Abstract
Background
Chronic pain after surgery occurs in 10-40% of individuals, including 5-20% of women after cesarean delivery in previous reports. Pain and depression 2 months after childbirth are independently associated with more severe acute post-delivery pain. Here we examine other predictors of pain at 2 months and determine the incidence of pain at 6 and 12 months after childbirth.
Methods
Following Institutional Review Board approval, 1228 women were interviewed within 36 hr of delivery. Of these, 937 (76%) were successfully contacted by telephone at 2 months, and, if they had pain, at 6 and 12 months after delivery. The primary outcome measure was presence of pain which began at the time of delivery. We also generated a model of severity of acute post-delivery pain and 2 month pain and depression.
Results
Pain which began at the time of delivery was remarkably rare 6 and 12 months later (1.8% and 0.3% [upper 95% confidence limit, 1.2%], respectively). Past history of pain and degree of tissue damage at delivery accounted for 7.0% and 16.7%, respectively of one aspect in the variability in acute post-delivery pain. Neither of these factors was associated with incidence of pain 2 months later.
Conclusions
Using a definition of new onset pain from delivery, we show a remarkably low incidence of pain 1 year after childbirth, including those with surgical delivery. Additionally, degree of tissue trauma and history of chronic pain, risk factors for pain 2 months after other surgery, were unimportant to pain 2 months after cesarean or vaginal delivery.
Introduction
Major physical trauma, including surgery, results in nearly universal acute pain which resolves in most individuals over weeks to a few months. For those with pain several weeks after surgery, pain resolves slowly, with an estimated half-life of 6-7 years.1,2 Thus, if the initial incidence is high, the burden on patients and health care can be great. Important risk factors for chronic pain after surgery include the degree of tissue trauma and preexisting patient characteristics, especially preexisting chronic pain.3,4 Childbirth is associated with physical trauma and nearly 1/3 of deliveries are performed by cesarean section in the United States. In a 2 year follow up of nearly 1,000 women for breech delivery by cesarean section, there was a 20% incidence of pain, mostly comprising back- and headache, with approximately 5% with pain in the superficial or deep abdomen.5 A Danish postal survey indicated pain in the surgical area of 19% at 3 months and 12% at 10 months after cesarean delivery, with half of these women experiencing daily or near daily pain.6 These data suggest that childbirth, especially cesarean delivery, represents a major cause of chronic pain in women.
Previous studies have often not critically separated new pain after the surgery from pre-existing pain. For example, of the 32% of 1,300 Danish women experiencing pain one year following abdominal hysterectomy, only 4.4% ascribed new pain from the surgery itself.4 During pregnancy there is a high incidence of abdominal, back, and pelvic pain,7,8 which could, if included, inflate the observed incidence of chronic pain from childbirth. To better understand the incidence and risk factors for chronic pain after delivery, we performed a prospective, multi-center study with specific focus on new pain which began at the time of labor and delivery. We previously reported that presence of this pain and postpartum depression 2 months after delivery was predicted by severity of acute, post-delivery pain but not by mode of delivery (vaginal or cesarean).9 That report9 represented a secondary analysis of the Pain After Delivery study, whose primary outcome measure was the incidence of pain beginning at the time of delivery and still present 1 year after childbirth. Here we report the results of this primary outcome analysis.
A secondary purpose of this study was to generate a predictive model of chronic pain after childbirth. The extremely low incidence of pain 6 and 12 months after delivery did not allow us to generate such a model for truly chronic pain. Nonetheless, approximately 10% of women in this study had persistent pain 2 months after delivery, which interfered with their normal activities,9 and a similar proportion suffered from post-partum depression at this time. We therefore sought to generate a predictive model for pain and depression 2 months after delivery, asking whether factors other than the severity of acute post-delivery pain were involved. Since past history of pain10 and degree of surgical trauma3 have been associated with risk of chronic pain after other types of surgery, we applied a data reduction strategy which focused primarily on these factors.
Materials and Methods
Following Institutional Review Board approval and written informed consent, 2,518 women hospitalized for childbirth at Forsyth Medical Center, Wake Forest University, Winston-Salem, NC, Columbia University Medical Center, New York, NY, Université Catholique de Louvain, Brussels, Belgium, and Hôpitaux Universitaires de Genève, Geneva, Switzerland from September 2004 to December 2005 were interviewed within 36 hr of delivery and their medical records reviewed, with focus on characteristics of pregnancy and delivery and past medical history, including history of pain during or preceding pregnancy. Full details of the interview questions and chart review are provided in our previous publication from a secondary analysis from this dataset.9 Although all pain was recorded, the primary outcome measure was defined as pain which began at the time of labor and delivery and included a location which could be ascribed to the delivery (pelvis, perineum, abdomen). Patients were then contacted at 2, 6 and 12 months after delivery and questioned regarding these specific locations of pain beginning at the time of labor and delivery using a scripted telephone interview with simultaneous data entry by interviewers (US sites), or postal survey (European sites). Due to the different methodology of follow up and response rate between the United States and European sites, the European data were not used for long term follow up in the current study, nor were they used in the 2 month report.9
Patients who reported pain which began at the time of delivery and which was still present 2 months later were contacted by telephone at 6 months, and those with pain at 6 months were contacted again at 12 months after delivery. At both 6 and 12 months, subjects were queried regarding their average and worst pain for the preceding week as well as the intensity of their current pain using a 0-10 verbal scale, with 0 being no pain and 10 being the worst imaginable pain. Patients were asked to describe their pain using the short form McGill Pain Questionnaire,11 its location, its effect on various activities of daily living, and whether they sought medical attention for its treatment. For activities of daily living, subjects were asked whether pain affected walking, standing, climbing stairs, getting up from a chair, carrying bags, driving, participation in athletics or working and if effects of pain were present on their mood, sleep, or ability to concentrate. In addition, at the 6 month interview, the degree to which their pain was neuropathic in character was quantified using a validated inventory described by Bouhassira et al.12 Finally, the presence of depression at the 12 month interview was assayed using the Edinburgh Post Partum Depression Inventory, a series of questions validated for the postpartum period.13
Statistical analysis
There were two goals of data analysis: 1) to describe the incidence of the onset and course of delivery-related pain; 2) to generate a predictive model for pain and depression at two months after delivery.
The estimation of pain incidence at each measurement occasion is straightforward without missing data. According to the study design, each participant was queried about the existence of pain related to her delivery at each measurement occasion as previously described.9 After a participant indicated that she did not have pain related to her delivery, she was not queried at later occasions and a “no pain” score was imputed for the remaining measurement occasions. The value of this plan is based on the assumption that pain related to delivery is unlikely to remit and then re-initiate at a later time. It is of note that these individuals could not be lost to observation, because no attempts were made to contact them after they reported being pain free. This is in contrast to the individuals who continued to report pain and who were contacted at each measurement occasion. These individuals could be lost to observation, thus potentially biasing the incidence estimate downward. To account for this differential pattern of missing data, three different estimates of the incidence rates were calculated and reported for each measurement occasion.
The first estimate of the incidence rates assumed the data were missing completely at random (MCAR) and were simply calculated as the observed proportion of participants with pain at each time point. Because of the specific potential for downward bias induced by the sampling plan, this estimate served as the lower bound of the incidence rate. The second estimate of the incidence rate assumed that the data were missing at random (MAR) and was calculated using several multiple imputation (MI) models.14,15 Multiple imputation assumes that the values for the missing outcomes are conditional on the values of the actually observed outcomes (and other predictors). The MI procedure draws repeated estimates of the missing values to impute plausible values, and these values can be combined to produce estimates of the likely values for these missing data. The MI models were conducted using Proc MI (SAS 9.2; SAS Inc. Cary, NC) with 100 imputations. One model was created for each measurement occasion (2 months, 6 months, 12 months) with the presence/absence of pain being conditional on study site, worst pain rating within 72 hours after delivery, parturient age, gestational age, total neonate weight, reported pain with menstruation, number of fetuses, previous history of cesarean section, intensive care unit admission during birth, previous delivery problems, smoking status, alcohol use, reported pain during pregnancy, delivery type, reported state of health, and somatization score. The final estimate of pain incidence assumed the data were not missing at random (NMAR). These estimates relied on the same MI model predictors, but assumed that having pain at the previous measurement occasion increased the probability of being lost to observation on the next occasion (pain drop out model, PDOM). To produce this effect, the MI models were conducted iteratively, with the results of each measurement occasion informing the next such that the imputed values from the previous measurement occasion were used to impute the next value. These estimates served as the likely upper bound of the estimates.
To accomplish the second goal of the analysis, two analytical steps were undertaken. Because pain after delivery was previously demonstrated to be related to the presence of pain at 2 months,9 we sought to develop models that predicted pain after delivery to examine if these predictors could themselves predict prolonged pain. First, a multivariate association between three estimates of the post-delivery pain experience (pain now, worst pain, average pain) was examined with three different theoretical predictor groups (patient characteristics, pain history, and tissue damage) to determine if any of these predictor sets could predict any element of the pain experience. All of the individual predictors from these three groups are listed in Table 1.
Table 1.
Standardized canonical weights of the first (best) canonical variate for the three predictor groups and pain scores
| Predictor | Predictor Group N = 937 |
|||
|---|---|---|---|---|
| Non-missing sample size % of available |
Patient characteristics n = 803/911 (86%)/(97%)† |
Pain history n = 908 (97%) |
Tissue damage n = 887 (95%) |
Missing Data |
| age | −0.00 | 4 (0.4%) | ||
| Body mass index | 0.04 | 116 (12.4%) | ||
| gestational age | −0.02 | 10 (1.1%) | ||
| state of health | −0.93 | 0 (0%) | ||
| somatization | 0.11 | 2 (0.2%) | ||
| cigarette | 0.36 | 1 (0.1%) | ||
| Alcohol | 0.70 | 2 (0.2%) | ||
| first baby | −0.11 | 2 (0.2%) | ||
| pain prior to pregnancy | 0.24 | 4 (0.4%) | ||
| relative with pain | −0.02 | 1 (0.1%) | ||
| pain with menstruation | 0.44 | 0 (0%) | ||
| doctor/medications | −0.43 | 10 (1.1%) | ||
| chronic medical condition | 0.03 | 0 (0%) | ||
| previous history pain during pregnancy |
0.12 | 1 (0.1%) | ||
| pain during pregnancy | 0.70 | 6 (0.6%) | ||
| delivery type | 1.08 | 0 (0%) | ||
| number of fetuses | 0.14 | 3 (0.3%) | ||
| episiotomy | 0.22 | 6 (0.6%) | ||
| perineal lasceration | 0.14 | 16 (1.7%) | ||
| blood loss | −0.08 | 1 (0.1%) | ||
| other surgery performed | 0.13 | 1 (0.1%) | ||
| total neonate weight | 0.08 | 25 (2.7%) | ||
| Standardized canonical Pain Weights | ||||
| Average pain | 0.39 | 0.86 | −0.30 | 3 (0.3%) |
| Worst pain | 0.32 | 0.35 | 0.96 | 5 (0.5%) |
| Pain now | 0.43 | −0.26 | 0.40 | 3 (0.3%) |
Because of missing data, model was conducted twice, once with BMI (body mass index) and once without
Canonical correlation was used to examine the multivariate associations.16 Canonical correlation examines the association between two sets of variables (rather than two variables as in bivariate correlation) by creating linear composites of each set that maximizes the association between the sets.16 There are a number of different solutions that could be applied (with the number of sets being equal to the least number of variables in either set), and each solution weights the variables in a unique way, highlighting different aspects of the multivariable relationships. Each association can be evaluated using a traditional inference, with the strength of the relationship indexed using multiple R2. In this way, the greatest observable association is created by weighting the variables optimally to produce optimal associations.
The second analytical step utilized the canonical variates (i.e., weighted scores) from the first step to produce total scores for each of the predictor sets. These total scores were used to predict the presence or absence of pain and the degree of depressive symptoms at 2 months. To accomplish this, all three total scores were forced into a logistic regression to predict the presence of pain and a linear regression to predict the severity of depressive symptoms each at 2 months.
Unless otherwise stated, data are presented as mean (SD) or median [interquartile range]. Nonparametric data in the description of patients with pain at 6 and 12 months were compared using Mann-Whitney U test. All analyses were conducted in SAS 9.2. Where appropriate, all inferences are two-tailed with p < 0.05 interpreted for statistical significance. No efforts were made to adjust p-values for multiplicity. The interpretation of the multiple R2 should be made with caution because data driven procedures, like canonical correlation, capitalize on chance associations within the data and are thus expected to shrink on replication in future data sets. However, the goal of the present analysis was to examine if any combination of the predictor sets had value in predicting future pain state in this data set, making these data driven procedures defensible.
Results
Patient Characteristics and Missing Data
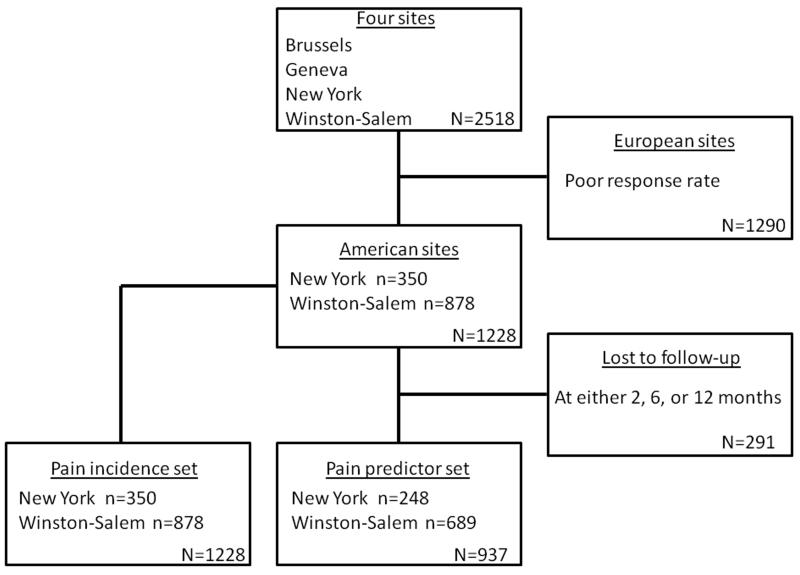
From September 2004 to December 2005, 2518 patients were enrolled at the four study sites. After excluding the European sites due to poor differences in methodology and response rates (n = 1290), the number of participants available for analysis at the American sites were N = 1228. Two analysis sets were derived from these available participants, the pain prevalence set that utilized all available participants to estimate the incidence of pain after delivery, and the pain predictor set that utilized only the n = 937 participants that were available at each of the measurement occasions for the creation of incidence models (See Figure 1).
Figure 1.
Participant disposition for both aspects of the data analysis
The characteristics of these patients have been extensively detailed in the analysis of effect of mode of delivery on pain 2 months later.9 Briefly, n = 837 (68.2%) of the participants had a vaginal delivery, while n = 391 (31.8%) underwent a cesarean delivery. The mean (SD) age for parturients was 29.2 (6.4) years, with a mean body mass index of 31.6 (6.8). At delivery, the mean gestational age was 38.4 (2.6) weeks, with 1178 (95.9%) of paturients giving birth to singletons.
Incidence of pain over time
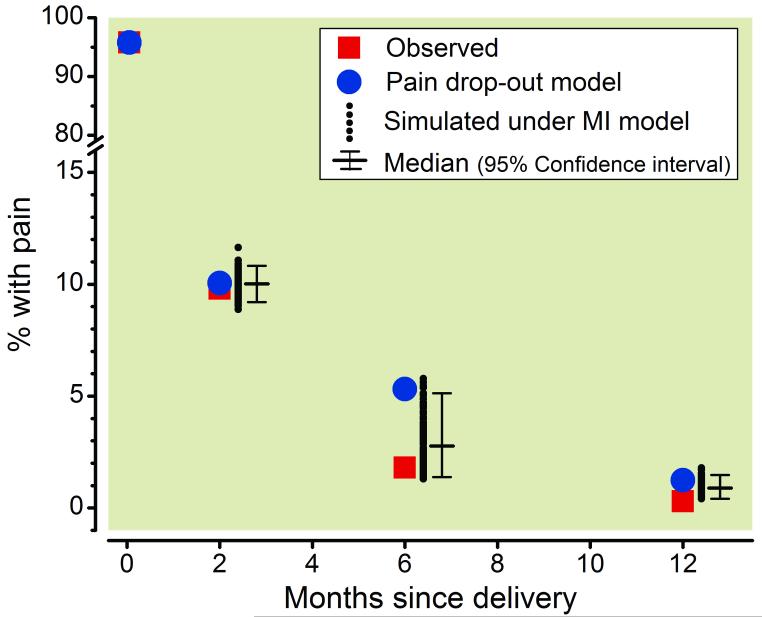
Figure 2 displays the observed incidence of pain along with two estimates of the likely incidence in the population, given that the available sample exhibited missing data. Although 1169 of 1223 (95.6%) of participants reported pain immediately after delivery, the observed rate fell to 95 of 972 (9.8%) at 2 months, 17 of 942 (1.8%) at 6 months, and 3 of 937 (0.3%) at 1 year. Our efforts to consider missing data using several imputation strategies led to slightly higher pain incidence estimates (with likely lower and upper bounds) of 10.0% (9.8% to 10.1%) at 2 months, 2.8% (1.4% to 5.3%) at 6 months, and 0.90% (0.3% to 1.2%) at 1 year.
Figure 2.
Pain incidence after delivery, observed or calculated with the pain drop out model. In addition, multiple imputation model results are shown as small dots with their median and 95% confidence intervals. MI = multiple imputation
Characteristics of pain at 6 months
Of the 95 women with pain 2 months after surgery, 65 (68%) were successfully reached for telephone interview at 6 months. Of these 65 women, 17 (1.4% of the original cohort) reported pain which began at the time of delivery (6 with cesarean and 11 with vaginal delivery, Table 2). Pain was identified in a median of 2 locations per patient, with abdominal scar being the most common location after cesarean delivery and the pelvis after vaginal delivery. Of the 17 women reporting pain at 6 months, only 10 had non-zero scores on the neuropathic pain inventory. The median score was 2.2 [0,5.5] out of a maximum of 10. The number of women with pain 6 months after delivery was not great enough to generate a model of characteristics which predicted pain at this time.
Table 2. Pain characteristics 6 months after delivery.
| Vaginal Delivery (n=11) |
Cesarean Delivery (n=6) |
Overall (n=17) |
|
|---|---|---|---|
| Pain severity | |||
| Average for last week | 3.7 ± 2.3 | 2.0 ± 1.3 | 3.1 ± 2.1 |
| Worst in last week | 4.5 ± 2.7* | 1.8 ± 1.0 | 3.5 ± 2.6 |
| Now | 1.3 ± 2.2 | 1.0 ± 1.3 | 1.2 ± 1.9 |
| Pain interference or problem with | |||
| Standing > 30 min | 73% | 17% | 53% |
| Sitting > 30 min | 64% | 17% | 47% |
| Carrying heavy bags | 45% | 50% | 47% |
| Athletics/sports | 64% | 17% | 47% |
| Getting up from a chair | 45% | 33% | 41% |
| Going up/down stairs | 55% | 17% | 41% |
| Walking | 36% | 17% | 29% |
| Mood | 36% | 17% | 29% |
| Sleep | 45% | 0% | 29% |
| Working | 45% | 0% | 29% |
| Relations with others | 27% | 0% | 18% |
| Ability to concentrate | 18% | 0% | 12% |
| Driving | 9% | 0% | 6% |
| # of items/patient | 5 [1.25, 10] | 2 [0, 3] | 2 [1, 7.25] |
| Pain frequency | |||
| Constantly | 9% | 17% | 12% |
| Daily | 18% | 17% | 18% |
| Several times/week | 36% | 17% | 29% |
| Once a week | 36% | 17% | 29% |
| Less than once a week | 0% | 33% | 12% |
| Taking medication for pain | 73%τ | 0% | 47% |
| Location of pain | |||
| Pelvis | 55% | 50% | 53% |
| Area of incision | 27% | 83% | 47% |
| Back | 55% | 33% | 47% |
| Abdomen | 27% | 17% | 24% |
| Buttocks | 18% | 0% | 12% |
| Legs | 18% | 0% | 12% |
| Headache | 18% | 0% | 12% |
P = 0.047 compared to cesarean delivery by Student’s t test
P = 0.009 compared to cesarean delivery by Fisher’s exact test
Characteristics of pain at 12 months
Of the 17 women who reported pain at the 6 month interview, 13 (72%) were successfully reached for telephone interview at 12 months. Of the 3 women with pain 12 months after delivery, all had experienced a vaginal delivery (Table 3). They had a high burden of pain on activities of daily living and all of them exceeded the threshold of 12 to meet the Edinburgh postpartum depression index for presence of depression (individual values 14, 13, 13). The number of women with pain 12 months after delivery was not great enough to generate a model of characteristics which predicted pain at this time.
Table 3. Pain characteristics 12 months after delivery (n=3).
| Pain severity | |
| Average for last week | 4 [0,4] |
| Worst in last week | 6 [0,7] |
| Now | 2 [0,2] |
| Pain interference or problem with | |
| Standing > 30 min | 2 |
| Sitting > 30 min | 2 |
| Carrying heavy bags | 2 |
| Getting up from a chair | 2 |
| Mood | 2 |
| Sleep | 2 |
| Working | 2 |
| Ability to concentrate | 2 |
| Going up/down stairs | 1 |
| Walking | 1 |
| Relations with others | 1 |
| Driving | 1 |
| # of items/patient | 10 [5,10] |
Predicting Postpartum Acute Pain at 24 hours
The canonical correlation analysis optimized the association between each of the theoretical prediction groups (patient characteristics, tissue damage, and pain history) and some aspect of pain after delivery (pain now, average pain, and worst pain). The optimal association was found by weighting each of the predictors in the group by the standardized weights listed in Table 1. The weights can be interpreted as the relative importance of that predictor in the uncovered association. For example, lower ratings of state of health (-0.90 weight) along with higher levels of alcohol use prior to pregnancy (0.70), and smoking status (0.36) were the most heavily weighted factors that could account for an evenly weighted representation of the post delivery pain experience (i.e., the pain variables were all weighted between 0.32 to 0.43 giving them equal importance in the interpretation). Weighting the predictors in this way created scores that shared R2 = 5.1% of variance in the pain experience, p < 0.0001.
The pain history predictors were principally pain during pregnancy (0.70 weight), and pain ratings during menstruation (0.44). Interestingly, not seeing a doctor or not receiving medications for pain (-0.43) were also weighted modestly in the association. To achieve the optimal association, the average pain experienced was weighted very heavily (0.86) making a patient’s retrospection of the pain they experienced paramount for this association. Weighting the predictors in this way created scores that shared R2 = 7.0% of variance in the pain experience, p < 0.0001.
The tissue damage predictors were dominated by giving birth via cesarean section (1.08 weight), with none of the other predictors being weighted over 0.22. To achieve the optimal association, the worst pain experienced was weighted very heavily (0.96) making this association different than the other predictor groups. Weighting the predictors in this way created scores that shared R2 = 16.7% of variance in this aspect of the pain experience, p < 0.0001.
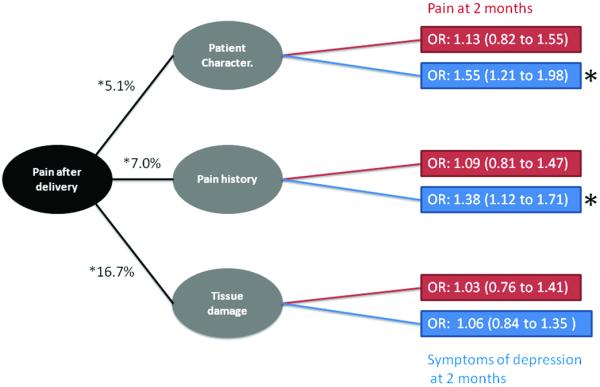
Predicting Pain and Depression at 2 Months After Delivery
The optimal composite scores for each of the theoretical domains were then forced into a regression model to predict the presence of pain and the degree of depressive symptoms at 2 months after delivery. Figure 3 displays the uncovered associations with none of the optimized predictors able to predict the presence of pain at 2 months, p > 0.05. Conversely, both the patient characteristics, 0.93 (95% CI: 0.60 to 1.3), and pain history scores, 0.81 (95% CI: 0.50 to 1.13), were able to predict the degree of depressive symptoms, with each one standard deviation change in the scores being associated with 0.93 and 0.81 points difference in the Edinburgh Post Partum Depression Inventory. For illustration purposes, the odds ratios associated with surpassing the clinical cut-off (>= 13 points) are also presented in Figure 3.
Figure 3.
Predictive model for acute pain after delivery and its application to pain and depression 2 months later. Acute pain after delivery was significantly modeled by each of three factors, patient characteristics, pain history, and tissue damage. These factors failed, however, to result in significant odds ratio (OR) for pain at 2 months (red), although patient characteristics and pain history did significantly affect the OR for depression (blue). *P < 0.05
Discussion
Nearly half of the world’s population experiences labor and delivery, processes which are associated with microscopic or gross tissue injury to the mother. Since this experience is widespread and occurs relatively early in life, the psychosocial, medical, and financial consequences of chronic pain following childbirth could be enormous. Surprisingly, previous studies with long term follow up of new mothers have included pain as a secondary measure and/or have focused on prevalence of pain without determining whether pain predated delivery or even pregnancy itself. This gap in our knowledge is addressed in the current study which focused intentionally on pain which began during the childbirth itself, finding it to be rare in comparison to other physical injuries. Additionally, two central factors hypothesized to confer risk of chronic pain after other injuries including surgery, pre-dating chronic pain and degree of tissue and nerve injury, contributed minimally to the acute and sub-acute pain after childbirth. These two observations, low incidence of chronic pain and minimal effect of degree of tissue injury and history of chronic pain on sub-acute pain, point towards a potential protective effect of pregnancy or delivery on the response to physical injury.
Tissue injury does not inevitably result in chronic pain, yet there are several reasons to anticipate a high incidence of chronic pain from the tissue injury associated with childbirth. Sensory afferents to the uterine cervix and lower uterine segment sprout preceding labor and delivery, become spontaneously active, and become more sensitive to distension of the uterine cervix.17 This may reflect increased estrogen signaling which occurs just prior to the onset of labor, since estrogen increases spontaneous and pressure-evoked responses of uterine cervical afferents by a mechanism involving transient receptor vanilloid-1 channels.18,19 Cervical remodeling, which also begins just prior to the onset of labor, is associated with and dependent upon release of inflammatory substances, including prostaglandins and cytokines, into the cervical tissue,20 and these inflammatory substances are known to sensitize nociceptors.21 One would anticipate that local inflammation and sensory nerve sprouting and sensitization would increase the likelihood of chronic pain by tissue injury in this area. As regards cesarean delivery, traction on ilio-inguinal and ilio-hypogastric nerves and surgical injury to the lower uterine segment with sensitized afferents would also logically increase the likelihood of chronic pain.
In contrast to these considerations, our study suggests that chronic pain after childbirth is much rarer than would be expected from the degree of physical trauma. For example, the incidence of chronic pain after cesarean delivery in our study is over an order of magnitude less than that observed after total abdominal hysterectomy or inguinal herniorrhaphy,10 surgical procedures with similar or lesser degree of trauma to the abdominal wall. Previous studies have suggested a higher incidence of pain after childbirth, but these included pain of uncertain relevancy to the labor and delivery process itself, including predating back pain and headache.5,22,23 We utilized a scripted telephone interview method with simultaneous computer entry rather than interviewing these new mothers in person, and it is conceivable, but unlikely, that some women would have reported pain in person but not over the telephone. Additionally, some women were lost to follow up, and we have no direct knowledge of their incidence of ongoing pain from delivery. For this reason we applied analytic approaches to estimate the likely upper and lower bounds for incidence of pain. Using conservative approaches, the incidence of pain in these estimates still remain remarkably lower than those of abdominal hysterectomy or inguinal herniorraphy.
This is not to say that chronic pain never occurs as a result of childbirth or that its residua are trivial. We previously reported that pain and postpartum depression were present in nearly 10% of women 2 months after cesarean or vaginal delivery, associated with interference with activities of daily living,9 similar to an incidence of 7% 6 weeks after delivery in another large prospective study.23 Although pain was rare in our study 6 and 12 months after delivery, those with chronic pain experienced moderate to severe intensity of pain which was associated with a high utilization of health care and interference with activities of daily living.
We previously showed that pain at 2 months after delivery was strongly predicted by severity of acute pain within 36 hr after delivery,9 but the small incidence of chronic pain after delivery in the longer follow up precluded us from determining a predictive model. We did, however, probe factors which increased the likelihood of acute post-delivery pain and whether the resultant predictive model applied to pain 2 months after delivery, after removing the previously described effect of severity of acute pain. We defined a priori from the dozens of observations those which would likely be related to degree of physical trauma and those related to history of ongoing chronic pain. Although presumed degree of tissue injury contributed to severity of acute pain after delivery, its association was surprisingly small, perhaps reflecting the inability of this somewhat crude approach to quantify tissue injury or a relatively small variability in tissue injury with childbirth. Similarly, the small contribution of pre-dating chronic pain on severity of acute pain and pain 2 months after surgery might reflect a small proportion of women with this condition or the crude assessment of the questions posed. Nonetheless, other studies have utilized these simple methods to demonstrate a clear effect of tissue injury and chronic pain on these outcome measures.3,4,24
Taken together, these observations suggest that either the physical trauma of childbirth, including cesarean delivery, is inadequate to produce chronic pain, or that there are protective biologic or psychosocial factors during pregnancy or the puerperium which nearly eliminate injury-induced chronic pain. Ongoing studies at the Pain Mechanisms Laboratory at Wake Forest University School of Medicine suggest a protective effect of the pueperium from surgical nerve injury induced hypersensitivity,25 consistent with the latter explanation.
In summary, in a prospective study using telephone interviews we observed an incidence of pain 1 year after childbirth of < 1%. Factors presumed to reflect the degree of tissue trauma at delivery and history of chronic pain did not increase the risk of pain 2 months after delivery, after controlling for the effect of severity of acute pain, although they were associated with postpartum depression. These data suggest that chronic pain from childbirth itself does not represent a major public health problem in the United States and we speculate that the puerperium is associated with factors which diminish the risk of chronic pain after physical injury including surgery.
MS #201111123 - Final Boxed Summary Statement.
What we already know about this topic:
-
*
Approximately 10% of women still have pain 2 months following childbirth, suggesting a significant public health burden
What this article tells us that is new:
-
*
By 6 to 12 months most of the pain evident in the first few months has resolved, with an incidence of just 1.8% at 6 months and 0.3% at 12 months
-
*
The reasons for the lower incidence of chronic pain after childbirth compared to surgery are unknown
Acknowledgments
Supported in part by grants GM48805 and NS57594 from the National Institute of Health, Bethesda, MD and from the Sceptor Foundation, Winston-Salem, NC.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Marchand F, Jones NG, McMahon SB. Future Treatment Strategies for Neuropathic Pain. In: Canning BJ, Spina D, editors. Handbook of Experimental Pharmacology. Springer Verlag; Berlin: 2010. pp. 589–617. [DOI] [PubMed] [Google Scholar]
- 2.Kaasa T, Romundstad L, Roald H, Skolleborg K, Stubhaug A. Hyperesthesia one year after breast augmentation surgery increases the odds for persistent pain at four years. A prospective four-year follow-up study. Scandinavian Journal of Pain. 2010;1:75–81. doi: 10.1016/j.sjpain.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 3.Gartner R, Jensen MB, Nielsen J, Ewertz M, Kroman N, Kehlet H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302:1985–92. doi: 10.1001/jama.2009.1568. [DOI] [PubMed] [Google Scholar]
- 4.Brandsborg B, Nikolajsen L, Hansen CT, Kehlet H, Jensen TS. Risk factors for chronic pain after hysterectomy: A nationwide questionnaire and database study. Anesthesiology. 2007;106:1003–12. doi: 10.1097/01.anes.0000265161.39932.e8. [DOI] [PubMed] [Google Scholar]
- 5.Hannah ME, Whyte H, Hannah WJ, Hewson S, Amankwah K, Cheng M, Gafni A, Guselle P, Helewa M, Hodnett ED, Hutton E, Kung R, McKay D, Ross S, Saigal S, Willan A. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: The international randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191:917–27. doi: 10.1016/j.ajog.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Nikolajsen L, Sorensen HC, Jensen TS, Kehlet H. Chronic pain following Caesarean section. Acta Anaesth Scand. 2004;48:111–6. doi: 10.1111/j.1399-6576.2004.00271.x. [DOI] [PubMed] [Google Scholar]
- 7.Röst CCM, Jacqueline J, Kaiser A, Verhagen AP, Koes BW. Pelvic pain during pregnancy -A descriptive study of signs and symptoms of 870 patients in primary care. Spine. 2004;29:2567–72. doi: 10.1097/01.brs.0000145416.22782.9f. [DOI] [PubMed] [Google Scholar]
- 8.Mogren IM, Pohjanen AI. Low back pain and pelvic pain during pregnancy - Prevalence and risk factors. Spine. 2005;30:983–91. doi: 10.1097/01.brs.0000158957.42198.8e. [DOI] [PubMed] [Google Scholar]
- 9.Eisenach JC, Pan PH, Smiley R, Lavand’homme P, Landau R, Houle TT. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140:87–94. doi: 10.1016/j.pain.2008.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: Risk factors and prevention. Lancet. 2006;367:1618–25. doi: 10.1016/S0140-6736(06)68700-X. [DOI] [PubMed] [Google Scholar]
- 11.Melzack R. The short-form mcgill pain questionnaire. Pain. 1987;30:191–7. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 12.Bouhassira D, Attal N, Fermanian J, Alchaar H, Gautron M, Masquelier E, Rostaing S, Lanteri-Minet M, Collin E, Grisart J, Boureau F. Development and validation of the neuropathic pain symptom inventory. Pain. 2004;108:248–57. doi: 10.1016/j.pain.2003.12.024. [DOI] [PubMed] [Google Scholar]
- 13.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 14.Rubin DB. Inference and Missing Data. Biometrika. 1976;63:581–92. [Google Scholar]
- 15.Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons; New York: 1987. [Google Scholar]
- 16.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th edition Allyn and Bacon; Boston: 2007. [Google Scholar]
- 17.Liu B, Tong C, Eisenach JC. Pregnancy increases excitability of mechanosensitive afferents innervating the uterine cervix. Anesthesiology. 2008;108:1087–92. doi: 10.1097/ALN.0b013e31817302e0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yan T, Liu BG, Du DP, Eisenach JC, Tong C. Estrogen amplifies pain responses to uterine cervical distension in rats by altering transient receptor potential-1 function. Anesth Analg. 2007;104:1246–50. doi: 10.1213/01.ane.0000263270.39480.a2. [DOI] [PubMed] [Google Scholar]
- 19.Liu B, Eisenach JC, Tong C. Chronic estrogen sensitizes a subset of mechanosensitive afferents innervating the uterine cervix. J Neurophysiol. 2005;93:2167–73. doi: 10.1152/jn.01012.2004. [DOI] [PubMed] [Google Scholar]
- 20.Maul H, MacKay L, Garfield RE. Cervical ripening: biochemical, molecular, and clinical considerations. Clin Obstet Gynecol. 2006;49:551–63. doi: 10.1097/00003081-200609000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Hucho T, Levine JD. Signaling pathways in sensitization: Toward a nociceptor cell biology. Neuron. 2007;55:365–76. doi: 10.1016/j.neuron.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 22.Declercq E, Cunningham DK, Johnson C, Sakala C. Mothers’ reports of postpartum pain associated with vaginal and cesarean deliveries: Results of a national survey. Birth. 2008;35:16–24. doi: 10.1111/j.1523-536X.2007.00207.x. [DOI] [PubMed] [Google Scholar]
- 23.Macarthur AJ, MacArthur C. Incidence, severity, and determinants of perineal pain after vaginal delivery: A prospective cohort study. Am J Obstet Gynecol. 2004;191:1199–204. doi: 10.1016/j.ajog.2004.02.064. [DOI] [PubMed] [Google Scholar]
- 24.Perkins FM, Kehlet H. Chronic pain as an outcome of surgery - A review of predictive factors. Anesthesiology. 2000;93:1123–33. doi: 10.1097/00000542-200010000-00038. [DOI] [PubMed] [Google Scholar]
- 25.Gutierrez S, Liu B, Hayashida K-I, Houle T, Eisenach JC. Reversal of peripheral nerve injury-induced hypersensitivity in the post-partum period: Role of spinal oxytocin. Anesthesiology. 2012 doi: 10.1097/ALN.0b013e318278cd21. ACCOMPANYING ARTICLE. [DOI] [PMC free article] [PubMed] [Google Scholar]