Abstract
Introduction:
Physician communication skills are paramount to patient satisfaction and are linked to important clinical outcomes. Although well-codified in the Royal College of Physicians and Surgeons of Canada (RCPSC) CanMEDS program, the knowledge, skills, and assessment of communication skills in surgical specialty training are rarely addressed. We assess Canadian urology residents’ experience of and attitudes towards this crucial competency in training and practice.
Methods:
An anonymous, cross-sectional, self-reported questionnaire was administered to all final year urology residents in Canada from 2 consecutive graduating years (2010 and 2011). A closed-ended 5-point Likert scale was used to assess familiarity with the concept of the RCPSC Communicator role and its application and importance to training and practice. Descriptive and correlative statistics were used to analyze the responses, such as the availability of formal training and resident participation in activities involving health communication. For ease of reporting, an agreement score was created for those responding with “strongly agree” and “agree” on the Likert scale.
Results:
There was a 100% response rate from the chief residents for both of the 2 years of the survey (n = 58). When questioned about the RCPSC CanMEDS roles, only 45% could identify the correct number of roles, and only 19% could correctly list all 7 roles. However, most residents were well aware of the Communicator role (90% agreement [mean 4.47 ± 0.78]), and most agreed that it plays an important role during training and future practice (83% [4.16 ± 0.84], 90% [4.39 ± 0.84] respectively). This is in stark contrast to perceived formal training. Only 31% (3.00 ± 1.04) agreed that formal training or mentorship in communication was available at their institution, and only 38% (3.14 ± 1.19) felt that communication had been formally addressed during explicit sessions. Despite most of the respondents agreeing they had a significant mentor/role model to emulate regarding communication skills, only 48% believed that faculty frequently addressed communication during clinical learning experiences.
Conclusions:
Despite knowledge and acceptance of the importance of the Communicator role, there is a perceived lack of formal and explicit training in this essential non-medical expert role of urology residency. It would seem apparent from this needs assessment that there may be an opportunity to coordinate efforts to ensure formal instruction and evaluation in our training programs.
Introduction
There have been many calls for greater attention, study and intervention with respect to medical communication; this may be specifically pertinent in the surgical disciplines, such as urology. Its importance to our profession is not a new concept and, in general, there is consensus on the basics of good communication in health care. There is ample evidence that communication should be considered a focus of medical education and evaluation given its importance in the diagnostic and therapeutic process.1–6 Outcome studies have shown that good physician-patient communication can positively influence medical care. This includes domains, such as patient recall and understanding, adherence to therapy, symptom resolution and physiological outcomes, patient satisfaction, physician satisfaction and malpractice claims.1–3 The opposite is equally telling. Excellent technical proficiency combined with unsatisfactory interactions may not lead to quality care or healthier patients.4,5
The importance of communication and other non-clinical skills prompted the Royal College of Physicians and Surgeons of Canada (RCPSC) Health and Public Policy Committee to establish the innovative Canadian Medical Education Directions for Specialists (CanMEDS) in 1996. This project was established to ensure that postgraduate programs are fully responsive to societal needs and to encourage the design of new residency training programs, curricula, and evaluation processes that would facilitate these goals.6 This shift towards a global competency as opposed to merely mastering medical knowledge and skills prompted the creation of the 7 CanMEDS domains: Medical Expert, Professional, Health Advocate, Scholar, Manager, Collaborator, and Communicator. These roles and competencies have been adopted by major accreditation bodies mandating their incorporation in our postgraduate curricula. There is no question that the teaching, learning and evaluation of these roles are essential, yet these tasks are challenging.7
The most evaluated and taught competency has been Medical Expert, although some have argued that the Communicator role supersedes even this, given its importance in attaining and maintaining good health.8 While some roles easily fit classical models of medical education, others, such as the Communicator role, is more complex for educators and students.9,10 We assess urology residents’ perceptions and attitudes toward the Communicator Role, and the current effectiveness of education aimed at this crucial competency.
Methods
This prospective study surveyed a convenience sample of postgraduate year 5 (PGY-5) residents in English-speaking Canadian urology training programs (n = 58) at a review course in consecutive years (2010 and 2011). Participation was completely voluntary and confidential; no identifying information was recorded in the survey results. Ethics approval was attained from the Queen’s University institutional review board and explanations for the objectives of the study and assurance of confidentiality was distributed to the residents responding to the survey.
The questionnaire consisted of 28 closed-ended questions, as well as open-ended questions to explore the experiences of, and attitudes involving the Communicator role in the urology training programs (Appendix 1, http://journals.sfu.ca/cuaj/index.php/journal/article/view/264/1456). These questions included familiarity with the concepts of the Communicator role, as well as its application and perceived importance in training and practice. The first 3 questions assessed demographic information, background and career aspirations for the respondents, as well as past experience with teaching and evaluation. The rest of the questions addressed the above-described objectives, including attitudes and experiences regarding formal training and resident participation in communication role activities. Questionnaire development resulted from an initial experience with a previous survey construction for similar attitudes for specialty residents. Residents and educators involved in both undergraduate and postgraduate programs were asked to assess and modify the survey for clarity.
Descriptive statistics were used to tally demographics and background information. Responses to the questions using the 5-point Likert scale are described as means ± standard deviation. For ease of reporting, agreement responses of 4 and 5 to were grouped together, as were the disagreement responses of 1 and 2. All other quantitative statistics utilized the full 5-point Likert scale. A Mann-Whitney test was used to compare Likert scale scores between respondents between the 2 years of the study and between specifically linked questions. Spearman or Pearson tests, depending on normality of distribution, were used to demonstrate correlations of respondents to questions using the Likert scale. The GraphPad Prism 4 statistical software package (GraphPad Software, Inc., San Diego, CA) was used for analysis.
Results
There was a 100% response rate from all chief residents in this convenience sample (n = 58). In total, 26 residents (45%) reported that they worked between 60 and 70 hours per week on average. Five residents (9%) estimated they worked 71 to 80 hours a week and 6 (10%) stated they worked more than 80 hours per week. Of the graduating urology residents, 83% were planning on completing a fellowship, and 47% felt it would be likely that they would work at a non-academic centre.
Comparing the 2 groups of residents, there was very little difference in responses to the closed-ended questions other than a reported increased understanding of the CanMEDS roles in the 2011 cohort. The correct number of CanMEDS roles (7) was recognized by roughly half of the respondents (55%), and only 19% could correctly list all 7 roles. The results were significantly different between the graduating cohorts of 2010 and 2011; the 2011 group were better able to list the 7 CanMEDS roles (p = 0.03). The 2011 group were also more aware that communication skills are part of their residency objectives (p = 0.01). As no other differences were noted with respect to the reported attitudinal/experiential aspects of the survey, the data from both years were combined and analyzed together.
Respondents were mostly cognizant of the Communicator role as defined by CanMEDS (90% agreement, mean 4.47 ± SD 0.78); however, only 67% felt the role was clearly defined (3.86 ± 0.94). Most respondents (83%) felt that the Communicator role is important (4.16 ± 0.84) to address during urological training and they nearly uniformly agreed (90%) that proper communication would play a substantial role in their future practice (4.39 ± 0.84) (Fig. 1). There was a positive correlation between those who believed communication is an important aspect of urological practice and those who felt a need for formal communication training in residency (correlation coefficient 0.635, p < 0.001). As well, those that reported a good understanding of the Communicator role also reported a desire for formal education in training (correlation coefficient 0.483, p < 0.001). There was, however, some reported ambivalence about whether formal training in communication should be mandatory during urology residency training; only 50% agreed it should be mandatory (3.53 ± 0.94).
Fig. 1.
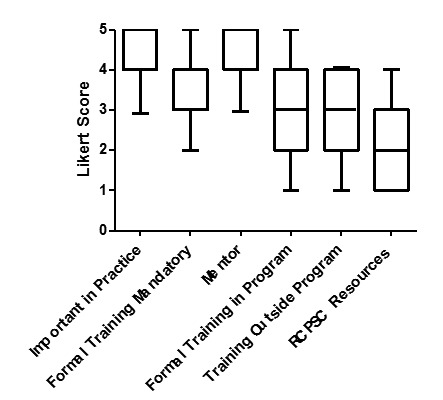
Attitudes and Experience of Communicator Role in Training. Box and whisker plot (Box=mean Likert score, 95% confidence limit) of Likert score responses to questions on awareness of role in residency as well as experience and knowledge of formal training opportunities. Respondents felt communication was important in practice and had a mentor but did not access outside resources or receive formal training.
Most respondents felt they had a positive mentor/role model for effective communication (84%, 4.04 ± 0.81) (Fig.1). However, any formal training experience with communication was surprisingly low. Only 36% agreed that there was formal training available to them from their urology program, core curriculum or postgraduate department (3.00 ± 1.04) (Fig. 1). Additionally, a mere 31% reported having training in communication from any other sources outside of their University, such as the College of Physicians and Surgeons of Ontario, RCPSC or Canadian Medical Protective Association (2.72 ± 1.16). The RCPSC has developed online modules regarding non-medical expert CanMEDS roles, including the Communicator, but only 15% of respondents were aware of these resources. Forty-eight percent felt that faculty frequently addressed communication during clinical learning experiences (3.45 ± 1.08), and 38% responded that faculty frequently formally addressed communication during explicit sessions or role modeling (3.14 ± 1.19) (Fig. 1). There was a good correlation of the resident-reported comfort with their role as communicator in urology and their reported explicit educational experiences in communication skills, in particular with formal training at their respective programs (correlation coefficient 0.363, p = 0.005).
Nearly all respondents (93%) were aware that communication is a part of the evaluation reports in their residency program (4.43 ± 0.68), and also part of their formal objectives (88%, 4.25 ± 0.80) with a correlation coefficient of 0.747 (p < 0.001). However, there was relatively low agreement that residents received even an informal direct evaluation of their communication skills in clinic or non-clinical situations, including role-modelling exercises (Fig. 2). Furthermore 41% of chief residents responded that they never received feedback on even one specific problem they had experienced with communication during their training (2.71 ± 1.11). Tools and aids for evaluating residents’ communication appear to be underused in urology training programs across Canada (Table 1).
Fig. 2.
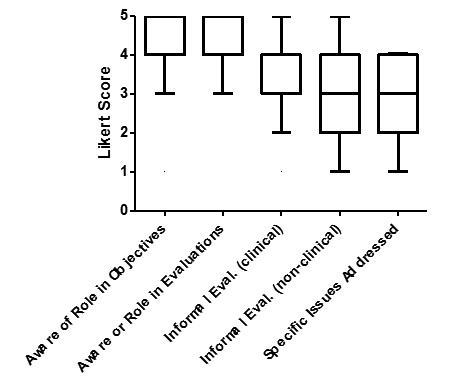
Evaluation of Communicator Role in Training. Box and whisker plot (Box=mean, 95% confidence limit) of Likert score responses to survey questions on awareness and experience of role in objectives and evaluations in training. Respondents are highly aware of communication role as an objective and part of their evaluations, but evaluations specific to communication are not uniformly administered.
Table 1.
Percentages of respondents who had been exposed to formalized CanMEDS teaching tools
| Type of teaching/evaluation tool used | Percentage of respondents exposed |
|---|---|
| Video encounters | 10% |
| 360-degree evaluations | 28% |
| Portfolios | 16% |
| Simulator scenarios | 31% |
Discussion
The method of training surgeons exclusively to master technical skills and clinical knowledge is slowly becoming an outdated practice. Indeed, educational governing bodies have now mandated the instruction and evaluation of expanded competences, such as the seven CanMEDS roles to grant accreditation.11–13 Paramount in the skill set of the “new physician” is the ability to effectively and sensitively communicate with patients. This survey of chief residents in Canadian urology training programs was intended to identify awareness of, and attitudes towards, the CanMEDS Communicator role in urology, and assess how residents are being trained and evaluated in this crucial role.
There was an overall consensus that skillful communication is vital; almost all respondents were aware of the CanMEDS role of communication. This proclaimed importance is in discordance with the utilization of available communication resources, and formal instruction regarding communication. Most residents did not have any instruction or use available resources to develop communication skills. The inconsistent availability or use of formal instruction shown in this study is similar to findings from studies involving other subspecialties.7
Communication is a learned skill, and therefore can be taught. Particularly, doctor-patient communication skills have been shown to be effectively acquired though formal teaching.14 The only “training” that most urology residents receive is through role models and mentoring. This form of learning can be effective, but has inherent problems. As Razack and colleagues have articulated, medical specialties function much like subcultures, with slightly different values and behavioural norms associated with each discipline. This analogy is particularly relevant with respect to communication skills, which are often taught implicitly in day-to-day clinical interactions, in a manner similar to the way culture is transmitted.15 Experientially, most urologists would agree that we have a particular and unique culture that is passed down and across to each member of our “tribe.” If the communication milieu of urologists is flawed, we pass those shortcomings along as well.
The lack of explicit teaching in communication among Canadian urology programs is also troubling because communication skills were incorporated into our objectives and evaluations more than a decade ago. This survey revealed a considerable gap, as most residents knew communication was part of their objectives and evaluation, but also conceded that only modest formal teaching or evaluation was taking place. This is not to say that our graduates are necessarily falling short, as there is scarce objective outcomes research on trainees’ ability to communicate. Our current format of model learning is arguably effective, but lacks adequate evaluation. It is the our perception that with the advent of the CanMEDS roles, more attention has been placed on the non-medical expert spheres of training physicians; however, this has not necessarily translated into ubiquitous, structured teaching or evaluation as outlined in this study. We are currently situated to place our specialty at the forefront of empirical training and evaluation of the CanMED roles. Systematic incorporation of currently available communication resources, such as those offered by the RCPSC, into urology program curriculum with pre- and post-evaluation of communication skills would provide an excellent prototype for other specialties to follow, and also provide trainees with feedback and confidence in their abilities to communicate with patients and their peers.
Some of the weaknesses of this study are as follows. This survey was conducted as a convenience sample with the participation of only PGY-5 urology residents. This may not be a fully representative sample of postgraduate trainees, although these residents have been a part of postgraduate training for more than 4 years. This survey represents only a snapshot of their self-reported attitudes and experience close to their RCPSC certification exams, and therefore their focus may be on the “medical expert” aspects of their specialty. The survey relies on the residents’ accurate recollection of formal CanMED’s teaching sessions from their residency training. This bias is highlighted by the fact that a minority recalled receiving formal teaching, but all training programs are required to administer these sessions to receive accreditation from the Royal College.
However, whether there is a perceived or real paucity of formal teaching, the response rate of the residents and the similarity of responses between the 2 cohorts could attest to the veracity of the findings. Two discrepancies between the 2 cohorts: the 2011 group was more familiar with the CanMEDS roles and more aware that communication skills were formally a part of residency objectives. This may reflect increasing exposure of residents to the CanMEDS roles – this was an encouraging finding.
The results from the present study underscore the variable experiences of and attitudes towards the Communicator role during urology residency. The issues around the poor uptake of formal teaching and evaluation of communication skills is likely not unique to urology. Chou and colleagues reported that 92% of Canadian postgraduate training programs evaluated CanMEDS roles, but program directors were concerned with how roles other than medical expert were being taught and evaluated.15 Our results appear to be similar to others,7 suggesting that although we may feel like residency programs are prioritizing the teaching of complementary CanMEDS, we are, in fact, falling short. The question that needs to be answered is: Are the CanMEDS RCPSC standards unattainable or does formal resident education need a complete redesign?
As George Bernard Shaw said, “The single biggest problem in communication is the illusion that it has taken place.”
Conclusions
Despite knowledge and acceptance of the importance of the CanMEDS Communicator role, there is a perceived lack of formal and informal training of this essential non-medical expert role of urology residency. It would seem that there is a need to redouble efforts to ensure appropriate instruction and evaluation in our training programs.
Footnotes
Competing interests: Dr. Siemens is the Editor-in-chief at CUAJ and he along with Dr. Roberts, Dr. Beiko and Dr. Touma declare no other competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.White K. The task of medicine. Menlo Park, California: The Henry J. Kaiser Family Foundation; 1988. [Google Scholar]
- 2.Bensing J. Bridging the gap: the separate worlds of evidence-based medicine and patient-centered medicine. Patient Educ Couns. 2000;39:17–25. doi: 10.1016/S0738-3991(99)00087-7. [DOI] [PubMed] [Google Scholar]
- 3.Levinson W, Roter DL, Mullooly JP, et al. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277:553–9. doi: 10.1001/jama.1997.03540310051034. [DOI] [PubMed] [Google Scholar]
- 4.Roter DL, Hall JA. Doctors talking with patients/patients talking with doctors. Improving communication in medical visits. Westport, Connecticut: Auburn House; 1992. [Google Scholar]
- 5.Koehler WF, Fottler MD, Swan JE. Physician–patient satisfaction: Equity in the health services encounter. Med Care Rev. 1992;49:455–84. doi: 10.1177/002570879204900404. [DOI] [PubMed] [Google Scholar]
- 6.Crow R, Gage H, Hampson S, et al. The role of expectancies in the placebo-effect and their use in the delivery of health care: a systematic review. Health Technol Assess. 1999;3:1–96. [PubMed] [Google Scholar]
- 7.Leveridge M, Beiko D, Wilson JWL, et al. Health advocacy training in urology: a Canadian survey on attitudes and experience in residency. Can Urol Assoc J. 2007;1:363–9. doi: 10.5489/cuaj.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lipkin M, Putnam SM, Lazare A. The medical interview: clinical care, education and research. New York: Springer; 1995. [DOI] [Google Scholar]
- 9.Bensing JM. Doctor–patient communication and the quality of care: an observational study into affective and instrumental behaviour. Utrecht: NIVEL; 1991. [Google Scholar]
- 10.van Dulmen AM, Bensing JM. The effect of context in healthcare a programming study. The Hague: RGO; 2001. [Google Scholar]
- 11.Frank J, Jabbour M, Tugwell P, et al. Skills for the new millenium: report of the societal needs working group. Ottawa: Royal College of Physicians and Surgeons of Canada; 1996. [Google Scholar]
- 12.Nasca TJ. The next step in the outcomes-based accreditation project. ACGME Bull. 2008:2–4. [Google Scholar]
- 13.Frank JR, editor. Better standards Better physicians Better care. Ottawa: The Royal College of Physicians and Surgeons of Canada; 2005. The CanMEDS 2005 physician competency framework. [Google Scholar]
- 14.Maguire P. Can Communication Skills be Taught? Br J Hosp Med. 1990;43:215–6. [PubMed] [Google Scholar]
- 15.Razack S, Meterissian S, Morin L, et al. Coming Of Age As Communicators: Differences In The Implementation Of Common Communications Skills Training In Four Residency Programmes. Med Educ. 2007;41:441–9. doi: 10.1111/j.1365-2929.2007.02722.x. [DOI] [PubMed] [Google Scholar]
- 16.Chou S, Cole G, McLaughlin K, Lockyer J. CanMeds evaluation in Canadian postgraduate training programmes: tools used and programme director satisfaction. Med Educ. 2008;42:879–86. doi: 10.1111/j.1365-2923.2008.03111.x. [DOI] [PubMed] [Google Scholar]


