Abstract
Objective. To examine whether expanding coverage for the nonelderly affects primary care utilization among Medicare beneficiaries.
Data Source. Zip code–level files from Dartmouth Atlas for Massachusetts and surrounding states, including Medicare utilization for 2005 (pre expansion) and 2007 (post expansion), and health insurance coverage for 2005.
Study Design. We use two zip code–level outcomes: arc percent change in primary care visits per Medicare beneficiary per year, and percentage point change in the share of beneficiaries with one or more primary care visits. We use a regression-based difference-in-difference analysis that compares Massachusetts with surrounding states, and zip codes with high, medium, and low uninsurance rates in 2005. The 2005 uninsurance rates correspond to the size of Massachusetts' coverage expansion. We use propensity scores for identification of comparable zip codes and for weighting.
Principal Findings. In areas of Massachusetts with the highest uninsurance rates—where insurance expansion had the largest impact—visits per beneficiary fell 6.9 percent (p < .001) relative to areas of Massachusetts with the smallest uninsurance rates.
Conclusions. The expansion of coverage for the nonelderly reduced primary care visits, but it did not reduce the percent of beneficiaries with at least one visit. These results could imply restricted access, increased efficiency, or some blend.
Keywords: Medicare, health insurance expansion, primary care
During the debate in 2009–2010 over the Affordable Care Act (ACA), one major concern was its potential negative impact on currently insured individuals. The coverage expansion might, critics argued, force people out of coverage they were happy with or otherwise reduce their access to care. The Massachusetts health reform enacted in 2006 is an important case study that gives us insight into what to expect from the ACA.
A large body of research has shown that the Massachusetts reform clearly decreased uninsurance and increased various measures of access and affordability (Long, Stockley, and Dahlen 2012). But little is known about its effects on the continuously insured.
Newly insured patients will seek physician services. There are four ways that increase inpatient demand could be accommodated: physicians could work longer hours, physicians could provide more visits per hour worked, additional providers such as nurse practitioners and physician assistants could see more patients, or physicians could reduce the number of visits they provide to continuously insured patients. This article looks specifically at the Medicare population and their trends in primary care utilization. Based on anecdotal reports in 2007, some individuals faced difficulties getting appointments with physicians following the Massachusetts coverage expansion, allegedly due to the influx of newly insured individuals (Massachusetts Medical Society 2010). Medicare beneficiaries, even though their coverage remained constant, might have reduced their utilization of physician services.
Our empirical approach is to compare Massachusetts with surrounding states, and to compare areas within the state where there was a large insurance expansion to areas where the expansion was small. This enables us to ask the question of whether beneficiaries in areas largely affected by the insurance expansion were differentially impacted by reform relative to those in less affected areas.
Massachusetts is well recognized as having a high number of physicians per capita and high levels of insurance prior to reform. One empirical concern is that trends in Massachusetts are, therefore, not comparable to trends in other states. Our approach uses propensity scores to limit the analysis to zip codes that are comparable and to weight those zip codes to make them even more comparable to Massachusetts. The addition of propensity score weighting is an attempt to account for and mitigate the differences between Massachusetts and the surrounding states.
Massachusetts Health Reform and Its Parallels to National Health Reform
With its 2006 landmark health reform law, Massachusetts took enormous strides toward nearly universal health insurance coverage. Between 2006 and 2009, the state uninsurance rate for nonelderly adults dropped from 13.4 percent to 5.8 percent through many of the same legislative components included in national health reform (Long, Stockley, and Nordahl 2012/2013). Both pieces of legislation contain a Medicaid expansion and the creation of a health insurance exchange for both the near poor who receive subsidies and those in the small or individual group market who are unsubsidized. In addition, both reforms include an individual mandate and employer penalty to encourage higher participation rates.
Previous Work
Numerous studies have explored the effects of Massachusetts health reform on health care access and affordability. In particular, the Urban Institute has published many reports on their biannual Massachusetts Health Reform Survey, which samples the nonelderly. From 2006 to 2010 the percent of the population with a usual source of care increased by 4.7 percentage points, and the percent of the population with a preventative health visit increased by 5.9 percentage points (Long, Stockley, and Nordahl 2012/2013). The percentage of the population with visits to specialists, multiple physicians, and dentists also increased (Long, Stockley, and Dahlen 2012). The most recent survey also demonstrated decreases in emergency department utilization and in hospital stays.
A number of more robust differences-in-difference studies support many of Urban Institute's findings on changes to access and utilization relative to neighboring states. A study by Miller (2012/2013) used the National Health Interview Survey to look directly at office visits, which suggests an increase of 4% in office visits for those aged 18–64 years in Massachusetts relative to surrounding states. Using the Healthcare Cost and Utilization Project National Inpatient Sample, Kolstad and Kowalski (2012) reported a decreased length of stay and decreased admissions originating from the Emergency Department (ED) in Massachusetts after reform. Their results also suggest that there was little change in the rate of preventable hospitalizations, but that the severity of patients with preventable hospitalizations decreased. Another study by Miller (2012) using administrative data looking directly at ED visits found a 2.4 percentage point decrease in Massachusetts. A number of these results may indicate increased primary care access with patients on average able to access care at an earlier stage.
The one known study looking directly at Medicare beneficiaries uses preventable hospital admissions as a proxy for access to preventative primary care visits and finds no detrimental effect of the insurance expansion on the Medicare population (Joynt et al. 2013). The results indicate that preventable hospital admissions declined more in Massachusetts than in surrounding states. In addition, this article briefly notes that areas in Massachusetts with a larger insurance expansion had a smaller decrease in preventable hospitalizations than other areas in Massachusetts. The authors interpret their findings as evidence that Medicare beneficiaries did not face problems accessing primary care. Their findings could be due, however, to Medicare beneficiaries facing reduced access to hospital care due to congestion caused by the newly insured. Our article will more directly address this topic by measuring primary care utilization.
Methods
Identification Strategy
This study takes advantage of the Massachusetts state-level policy change—its 2006 health reform—that greatly increased health insurance coverage. Unlike other nearby states, Massachusetts had a consistent and large increase in insurance levels across the state.
One possible identification strategy would be to compare state-level changes in Massachusetts with state-level changes in surrounding states. However, Massachusetts is unique in many respects and simply using surrounding states may not be an adequate comparison group. Prior to reform, Massachusetts had one of the highest rates of insurance coverage, higher than all of the New England states except for New Hampshire (Levy 2012/2013). Massachusetts is also unusual in its physician supply, particularly specialists. Relative to surrounding states, Massachusetts also has high levels of income and education (Levy 2012/2013).
We explore state-level trends in spending per beneficiary in physician and clinical services from the State Health Expenditures (see Figure 1). Massachusetts is compared to the national average as well as the average of surrounding states—Connecticut, Maine, New Hampshire, New Jersey, New York, Rhode Island, and Vermont. Comparing each year's spending per beneficiary to its 2005 spending level demonstrates that prior to reform, only a small variation in spending growth existed. However, the spending in Massachusetts grew at a faster rate in 2006 and 2007 than the national average and the average of surrounding states. Since the increase in Massachusetts occurred the year of health reform enactment, it is not clear whether the growth is linked to health reform or caused by a factor outside of health reform. If growth was associated with primary care, then we would expect to see an increase in primary care visits. Unfortunately, these data do not differentiate care provided by specialists from primary care physicians, so it is not possible to determine what is driving the faster growth.
Figure 1.
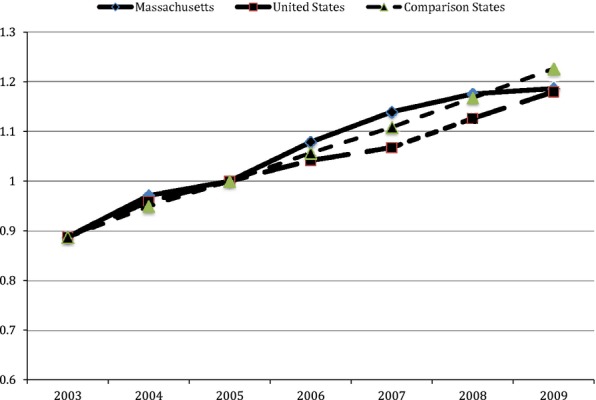
Trends in Medicare Spending per Beneficiary on Physician and Clinical Services in Massachusetts, Comparison States, and Nationwide
Notes. “Comparison states” are Connecticut, Maine, New Hampshire, New Jersey, New York, Rhode Island and Vermont.
Source: Authors analysis of State Health Expenditures (by residence).
To take into account some of the observable differences, a propensity-based weighting method is included. These observables characteristics include insurance rate, physicians per capita, education, and income. We do not include spending per Medicare beneficiary because the volume of visits is a component of total spending.
Data
To construct the outcomes of interest, we use the publicly available Medicare utilization data file compiled by the Dartmouth Atlas group. Based on the 20% Medicare Part B file and 100% Outpatient File, the Dartmouth Atlas group estimated zip code tabulation area (ZCTA) level values for various utilization measures. The only 2 years of available data are for 2005 and 2007. Fortunately, these 2 years capture the year prior to Massachusetts health reform passage and 1 year after its passage; the implementation of various components of the legislation occurred in 2006 and early 2007. The two outcomes of interest are the percent of Medicare beneficiaries with at least one primary care visit and the number of primary care visits per Medicare beneficiary.
To create propensity score weights at the zip code level, we need additional data at the zip code level. Unfortunately, the only dataset available is the Census or 5-year American Community Surveys. Many of the zip code–level attributes are therefore from 2010 or 2011.
To account for the high number of physicians per capita in Massachusetts, we focus separately on primary care physicians and specialist physicians. Dartmouth Atlas also produced a 2007 Physician Characteristics file that gives the number and specialty of physicians at the ZCTA and primary care service area (PCSA). We use the larger PCSA grouping because the Dartmouth Atlas group designed this area, an aggregation of zip codes, to represent where a Medicare beneficiary typically seeks primary care.
One of the most important variables for both the propensity score weighting and the exploration of variation within Massachusetts is the insurance rate. This is another variable not readily available at the ZCTA level. Fortunately, Dartmouth Atlas calculated a 2006 ZCTA-level health insurance estimate based on the 2005 Census Bureau's Small Area Health Insurance Estimates (SAHIE) at the county level and 2006 ZCTA population estimates by Claritas. ZCTA-level health insurance estimates for 2007 are not available so it is not possible to directly use the change in health insurance between 2005 and 2007 to place ZCTAs in the high, medium, or low insurance expansion areas.
Using SAHIE county-level estimates, a simple regression of 2005 insurance coverage estimates on the percent change in insurance coverage from 2005 to 2007 in Massachusetts has an R2 of .89, suggesting that the 2005 ZCTA-level health insurance coverage is a good proxy for the size of the insurance expansion. Furthermore, it is intuitive that the largest expansion would occur in the areas where there is the largest relative number of uninsured individuals.
Empirical Strategy
Given below is the regression we estimated at the zip code level using ordinary-least squares:
where i indexes the zip code. Because we only have 2 years of data, our outcome, ΔUi, is the change in visits per beneficiary or change in percent of beneficiaries with at least one visit over time. Using the change over time as the outcome rather than using individual year outcomes and running a traditional difference-in-difference-in-difference model produces a more compact regression. In addition, we used the arc percent change in visits per beneficiary rather than the simple but less stable percent change.
The Uninsurance Terciles 2 and 3 represent the zip codes that have uninsurance rates that fall between the 33rd and 67th percentiles and the 67th and 100th percentiles, respectively. The percentiles are weighted by the final propensity-based weight so that each tercile contains an equal number of beneficiaries. When these areas are interacted with Massachusetts, they represent areas moderately and highly affected by the insurance expansion.
Our weight combined the average number of beneficiaries in each ZCTA and propensity scores, and we clustered them at the PCSA level.
Results
Descriptive Statistics and Propensity Score–Based Weighting
The purpose of using propensity score weighting is to create two groups that are balanced on the observable characteristics. Propensity score weighting is assigned based on two logistic regressions where the outcome is 1 if a ZCTA is in Massachusetts and 0 if the ZCTA is outside of Massachusetts. External states include Connecticut, Maine, New Hampshire, New Jersey, New York, Rhode Island, and Vermont. The logistic regressions contain covariates, including median household income, percent of minorities, percent of the population under 65, percent uninsured, primary care physicians per capita, specialist physicians per capita, and percent of population under 100% of the Federal Poverty Level. Using the probability of being in Massachusetts generated from the first logistic regression, we decided to drop any ZCTAs outside of Massachusetts that were extremely different from Massachusetts or any ZCTAs inside Massachusetts that were very different from outside of the state. To create the final balanced ZCTA dataset, we use a second logistic regression where only ZCTAs with the probability of being in Massachusetts is between 10 and 90 percent are included. The probability from the second regression and the number of Medicare beneficiaries in a ZCTA are used to create the propensity score weights.
Table 1 displays the ZCTA level means in and outside of Massachusetts with and without propensity score weighting. A significant portion of ZCTAs is dropped, particularly outside of Massachusetts demonstrating that a relatively large number of ZCTAs in comparison states are very dissimilar from those in Massachusetts or vice versa. With the inclusion of propensity-based weighting, the difference between characteristics of Massachusetts and its comparator state decreases, but generally does not match. Nonetheless, a number of the covariates with significant differences between the two groups become much closer in magnitude—median household income, percent uninsured, and primary care physicians per capita. As a balance check, the standardized mean difference of the covariates were generally above .1 prior to using propensity score and most fall below .1 or .2 with the addition of the weights (Rosenbaum and Rubin 1983; Stuart 2010).
Table 1.
Comparing Massachusetts Zip Code Tabulation Areas (ZCTAs) to Non-Massachusetts ZCTAs
| Unweighted | Weighted by Inverse Probability of Treatment | |||||
|---|---|---|---|---|---|---|
| Massachusetts | Comparison States | Standardized Bias | Massachusetts | Comparison States | Standardized Bias | |
| N | 495 | 5,070 | – | 402 | 1,168 | – |
| Propensity score covariates | ||||||
| Percent under 65 | 15.3 | 15.6 | 0.06 | 15.5 | 15.6 | −0.01 |
| Median household income | 71,589 | 65,116 | −0.24 | 70,556 | 69,722 | 0.03 |
| Average household size | 2.47 | 2.52 | 0.18 | 2.43 | 2.44 | 0.07 |
| Percent with high school degree or less | 36.6 | 43.5 | 0.46 | 35.9 | 36.3 | 0.03 |
| Percent renal units | 34.7 | 34.1 | −0.03 | 35.0 | 34.2 | −0.04 |
| Percent minority | 17.0 | 21.3 | 0.29 | 15.5 | 17.7 | 0.19 |
| Percent under 100% FPL | 9.9 | 11.1 | 0.14 | 10.0 | 10.1 | 0.02 |
| PCPs per 100,000 persons | 116 | 103 | −0.41 | 114 | 115 | 0.02 |
| Specialists per 100,000 persons | 99 | 86 | −0.14 | 98 | 100 | 0.03 |
| Percent uninsured | 9.9 | 11.9 | 1.16 | 9.8 | 9.8 | −0.01 |
| Outcomes of interest | ||||||
| Arc percent change in primary care physician visits | 0.6 | −3.0 | – | 0.5 | −3.3 | – |
| Percentage point difference of beneficiaries with at least one primary care physician visit between 2005 and 2007 | 2.56 | −1.68 | – | 2.34 | −0.50 | – |
Note. “Comparison states” are Connecticut, Maine, New Hampshire, New Jersey, New York, Rhode Island and Vermont.
Source: Authors' calculations using zip code-level data from the Census and Dartmouth Atlas.
This table also includes the outcomes of interest, which should be consistent with overall trends between Massachusetts and other states in the final regressions. These means demonstrate a general Massachusetts trend of increases in both primary care utilization measures while other states decrease or do not change. For the most part, the addition of propensity-based weights does not significantly change the results. The percentage point difference of beneficiaries with at least one PCP visit for non Massachusetts states does increase from −1.68 to −0.50, however, the trend between Massachusetts and non Massachusetts states does not change.
Regression Results
Utilization regression results are presented in Table 2. The table includes both primary care utilization outcome measures and regressions with and without propensity-based weighting.
Table 2.
Regression Results
| Propensity Score Weighting, Selected ZCTAs | No Propensity Score Weighting, All ZCTAs | |||
|---|---|---|---|---|
| PCP, Arc Percent Change | PCP, Percentage Point Change, At Least 1 Visit | PCP, Arc Percent Change | PCP, Percentage Point Change, At Least 1 Visit | |
| Constant | −0.046 (0.010)** | 0.003 (0.002) | −0.050 (0.011)** | 0.001 (0.003) |
| Uninsurance tercile 2 | 0.011 (0.011) | 0.001 (0.003) | 0.012 (0.012) | 0.004 (0.003) |
| Uninsurance tercile 3 | 0.028 (0.012)* | 0.005 (0.003)+ | 0.026 (0.011)* | 0.005 (0.003)+ |
| Massachusetts | 0.067 (0.012)** | 0.017 (0.004)** | 0.070 (0.013)** | 0.019 (0.004)** |
| Massachusetts*Uninsurance tercile 2 | −0.017 (0.017) | −0.003 (0.006) | −0.007 (0.017) | −0.004 (0.006) |
| Massachusetts*Uninsurance tercile 3 | −0.069 (0.017)** | −0.007 (0.005) | −0.064 (0.015)** | −0.007 (0.005) |
| N | 1,437 | 1,437 | 4,547 | 4,547 |
Note. **p < .01, *p < .05, +p < .1.
The uninsurance tercile 2 represents ZCTAs with the medium levels of uninsurance in 2005, whereas the uninsurance tercile 3 represents the ZCTAs with the highest level of uninsurance in 2005. All regressions were clustered at the PCSA level and used robust standard errors. “Selected ZCTAs” are those that have a predicted probability of being in Massachusetts between 0.1 and 0.9.
Source. Authors' calculations.
Column 1 shows the results of the percent change in primary care visits per Medicare beneficiary. Overall, there was a 4.6 percent decrease in visits per Medicare beneficiary or an average decrease of 137 visits per one thousand beneficiaries. The coefficients for areas with higher uninsurance rates also suggest decreases in visits per beneficiary, however, there is slightly less of a decrease in these areas with the coefficient positive and weakly significant (p < .10). The result suggests that people in the highest areas of uninsurance in 2005 experienced a 1.7 percent decrease or an average decrease of 51 visits per 1,000 beneficiaries.
Moving to results specific to Massachusetts, the state coefficient matches previous work demonstrating a statistically significant and positive increase in visits per beneficiary relative to comparable surrounding areas. Relative to comparison states, Massachusetts experienced a 6.7 percent increase in visits and overall experienced a 2.2 percent increase. The overall increase corresponds to an increase in 64 visits per 1,000 Medicare beneficiaries. When looking at the interacted uninsurance terciles, the story in Massachusetts is the opposite of the overall trend, which may be indicative of the effect of the insurance expansion. Areas with higher uninsurance rates in Massachusetts in 2005 experienced a significant decrease in visits per beneficiary from 2005 to 2007. The 6.7 percent increase in Massachusetts overall is completely offset by the decrease found in areas with a large insurance expansion (p < .01). Relative to Massachusetts overall, those most affected by the expansion experienced a decrease of 117 visits per 1,000 beneficiaries.
The results in Column 2 describe a simpler story about the percentage point change in one or more primary care visits. Overall, there appears to be little change in this outcome over time. The coefficient for the areas with largest uninsurance rates in 2005 is weakly significant and very small in magnitude. The only strongly significant coefficient (p < .01) is Massachusetts with a 1.7 percentage point increase. This coefficient is small in magnitude but represents a 7 percent decrease in the percent of the population without an annual visit to a primary care physician. All other Massachusetts coefficients are not statistically significant.
The results in Columns 3 and 4 represent the same regressions in Columns 1 and 2, respectively, without propensity-based weighting. The results are very similar in magnitude and statistical significance, implying that the covariates used in the propensity-based weighting affected baseline observable characteristics, but did not strongly affect the change in primary care utilization over time.
Limitations
This study has a number of limitations. It is important to look both at the short- and long-term changes, and unfortunately this study only compares changes between 1 year prior and 1 year post reform due to data availability. Longer term changes may lessen or exacerbate the differences between geographic regions as patterns of use shift or providers move. Additional data limitations lie in the use of the 20 percent rather than 100 percent Part B file. These data only include fee-for-service beneficiaries, so it is notclear how Medicare Advantage beneficiaries would be affected.
Finally, it is always difficult to ensure one is truly measuring utilization. Utilization is confounded by mortality and access—as one becomes sicker, a person is more likely to seek care. By only using primary care measures, in particular the percent of the population with at least one primary care visits, this bias is lessened.
Discussion
With national health reform's insurance expansion in full swing in 2014, it is important to understand how the expansion may affect the Medicare population. Massachusetts is often referred to as the model for national health reform with many components of national health insurance expansion—Medicaid expansion, insurance exchange for those with and without subsidies—in both pieces of legislation.
Similar to previous studies on the nonelderly, we find an overall increase in primary care utilization for the Medicare population relative to other states. However, unlike previous studies we also find a reduction in primary care utilization for Medicare beneficiaries residing in areas heavily impacted by the health insurance expansion. Little clinical evidence exists describing the average or recommended number of primary care visits a year. It is unclear whether the decrease of 117 visits per 1,000 beneficiaries a year, or the upper and lower bound that the confidence interview implies, a decrease of 22 visits and 212 visits, is clinically meaningful. To provide some context, in 2005 and 2007 Massachusetts had significantly fewer visits per person a year relative to the national average (p < .001). The difference of 268 visits per 1,000 beneficiaries per year suggests that the difference from the national average increased about 50 percent for those who reside in areas most affected by reform.
Although this estimate only applies to areas most affected by reform, these areas are likely the most generalizable to many states outside of Massachusetts. Areas most impacted by the expansion had an uninsurance rate prior to reform 16 percent higher than the state average. These areas also had 30 percent more minority residents and a 10 percent higher rate of poverty relative to the state average. Surprisingly, these areas had more physicians per capita—6 percent more primary care physicians and 18 percent more specialist physicians—possibly suggesting the lower insured populations reside near large safety net providers. It is important to note that even though these characteristics are more comparable to other areas of the country, Massachusetts is still different and any generalization should be taken cautiously.
It is not clear from our results whether Medicare beneficiaries were having trouble getting appointments, or if their doctors were just recommending that a patient not return as soon. If the latter occurred, it is reasonable to hope that physicians were rationing in an efficient manner, that is, reducing visits for those who needed them least. Results from Joynt et al. (2013) provide some reassurance in demonstrating that the preventable hospital admissions for Medicare beneficiaries did not increase. However, we do not know whether patients simply turned to other specialist physicians for services better suited for a primary care setting.
It is also possible that other types of providers such as nurse practitioners and physician assistants mitigated any spillover effect from an increase in newly insured individuals to the Medicare population. However, this study did not address the role these clinicians may have played in changes in primary care utilization.
Medicare's finances are under severe strains and its fiscal troubles are only expected to grow. If the ACA reduces Medicare utilization, it would be a good thing for the federal budget. Although our analysis is limited to 2005–2007, the state-level trends beyond 2007 (see Figure 1) suggest that Medicare physician spending growth continued to slow down in Massachusetts.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors thank Susan Yeh for her helpful input.
Disclosures: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
References
- Joynt KE, Chan D, Orav EJ, Jha AK. “Insurance Expansion in Massachusetts Did Not Reduce Access among Previously Insured Medicare Patients”. Health Affairs. 2013;32(3):571–8. doi: 10.1377/hlthaff.2012.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolstad JT, Kowalski AE. “The Impact of Health Care Reform on Hospital and Preventive Care: Evidence from Massachusetts”. Journal of Public Economics. 2012;96(11–12):909–29. doi: 10.1016/j.jpubeco.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy H. “Health Reform: Learning from Massachusetts”. Inquiry. 2012;49:300–2. doi: 10.5034/inquiryjrnl_49.04.06. /2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long SK, Stockley K, Dahlen H. “Massachusetts Health Reforms: Uninsurance Remains Low, Self-Reported Health Status Improves as State Prepares to Tackle Costs”. Health Affairs. 2012;31(2):444–51. doi: 10.1377/hlthaff.2011.0653. [DOI] [PubMed] [Google Scholar]
- Long SK, Stockley K, Nordahl KW. “Coverage, Access, and Affordability under Health Reform: Learning form the Massachusetts Model”. Inquiry. 2012;49:303–16. doi: 10.5034/inquiryjrnl_49.04.03. /2013. [DOI] [PubMed] [Google Scholar]
- Massachusetts Medical Society. “MMS Physician Workforce Study”. 2010. [accessed on August 31, 2013] Available at: http://www.massmed.org/News-and-Publications/Research-and-Studies/MMS-Physician-Workforce-Study-2010/#.UhGV22TTVgI.
- Miller S. “The Effect of Insurance on Emergency Room Visits: An Analysis of the 2006 Massachusetts Health Reform”. Journal of Public Economics. 2012;96(11–12):893–908. /2013. [Google Scholar]
- Miller S. “The Effect of the Massachusetts Reform on Health Care Utilization”. Inquiry. 2012;49:317–26. doi: 10.5034/inquiryjrnl_49.04.05. [DOI] [PubMed] [Google Scholar]
- Rosenbaum P, Rubin D. “The Central Role of the Propensity Score in Observational Studies for Causal Effects”. Biometrika. 1983;70(1):41–55. [Google Scholar]
- Stuart EA. “Matching Methods for Causal Inference: A Review and a Look Forward”. Statistical Science: A Review Journal of the Institute of Mathematical Statistics. 2010;25(1):1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


