Abstract
Objective. To describe small area variation in ambulatory electronic health record (EHR) adoption and assess evidence of a “digital divide” in whether adoption is lagging in traditionally underserved communities.
Data Sources. Survey data on U.S. ambulatory health care sites (261,973 sites representing 716,160 providers) collected by SK&A Information Services in 2011.
Study Design. We examined cross-sectional variation in two measures of local area EHR adoption: share of providers at sites using an EHR with e-prescribing functionality; and predicted probability of EHR adoption for the average site. Local areas were defined as Public Use Microdata Areas (n = 2,068). Using multivariate regression, we examined the association between adoption and three area characteristics: high concentration of minority population; high concentration of low-income population; and metropolitan status.
Principal Findings. EHR adoption varied significantly across local areas, ranging from 8 to 88 percent with a median of 41 percent. Adoption was lower in large metropolitan areas; areas with high concentration of minority population in the Northeast and West; and areas with high concentration of low-income population in the Midwest.
Conclusions. Our 2011 estimates suggest there was substantial room for increased EHR adoption across the United States, including some underserved areas with relatively low EHR adoption rates. Further research should monitor policy initiatives in these areas and examine sources of heterogeneity in low- and high-adoption communities.
Keywords: Electronic health records, geographic variation, underserved populations, ambulatory care
Ambulatory electronic health record (EHR) adoption in the United States has surged in recent years, concurrent with implementation of the Health Information Technology for Economic and Clinical Health (HITECH) Act provisions designed to support adoption and meaningful use of EHRs. In 2011, a third of office-based physicians (34 percent) used a basic EHR, while just over one in five physicians did in 2009 (Hsiao et al. 2012). Adoption among primary care physicians has nearly doubled over the same time period, rising from 20 percent in 2009 to 39 percent in 2011 (Patel et al. 2013).
Growth in EHR adoption has the potential to lead to improved health care quality, efficiency, and outcomes (Chaudhry et al. 2006; Goldzweig et al. 2009; Buntin et al. 2011), and ensuring that these benefits accrue to all patient populations is a national priority (Office of the National Coordinator for Health Information Technology 2011). Of particular concern are geographic areas and population groups that have traditionally experienced disparities in health care access, quality, and outcomes. These disparities may be caused by many interrelated mechanisms (Smedley, Stith, and Nelson 2003), including limited or delayed access to new health technology (Ferris et al. 2006). Ambulatory providers who serve these populations may face disproportionate barriers to EHR adoption, including resource constraints, organizational complexity, a less favorable business case for adoption, and lack of expertise necessary to implement and integrate EHRs into practice workflow (Miller and West 2007; Miller et al. 2009; Dennehy et al. 2011; Gibbons 2011). If the adoption of EHRs is slower in underserved areas, there is a risk of creating a “digital divide” in access to benefits from health information technology (Blumenthal et al. 2006).
Prior studies have estimated rates of EHR adoption in ambulatory care at various levels of geography, including national (DesRoches et al. 2008; Hsiao et al. 2012), state (Simon et al. 2007; Bramble et al. 2010; Baier et al. 2011; Menachemi et al. 2011), and regional (Bell, Daly, and Robinson 2003; Rosenthal and Layman 2008). Other studies have estimated ambulatory EHR adoption rates by specialty (Kemper, Uren, and Clark 2006; Chiang et al. 2008; Stream 2009; Bazemore et al. 2011), practice type (Shields et al. 2007; Robinson et al. 2009), and setting (Singh et al. 2011).
However, few studies have compared adoption rates across geographic areas. Recent national surveys showed substantial variation across states in the share of physicians with basic EHRs (Hsiao et al. 2012). However, beyond a few single-state studies indicating that EHR adoption varied according to some local health care market characteristics (Abdolrasulnia et al. 2008; Menachemi et al. 2012), little is known about the extent of geographic variation in adoption between local areas within states.
There are also limited recent data on differences in physician EHR adoption according to patient population characteristics. The available evidence is mixed and are derived from surveys conducted prior to the recent surge in EHR use. An analysis of national survey data from 2005 to 2006 found that uninsured black and Hispanic patients and Hispanic Medicaid patients were less likely than privately insured white patients to have primary care physicians who used an EHR (Hing and Burt 2009). Another study found a negative association between the proportion of Hispanic patients on physicians’ patient panels and physician EHR adoption (Li and West-Strum 2010). In 2006, community health centers serving a higher volume of uninsured patients and patients with incomes below the poverty level were less likely to have an EHR than other centers (Shields et al. 2007). However, other analyses of national and single-state surveys conducted between 2000 and 2008 found no association between EHR adoption and county-level race, ethnicity, or income (Blumenthal et al. 2006) or the race and insurance status of physicians’ patient panels (Grossman and Reed 2006; DesRoches et al. 2008; Jha et al. 2009). Whether such patterns have persisted throughout the recent rapid growth in EHR adoption is unknown.
This analysis provides an updated and uniquely comprehensive assessment of small area variation in ambulatory EHR adoption. Specifically, we use data collected from all known ambulatory health care sites in the United States to estimate local area EHR adoption rates and assess whether adoption is lagging behind in areas with high concentrations of traditionally underserved populations. We focus on geographic areas and population groups identified as federal priority populations for monitoring disparities in health care access and outcomes: racial and ethnic minorities; low-income populations; and residents of rural areas and inner cities (Agency for Healthcare Research and Quality 2010).We examine associations at both the national and regional levels to shed light on how best to target limited resources to increase EHR adoption. Disparities observed at the national level could be driven by differences in EHR adoption between regions of the country—for example, local areas with high concentrations of minority population may be disproportionately located in regions with low-adoption rates in all areas, including those with high minority and low minority population concentrations. If this were the case, national disparities may be better remedied by efforts to increase adoption in those regions overall rather than efforts targeted specifically to areas with high-minority population concentrations. On the other hand, if disparities by minority population concentration are present across all regions, it will be important to target resources to equalizing EHR adoption rates within regions (Skinner et al. 2003; Baicker et al. 2004).
Our findings have important policy implications in assessing the presence of a “digital divide” in access to EHR technology and in setting a baseline for monitoring the change in EHR adoption rates over time as HITECH and other initiatives target underserved communities.
Methods
Data on Ambulatory Health Care Sites
We obtained data on ambulatory health care sites in 2011 from the SK&A Office-Based Providers Database, a product of SK&A Information Services, Irvine, CA. The database is designed to comprise a census of ambulatory health care sites with at least one provider with prescribing authority in the 50 states and District of Columbia. Information on the sites and the providers practicing in them are gathered from a range of sources, including the National Provider Identifier database, state licensing data, and administrative data from insurers and medical device and pharmaceutical vendors. These data are phone verified through a rolling telephone survey. All sites are contacted twice a year and asked to confirm information on practice location, the providers who work at the site, and other site characteristics. The target respondent is the office manager. The data used for this study reflect providers who were in active practice during calendar year 2011.1
The sites are asked whether they had installed EHR technology and, if so, whether it had e-prescribing functionality. For this analysis, we created a dichotomous measure of whether the site used an EHR with e-prescribing functionality. EHR adoption with e-prescribing functionality is a requirement for the receipt of technical assistance from some HITECH programs (Maxson et al. 2010) and has been shown to be highly correlated with EHR adoption across geography (Maxson, Buntin, and Mostashari 2010).
We also created variables for several site characteristics, including the number of providers at the site (counting physicians, nurse practitioners, and physician assistants); whether the site was part of a multi-site group practice; the mix of provider types at the site (physicians only, physicians and nurse practitioners or physicians assistants, nurse practitioners or physicians assistants only); the mix of provider specialties at the site (primary care only, specialists only, or multi-specialty; primary care was defined as general or family practice, internal medicine, geriatrics, pediatrics, adolescent medicine, and obstetrics and gynecology); whether the site was owned by a hospital; and whether the site was affiliated with a health system.
Local Area EHR Adoption Rates
To characterize local area EHR adoption, we employed U.S. Census Public Use Microdata Area (PUMA) boundaries. Defined for use in census data collection and reporting, PUMAs are areas of 100,000 residents or more and are comprised of contiguous census tracts or counties (U.S. Census Bureau 2009). In most cases, PUMAs are defined by State Data Centers and are designed to represent communities with relatively homogenous characteristics. The most recently defined PUMAs are based on census data from 2000 and delineate 2,068 local areas across the country. Because they are constructed to represent homogenous communities, PUMAs are likely to capture meaningful differences in population characteristics of interest in this study. Moreover, the minimum population threshold of PUMAs enables the estimation of relatively stable rates of local area EHR adoption (as compared with counties or primary care service areas, many of which have very small population sizes, for example) while allowing the examination of EHR adoption patterns at a more granular level than health care market boundaries that contain larger, more heterogeneous populations and geographic areas (hospital referral regions, for example). Though not widely used in health services research, PUMAs have been used to assess small area variation in phenomena such as health insurance coverage (Kenney et al. 2010), health literacy (Lurie et al. 2009), and ambulatory care sensitive health care utilization (Gresenz, Ruder, and Lurie 2009).
To describe geographic variation in ambulatory EHR adoption, we calculated two measures of EHR adoption across local areas. The first measure was the share of providers in each local area who were practicing at sites using an EHR with e-prescribing functionality, incorporating shrinkage factors to adjust for variability due to the small number of ambulatory providers in some PUMAs. We estimated a multilevel linear probability model of the probability that a provider was at a site using an EHR with e-prescribing functionality. The model included PUMA random effects and no covariates. From this model, we obtained the predicted probability of EHR adoption (incorporating predictions of the PUMA random effects) and calculated the average predicted probability of EHR adoption across all providers in each PUMA. These predicted probabilities differ from the raw EHR adoption rates by incorporating the PUMA random effects to adjust for random error including error due to small numbers of providers in some PUMAs. The predicted PUMA random effects (shrinkage factors) adjust the local area EHR adoption rate toward the overall mean at a rate that is inversely proportional to the precision of the PUMA-specific estimate and the variance of the PUMA random effects (Rabe-Hesketh and Skrondal 2005).
Our second measure was the predicted probability of EHR adoption for the average provider's site, which allowed us to assess variation in local EHR adoption rates independent of differences in provider and site characteristics across areas. We estimated a multilevel linear probability model of the probability that a site used an EHR with e-prescribing functionality as a function of the site-level characteristics described above. The model also included PUMA random effects. We calculated the predicted probability of EHR adoption for the average provider's site, calculated at the mean of site characteristics weighted by the number of providers. We allowed this prediction to vary across PUMAs by incorporating the predicted value of the PUMA random effect. Thus, this second local area EHR adoption rate reflects variation across areas in the probability of EHR adoption independent of differences in site characteristics.
Data on Local Area Characteristics
We examined three local area characteristics corresponding to geographic areas and population groups that have traditionally experienced disparities in health care access and outcomes: concentration of racial and ethnic minority population; concentration of low-income population; and metropolitan status. We obtained data on the share of the PUMA population that was from a racial or ethnic minority group (defined as being of nonwhite race and/or Hispanic origin) and the share of the PUMA population that was low income (defined as having a family income below 200 percent of the federal poverty level) from the American Community Survey 2008–2010 3-year estimates.
To characterize the metropolitan status of PUMAs, we used a slight adaptation of the National Center for Health Statistics (NCHS) Urban-Rural Classification Scheme (Ingram and Franco 2012). We assigned PUMAs into one of four groups: large-central metropolitan (akin to inner cities that are part of a metropolitan area with at least 1 million population); large-fringe metropolitan (akin to suburban areas that are part of a metropolitan area with at least 1 million population); medium/small metropolitan (metropolitan areas with at least 50,000 but less than 1 million population); and nonmetropolitan (areas with no urban area with at least 50,000 population). As the NCHS scheme is defined at the county level, we categorized each PUMA based on the NCHS designation of the county in which the PUMA is located. In cases where a PUMA's boundaries spanned two or more counties and those counties had different NCHS designations (n = 437 PUMAs), we assigned the PUMA to the NCHS designation in which the majority of the PUMA population was located.
We also created control variables for area characteristics that have been shown or are hypothesized to influence EHR adoption (Abdolrasulnia et al. 2008; Menachemi et al. 2012), including health maintenance organization (HMO) penetration; supply of health care resources; insurance coverage; and changes in unemployment. From HealthLeaders-InterStudy, we obtained county-level data on the share of the population that was enrolled in an HMO in 2011. From the Area Resource File, we obtained county-level information on short-term general hospital beds per 1,000 population in 2008; share of the population that was uninsured in 2009; and change in unemployment rate between 2007 and 2009. To transform these county-level variables to the PUMA level, we assigned to each PUMA the value of the county in which the PUMA is located. For PUMAs that spanned multiple counties, we assigned to the PUMA the average value across relevant counties, weighted proportionally to the share of the PUMA population living in each county. Finally, we calculated the number of ambulatory providers per 1,000 population in the PUMA using the total number of providers from SK&A.
Analysis of Variation in Local Area EHR Adoption Rates
We first used descriptive visualizations to assess the extent of variation in local area EHR adoption rates nationally, within states, and according to priority population characteristics. We then conducted multivariate logistic regression analyses to assess the association between local area EHR adoption and each of the priority population indicators. We estimated two sets of models—one with the dependent variable based on the local area EHR adoption rate unadjusted for site characteristics and a second with the dependent variable based on the predicted probability of EHR adoption for the average provider's site, as described above.
We estimated models with dependent variables as dichotomous measures of whether the area was a low-EHR adoption area, defined as being in the lowest quartile of EHR adoption rates nationally. The independent variables were indicators of whether the local area had high concentrations of minority and low-income populations (defined as being in the highest quartiles nationally) and indicators for each category of metropolitan status. The reference categories were the area types that typically are less likely to experience disparities: areas without high concentrations of minority and low-income populations and large fringe metropolitan areas, which are akin to suburban areas (Agency for Healthcare Research and Quality 2010).
We then conducted regional-level analyses by estimating models predicting if the area was in the lowest quartile of EHR adoption rates within the area's Census region. Similarly, in these models the key independent variables were equal to one if the share of the local area population that was minority or low income was in the highest quartile within the area's region. We included indicator variables for the Census regions (with the modal region, South, as the reference category) and interactions between these region indicators and the area characteristics. We calculated the marginal effects associated with the priority population indicators in each region and evaluated whether they were significantly different from zero using standard errors obtained by the delta method (Karaca-Mandic, Norton, and Dowd 2012). In contrast to the national analysis in which thresholds for high concentration of minority and low-income populations were based on the national distributions, thresholds in the regional analysis were based on the regional distributions to better measure whether areas with high concentrations of minority and low-income population relative to other areas in the region were more likely to have low-adoption rates.
Finally, we estimated additional models to assess whether associations between priority population characteristics and local area EHR adoption persisted after controlling for other area characteristics that may influence adoption.
Sensitivity Analyses
We assessed the robustness of our findings to alternate specification and estimation strategies. In addition to using linear probability models with random effects to estimate the local area EHR adoption rates, we estimated these rates using logistic regression with random effects. Results were nearly identical, so we proceeded with the linear probability estimates for ease of estimation and interpretation.
We also estimated additional models to examine the association between local area EHR adoption rates and local area priority population characteristics with continuous specifications of the dependent variable (EHR adoption rate) and key independent variables (share of population that was minority and share of population that was low income) instead of dichotomous indicators of low adoption and high-priority population concentration. Results were substantively similar to our main results reported here.
Results
Characteristics of Ambulatory Health Care Sites and Local Areas
The top panel of Table 1 describes the characteristics of ambulatory health care sites in the United States. In 2011, about half of all ambulatory health care sites (49 percent) had one provider (physician, nurse practitioner, or physician assistant) and 89 percent of sites had five or fewer providers (Table 1). However, the 12 percent of sites with more than five providers accounted for 46 percent of all providers. The majority of sites (85 percent) did not report being part of a multi-site group practice, although one-quarter of all providers were in a multi-site group practice with more than 10 providers in the group. About one-quarter of sites (26 percent) had a mix of physicians and nurse practitioners or physician assistants; half of providers worked in these types of sites. Just over half of sites (54 percent) had specialist providers only and 40 percent had primary care providers only. Nearly one in five providers (18 percent) worked in the 6 percent of sites with a mix of primary care and specialist providers. The majority of sites and providers were not owned by a hospital nor affiliated with a health system.
Table 1.
Characteristics of US Ambulatory Health Care Sites and Public Use Microdata Area (PUMA)
| Characteristics of US Ambulatory Health Care Sites | % of Sites (N = 261,973) | % of Providers (N = 716,160) |
|---|---|---|
| Number of providers at site | ||
| 1 | 49 | 15 |
| 2 | 19 | 13 |
| 3–5 | 21 | 27 |
| 6–10 | 8 | 20 |
| 11 or more | 4 | 26 |
| Site is part of multi-site group practice | ||
| No | 85 | 73 |
| Yes, 10 or fewer providers in group | 3 | 3 |
| Yes, >10 providers in group | 12 | 25 |
| Providers at site | ||
| Physicians only | 73 | 50 |
| Physicians and NPs or PAs | 26 | 50 |
| NPs or PAs only | 1 | 0.3 |
| Provider specialty mix at site | ||
| Specialist providers only | 54 | 48 |
| Primary care providers only | 40 | 34 |
| Mixed primary care and specialists | 6 | 18 |
| Site is owned by a hospital | ||
| No | 86 | 76 |
| Yes | 14 | 24 |
| Site is affiliated with a health system | ||
| No | 88 | 77 |
| Yes | 12 | 23 |
| Any electronic health record with e-Rx capability | 30 | 43 |
| Priority Population Characteristics of PUMA | PUMAs (N = 2,068) | Sites (N = 261,973) |
|---|---|---|
| Share of the population that is minority | ||
| Average | 35 | 36 |
| 75th percentile | 51 | 51 |
| Share of the population that is low income | ||
| Average | 33 | 32 |
| 75th percentile | 41 | 40 |
| Metropolitan status | ||
| Large central metropolitan | 30 | 34 |
| Large fringe metropolitan | 24 | 25 |
| Medium or small metropolitan | 29 | 29 |
| Non-metropolitan | 17 | 12 |
In 2011, 30 percent of ambulatory health care sites used an EHR with e-prescribing functionality, accounting for 43 percent of providers (Table 1).2
These health care sites were situated across the 2,068 PUMAs in the United States (bottom panel of Table 1). In the average PUMA, 35 percent of the population was a racial or ethnic minority and 33 percent of the population was low income. In one-quarter of PUMAs, over half of the population was a racial or ethnic minority and over 41 percent of the population was low income. Over half of PUMAs were part of large metropolitan areas with a population of at least 1 million. Another 29 percent of PUMAs were in medium/small metropolitan areas and the remaining 17 percent of PUMAs were in nonmetropolitan areas.
Variation in Local Area EHR Adoption Rates
Looking first at local area EHR adoption rates prior to adjustment for site characteristics, we found substantial variation in local area EHR adoption rates nationally, between states, and within states. Nationally, local area EHR adoption rates ranged from 8 to 88 percent, with a median of 41 percent and an interquartile range of 32–50 percent (Figure 1). At the state level, the median local area EHR adoption rate ranged from a low of 27 percent in New Jersey to a high of 65 percent in Minnesota (Figure 2). Within states, the range in local area EHR adoption rates was at least 20 percentage points in nearly all states (46) and was at least 50 percentage points in a third of states (17). California, Illinois, and Missouri had the largest ranges, while Delaware, the District of Columbia, and Wyoming had the smallest ranges.
Figure 1.
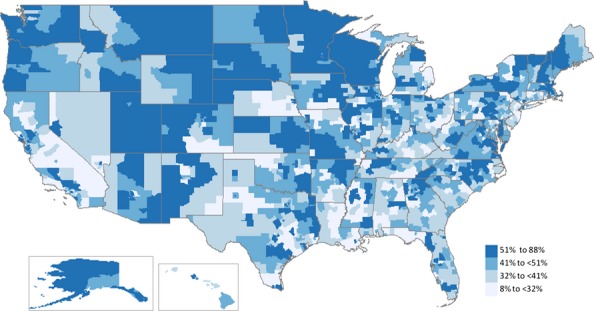
Local Area Electronic Health Record (EHR) Adoption Rates Unadjusted for Site Characteristics
Note. Local area EHR adoption rates are the share of ambulatory physicians, physician assistants, and nurse practitioners in the Public Use Microdata Area (PUMA) (n = 2,068) with an EHR with e-prescribing functionality. Rates were calculated as the average predicted probability of EHR adoption across all providers in the PUMA based on a multilevel linear probability model including PUMA random effects and no covariates.
Figure 2.
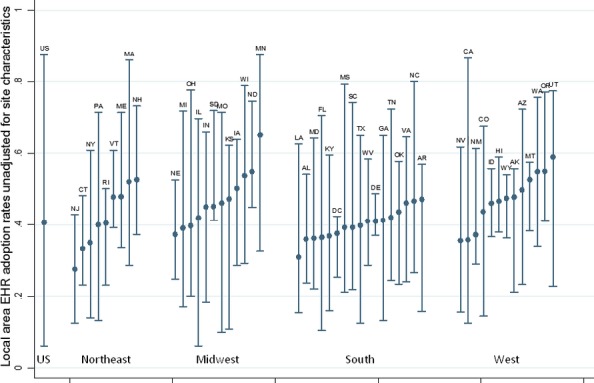
Ranges in Local Area Electronic Health Record (EHR) Adoption Rates, U.S. Overall and by State
Note. Bars represent ranges and dots represent medians of local area EHR adoption rates within each state. Local area EHR adoption rates are the share of ambulatory physicians, physician assistants, and nurse practitioners in the Public Use Microdata Area (PUMA) (n = 2,068) with an EHR with e-prescribing functionality. Rates were calculated as the average predicted probability of EHR adoption across all providers in the PUMA based on a multilevel linear probability model including PUMA random effects and no covariates.
Compared with the nation overall, local area EHR adoption was slightly lower in some areas with high concentrations of priority populations (Figure 3). The median local area EHR adoption rate was 36 percent in areas with high concentrations of minority population and 38 percent in areas with high concentrations of low-income population compared with 41 percent overall. Relative to medium/small metropolitan areas and nonmetropolitan areas, which had median local area EHR adoption rates of 43 percent, the median rate was lower in large metropolitan areas (38 percent in large-central metropolitan areas and 39 percent in large-fringe metropolitan areas). Areas with high concentrations of minority and low-income populations and large metropolitan areas were also more likely than average to be in the lowest quartile of EHR adoption nationally. At the same time, we found substantial variation in local area EHR adoption rates across all types of areas; areas with both relatively high and relatively low-EHR adoption rates were heterogeneous in terms of minority population, low-income population, and metropolitan status.
Figure 3.
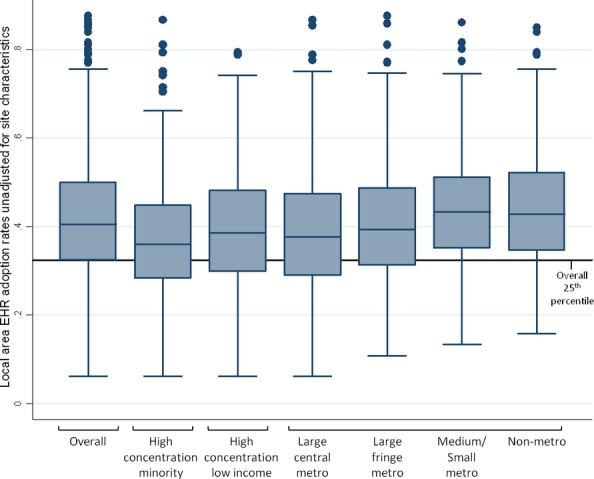
Distribution of Local Area Electronic Health Record (EHR) Adoption Rates by Priority Population Characteristics
Note. Boxes represent inter-quartile ranges (25th to 75th percentile), horizontal lines inside boxes represent medians, vertical lines extending from boxes represent the range of values within 1.5 times the inter-quartile range, and dots represent values outside 1.5 times the inter-quartile range. Local area EHR adoption rates are the share of ambulatory physicians, physician assistants, and nurse practitioners in the Public Use Microdata Area (PUMA) (n = 2,068) with an EHR with e-prescribing functionality. Rates were calculated as the average predicted probability of EHR adoption across all providers in the PUMA based on a multilevel linear probability model including PUMA random effects and no covariates.
At the national level, many of these patterns persisted in multivariate analyses that considered all priority area characteristics simultaneously (left-hand panel of Table 2). Compared with other areas, the probability of being in the lowest adoption quartile was 12 percentage points higher for areas with high concentrations of minority population. Compared with large fringe metropolitan areas, medium/small metropolitan areas and nonmetropolitan areas were less likely to be in the lowest adoption quartile (by 12 and 10 percentage points, respectively), and there was no difference between large central metropolitan areas and large fringe metropolitan areas. However, there was not an overall association between concentration of low-income population and local area EHR adoption after controlling for other factors.
Table 2.
Incremental Effects from Logistic Regression of Likelihood of Being a Low Electronic Health Record (EHR) Adoption Area
| EHR Adoption Rate Unadjusted for Site Characteristics | Probability of Adoption for the Average Provider's Site | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| US | Northeast | Midwest | South | West | US | Northeast | Midwest | South | West | |
| Area has high concentration of minority population | ||||||||||
| No | —† | —† | —† | —† | —† | —† | —† | —† | —† | —† |
| Yes | 0.12*** | 0.019** | 0.06 | 0.00 | 0.21*** | 0.08** | 0.16* | 0.11 | 0.05 | 0.14** |
| Area has high concentration of low-income population | ||||||||||
| No | —† | —† | —† | —† | —† | —† | —† | —† | —† | —† |
| Yes | 0.03 | −0.05 | 0.19** | 0.03 | 0.05 | 0.08** | −0.01 | 0.21** | 0.09 | 0.07 |
| Metropolitan status | ||||||||||
| Large central metropolitan | −0.01 | −0.09 | 0.06 | 0.03 | 0.14* | 0.01 | −0.03 | 0.05 | −0.01 | 0.15** |
| Large fringe metropolitan | —† | —† | —† | —† | —† | —† | —† | —† | —† | —† |
| Medium or small metropolitan | −0.12*** | −0.28*** | −0.04 | −0.07 | 0.04 | −0.08** | −0.14* | 0.02 | −0.09 | 0.03 |
| Non-metropolitan | −0.10** | −0.26*** | 0.05 | −0.04 | −0.07 | −0.13*** | −0.22** | 0.01 | −.011* | −0.10 |
| Cutoff for lowest quartile, % | 32 | 29 | 35 | 33 | 33 | 32 | 30 | 33 | 33 | 32 |
| N | 2,068 | 405 | 469 | 735 | 459 | 2,068 | 405 | 469 | 735 | 459 |
| Test for metropolitan status (χ2) | 28.6*** | 36.1*** | 4.5 | 5.1 | 16.9*** | 30.7*** | 14.8** | 0.7 | 6.5 | 26.3*** |
Note. Incremental effects are the percentage point differences in the likelihood of being a low-adoption area for the area type relative to the reference category based on logistic regression coefficient estimates. Results for the United States are based on a national model with dependent and independent variables defined based on national distributions of EHR adoption and minority and low-income population concentration. Region-specific results are based on a model with dependent and independent variables defined based on regional distributions and including interactions between region and the independent variables reported in the table.
Marginal effect estimate statistically different from zero at ***p < .001, **p < .01, *p < .05 based on standard errors obtained by the delta method.
Reference category.
These relationships between local area EHR adoption and population characteristics varied regionally. The associations between minority population and EHR adoption were strongest in the Northeast and West, where areas with high concentrations of minority population were 19 to 21 percentage points more likely to have relatively low adoption. There were no statistically significant differences by minority population concentration in the Midwest or South. However, in contrast to the nation overall, there were disparities by low-income population in the Midwest, where areas with high concentrations of low-income population were 19 percentage points more likely to be low-adoption areas. The association between metropolitan status and local area EHR adoption was strongest in the Northeast and West. In the Northeast, large fringe and large central metropolitan areas lagged behind: medium/small metropolitan areas and nonmetropolitan were significantly less likely to be low-adoption areas compared with large metropolitan areas. In the West, large central metropolitan areas were 14 percentage points more likely to have relatively low-EHR adoption compared with large fringe metropolitan areas; there was no statistically significant difference between large fringe metropolitan areas and medium/small metropolitan or nonmetropolitan areas in the West.
These patterns persisted after controlling for site characteristics (right-hand panel of Table 2). Across all areas, the predicted probability for the average provider's site (calculated at the mean of site characteristics weighted by the number of providers) was 36 percent and the lowest quartile of areas had predicted probabilities below 32 percent.
The relationships between local area EHR adoption and priority population characteristics using this adjusted outcome variable were similar to those based on the unadjusted outcome variable. Differences according to minority population persisted in the United States overall and in the Northeast and West but were slightly smaller in magnitude. One notable difference was a statistically significant association between low-income population concentration and adoption in the nation overall, which appeared primarily to be driven by differences in the Midwest. Large metropolitan areas continued to lag behind medium/small metropolitan and nonmetropolitan areas in the nation overall and in the Northeast, although differences were attenuated. The disparity between large central metropolitan areas and large fringe metropolitan areas in the West also persisted after adjusting for site characteristics. These patterns persisted after including other local area characteristics as additional controls (results available upon request).
Variation in EHR Adoption by Site Characteristics
The likelihood that a health care site had adopted an EHR with e-prescribing functionality varied significantly according to site characteristics (Table SA1). There was a strong positive association between EHR adoption and the number of providers at the site. Sites that were part of a multi-site group practice were more likely to have adopted an EHR, independent of the number of providers at the site. Sites with primary care providers and sites with a mix of physicians and nurse practitioners or physician assistants had higher adoption relative to sites with specialist providers only and sites with physicians only, respectively. Hospital ownership and health system affiliation were also associated with greater likelihood of EHR adoption.
Discussion
We found substantial geographic variation in local area EHR adoption rates. These variations point to important opportunities for increased adoption of EHRs. In one-quarter of local areas, less than a third of ambulatory physicians, nurse practitioners, and physician assistants were in sites with an EHR with at least e-prescribing functionality. Moreover, areas where some traditionally underserved populations live were disproportionately likely to have relatively low-adoption rates, including large metropolitan areas, areas with high concentrations of minority population, and areas with high concentrations of low-income population.
Our results suggest that concerns about equitable access to EHRs are warranted. Consistent with studies of other national data sources, we found that some states had relatively high median EHR adoption rates in 2011 (Hsiao et al. 2011). However, our results further show that EHR adoption was lagging in some local areas within nearly all states, indicating that areas nationwide could benefit from efforts to accelerate EHR diffusion. To ensure that EHR use increases across all areas and that baseline disparities are not exacerbated, it may be particularly important to target resources to areas with high concentrations of minority population in the Northeast and West, areas with high concentrations of low-income population in the Midwest, large metropolitan areas in the Northeast, and large central metropolitan areas in the West.
Our results also show that some local areas have achieved substantially higher adoption rates—one quarter of local areas had adoption rates of at least 50 percent—and that both the highest and lowest EHR adoption quartiles include areas with diverse characteristics. This suggests there are opportunities for communities with low-adoption rates to learn from communities with similar characteristics that have achieved higher adoption rates. We also found that nonmetropolitan and medium/small metropolitan areas had higher rates of EHR adoption than large metropolitan areas. While unexpected based on traditional disparities experienced by rural populations (Agency for Healthcare Research and Quality 2010), this finding is consistent with other data sources showing that in recent years physician EHR adoption has increased faster in nonmetropolitan areas than metropolitan areas in the nation as a whole (Decker, Jamoom, and Sisk 2012). This trend may partly reflect early impacts of the Office of the National Coordinator for Health Information Technology (ONC) Regional Extension Centers, many of which are targeting their services toward rural and health professional shortage areas (Samuel et al. 2013).
Our results may be useful to numerous initiatives under way to advance EHR adoption in underserved communities. The ONC Regional Extension Centers program is providing technical assistance and implementation support to providers across the country, prioritizing assistance to primary care providers in small practices and underserved settings (Maxson et al. 2010). The Health Services and Resources Administration is supporting EHR adoption in community health centers, which are important safety net providers of care for traditionally underserved populations (Health Resources and Services Administration 2012). Our study can point these programs and others like them toward more and less successful examples of EHR adoption across otherwise similar areas.
Our study contributes to the literature in several ways. We used new and comprehensive site-level data to document small area variation in adoption of EHR technology within all 50 states, a level and scope of analysis that had not been possible previously due to data limitations. Our study at the area level builds upon prior studies at the provider level that examined differences in EHR adoption by patient panel characteristics. Both provider-level and area-level studies provide important insights into potential disparities in access to the benefits of health IT. Provider-level studies can assess technology adoption by practitioners who are caring for traditionally underserved patients, while area-level studies can add information about health IT diffusion in places where traditionally underserved populations live. Living in a location does not guarantee access to the providers who practice there; nonetheless, this area-level perspective on EHR adoption and use is important, especially given the potential for health IT to enable improved public health monitoring and population health management which may benefit individuals beyond those who have made an office visit during a certain period of time (Friedman 2006; Diamond, Mostashari, and Shirky 2009; Buck et al. 2012).
Our study has some important limitations. First, although SK&A is timely and comprehensive, the data are self-reported and may be subject to measurement error. Second, the adoption patterns for EHRs with e-prescribing functionality could differ from those of more robust EHR systems. Finally, it is possible that the patterns observed here could shift in the near term given the rapid growth in EHR adoption and changes in health care markets.
This analysis presents a baseline estimate of local area variation in ambulatory EHR adoption. It will be important to track changes over time as the rapid diffusion of EHR technology continues over the next several years. Future research should examine the factors driving variation in EHR adoption in underserved areas, and whether financial incentives or technical assistance programs can address these disparities.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The views represented in this paper are those of the authors and are not necessarily those of the Office of the National Coordinator for Health Information Technology or the Congressional Budget Office.
Disclosures: None.
Disclaimers: None.
Notes
The number of ambulatory physicians in the SK&A database compares favorably to estimates of active office-based providers derived from other sources. For example, estimates of the number of office-based primary care physicians in 2010 based on the American Medical Association Masterfile ranged from 205,000 (Iglehart 2011) to 208,800 (Agency for Healthcare Research and Quality 2011). These estimates consider primary care to include general or family practice, pediatrics, internal medicine, and geriatrics. The SK&A database contained 202,900 physicians with these specialties in 2011 (99 percent of the 205,000 estimate and 97 percent of the 208,800 estimate).
This estimate is very similar to the estimates derived from authors’ analysis of two other national data sources. First, analysis of 2011 survey data from the National Ambulatory Medical Care Survey Electronic Medical Record Supplement found that 45 percent of office-based physicians reported having any EHR and having computerized capability to submit prescriptions electronically. Second, we analyzed transactional data from SureScripts, the largest e-prescribing network in the United States. In December 2011, approximately 305,900 physicians, nurse practitioners, and physician assistants used an EHR to transmit at least one prescription electronically on the SureScripts network. In the SK&A database, approximately 307,000 physicians, nurse practitioners, and physician assistants practiced in offices using an EHR with e-prescribing functionality. Both the SureScripts and SK&A counts yield an estimate that 43 percent of providers used an EHR with e-prescribing functionality in the nation overall. We also calculated counts of providers using an EHR with e-prescribing functionality at the state and PUMA levels; the SK&A and Surescripts counts were highly correlated at both the state (0.98) and PUMA (0.86) levels.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Linear Probability Regression of EHR Adoption among U.S. Ambulatory Health Care Sites.
Appendix SA2: Author Matrix.
References
- Abdolrasulnia M, Menachemi N, Shewchuk RM, Ginter PM, Duncan WJ, Brooks RG. “Market Effects on Electronic Health Record Adoption by Physicians”. Health Care Management Review. 2008;33(3):243–52. doi: 10.1097/01.HMR.0000324904.19272.c2. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. 2010. “2010 National Healthcare Disparities Report” [accessed on June 19, 2012]. Available at http://www.ahrq.gov/qual/nhdr10/nhdr10.pdf. [DOI] [PubMed]
- Agency for Healthcare Research and Quality. 2011. “Primary Care Workforce Facts and Stats No. 1: The Number of Practicing Primary Care Physicians in the United States” [accessed on June 19, 2012]. Available at http://www.ahrq.gov/research/pcwork1.htm. [DOI] [PubMed]
- Baicker K, Chandra A, Skinner JS, Wennberg JE. “Who You Are and Where You Live: How Race and Geography Affect the Treatment of Medicare Beneficiaries”. Health Affairs. 2004;(Suppl Variation):VAR33–44. doi: 10.1377/hlthaff.var.33. [DOI] [PubMed] [Google Scholar]
- Baier R, Voss R, Morphis B, Viner-Brown S, Gardner R. “Rhode Island Physicians’ Health Information Technology (HIT) Use, 2009–2011”. Medicine & Health/Rhode Island. 2011;94(7):215–7. [PubMed] [Google Scholar]
- Bazemore A, Burke M, Xierali I, Petterson S, Rinaldo J, Green LA, Puffer J. “Establishing a Baseline: Health Information Technology Adoption among Family Medicine Diplomates”. Journal of the American Board of Family Medicine. 2011;24(2):132. doi: 10.3122/jabfm.2011.02.110010. [DOI] [PubMed] [Google Scholar]
- Bell DS, Daly DM, Robinson P. “Is There a Digital Divide among Physicians? A Geographic Analysis of Information Technology in Southern California Physician Offices”. Journal of the American Medical Informatics Association. 2003;10(5):484–93. doi: 10.1197/jamia.M1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal D, DesRoches C, Donelan K, Ferris TG, Jha AK, Kaushal R, Sowmya R, Rosenbaum S, Shields A. Health Information Technology in the United States: The Information Base for Progress. Princeton, NJ: Robert Wood Johnson Foundation; 2006. [Google Scholar]
- Bramble JD, Galt KA, Siracuse MV, Abbott AA, Drincic A, Paschal KA, Fuji KT. “The Relationship between Physician Practice Characteristics and Physician Adoption of Electronic Health Records”. Health Care Management Review. 2010;35(1):55–64. doi: 10.1097/HMR.0b013e3181c3f9ad. [DOI] [PubMed] [Google Scholar]
- Buck MD, Anane S, Taverna J, Amirfar S, Stubbs-Dame R, Singer J. “The Hub Population Health System: Distributed Ad Hoc Queries and Alerts”. Journal of the American Medical Informatics Association. 2012;19(e1):e46–50. doi: 10.1136/amiajnl-2011-000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. “The Benefits of Health Information Technology: A Review of the Recent Literature Shows Predominantly Positive Results”. Health Affairs. 2011;30(3):464–71. doi: 10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. “Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care”. Annals of Internal Medicine. 2006;144(10):742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- Chiang MF, Boland MV, Margolis JW, Lum F, Abramoff MD, Hildebrand PL. “Adoption and Perceptions of Electronic Health Record Systems by Ophthalmologists: An American Academy of Ophthalmology Survey”. Opthalmology. 2008;115(9):1591–7. doi: 10.1016/j.ophtha.2008.03.024. [DOI] [PubMed] [Google Scholar]
- Decker SL, Jamoom EW, Sisk JE. “Physicians in Nonprimary Care and Small Practices and Those Age 55 and Older Lag in Adopting Electronic Health Record Systems”. Health Affairs. 2012;31(5):1108–14. doi: 10.1377/hlthaff.2011.1121. [DOI] [PubMed] [Google Scholar]
- Dennehy P, White MP, Hamilton AH, Pohl JM, Tanner C, Onifade TJ, Zheng K. “A Partnership Model for Implementing Electronic Health Records in Resource-Limited Primary Care Settings: Experiences from Two Nurse-Managed Health Centers”. Journal of the American Medical Informatics Association. 2011;18(6):820–6. doi: 10.1136/amiajnl-2011-000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, Jha A, Kaushal R, Levy DE, Rosenbaum S, Shields AE, Blumenthal D. “Electronic Health Records in Ambulatory Care–A National Survey of Physicians”. New England Journal of Medicine. 2008;359(1):50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- Diamond CC, Mostashari F, Shirky C. “Collecting and Sharing Data for Population Health: A New Paradigm”. Health Affairs. 2009;28(2):454–66. doi: 10.1377/hlthaff.28.2.454. [DOI] [PubMed] [Google Scholar]
- Ferris TG, Kuhlthau K, Ausiello J, Perrin J, Kahn R. “‘Are Minority Children the Last to Benefit from a New Technology?’ Technology Diffusion and Inhaled Corticosteriods for Asthma”. Medical Care. 2006;44(1):81–6. doi: 10.1097/01.mlr.0000188914.47033.cd. [DOI] [PubMed] [Google Scholar]
- Friedman DJ. “Assessing the Potential of National Strategies for Electronic Health Records for Population Health Monitoring and Research, National Center for Health Statistics”. Vital and Health Statistics. 2006;2(143) [PubMed] [Google Scholar]
- Gibbons MC. “Use of Health Information Technology among Racial and Ethnic Underserved Communities”. Perspectives in Health Information Management. 2011;8:1–13. [PMC free article] [PubMed] [Google Scholar]
- Goldzweig CL, Towfigh A, Maglione M, Shekelle PG. “Costs and Benefits of Health Information Technology: New Trends from the Literature”. Health Affairs. 2009;28(2):w282–93. doi: 10.1377/hlthaff.28.2.w282. [DOI] [PubMed] [Google Scholar]
- Gresenz CR, Ruder T, Lurie N. 2009. “Ambulatory Care Sensitive Hospitalizations and Emergency Department Visits in Baltimore City” [accessed June 19, 2012]. RAND Technical Report. Available at http://www.rand.org/pubs/technical_reports/TR671.html.
- Grossman JM, Reed MC. 2006. “Clinical Information Technology Gaps Persist among Physicians” [accessed on June 19, 2012]. Available at http://www.hschange.com/CONTENT/891/891.pdf.
- Health Resources and Services Administration. 2012. “What Is a Health Center Controlled Network” [accessed June 29, 2012]. Available at http://www.hrsa.gov/healthit/toolbox/HealthITAdoptiontoolbox/OpportunitiesCollaboration/abouthccns.html.
- Hing E, Burt CW. “Are There Patient Disparities When Electronic Health Records Are Adopted?”. Journal of Health Care for the Poor and Underserved. 2009;20(2):473–88. doi: 10.1353/hpu.0.0143. [DOI] [PubMed] [Google Scholar]
- Hsiao CJ, Hing E, Socey TC, Cai B. Electronic Health Record Systems and Intent to Apply for Meaningful Use Incentives among Office-Based Physician Practices: United States, 2001-2011. Hyattsville, MD: National Center for Health Statistics; 2011. NCHS Data Brief, no 79. [PubMed] [Google Scholar]
- Hsiao CJ, Decker SL, Hing E, Sisk JE. “Most Physicians Were Eligible for Federal Incentives in 2011, but Few had EHR Systems That Met Meaningful-Use Criteria”. Health Affairs. 2012;31(5):1100–7. doi: 10.1377/hlthaff.2011.1315. [DOI] [PubMed] [Google Scholar]
- Iglehart JK. “The Uncertain Future of Medicare and Graduate Medical Education”. New England Journal of Medicine. 2011;365(14):1340–5. doi: 10.1056/NEJMhpr1107519. [DOI] [PubMed] [Google Scholar]
- Ingram DD, Franco SJ. “NCHS Urban-Rural Classification Scheme for Counties. National Center for Health Statistics”. Vital and Health Statistics. 2012;2(154) [PubMed] [Google Scholar]
- Jha AK, Bates DW, Jenter C, Orav EJ, Zheng J, Cleary P, Simon SR. “Electronic Health Records: Use, Barriers and Satisfaction among Physicians who Care for Black and Hispanic Patients”. Journal of Evaluation in Clinical Practice. 2009;15(1):158–63. doi: 10.1111/j.1365-2753.2008.00975.x. [DOI] [PubMed] [Google Scholar]
- Karaca-Mandic P, Norton EC, Dowd B. “Interaction Terms in Nonlinear Models”. Health Services Research. 2012;47(1 Pt 1):255–74. doi: 10.1111/j.1475-6773.2011.01314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemper AR, Uren RL, Clark SJ. “Adoption of Electronic Health Records in Primary Care Pediatric Practices”. Pediatrics. 2006;118(1):e20–4. doi: 10.1542/peds.2005-3000. [DOI] [PubMed] [Google Scholar]
- Kenney GM, Lynch V, Cook A, Phong S. “Who and Where Are the Children yet to Enroll in Medicaid and the Children's Health Insurance Program?”. Health Affairs. 2010;29(10):1920–9. doi: 10.1377/hlthaff.2010.0747. [DOI] [PubMed] [Google Scholar]
- Li C, West-Strum D. “Patient Panel of Underserved Populations and Adoption of Electronic Medical Record Systems by Office-Based Physicians”. Health Services Research. 2010;45(4):963–84. doi: 10.1111/j.1475-6773.2010.01113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N, Martin LT, Ruder T, Escarce JJ, Ghosh-Dastidar B, Sherman D, Bird CE, Freemont A. 2009. “Estimating and Mapping Health Literacy in the State of Missouri” [accessed June 19, 2012]. RAND Health Working Paper. Available at http://www.rand.org/pubs/working_papers/WR735.html. [DOI] [PMC free article] [PubMed]
- Maxson ER, Buntin MB, Mostashari F. “Using Electronic Prescribing Transaction Data to Estimate Electronic Health Record Adoption”. American Journal of Managed Care. 2010;16:e320–6. [PubMed] [Google Scholar]
- Maxson ES, Jain M, Kendall F, Blumenthal D. “The Regional Extension Center Program: Helping Physicians Meaningfully Use Health Information Technology”. Annals of Internal Medicine. 2010;153(10):666–70. doi: 10.7326/0003-4819-153-10-201011160-00011. [DOI] [PubMed] [Google Scholar]
- Menachemi N, Yeager VA, Bilello L, Harle CA, Sullivan CB, Siler-Marsiglio KI. “Florida Doctors Seeing Medicaid Patients Show Broad Interest in Federal Incentives for Adopting Electronic Health Records”. Health Affairs. 2011;30(8):1461–70. doi: 10.1377/hlthaff.2011.0261. [DOI] [PubMed] [Google Scholar]
- Menachemi N, Mazurenko O, Kazley AS, Diana ML, Ford EW. “Market Factors and Electronic Medical Record Adoption in Medical Practices”. Health Care Management Review. 2012;37(1):14–22. doi: 10.1097/HMR.0b013e3182352562. [DOI] [PubMed] [Google Scholar]
- Miller RH, West CE. “The Value of Electronic Health Records in Community Health Centers: Policy Implications”. Health Affairs. 2007;26(1):206–14. doi: 10.1377/hlthaff.26.1.206. [DOI] [PubMed] [Google Scholar]
- Miller RH, D'Amato K, Oliva N, West CE, Adelson JW. “California's Digital Divide: Clinical Information Systems for the Haves and Have-Nots”. Health Affairs. 2009;28(2):505–16. doi: 10.1377/hlthaff.28.2.505. [DOI] [PubMed] [Google Scholar]
- Office of the National Coordinator for Health Information Technology. 2011. “Federal Health Information Technology Strategic Plan, 2011–2015” [accessed on June 19, 2012]. Available at http://healthit.hhs.gov/portal/server.pt?open=512&objID=1211&parentname=CommunityPage&parentid=2&mode=2.
- Patel V, Jamoom EW, Hsiao CJ, Furukawa MF, Buntin MB. “Variation in Electronic Health Record Adoption and Readiness for Meaningful Use: 2008 to 2011. Journal of General Internal Medicine. 2013 doi: 10.1007/s11606-012-2324-x. published online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. College Station, TX: Stata Press; 2005. [Google Scholar]
- Robinson JC, Casalino LP, Gilles RR, Rittenhouse DR, Shortell SS, Fernandes-Taylor S. “Financial Incentives, Quality Improvement Programs, and the Adoption of Clinical Information Technology”. Medical Care. 2009;47(4):411–7. doi: 10.1097/MLR.0b013e31818d7746. [DOI] [PubMed] [Google Scholar]
- Rosenthal DA, Layman EJ. “Utilization of Information Technology in Eastern North Carolina Physician Practices: Determining the Existence of a Digital Divide”. Perspectives in Health Information Management. 2008;5(3):1–20. [PMC free article] [PubMed] [Google Scholar]
- Samuel CA, King J, Adetosoye FA, Samy L, Furukawa MF. “Engaging Providers in Underserved Areas to Adopt Electronic Health Records”. American Journal of Managed Care. 2013;19(3):229–34. [PubMed] [Google Scholar]
- Shields AE, Shin P, Leu MG, Levy DE, Betancourt RM, Hawkins D, Proser M. “Adoption of Health Information Technology in Community Health Centers: Results of a National Survey”. Health Affairs. 2007;26(5):1373–83. doi: 10.1377/hlthaff.26.5.1373. [DOI] [PubMed] [Google Scholar]
- Simon SR, Kaushal R, Cleary PD, Jenter CA, Volk LA, Poon EG, Orav EJ, Lo HG, Williams DH, Bates DW. “Correlates of Electronic Health Record Adoption in Office Practices: A Statewide Survey”. Journal of the American Medical Informatics Association. 2007;14(1):110–7. doi: 10.1197/jamia.M2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R, Lichter MI, Danzo A, Taylor J, Rosenthal T. “The Adoption and Use of Health Information Technology in Rural Areas: Results of a National Survey”. Journal of Rural Health. 2011;28:16–27. doi: 10.1111/j.1748-0361.2011.00370.x. [DOI] [PubMed] [Google Scholar]
- Skinner J, Weinstein JN, Sporer SM, Wennberg JE. “Racial, Ethnic, and Geographic Disparities in Rates of Knee Arthroplasty among Medicare Patients”. New England Journal of Medicine. 2003;349(14):1350–9. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Stream GR. “Trends in Adoption of Electronic Health Records by Family Physicians in Washington State”. Informatics in Primary Care. 2009;17:145–52. doi: 10.14236/jhi.v17i3.729. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. A Compass for Understanding and Using American Community Survey Data: What PUMS Data Users Need to Know. Washington, DC: U.S. Government Printing Office; 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


