20 Technology-enabled instruction using virtual patients has also been envisioned as a means to provide safe environments to teach and practice the cognitive aspects of managing medical chronic conditions,21 with potential to overcome existing training problems such as limited exposure to a complete variety of patient presentations for chronic diseases and lack of long-term care continuity in ambulatory centers.22 However, there are very few good examples of cognitive simulations related to chronic diseases, primarily because of the complexity and resources needed to develop them.23 We describe the development, implementation, and preliminary evaluation of an innovative online simulated learning technology designed to teach diabetes care management skills comprehensively to primary care residents.
Methods
Trial Design
Nineteen U.S. primary care residency programs agreed to participate in a federally funded translational research trial called Simulated Diabetes Training for Resident Physicians. These residency programs distributed emails and brochures to their 723 residents in all postgraduate years (PGYs), inviting them to participate voluntarily and consent to a study of the educational activity. Residents were offered a $50 gift card for their participation and evaluation. The 19 residency programs were then randomized to receive or not receive the learning activity. Randomized trial data of the impact of the learning activity on measures of objective knowledge test responses and competence (ability to achieve patient care goals on simulated assessment cases) are currently undergoing collection and analysis, and these results are essential and forthcoming. The objective of this article is to describe preliminary findings, including the important effects of the learning activity on satisfaction, self-reported changes in practice patterns, and pre–post changes in self-assessed knowledge and self-confidence in managing diabetes. This analysis is conducted through mixed quantitative and qualitative methods of baseline and postactivity evaluation responses for the 10 programs (with 177 residents) that received the intervention. Figure 1 identifies the 10 residency programs and rates of educational activity and evaluation completion.
Figure 1.
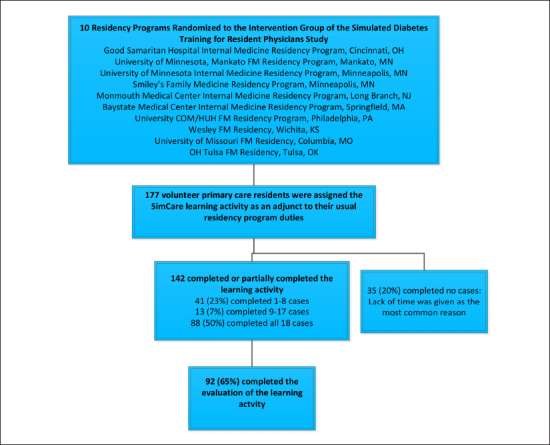
Flow of consented residents randomized to receive the simulated learning activity.
Key Design Components of the Simulated Learning Activity
Curriculum Development
The curriculum was developed by a team of physicians and medical experts at HealthPartners Institute for Education and Research, a nonprofit institute and recognized leader in education and research, in collaboration with the University of Minnesota. The work was funded by a series of federal grants received from the Agency for HealthCare Research and Quality and the National Institutes of Health over 12 years, with estimated development costs totaling millions of dollars. The research team began the development of the resident learning objectives using data and analysis of treatment appropriateness and medical errors observed in practicing physicians to assess needs and gaps in knowledge, a process recommended by the Accreditation Council for Continuing Medical Education.24,25 The learning curriculum was then integrated into 18 virtual cases that each contained distinct basic, intermediate, and advanced educational topics that replicated real and challenging type 1 and type 2 diabetes scenarios (see Figure 2). The learning objectives concentrated on appropriate screening, diagnostic testing, referring, prescribing drugs, monitoring for goal achievement and safety, and managing complications. The educational content was consistent with the latest national guidelines for diabetes, hypertension, and lipid management (American Diabetes Association, Joint National Committee on Hypertension, National Cholesterol Education Program, and Institute for Clinical Systems Improvement).26–30
Figure 2.
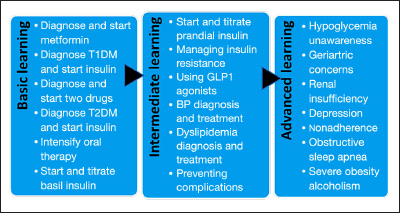
Content covered in the 18 learning case curriculum. Each case was a mix of basic, intermediate, and advanced learning topics. T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; GLP1, glucagon-like peptide 1.
No substantial updates to the curriculum or simulation model were needed during the period of implementation for this study.
Web Design
A web-based interface (see Figure 3) was designed to mimic an interactive electronic health record, and it engaged the resident in care actions over longitudinal visits with the virtual patient. Medical scenarios were portrayed through narrative information displayed on a “snapshot screen.” Users responded by taking actions such as reviewing the chart history; prescribing medications; starting and adjusting insulin; ordering laboratory and diagnostic tests such as electrocardiograms, chest X rays, and sleep studies; making referrals; giving patient advice; viewing self-monitored blood glucose (SMBG) results and changing SMBG frequency; and scheduling phone or visit follow-ups at any desired frequency. Changes in dietary and exercise habits, behavioral and medication adherence, emotional state, and readiness to change were also modeled, and clues to these patient states were provided through narrative supplied at the start of each virtual encounter. The resident could respond to these behavioral and emotional issues by selecting applicable advice topics to discuss with the patient and by referring to multidisciplinary support such as educators, dietitians, psychologists, and pharmacists. The learning environment did not address communication techniques or health literacy.
Figure 3.
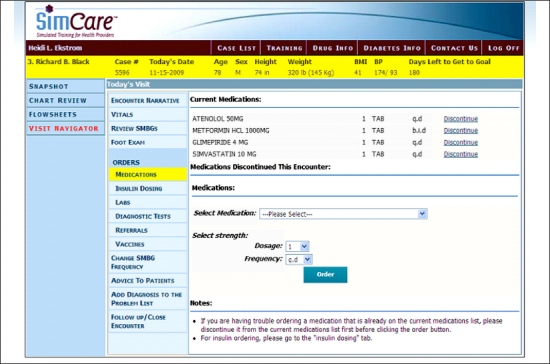
Screenshot of the interface for treating a virtual patient in the SimCare educational activity. The patient name and data is Personal health information was not used to create virtual patients.
Programming the Physiologic Model
The simulation model was developed using a Java31 application running on Linux32 servers, and the data were stored in an Oracle33 database. A physiologic model (or engine) was derived from pharmacokinetic curves and formulas published in literature that were programmed to compute realistic physiologic responses to resident actions.34,35For example, short- and long-acting insulin and oral glycemic drug effects were based on pharmacokinetic curves that distribute the SMBG effects of the drugs over SMBG values through the day. The clinical responses modeled were based on average effects observed in clinical trials. However, to mirror the individual variation of responsiveness also observed in real clinical practice, the average drug effects were attenuated by other virtual patient states such as poor adherence, insulin resistance, and emotional distress. For example, the degree of blood glucose effects to insulin were dampened if the patient had type 2 diabetes (versus type 1), if they were very obese and had higher levels of insulin resistance, if they were nonadherent, or if they had significant depressive symptoms. Blood pressure and lipid effects were similarly modeled.36,37 Prior to implementation with the residents, pilot testing by practicing physicians and diabetes nurse educators validated that the clinical effects observed with each virtual patient were realistic.
Developing the Feedback
Residents learned through multiple modalities. The primary learning mode was “learning by doing,” such that the resident saw realistic clinical responses after each encounter to the treatment actions he/she took. Secondly, the resident learned to anticipate the accumulated effects of treatment decisions through graphic and numerical representations of the projected clinical goals at 6 months of virtual patient time. Lastly, through a predefined rule management system, residents received textual feedback between encounters to suggest future actions and critique past actions taken. The rule management system was maintained on a platform independent from the application that could be edited from a nonprogrammer clinician perspective. Feedback related to many aspects of medical care, including (a) screening, diagnosis, and goal setting; (b) medication starts and adjustments; (c) lifestyle advice and patient education; (d) complication prevention and treatment; (e) safety and monitoring; (f) SMBG frequency and pattern recognition; and (g) appropriateness of the chosen follow-up interval. At the case conclusion, the learner was also provided with actions an expert might take in the case. If care goals were achieved through inappropriate management or with unresolved errors, the case ended but the resident was encouraged to repeat the case using the expert feedback received.
Implementing the Learning Activity
At the start of the activity, the learner received a web link to a brief 10 min demonstration case and completed a hands-on proficiency test to demonstrate ability to care for virtual patients using the simulation model and web-based interface. Then, each month for 6 months, residents received three new learning cases that could be completed from any anywhere with Internet access. Each virtual case took approximately 15–20 min to complete, and residents were challenged to repeat each case as many times as necessary to achieve mastery. Mastery was defined as reaching appropriate clinical targets for glycated hemoglobin (A1C), BP, and low-density lipoprotein (LDL) cholesterol within 6 months of simulated time for each case without clinical management errors or patient safety concerns. Residents did not need to complete the monthly set of learning cases in one sitting and could save their work and come back to complete the cases at any time.
Analysis
Resident characteristics were collected online at baseline for demographics, specialty, and previous diabetes educational experience. Four knowledge assessment questions and one question on confidence in managing diabetes were asked on both the baseline and follow-up surveys, and mean change was calculated for these variables. At the conclusion of the learning activity, an online evaluation survey was conducted that included five satisfaction items, four items evaluating the usefulness of program features, and four items assessing care practice changes. Most items used five-point Likert scale response options. For presentation in tables, some response categories were collapsed because of sparse data. In addition, two open-ended questions were asked to assess the most valuable things learned and areas for improvement, and these responses were categorized into major themes.
Differences in survey item responses by PGY, evaluation survey completion status, gender, race, age, and program type were tested with one-way analysis of variance, Pearson chi-square tests, and Fisher’s exact test. Change in self-assessed knowledge and confidence over time and differential change by PGY were tested with mixed model regression incorporating predictors of PGY, time (baseline versus postintervention), and their interaction.
Protection of Human Subjects
The study was reviewed in advance, approved, and monitored by the HealthPartners Institutional Review Board.
Results
At least one learning case was completed by 142/177(80%) of residents assigned to the learning activity (see Figure 1) and 88/177 (50%) completed all 18 cases. Among the 142 of 177 residents who attempted learning cases, 59/142 (42%) repeated a case at least once. A satisfaction survey was completed by 92/142 (65%) of residents with exposure to any learning case and 75/88 (85%) of residents who completed all 18 cases. At baseline (see Table 1), the residents were 50% female, 44% white, mean age 30 years, 39% family medicine, 51% internal medicine, 6% combined internal medicine– pediatrics, and 6% other specialty. Mean age and race distribution differed by PGY, as did proportion completing an elective rotation with an endocrinologist (6% of PGY-1, 14% of PGY-2, and 44% of PGY-3). Previous diabetes learning experiences, specialty, and self-assessed baseline knowledge of residents who completed the learning activity and evaluation survey did not differ significantly from those who did not complete them (data not shown).
Table 1.
Baseline Characteristics of Primary Care Residents Assigned to the Learning Activity by Postgraduate Year
| Characteristic | All PGY N = 177 | PGY-1 N = 69 | PGY-2 N = 52 | PGY-3–4 N = 56 |
| Female, % | 49.7 | 53.6 | 38.5 | 57.1 |
| Race, % | ||||
| White | 44.1 | 60.9 | 30.8 | 35.7 |
| Asian | 32.2 | 21.7 | 38.5 | 39.3 |
| Black | 5.1 | 2.9 | 5.8 | 7.1 |
| Native American | 2.3 | 4.4 | 1.9 | 0.0 |
| Hispanic | 5.1 | 2.9 | 3.9 | 8.9 |
| Other | 7.9 | 4.4 | 15.4 | 5.4 |
| Not specified | 3.4 | 2.9 | 3.9 | 3.6 |
| White, %a | 44.1 | 60.9 | 30.8 | 35.7 |
| Age, mean (standard deviation)a | 30.4 (3.9) | 29.4 (4.1) | 30.0 (3.0) | 32.1 (4.0) |
| Specialty, % | ||||
| Family medicine | 38.6 | 44.9 | 34.6 | 34.6 |
| Internal medicine | 50.6 | 47.8 | 57.7 | 47.3 |
| Med-peds | 5.7 | 1.5 | 3.9 | 12.7 |
| Other (dermatology, psychiatry, other) | 5.1 | 5.8 | 3.9 | 5.5 |
| Completed a previous online diabetes education program, % | 0.6 | 0.0 | 1.9 | 0.0 |
| Completed an elective rotation with an endocrinologist or diabetologist, %a | 20.1 | 6.0 | 13.5 | 43.6 |
| Learning cases completed, % | ||||
| 0 | 19.8 | 21.7 | 13.5 | 23.2 |
| 1–8 | 23.2 | 27.5 | 17.3 | 23.2 |
| 9–17 | 7.3 | 7.3 | 13.5 | 1.8 |
| 18 | 49.7 | 43.5 | 55.8 | 51.8 |
p < .01
Table 2 shows that self-assessed knowledge and confidence scores increased significantly from baseline to post-intervention, and increases were significantly greater for lower PGY residents. At least 90% had favorable responses to questions about recommending the learning program, being satisfied with the program, and finding the training for the learning experience to be adequate. Half of all residents agreed that finding time to do the learning cases was a problem. Learning program features found very useful by more than 75% of residents included displays of SMBG values (86%), feedback received after the encounter (82%), and diabetes and drug information in the help menu (76%). Graphs showing progress toward A1C, BP, and LDL goals were very useful for 49% of residents. Navigation within the program was reported as very or somewhat easy for 92% of residents. Residents aged 30 years and older were more likely than younger residents (100% versus 82%; p < .01) to recommend the learning program to others; data not shown.
Table 2.
Results of Evaluation Survey (N = 92 Residents) by Postgraduate Year of Residency
| Survey topic | All PGY N = 92 | PGY-1 N = 32 | PGY-2 N = 33 | PGY-3–4 N = 27 |
| Finding time to do the cases was a big problem | ||||
| Agree, % | 50.0 | 65.6 | 39.4 | 44.4 |
| Neutral, % | 26.1 | 18.8 | 24.4 | 37.0 |
| Disagree, % | 23.9 | 15.6 | 36.4 | 18.5 |
| Would recommend the SimCare program to colleagues | ||||
| Agree, % | 91.3 | 84.4 | 100.0 | 88.9 |
| Neutral, % | 6.5 | 9.4 | 0 | 11.1 |
| Disagree, % | 2.2 | 6.3 | 0 | 0 |
| Was satisfied with the SimCare program | ||||
| Agree, % | 93.5 | 87.5 | 100.0 | 92.6 |
| Neutral, % | 3.3 | 6.3 | 0 | 3.7 |
| Disagree, % | 3.3 | 6.3 | 0 | 3.7 |
| Training adequately prepared me to do the learning cases | ||||
| Agree, % | 91.3 | 87.5 | 97.0 | 88.9 |
| Neutral, % | 7.6 | 9.4 | 3.0 | 11.1 |
| Disagree, % | 1.1 | 3.1 | 0 | 0 |
| How easy to navigate through cases | ||||
| Very easy, % | 44.6 | 31.3 | 60.6 | 40.7 |
| Somewhat easy, % | 47.8 | 53.1 | 36.4 | 55.6 |
| Somewhat difficult, % | 7.6 | 15.6 | 3.0 | 3.7 |
| Very difficult, % | 0 | 0 | 0 | 0 |
| Displays of SMBG values | ||||
| Very useful, % | 85.9 | 84.4 | 84.9 | 88.9 |
| Somewhat useful, % | 13.0 | 12.5 | 15.2 | 11.1 |
| Not useful, % | 1.1 | 3.1 | 0 | 0 |
| Feedback received after each encounter | ||||
| Very useful, % | 81.5 | 84.4 | 87.9 | 70.4 |
| Somewhat useful, % | 18.5 | 15.6 | 12.1 | 29.6 |
| Not useful, % | 0 | 0 | 0 | 0 |
| Diabetes and drug information in the links and help menu | ||||
| Very useful, % | 76.1 | 75.0 | 81.8 | 70.4 |
| Somewhat useful, % | 23.9 | 25.0 | 18.2 | 29.6 |
| Not useful, % | 0 | 0 | 0 | 0 |
| Graphs showing progress towards A1C, BP, LDL goal | ||||
| Very useful, % | 48.9 | 59.4 | 45.5 | 40.7 |
| Somewhat useful, % | 41.3 | 28.1 | 45.5 | 51.9 |
| Not useful, % | 9.8 | 12.5 | 9.1 | 7.4 |
| I have already applied what I learned from the simulated cases to actual patients | ||||
| To most patients | 13.0 | 9.4 | 15.2 | 14.8 |
| To many patients | 20.7 | 25.0 | 24.2 | 11.1 |
| To some patients | 44.6 | 46.9 | 42.4 | 44.4 |
| To a few patients | 20.7 | 18.8 | 18.2 | 25.9 |
| Not at all | 1.1 | 0.0 | 0.0 | 3.7 |
| Since doing the SimCare Diabetes cases, the interval between diabetes visits that I recommend for actual patients has | ||||
| Shortened | 63.0 | 59.4 | 57.6 | 74.1 |
| Stayed the same | 34.8 | 40.6 | 36.4 | 25.9 |
| Lengthened | 2.2 | 0.0 | 6.1 | 0.0 |
| Since doing the SimCare Diabetes cases, I am more likely to add a drug or increase the dose of a current medication when an actual patient is above goal | ||||
| Agree, % | 79.4 | 81.3 | 75.8 | 81.5 |
| Neutral, % | 19.6 | 18.8 | 21.2 | 18.5 |
| Disagree, % | 1.1 | 0.0 | 3.0 | 0.0 |
| Since doing the SimCare Diabetes cases, I am more confident about how to use insulin | ||||
| Agree, % | 91.3 | 90.6 | 93.9 | 88.9 |
| Neutral, % | 7.6 | 9.4 | 6.1 | 7.4 |
| Disagree, % | 1.1 | 0.0 | 0.0 | 3.7 |
| How knowledgeable are you about how to use all available drug classes to manage patients with diabetes? (mean) | ||||
| Baseline | 3.2 | 2.7 | 3.4 | 3.4 |
| Postintervention | 3.6 | 3.5 | 3.6 | 3.8 |
| Changea | +0.5b | +0.8b | +0.2 | +0.4b |
| How knowledgeable are you about how to start and adjust insulin? (mean) | ||||
| Baseline | 3.2 | 2.7 | 3.3 | 3.6 |
| Postintervention | 4.1 | 4.0 | 4.1 | 4.3 |
| Changec | +0.9b | +1. 3 b | +0.8b | +0.7b |
| How knowledgeable are you about interpreting patient SMBG? (mean) | ||||
| Baseline | 3.4 | 3.1 | 3.4 | 3.7 |
| Postintervention | 4.2 | 4.3 | 4.2 | 4.2 |
| Changea | +0.8b | +1. 2 b | +1. 2 b | +0.5b |
| How knowledgeable are you about setting individualized treatment goals for people with diabetes? (mean) | ||||
| Baseline | 3.2 | 3.0 | 3.2 | 3.5 |
| Postintervention | 4.1 | 4.0 | 4.0 | 4.2 |
| Change | +0.8b | +1. 0 b | +0.8b | +0.7b |
| How confident are you in managing patients with diabetes? (mean) | ||||
| Baseline | 3.2 | 2.7 | 3.5 | 3.6 |
| Postintervention | 4.0 | 3.8 | 4.1 | 4.1 |
| Changec | +0.7b | +0.9b | +0.6b | +0.5b |
p < .01 residency year by time interaction.
p < .01 change from baseline to postintervention.
p < .05 residency year by time interaction.
A qualitative description of open-ended responses to the most and least valuable features, with categorized responses and examples of comments are presented in Table 3.
Table 3.
Qualitative Assessment of Comments and Suggestions (N = 92 Residents)
| Categories of the most valuable things learned | Number of responses | Example responses |
| Insulin management | 35 | This is the best tool that I’ve had all year on insulin initiation and management. This includes transition from basal to basal–prandial, and management of mixed insulins/transition to mixed insulin. Overall, fabulous learning tool. I would strongly encourage incoming interns to participate if the program was available. |
| General diabetes management | 23 | It was the most useful simulated course I have ever attended. My preceptor and I clearly noticed a difference in my diabetes management. I was so excited to see yesterday that one of my patients dropped from 13 A1C to 9. It was definitely because of this course. I would recommend to every resident. |
| Goal setting | 10 | Knowing the goals and working on it to get there. |
| Follow-up | 8 | Just the importance of quick follow-up to get patients to goal. |
| Medication use and safety | 5 | When to start medications and discontinue them, such as thiazolidinediones. |
| BP management | 4 | Use of multiple drugs to lower BP. |
| Hypoglycemia | 1 | Need for glucagon kit |
| Lipid management | 1 | The options for managing hyperlipidemia and the medications that can be used. |
| Categories of features that could be improved | Number of responses | Example responses |
| Software enhancements | 34 (total) | Medication changes could be a little easier (modify existing medications instead of discontinuing and reordering new dose). |
| Medication ordering | 15 | |
| Laboratory ordering | 13 | |
| General interface | 5 | |
| Accessing information | 4 | |
| Other—nothing bad to report | 27 | I liked the cases, and the overall program was helpful to me. |
| Content improvement | 19 | I would have benefited from more education regarding mixed insulins. |
| Unrealistic | 11 | Some aspects did not mimic actual clinical practice, for example, consults ordered. |
| Time barriers/number of cases | 9 | It was tough to find the time to use it during my busy intern year. |
| Implementation improvement | 3 | The exact duration, number of cases, and time commitment was not clear to me now that I look back on it. |
Discussion
This diabetes simulated educational activity was well-liked by primary care residents. Some enhancements were suggested by learners, including simplifying steps to view laboratory test results and change medication doses and changing the graphical displays of progress toward clinical goals. Notably, 91% of those who completed the evaluation survey indicated that they would recommend it to their colleagues. Comments received from residents included “fabulous learning tool” and “my preceptor has clearly noticed a difference in my [diabetes mellitus] management” and “the best tool I’ve had all year on insulin initiation and management.” Self-assessed ratings of knowledge and self-confidence in managing diabetes were significantly improved post-learning activity in all PGYs.
Virtual patient simulation activities can be a powerful method to change physician behavior in many settings.38While other methods of interactive education may also be effective (e.g., using physician opinion leaders or academic detailers), live methods can be difficult to standardize and disseminate and can be quite costly.39,40 Therefore, simulated learning activities delivered via the Internet have many potential advantages: increased standardization and enhanced scalability. Although there were considerable grant resources used to develop this complex diabetes educational activity, the enduring nature of it could potentially improve the cost-effectiveness over time. A formal cost analysis is planned after the main outcome results are known. Expenses are expected for personnel needed to keep the learning model up-to-date, including one or more content experts to annually review current national guidelines and evidence and recommend changes, programmers to amend the simulation model and feedback accordingly, and health care professionals to pilot test and validate the updates. Cost variation is expected based on the extent of the changes recommended each year (e.g., for 2013, only minor textual changes and no major revisions to the simulation model were recommended). Because the cost of keeping the program up-to-date are independent of the number of users, there is a lower cost for each health care professional who can be engaged if the education is broadly disseminated.
This preliminary evaluation has several possible limitations. Because the activity was voluntary (the proportion volunteering from a residency program ranged from 23–87% of eligible residents), there may have been self-selection of more motivated learners, but a sensitivity analysis showed that satisfaction was not significantly different for residency programs with higher or lower levels of participation. Secondly, not all residents were exposed to the intervention (80% completed one or more of the cases). However, a secondary analysis showed that residents who started but did not complete all 18 cases were just as likely to be satisfied with the learning activity and recommend it to their colleagues as those who completed all 18 cases. As opposed to dissatisfaction with the activity, finding time for the learning activity was identified as a major problem for 66% of first-year residents and 77% of those who did not complete all 18 cases. Lastly, noncompletion of the evaluation by some residents (35%) could potentially bias results toward stronger/more favorable opinions. However, the baseline characteristics of survey completers and noncompleters were not significantly different, and the pattern of results was similarly positive in all major subgroups of residents, including men and women, white and nonwhite, younger and older, family medicine and internal medicine, and community-based versus academically based residency settings. Interestingly, PGY-1 residents gained the most in terms of self-assessed knowledge and confidence but also had the most difficulty finding time to do the learning activity. Nevertheless, it would be of value to re-evaluate the learning activity were it to be implemented as a requirement by a residency program and/or with dedicated time to ensure higher completion rates.
Analysis of objective outcome measures of resident competence as assessed through the randomized trial design will more definitively prove effectiveness of the learning intervention, and these data are forthcoming. However, results of two previous published randomized trials using a prototype of the intervention showed effectiveness of this same simulation technology with practicing primary care providers by demonstrating improved glycemic control and reduced risky prescribing events in their real patients, without increasing costs.41,42 The evaluation of the simulation technology observed in residents, combined with the outcomes observed in practicing health care professionals in previous studies, suggest that the simulated educational technology is well liked and can be effective for health care professionals with a range of clinical experience.
Conclusions
In summary, there is a strong unmet need to develop and broadly disseminate virtual learning technologies potent enough to influence physician behavior and improve quality of chronic disease care. The simulated diabetes educational technology described has virtual case-based design characteristics consistent with adult learning principles that are believed to lead to more successful learning outcomes. As a potential explanatory model for forthcoming main trial analysis of objective knowledge and clinical performance indicators, it is helpful to understand these more qualitative perceptions of residents exposed to the learning activity. The virtual education was successfully developed and implemented with primary care residents, received high satisfaction scores, and demonstrated positive changes in self-assessed knowledge, self-confidence, and practice patterns.
Acknowledgments
Sperl-Hillen is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We gratefully acknowledge the assistance and support of Eugenia Canaan, Amy Murphy, and Debra Curran (staff within HPIER) for their understanding of graduate medical education and help with implementation and for their role in getting the program approved for continuing medical education credit. We also thank George Biltz from the University of Minnesota for his assistance in modeling the physiology within the simulation program.
Glossary
- (A1C)
glycated hemoglobin
- (BP)
blood pressure
- (LDL)
low-density lipoprotein
- (PGY)
postgraduate year
- (SMBG)
self-monitored blood glucose
Funding
This study is funded by an R18 translational research grant from the National Institute of Diabetes and Digestive and Kidney Diseases (grant number 5R18DK079861).
Disclosures
JoAnn Sperl-Hillen, Patrick O’Connor, Heidi Ekstrom, William Rush, Steve Asche, Omar Fernandes, Deepika Appana, and Gerald Amundson receive research support from public funding sources (National Institutes of Health) administered through HealthPartners Institute for Education and Research (HPIER), a nonprofit health care organization. Paul Johnson receives research support from public funding sources (National Institutes of Health) administered through the University of Minnesota.
JoAnn Sperl-Hillen and Omar Fernandes also received research support from Merck Sharp and Dohme Corp. administered through HPIER for a randomized trial of methods to educate patients with diabetes.
JoAnn Sperl-Hillen, Patrick O’Connor, Bill Rush, and Paul Johnson are listed inventors on a U.S. patent (8,388,348 B2) issued 3/5/2013 titled “Disease Treatment Simulation.” HPIER has a royalty-bearing license agreement with a third party to commercialize the simulation technology for the purpose of broader dissemination. The University of Minnesota has a contract with HPIER for revenue related to the royalty bearing license agreement. Dr. Sperl-Hillen serves as a non-paid member of the board of directors for that licensee. The HealthPartners and University of Minnesota intellectual property policies makes it possible for JoAnn Sperl-Hillen, Patrick O’Connor, Bill Rush, and Paul Johnson to potentially receive financial payments in the future as an inventor of the technology.
References
- 1.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291(3):335–342. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 2.Spann SJ, Nutting PA, Galliher JM, Peterson KA, Pavlik VN, Dickinson LM, Volk RJ. Management of type 2 diabetes in the primary care setting: a practice-based research network study. Ann Fam Med. 2006;4(1):23–31. doi: 10.1370/afm.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger JE, Ahmann AJ, Balfour DC, Owens GS, Beltran R, Bush MA, Culpepper L, Owens GS, Ringel M, Welty FK. Treating to target: implementing an effective diabetes care paradigm for managed care. Am J Manag Care. 2010;(16 Suppl Treating):S4–S35. [PubMed] [Google Scholar]
- 4.Phillips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, Miller CD, Ziemer DC, Barnes CS. Clinical inertia. Ann Intern Med. 2001;135(9):825–834. doi: 10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]
- 5.Schmittdiel JA, Uratsu CS, Karter AJ, Heisler M, Subramanian U, Mangione CM, Selby JV. Why don’t diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensification. J Gen Intern Med. 2008;23(5):588–594. doi: 10.1007/s11606-008-0554-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peyrot M, Rubin RR, Lauritzen T, Skovlund SE, Snoek FJ, Matthews DR, Landgraf R, Kleinebreil L. International DAWN Advisory Panel. Resistance to insulin therapy among patients and providers: results of the cross-national Diabetes Attitudes, Wishes, and Needs (DAWN) study. Diabetes Care. 2005;28(11):2673–2679. doi: 10.2337/diacare.28.11.2673. [DOI] [PubMed] [Google Scholar]
- 7.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 8.Phillips LS, Ziemer DC, Doyle JP, Barnes CS, Kolm P, Branch WT, Caudle JM, Cook CB, Dunbar VG, El-Kebbi IM, Gallina DL, Hayes RP, Miller CD, Rhee MK, Thompson DM, Watkins C. An endocrinologist-supported intervention aimed at providers improves diabetes management in a primary care site: improving primary care of African Americans with diabetes (IPCAAD) 7. Diabetes Care. 2005;28(10):2352–2360. doi: 10.2337/diacare.28.10.2352. [DOI] [PubMed] [Google Scholar]
- 9.Ziemer DC, Miller CD, Rhee MK, Doyle JP, Watkins C, Jr, Cook CB, Gallina DL, El-Kebbi IM, Barnes CS, Dunbar VG, Branch WT, Jr, Phillips LS. Clinical inertia contributes to poor diabetes control in a primary care setting. Diabetes Educ. 2005;31(4):564–571. doi: 10.1177/0145721705279050. [DOI] [PubMed] [Google Scholar]
- 10.Darer JD, Hwang W, Pham HH, Bass EB, Anderson G. More training needed in chronic care: a survey of US physicians. Acad Med. 2004;79(6):541–548. doi: 10.1097/00001888-200406000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Williamson JC, Glauser TA, Nevins PH, Schneider D, Kruger DF, Urquhart BS, Whitfield SF, Dubois AM. Current practice patterns and identified educational needs of health care providers in managing patients with type 2 diabetes. Clin Diabetes. 2013;31(1):3–9. [Google Scholar]
- 12.Knowles M. Adult learning. In: Craig RL, editor. The ASTD training and development handbook. New York: McGraw-Hill; 1996. pp. 253–264. [Google Scholar]
- 13.Gaba DM. The future vision of simulation in health care. Qual Saf Health Care. 2004;(13 Suppl 1):i2–i10. doi: 10.1136/qshc.2004.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Latorella K, Pliske R, Hutton R, Chrenka J. Cognitive task analysis of business jet pilots’ weather flying behaviors: preliminary results. NASA/ TM-2001-211034. 2001 Jul [Google Scholar]
- 15.Leitch RA, Moses GR, Magee H. Simulation and the future of military medicine. Mil Med. 2002;167(4):350–354. [PubMed] [Google Scholar]
- 16.Yesavage JA, Jo B, Adamson MM, Kennedy Q, Noda A, Hernandez B, Zeitzer JM, Friedman LF, Fairchild K, Scanlon BK, Murphy GM, Jr, Taylor JL. Initial cognitive performance predicts longitudinal aviator performance. J Gerontol B Psychol Sci Soc Sci. 2011;66(4):444–453. doi: 10.1093/geronb/gbr031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pacsi AL. Human simulators in nursing education. JNY State Nurses Assoc. 2008;39(2):8–11. [PubMed] [Google Scholar]
- 18.Michelson JD. Simulation in orthopaedic education: an overview of theory and practice. J Bone Joint Surg Am. 2006;88(6):1405–1411. doi: 10.2106/JBJS.F.00027. [DOI] [PubMed] [Google Scholar]
- 19.Le CQ, Lightner DJ, VanderLei L, Segura JW, Gettman MT. The current role of medical simulation in american urological residency training programs: an assessment by program directors. J Urol. 2007;177(1):288–291. doi: 10.1016/j.juro.2006.08.106. [DOI] [PubMed] [Google Scholar]
- 20.Wayne DB, Butter J, Siddall VJ, Fudala MJ, Linquist LA, Feinglass J, Wade LD, McGaghie WC. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17(3):210–216. doi: 10.1207/s15328015tlm1703_3. [DOI] [PubMed] [Google Scholar]
- 21.Lehmann ED. Interactive educational diabetes simulators: a look to the future. Diabetes Technol Ther. 2000;2(3):507–511. doi: 10.1089/15209150050194378. [DOI] [PubMed] [Google Scholar]
- 22.Karamanoukian RL, Ku JK, DeLaRosa J, Karamanoukian HL, Evans GR. The effects of restricted work hours on clinical training. Am Surg. 2006;72(1):19–21. doi: 10.1177/000313480607200105. [DOI] [PubMed] [Google Scholar]
- 23.Huang G, Reynolds R, Candler C. Virtual patient simulation at US and Canadian medical schools. Acad Med. 2007;82(5):446–451. doi: 10.1097/ACM.0b013e31803e8a0a. [DOI] [PubMed] [Google Scholar]
- 24.Wittich CM, Chutka DS, Mauck KF, Berger RA, Litin SC, Beckman TJ. Perspective: a practical approach to defining professional practice gaps for continuing medical education. Acad Med. 2012;87(5):582–585. doi: 10.1097/ACM.0b013e31824d4d5f. [DOI] [PubMed] [Google Scholar]
- 25.Fox RD. Revisiting “Discrepancy analysis in continuing medical education: a conceptual model” 1983. J Contin Educ Health Prof. 2011;31(1):71–76. doi: 10.1002/chp.20104. [DOI] [PubMed] [Google Scholar]
- 26.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT., Jr Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 27.American Diabetes Association. Standards of medical care in diabetes--2012. Diabetes Care. 2012;(35 Suppl 1):S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Institute for Clinical Systems Improvement. Minneapolis: Institute for Clinical Systems Improvement; 2010. Health care guideline: diagnosis and management of type 2 diabetes mellitus in adults. [Google Scholar]
- 29.National Institutes of Health; Department of Health and Human Services. Third report of the expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) 2004. http://www.nhlbi.nih.gov/guidelines/cholesterol/index.htm.
- 30.Institute for Clinical Systems Improvement. Minneapolis: Institute for Clinical Systems Improvement; 2011. Health Care guideline: lipid management in adults. [Google Scholar]
- 31.Oracle Technology Network. Java EE. http://www.oracle.com/technetwork/java/javaee/overview/index.html.
- 32.Linux. https://www.linux.com/
- 33.Oracle. Oracle Database. http://www.oracle.com/us/products/database/index.html.
- 34.Sherifali D, Nerenberg K, Pullenayegum E, Cheng JE, Gerstein HC. The effect of oral antidiabetic agents on A1C levels: a systematic review and meta-analysis. Diabetes Care. 2010;33(8):1859–1864. doi: 10.2337/dc09-1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bolen S, Feldman L, Vassy J, Wilson L, Yeh HC, Marinopoulos S, Wiley C, Selvin E, Wilson R, Bass EB, Brancati FL. Systematic review: comparative effectiveness and safety of oral medications for type 2 diabetes mellitus. Ann Intern Med. 2007;147(6):386–399. doi: 10.7326/0003-4819-147-6-200709180-00178. [DOI] [PubMed] [Google Scholar]
- 36.Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326(7404):1427. doi: 10.1136/bmj.326.7404.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sharma M, Ansari MT, Abou-Setta AM, Soares-Weiser K, Ooi TC, Sears M, Yazdi F, Tsertsvadze A, Moher D. Systematic Review: Comparative effectiveness and Harms of Combinations of Lipid-Modifying Agents and High-Dose Statin Monotherapy. Ann Intern Med. 2009;151(9) doi: 10.7326/0003-4819-151-9-200911030-00144. [DOI] [PubMed] [Google Scholar]
- 38.Cook DA, Erwin PJ, Triola MM. Computerized virtual patients in health professions education: a systematic review and meta-analysis. Acad Med. 2010;85(10):1589–1602. doi: 10.1097/ACM.0b013e3181edfe13. [DOI] [PubMed] [Google Scholar]
- 39.Soumerai SB, McLaughlin TJ, Gurwitz JH, Guadagnoli E, Hauptman PJ, Borbas C, Morris N, McLaughlin B, Gao X, Willison DJ, Asinger R, Gobel F. effect of local medical opinion leaders on quality of care for acute myocardial infarction: a randomized controlled trial. JAMA. 1998;279(17):1358–1363. doi: 10.1001/jama.279.17.1358. [DOI] [PubMed] [Google Scholar]
- 40.Avorn J, Soumerai SB. Improving drug-therapy decisions through educational outreach. A randomized controlled trial of academically based “detailing.”. N Engl J Med. 1983;308(24):1457–1463. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- 41.Sperl-Hillen JM, O’Connor PJ, Rush WA, Johnson PE, Gilmer T, Biltz G, Asche SE, Ekstrom HL. Simulated physician learning program improves glucose control in adults with diabetes. Diabetes Care. 2010;33(8):1727–1733. doi: 10.2337/dc10-0439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Connor PJ, Sperl-Hillen JM, Johnson PE, Rush WA, Asche SE, Dutta P, Biltz GR. Simulated physician learning intervention to improve safety and quality of diabetes care: a randomized trial. Diabetes Care. 2009;32(4):585–590. doi: 10.2337/dc08-0944. [DOI] [PMC free article] [PubMed] [Google Scholar]


