PURINE TRANSPORT AND SALVAGE IN PARASITIC PROTOZOA
One distinctive feature of the biochemistry of parasitic protozoa is their absolute reliance upon the salvage of preformed purines from their vertebrate and invertebrate hosts. While many mammalian cells possess the innate ability to synthesize purines de novo, all protozoa so far examined that exhibit a parasitic life style lack these biosynthetic pathways and have therefore elaborated a variety of salvage pathways (Fig. 1) that enable them to acquire preformed purines from their hosts (14). These nutrients are imported from the host as either nucleosides or nucleobases, either of which can serve as a purine source for the parasite. The first step in these salvage pathways entails the uptake of the purine nucleosides or nucleobases from the host milieu and is mediated by various nucleoside or nucleobase transporters, located in the plasma membrane of the parasite, that provide substrate-specific permeation routes. While the enzymes of purine salvage have been studied in considerable molecular detail (7), the identification of individual purine transporters at the molecular level is a more recent development. However, over the past several years a plethora of genes encoding nucleoside or nucleobase permeases from parasitic protozoa have been identified and functionally expressed. The increasing understanding of these carriers at the molecular level provides an appropriate setting for a timely review of these important transporters and a comparison of their properties to related and distinct purine permeases of other organisms. This article will concentrate primarily on purine transporters from the Kinetoplastid parasites Leishmania and Trypanosoma brucei, since these are the protozoa with which the majority of the studies have been accomplished. However, we will also briefly discuss related work on transporters from the Apicomplexa Plasmodium falciparum and Toxoplasma gondii. This review does not attempt to be exhaustive but focuses rather upon recent results utilizing molecular genetic approaches.
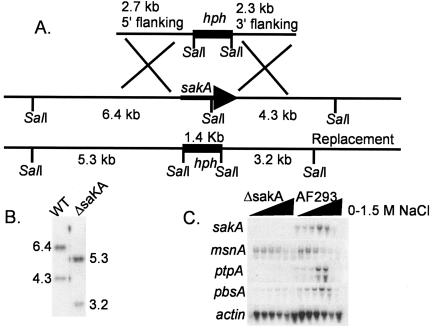
FIG. 1.
Purine uptake and salvage in Leishmania promastigotes. The large oval represents the cell surface membrane of the parasite. The four purine transporters that have been identified in L. donovani and L. major are indicated as NT1, NT2, NT3, and NT4, with their substrates indicated in parentheses (Ado, adenosine; Pyr, pyrimidine nucleosides; Ino, inosine; Guo, guanosine; Hyp, hypoxanthine; Xan, xanthine; Ade, adenine; Gua, guanine). The function of NT4 is currently under investigation. The purine salvage pathway is indicated schematically, with arrows representing the interconversion of individual purines (14).
A principal reason for the interest in purine transport in these protozoa is the essential nature of purine salvage for this large family of parasites. Thus, while some permeases may provide nutrients that are nonessential, albeit advantageous, to the fitness of the organism in its natural environment, the purine transporters as a group are likely to be required for parasite viability in all life cycle stages. A second compelling reason to study these transporters is that they also mediate the uptake of a variety of cytotoxic drugs, many, but not all, of which are purine homologs (11, 13, 49). Consequently, the import of subversive substrates that are metabolized, often uniquely, by parasite purine salvage enzymes is absolutely dependent upon the purine permeases. Thus, this family of permeases plays an important role in the delivery of drugs or experimental therapeutic compounds, and mutations in these carriers can cause drug resistance (5, 13, 36).
STUDIES OF PURINE TRANSPORT IN WHOLE PARASITES
Prior to the cloning of nucleoside and nucleobase transporters, there was a body of studies performed on purine uptake by intact parasites. In general, these investigations confirmed that proteins existed in the parasite surface membranes that mediated the uptake of nucleosides, nucleobases, or both types of purine.
Early studies by Hansen et al. using Leishmania braziliensis (27) promastigotes established that both purine nucleosides and nucleobases were taken up in a substrate-saturable manner and suggested the existence of three transport loci, one for adenosine, one for inosine, and one for the nucleobases hypoxanthine and adenine. Subsequent work by Ullman and coworkers with Leishmania donovani (5, 30) established the existence of two distinct nucleoside transporters with nonoverlapping substrate specificities that mediated the uptake of adenosine and the pyrimidine nucleosides in one case and of inosine and guanosine in the other case. Of particular importance, mutants deficient in each type of transporter were generated. The TUBA5 mutant was selected by use of the cytotoxic adenosine analog tubercidin and was deficient in adenosine and pyrimidine nucleoside uptake, and the FBD5 mutant was isolated by use of the inosine analog formycin B and was disabled in the uptake of inosine and guanosine. These mutants were later employed in a genetic screen to clone the first nucleoside transporter genes from the parasitic protozoa (12, 51). Additional whole-cell studies with L. donovani suggested the existence of an amastigote-specific transporter for adenosine, inosine, and guanosine (23). In addition, genetic selection for Leishmania mexicana mutants resistant to several nucleoside analogs produced lines with a reduced transport capacity for both nucleosides and nucleobases (34) that resulted from an amplified extrachromosomal locus designated TOR (for toxic nucleoside resistance). The pattern of drug resistance and transporter deficiency led the authors of that study to speculate that multiple purine nucleobase permeases exist. A nucleobase uptake activity (3) that transported adenine, hypoxanthine, and the hypoxanthine analog and drug allopurinol and whose inhibition profile strongly suggested that guanine and xanthine were also substrates was characterized with Leishmania major promastigotes. Finally, a transport system for S-adenosylmethionine was detected in L. donovani promastigotes and was also shown to be the route for uptake of the fungal nucleoside antibiotic sinefungin (40). S-Adenosylmethionine can be salvaged to make adenosine or adenine and can also be utilized in methyl transfer reactions and polyamine biosynthesis (24).
Extensive studies have also been performed using intact bloodstream form (BF) and procyclic (tsetse fly) form (PF) T. brucei. Initially, two distinct transport activities, designated P1 and P2, were identified (13). The P1 activity was expressed in both BF and PF parasites and imported adenosine, guanosine, and inosine. The P2 activity was expressed solely in BF parasites and transported adenosine and the nucleobase adenine. Furthermore, P2 activity was responsible for the uptake of melaminophenyl arsenicals such as melarsoprol, a compound used to treat African sleeping sickness, and a mutant deficient in P2 activity was resistant to melarsoprol. The P2 transporter was also shown to be a route for the uptake of the antitrypanosomal drug pentamidine (11). Further characterization of nucleoside transport in PF parasites provided strong evidence that the permeases function as proton symporters, as adenosine uptake was a linear function of the proton motive force across the plasma membrane (20) and was significantly inhibited by protonophores. A distinct transporter for the pyrimidine nucleoside uracil, designated the U1 transporter, was also identified in PF parasites (17). Related studies with BF and PF trypanosomes also identified three high-affinity uptake activities for purine nucleobases, namely H1, expressed in PF parasites (18), and H2 and H3, expressed in BF parasites (19). Principal distinctions between H2 and H3 were that the former, but not the latter, activity was inhibited by guanosine, with a Ki of ∼10 μM, and that H2 was a higher affinity permease for hypoxanthine than was H3 (respective apparent Km values were 123 nM and 4.7 μM). A separate study of BF trypanosomes also produced evidence for a distinct permease for S-adenosylmethionine (24). Purine transporters have also been studied with related Kinetoplastid parasites, including Crithidia fasciculata (21), Crithidia luciliae (26), and Trypanosoma cruzi (22).
The preceding reports of purine transport in whole parasites have played an essential role in defining carrier-mediated transport pathways present in various life cycle stages and in characterizing the uptake properties of such pathways in vivo. Furthermore, these observations strongly suggest that some drugs use purine transporters as routes of entry into parasites. Nonetheless, in vivo systems are often complicated by the coexpression of multiple permeases whose properties can be difficult to dissect convincingly from one another. Furthermore, there is an inherent limitation to the analysis of transporter structure and function or genetics that can be achieved by studying whole-cell systems. For these reasons, it has been necessary to clone and functionally characterize genes that encode individual purine permeases and to examine their comparative properties. Furthermore, the identification of transporter genes has made it possible to study the permeases in molecular detail, using approaches from genetics, molecular biology, protein biochemistry, and cell biology.
FAMILIES OF NUCLEOSIDE AND NUCLEOBASE PERMEASES PRESENT IN EUKARYOTIC ORGANISMS
Molecular genetic studies in a variety of eukaryotic organisms have defined several families of permeases that mediate the uptake of nucleosides or nucleobases. The first eukaryotic nucleoside transporters whose genes were cloned (6) belonged to the concentrative nucleoside transporter family, members of which are typically Na+ symporters exhibiting 13 predicted transmembrane segments. Although this family of permeases is widely distributed in both bacteria and eukaryotes, no members of this family have been found to date among the protozoa. The second family of nucleoside transporters to be identified, initially in mammals, encompassed the equilibrative nucleoside transporters (ENTs) (6, 29). These permeases have 11 predicted transmembrane domains (TMDs) (Fig. 2), in most cases function as equilibrative rather than concentrative permeases (however, see below for exceptions), and may be restricted to the eukaryotic branch of phylogeny, although a potential homology with outer membrane channels involved in the import of nucleosides into gram-negative bacteria has been postulated (1). All of the protozoan nucleoside and nucleobase permeases identified to date belong to the ENT family. Nucleobase transporter genes have been cloned from bacteria, fungi, and plants and belong to the following three distinct families (16): (i) the nucleobase-ascorbate transporter family, (ii) the microbial purine-related transporter family, and (iii) the plant purine-related transporter family. To date, no members of these families have been identified among the protozoa.
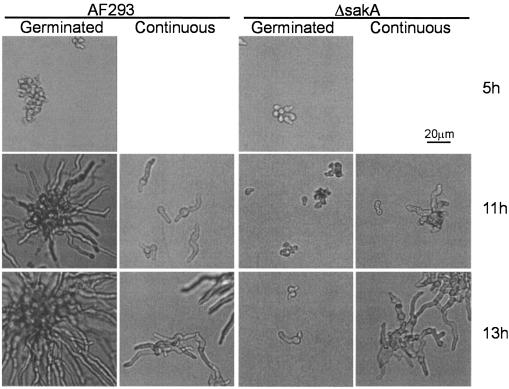
FIG. 2.
Topology of ENT transporters and identification of functionally important residues. Numbered rectangles represent the 11 predicted TMDs, “IN” and “OUT” designate the inside and outside of the plasma membrane, respectively, and the gray background represents the plasma membrane. Functionally important amino acids (single-letter code) are underlined and lines designate their approximate positions within TMDs. Each residue and its corresponding number reflects the particular ENT with which the study was performed as follows: M33, hENT1; C140, rENT2; G179, hENT1; G183, LdNT1.1; C337, LdNT1.1; D389, LdNT2; R393, LdNT2. Appropriate references are given in the text.
NUCLEOSIDE AND NUCLEOBASE TRANSPORTERS FROM LEISHMANIA
The first genes for protozoan nucleoside transporters were cloned (12, 51) from L. donovani by functional complementation of the adenosine-pyrimidine transport-deficient mutant (5) TUBA5 and the inosine-guanosine transport-deficient mutant FBD5. Two closely linked genes, designated LdNT1.1 and LdNT1.2, that encoded proteins that differed in only six amino acids were able to complement the TUBA5 mutant. The LdNT1.1 and LdNT1.2 permeases mediated the uptake of adenosine and the pyrimidine nucleosides with apparent Kms in the low micromolar range. A single gene, LdNT2, complemented the FBD5 mutant and encoded a permease that transported inosine and guanosine with Kms of <1 μM. All three permeases were members of the ENT family and exhibited ∼30% identity at the amino acid level to mammalian ENTs as well as the predicted 11-TMD topology according to appropriate predictive algorithms. There are, however, a number of important differences between the Leishmania ENTs and their mammalian homologs. First, high-affinity competitive inhibitors of the mammalian permeases, including nitrobenzylthioinosine (NBMPR), dipyridamole, and dilazep (29), were not high-affinity inhibitors of the protozoan carriers. Second, detailed electrophysiological studies of the three parasite permeases expressed in Xenopus oocytes (46) revealed that they are electrogenic proton symporters (Fig. 3) that are apparently able to concentrate their nucleoside substrates by using the strong proton electrochemical gradient across the parasite plasma membrane. Presumably, this concentrative mode of action and the low apparent Kms, which are ∼20- to 100-fold lower than those for the mammalian ENTs, allow the purine-requiring parasites to compete effectively with their hosts for these essential nutrients.
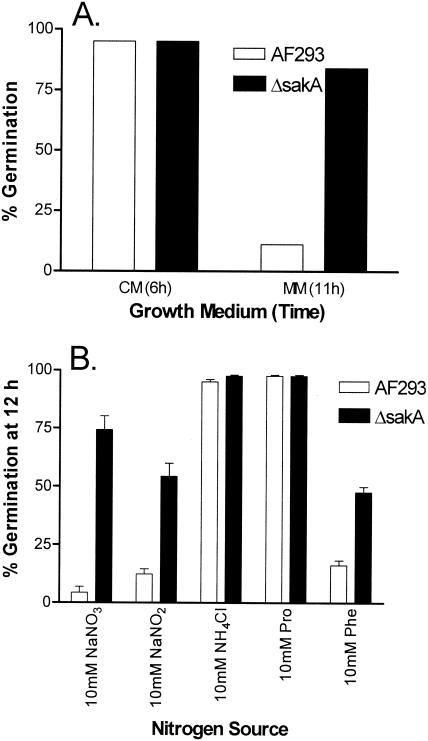
FIG. 3.
Two-electrode voltage clamp experiments demonstrate that LdNT2 and LdNT1.2 are electrogenic proton symporters. Each permease was expressed in Xenopus oocytes, and transmembrane currents [I (nA) or I (normalized)] specifically induced by each substrate were measured over a range of command potentials [Vm (mV)]. Inward-directed (negative) currents that increase at more negatively polarized membrane potentials are consistent with the cotransport of protons along with nucleoside substrates. For LdNT2 (A), significant currents were generated for the substrates inosine and guanosine but not for the nucleosides adenosine and thymidine, which are not substrates for the LdNT2 permease. For LdNT1.2 (B), adenosine-induced currents were measured at pHs 6.5, 7.5, and 8.5. The pronounced increase in current magnitude with increasing proton concentrations is consistent with proton symport. Reproduced from reference 46 with permission of the publisher.
The first protozoan nucleobase permease to be cloned and functionally expressed (28, 42) was the LmaNT3 transporter from L. major. This permease was initially identified as a homolog of LdNT1.1 in a search of the L. major database (http://www.ebi.ac.uk/parasites/leish.html), with 33% amino acid sequence identity between the two open reading frames (ORFs). The expression of LmaNT3 in Xenopus oocytes demonstrated that it transported hypoxanthine, xanthine, adenine, and guanine with apparent Kms ranging from 8 to 16 μM but that it did not transport nucleosides. Parallel studies (28) identified a related nucleobase permease from T. brucei, designated TbNT8.1, that shared 65% amino acid identity with LmaNT3. These results demonstrated that these, and likely other, parasite nucleobase permeases belong to the ENT family and not, for instance, to one of the three families previously identified in bacteria, fungi, or plants. The identities and substrate specificities of the three currently known Leishmania nucleoside and nucleobase permeases are tabulated in Table 1. In addition, a fourth member of the ENT family, LmaNT4, has been identified from the L. major genome sequencing project. This permease is currently being characterized.
TABLE 1.
Purinc transporters from Leishmania and T. brucei
| Transporter or organism | Systematic namea | Substratesb | Referencec |
|---|---|---|---|
| Leishmania | |||
| LdNT1.1 | AF065311, | Ado, Urd, Thy, Cyd | 51 |
| LdNT1.2 | AF041473 | ||
| LdNT2 | AF245276 | Guo, Ino | 12 |
| LmaNT3 | LmjF13.1210 | Hyp, Xan, Ade, Gua | 42 |
| LmaNT4 | LmjF11.0550 | Unknown | Unpublished results |
| T. brucei | |||
| TbAT1 | AF152369 | Ado, Ade | 36 |
| TbNT2 | AF153409 | Ado, Guo, Ino | 44 |
| TbNT2/927 | Tb927.2.6150 | Ado, Guo, Ino | 43 |
| TbNT3 | Tb927.2.6200 | Unknown | 43 |
| TbNT4 | Tb927.2.6220 | Unknown | 43 |
| TbNT5 | Tb927.2.6240 | Ado, Guo, Ino, Hyp | 43 |
| TbNT6 | Tb927.2.6320 | Ado, Guo, Ino, Hyp | 43 |
| TbNT7 | Tb927.2.6280 | Ado, Guo, Ino, Hyp | 43 |
| TbNT8.1 | AF516605 | Hyp, Xan, Ade, Gua | 28 |
| TbNBT1 | AY204876 | Hyp, Xan, Ade, Gua, Guo, Ino | 8 |
| TbNT9 | 90.t00137 | Ado, Guo, Ino, Hyp | Unpublished results |
| TbNT10 | Tb09.160.5480 | Ado, Guo, Ino | Unpublished results |
| TbNT11.1 | TRYP_X.469fIL.glc1 | Unknown | Unpublished results |
| TbNT11.2 | TRYP_X.469fIL.glc2 |
The systematic names are from GeneDB (http://www.genedb.org).
Ado, adenosine; Guo, guanosine; Ino, inosine; Urd, uridine; Thd, thymidine; Cyd, cytidine; Hyp, hypoxanthine; Xan, xanthine; Ade, adenine; Gua, guanine.
Unpublished results are from the S. Landfear laboratory.
NUCLEOSIDE AND NUCLEOBASE PERMEASES IN T. BRUCEI
The first nucleoside transporter gene from African trypanosomes (36), TbAT1, was cloned by functional complementation of a strain of Saccharomyces cerevisiae that was naturally deficient in purine nucleoside uptake and mutationally deficient in purine biosynthesis. Expression of the TbAT1 permease allowed this yeast strain to grow with exogenous adenosine as the sole purine source. A functional characterization revealed that TbAT1 possessed high-affinity transport activities for both adenosine and adenine and was expressed in BF parasites, confirming that it was the P2 transporter previously identified in BF trypanosomes.
Subsequently, another ENT family member, TbNT2, was identified by a homology search of the T. brucei genome database (http://parsun1.path.cam.ac.uk), using LdNT1.1 as the query sequence. The expression of TbNT2 in Xenopus oocytes revealed that it transported adenosine, inosine, and guanosine and thus qualified as a P1-type transporter (44). Continuing studies revealed a cluster of six genes (43), designated TbNT2 to TbNT7, whose ORFs were ∼85% identical to that of TbNT2. Expression in oocytes revealed that TbNT2, TbNT5, TbNT6, and TbNT7 all transported adenosine, inosine, and guanosine with Kms of about 1 μM but that the last three members of this family also transported the nucleobase hypoxanthine with Kms of ∼25 μM. Hence, like TbAT1, these three permeases were nucleoside and nucleobase transporters. RNAs from all genes in the cluster were expressed in BF parasites, but TbNT2 and TbNT5 mRNAs were also detectable in PF parasites. Thus, different members of this transporter family possessed distinct substrate specificities and life cycle expression patterns. In contrast, TbNT3 and TbNT4 did not transport nucleosides or nucleobases when expressed in oocytes, and their function is currently unknown. The substrate specificities of these and other T. brucei ENT family members are catalogued in Table 1.
An additional examination of the T. brucei database has identified four additional ENT family members, referred to as TbNT8, TbNT9, TbNT10, and TbNT11. Studies that are currently under way have revealed that TbNT9 expressed in oocytes recognizes adenosine, inosine, guanosine, and hypoxanthine, similar to TbNT5 to TbNT7. The TbNT10 gene has been expressed in nucleoside-nucleobase transport-deficient S. cerevisiae and was shown to encode a high-affinity purine nucleoside transporter (M. A. Sanchez, unpublished data). It is particularly interesting that TbNT10 mRNA and protein are expressed primarily in the stumpy form of the parasite life cycle (K. Matthews, unpublished data), which is a nondividing developmental form present in the bloodstream of the infected mammalian host that is adapted for infection of the tsetse fly (50). These results suggest that TbNT10 might subserve some unique function in the stumpy form of the life cycle. The TbNT11 transporters, which are represented by two very closely related ORFs, TbNT11.1 and TbNT11.2, have not been functionally characterized to date.
TbNT8 represents a family of clustered genes that carry closely related but nonidentical ORFs (28). The TbNT8.1 permease has been functionally expressed in both Xenopus oocytes and nucleoside-nucleobase transport-deficient yeast (28). A detailed functional characterization in yeast revealed that TbNT8.1 is a purine nucleobase transporter similar in function to the closely related LmaNT3 permease and has properties most similar to the H1 nucleobase transporter identified in intact PF parasites. TbNT8 mRNAs are expressed in both PF parasites and BF parasites but are more abundant in PF parasites. An independent study (8) identified what is apparently another member of the TbNT8 family that was designated TbNBT1. Its expression in yeast revealed high-affinity transport activities for hypoxanthine, xanthine, adenine, guanine, guanosine, and allopurinol and a moderate-affinity activity for inosine. Further examination of intact PF parasites identified a transport activity that was indistinguishable from that of TbNBT1, denoted H4. TbNBT1 mRNAs were present at similar levels in BF and PF parasites.
STRUCTURE-FUNCTION STUDIES ON ENT FAMILY PERMEASES
Much of the molecular genetic work over the past few years has been devoted to identifying and characterizing the genes that encode various nucleoside and nucleobase transporters of Leishmania and T. brucei. The fruits of these studies now allow us to probe in molecular detail the functions of this important family of permeases. Furthermore, since mammalian and protozoan members of the ENT family share many properties, results obtained with permeases from both types of organism will likely provide illuminating comparisons.
Work on ENTs from both parasites and mammals has begun to identify functionally important domains of these permeases. For example, the introduction of N-glycosylation signals into the human ENT (hENT1) (48) has confirmed experimentally the 11-TMD topology that is likely to apply to all family members. Furthermore, the construction of chimeras between hENT1 and the rat homolog rENT1 that differ in their sensitivities to the high-affinity competitive inhibitor NBMPR revealed that the segment encompassing TMDs 3 to 6 is likely to interact with substrates (47). Additional work revealed that the rENT2 permease transported nucleobases as well as nucleosides (55) and that a segment of rENT2 encompassing TMDs 5 and 6 could confer nucleobase transport activity upon hENT1, thus implicating this more discrete domain in substrate recognition. Mutagenesis of hENT1 and hENT2, which differ in their sensitivities to the competitive inhibitors dipyridamole and dilazep, revealed that residue 33, located at the end of the predicted TMD1, controls sensitivity to these inhibitors (53). Site-directed mutagenesis of G179 within TMD5 of hENT1 resulted in impaired transport activity and a reduced sensitivity to NBMPR, suggesting a potential role for this helix in substrate recognition. Finally, covalent modification with p-chloromercuriphenyl sulfonate of C140 in TMD4 of rENT2 resulted in the loss of transport activity, and this modification could be protected by coincubation with the substrate uridine (54), suggesting that TMD4 likely forms part of the substrate translocation channel.
Molecular genetic studies of LdNT1.1 and LdNT2 have revealed several functionally important components of these ENTs that are likely to play significant roles in many or all ENTs. Sequencing of the LdNT1.1 genes from the transport-deficient TUBA5 mutant revealed the presence of two mutant alleles that represented different point mutations (52). One allele encompassed a G187D mutation in the predicted TMD5 and the other had a C337Y mutation in the predicted TMD7, revealing that the TUBA5 line was a compound heterozygote. Site-directed mutagenesis of wild-type LdNT1.1 revealed that each mutation was impaired in transport activity but that both mutant proteins trafficked correctly to the plasma membrane; consequently, each mutation abolished the innate transport activity of the permease. Of particular interest was the observation that the site-directed mutant G187A retained the ability to transport adenosine but not the substrate uridine, i.e., G187A induced a change of substrate specificity. These results strongly implied that TMD5 of LdNT1.1 interacts with substrates. A confirmation of this hypothesis was obtained recently by use of the substituted cysteine accessibility method (31), for which the accessibility of each position of TMD5 to substrates was monitored. Substituted cysteine residues on the hydrophilic face of the amphipathic TMD5 were susceptible to covalent modification by sulfhydryl-specific reagents, and their modification could be protected by substrates (R. Valdés, G. Vasudevan, D. Conklin, and S. M. Landfear, submitted for publication). In another study (4), two residues within TMD8 of LdNT2, namely D389 and R393, that are conserved among both protozoan and mammalian ENTs were examined by site-directed mutagenesis to determine their potential roles in the transporter function. Even the conservative D389E mutation drastically impaired the transporter function, despite the fact that the mutant permease was targeted correctly to the plasma membrane, suggesting an essential role of D389 in permease activity. The R393K mutant was a functional transporter, but mutations that removed the positive charge, such as R393L, resulted in very poor trafficking to the plasma membrane, suggesting a role for R393 in establishing the permease structure. Intriguingly, D389K/R393D and D389N/R393N double mutants were incompetent for transport but trafficked properly to the plasma membrane, suggesting that an interaction between D389 and R393 is important for membrane targeting. The locations of functionally important residues within the topology model of the ENTs are indicated in Fig. 2.
POSSIBLE INTERACTION OF PARASITE NUCLEOSIDE TRANSPORTERS WITH NUCLEOTIDE AMP
In general, plasma membrane permeases of eukaryotes are thought not to transport charged nucleotides such as AMP, ADP, and ATP. However, the electrophysiological investigations of the L. donovani ENTs mentioned above (46) revealed that the application of AMP to Xenopus oocytes expressing LdNT1.1 or LdNT1.2 generated substrate-dependent currents and that the magnitudes of these currents were dependent upon the AMP concentration, with an apparent Km of 9.1 ± 3.2 μM (Fig. 4). Furthermore, the application of [3H]AMP to oocytes expressing LdNT1.1 or LdNT1.2, but not to water-injected oocytes, resulted in a robust uptake of the label, without the generation of [3H]adenosine in the medium surrounding the oocyte (S. M. Landfear, unpublished results). This latter result suggests that the uptake of the label was not due simply to hydrolysis of AMP with a release of free adenosine into the medium followed by transport of the released nucleoside. In contrast, the more highly phosphorylated nucleotides ADP and ATP were not taken up by either permease. Parallel studies (M. A. Sanchez, unpublished results) of the T. brucei permeases TbNT2, TbNT5, and TbNT10 revealed that these transporters also mediate the uptake of label from [3H]AMP. These results imply that various parasite ENTs may be able to use AMP as an alternate source for purine salvage and suggest a novel activity for this family of permeases. Detailed studies on the interaction of LdNT1.1 and LdNT1.2 with AMP are currently under way to determine whether AMP is a substrate for these permeases.
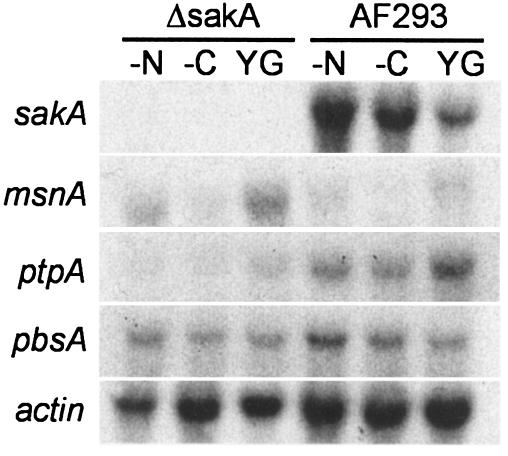
FIG. 4.
AMP induces transmembrane currents in oocytes expressing the LdNT1.2 nucleoside transporter. Two-electrode voltage clamp experiments were performed on LdNT1.2-expressing oocytes essentially as described for Fig. 3. (A) Current-voltage curves demonstrating that increasing concentrations of AMP (300 nM to 100 μM) induce increasing inward-directed currents. (B) AMP-induced currents saturated with increasing AMP concentrations. Reproduced from reference 46 with permission of the publisher.
NONRECIPROCAL INHIBITION OF SUBSTRATES FOR PARASITE ENTS
A conventional transport model invoking an alternating access pore (33) that recognizes multiple structurally related substrates predicts that each substrate will be able to reciprocally inhibit the uptake of the other substrates. Kinetic experiments employing ENTs from both Leishmania and trypanosomes have uncovered several striking exceptions to this straightforward prediction. For the LmaNT3 nucleobase transporter, hypoxanthine completely inhibited the uptake of [3H]xanthine, with an apparent Ki of 0.72 μM, while xanthine at concentrations up to 1 mM only inhibited the transport of [3H]hypoxanthine by 50 to 60% (42). The partial inhibition of hypoxanthine uptake by xanthine was also observed for intact L. major promastigotes as well as for LmaNT3 heterologously expressed in either oocytes or yeast. In contrast, adenine and guanine were able to completely inhibit the uptake of [3H]hypoxanthine. For the related TbNT8.1 permease expressed in yeast, hypoxanthine completely inhibited the uptake of [3H]guanine, but guanine only inhibited the uptake of [3H]hypoxanthine by a maximal value of 75% (28). In experiments using LdNT1.2 expressed in oocytes and examining a range of inhibitor concentrations, from 10−9 to 10−3 M, adenosine completely inhibited the import of [3H]AMP while AMP only inhibited the uptake of [3H]adenosine by a maximal value of ∼65% (S. M. Landfear, unpublished results). While the mechanistic explanation for these nonreciprocal patterns of inhibition is uncertain, the results imply that a simple model of competitive inhibition by multiple closely related substrates that bind to overlapping sites may not always apply for ENTs.
SUBCELLULAR LOCATION OF PARASITE ENTS
The subcellular distribution of LdNT1.1, LdNT1.2 (52), LdNT2 (4), LmaNT3 (M. A. Sanchez, unpublished results), and TbNT8.1 (28) has been examined by the fusion of green fluorescent protein to the cytoplasmically oriented NH2 termini of these transporters. In all cases, the fusion proteins were located primarily on the parasite surface, specifically on the pellicular plasma membrane, the flagellar pocket, and the flagellar membrane. Furthermore, all the NH2-terminally tagged transporters were functional and exhibited appropriate ligand selectivities. One intriguing observation was that the fraction of the R393L mutant of LdNT2 that did traffic to the parasite surface was largely located on the flagellar membrane, suggesting that this mutation within a predicted TMD induced a redistribution of the permease over the parasite surface membrane.
REGULATION OF ENT EXPRESSION IN KINETOPLASTID PARASITES
Several publications have documented that parasite ENTs can be strongly regulated both during the growth cycle and by the substrates of the permeases. Initial studies by two groups (2, 25) using C. luciliae revealed that the rates of purine nucleoside and nucleobase uptake were dramatically upregulated by purine starvation and by the stage of the growth cycle. Subsequent studies demonstrated that the CfNT1 and CfNT2 nucleoside permease activities of C. fasciculata were robustly expressed during mid-logarithmic growth but were dramatically downregulated during the stationary phase (21). Furthermore, permease activity was stimulated 5- to 15-fold in purine-depleted medium. In addition, the T. brucei P1 transporter was similarly upregulated by purine starvation. Studies of adenosine uptake by L. donovani promastigotes (45) have also revealed that the depletion of adenosine (a substrate of LdNT1), but not guanosine (not a substrate of LdNT1), from the culture medium upregulated adenosine transport ∼10-fold, whereas adenosine or guanosine transport activity was downregulated >20-fold by the transition from the logarithmic to the stationary phase (D. Rodriguez-Contreras, R. Valdés, and N. Carter, unpublished results). The upregulation of these and other (45) transporters by substrate depletion indicates that Kinetoplastid parasites employ a regulatory mechanism to salvage nutrients more efficiently under conditions of relative starvation, and a common pathway is likely to control the expression of multiple permeases in response to ligand concentrations. The mechanistic details of these regulatory processes remain to be elucidated.
ALTERATIONS IN PARASITE PURINE PERMEASES LEADING TO DRUG RESISTANCE
Since parasite purine transporters mediate the uptake of various antiparasitic drugs, both purine analogs and nonanalogs, the alteration or loss of transport function can induce partial or pronounced resistance to these therapeutic agents or cytotoxic compounds. One example of considerable interest emerged from early studies of the T. brucei P2 permease. A melarsen-resistant clone (67-fold more resistant than the parent to melarsoprol), derived in vivo from a susceptible parent clone, lacked a functional P2 adenosine-adenine transporter, suggesting that this permease may be responsible for the transport of melaminophenyl arsenicals (13). Subsequent work demonstrated that both melarsoprol and the diamidine drug pentamidine are high-affinity inhibitors of the P2 transporter (11, 13), strongly intimating that this permease constitutes a route of uptake for these drugs, both of which are administered to treat African sleeping sickness. A hypothesis has been advanced (9) suggesting that limited structural similarities between the 6-aminopurines, adenosine and adenine, and melarsoprol and pentamidine may be responsible for their common recognition by the P2 transporter. After the cloning of the TbAT1 transporter gene that encodes the P2 permease, it became possible to examine the sequence of this gene from the STIB 777S melarsen-sensitive parent and the derived STIB 777R melarsen-resistant clones. The ORF from the drug-resistant strain exhibited 10 nucleotide differences compared to that from the STIB 777S drug-sensitive strain, and six of these differences resulted in amino acid changes (36). While expression of the original TbAT1 gene in yeast conferred both adenosine transport and melarsen sensitivity, expression of the TbAT1r gene from the STIB 777R strain did not bestow either property on the transformed yeast cells. For further probing of the role of TbAT1 in the uptake of and resistance to drugs, a tbat1-null mutant was generated by targeted gene replacement (38). This null mutant was deficient in P2 transport activity but was surprisingly only slightly resistant to either melaminophenyl arsenicals or pentamidine. These results imply that both drugs have alternate routes of entry into BF trypanosomes, and indeed the existence of two other pentamidine transport proteins, HAPT1 and LAPT1, has been postulated. Nonetheless, the two- to threefold resistance to melaminophenyl arsenicals observed for this null mutant may still be clinically significant and is consistent with the absence of pronounced arsenical resistance in clinical isolates from melarsoprol-refractory patients (38). Another study of field isolates from distinct parts of Africa (37) revealed that many of the TbAT1 genes isolated from patients with relapsing infections after melarsoprol treatment exhibited the same set of nine mutations and that one relapse isolate was missing the TbAT1 gene altogether, again implicating this gene in drug resistance. It is difficult to fathom how a drug-resistant allele with so many of the same polymorphisms could have arisen independently on multiple occasions. However, many other isolates from relapse patients possessed wild-type TbAT1 genes, suggesting that drug refractoriness was not solely the result of mutational alterations in the TbAT1 gene.
Two examples from L. donovani, already referred to above, established that mutational inactivation of the LdNT1.1 (52) and LdNT2 (12) permeases conferred resistance to the cytotoxic purine analogs tubercidin and formycin B, respectively (5), as these two permeases constitute the pathways for uptake of these compounds. Furthermore, a doubly resistant mutant selected by sequential plating on tubercidin and then formycin B was defective in the uptake of all substrates of LdNT1.1 and LdNT2 but was able to grow on purine nucleobases, which permeate through the NT3 transporter. These studies with trypanosomes and Leishmania underscore the relevance of purine transporters to drug delivery and resistance in these pathogens.
POWER OF FORWARD GENETIC ANALYSIS FOR DISSECTION OF PURINE TRANSPORTER FUNCTION
A corollary of the ability of parasite purine permeases to transport cytotoxic compounds is that such reagents can be employed in strong genetic selections to identify transport-deficient mutants by nonbiased forward genetic strategies (5). One significant advantage of this approach is that it does not rely upon preconceived notions of what residues should be important for transport function but allows the genetic system to instruct us concerning what is required to make a functional permease. While initial loss-of-function mutants obtained by such screens could be of limited value in their own right, as they result in nonfunctional carriers, more conservative mutations introduced into the site of the original transport-deficient mutation often produce partial loss-of-function mutants that can be analyzed in more detail to dissect the role of the wild-type residue. This strategy has proven effective for identifying structurally and functionally important determinants in LdNT1.1, including residues involved in the determination of substrate specificity (52). Thus, the purine permeases offer one of the few transport systems among eukaryotes that can be comprehensively studied by classical genetic approaches. This property offers a significant advantage for structure-function analyses compared to most other systems. Site-directed mutagenesis, or the so-called reverse genetics that is available for the study of any permease, is a valuable avenue of investigation and can ultimately identify multiple functionally important residues. This approach has been used with remarkable success with the lactose permease of Escherichia coli (32), for which the strategy has identified six residues that are critical for transporter function. Nonetheless, this exercise was extremely labor-intensive and required the systematic mutagenesis of almost every residue in the permease. In contrast, the forward genetic approach allows the genetic selection to identify candidate residues of functional significance, thus removing much of the conceptual bias and labor required for discovery.
PURINE TRANSPORTERS AMONG THE APICOMPLEXA
The first purine transporter gene that was cloned from a member of the Apicomplexa was the TgAT gene of Toxoplasma gondii (15). This gene was identified by insertional mutagenesis of tachyzoites followed by selection on the cytotoxic adenosine analog adenine arabinoside (AraA). The permease is a member of the ENT family, transports [3H]adenosine when expressed in Xenopus oocytes, and is inhibited to varying extents by 500 μM adenosine, inosine, guanosine, hypoxanthine, guanine, and uridine, suggesting a broad substrate specificity. Since the insertional mutant was deficient in adenosine uptake, TgAT is the sole functional adenosine transporter in tachyzoites of Toxoplasma gondii. Because TgAT-deficient Toxoplasma gondii cells are viable and retain inosine and hypoxanthine uptake capabilities, other purine transporters must exist in this parasite.
Two groups have reported the cloning and functional expression in Xenopus oocytes of a gene encoding a purine transporter of the ENT family from P. falciparum, designated either PfNT1 (10) or PfENT1 (39). The investigations by Parker et al. showed that PfENT1 transports both the nucleoside adenosine and the nucleobase adenine, with identical Km values of 0.32 mM, and guanine and hypoxanthine were also transported. Carter et al. found that PfNT1 transported d-adenosine with a high affinity (apparent Km value of 13.2 μM) and d-inosine with a moderate affinity (Km value of 253 μM) and that [3H]adenosine transport was strongly inhibited by 500 μM adenosine, inosine, guanosine, thymidine, or uridine but was only inhibited ∼30% by the purine nucleobases at concentrations of 500 μM. The uptake of [3H]adenine and [3H]hypoxanthine by PfNT1 produced Km values of 0.45 and 1.1 mM, respectively (N. Carter and B. Ullman, unpublished data), indicating that nucleobases are relatively low-affinity substrates for PfNT1 compared to the high-affinity transport measured for adenosine. One intriguing observation (10) was that unlike the mammalian ENTs, PfNT1 also mediated the uptake of l-adenosine, albeit with a significantly lower affinity than d-adenosine (Km value of >500 μM). An antiserum raised against the hydrophilic NH2-terminal domain of PfNT1 was used to localize the permease to the plasma membrane of intraerythrocytic malaria parasites and to demonstrate that expression of the permease is upregulated during the late trophozoite and schizont stages of the life cycle (41). The potential reliance of bloodstream-stage parasites on purine uptake through this permease makes it worthy of consideration as a potential drug target.
SUMMARY AND PERSPECTIVES
The importance of purine salvage and transport to the biochemistry and pharmacology of parasitic protozoa has been appreciated for some time (7). The recent identification of cloned genes encoding nucleoside and nucleobase transporters in various parasites has advanced our ability to probe these essential uptake processes at the molecular and genetic levels. With these molecular reagents in hand, it should be possible to investigate the structure and function of the permeases at the individual amino acid level, to examine the role of individual and multiple transporters in the biochemistry of the parasites by mutagenesis and the generation of null mutants by targeted gene replacement, to probe the mechanisms of regulation of expression of the carriers in response to the physiological environment of the parasite, and to monitor the subcellular trafficking of individual transporters.
Several important conclusions have already emerged from work on parasite purine permeases. First, all of the transporters identified to date among the protozoa are members of the ENT family and are unrelated to concentrative nucleoside transporters. Second, transporters dedicated to the uptake of nucleobases rather than nucleosides are also ENT family members and are unrelated to nucleobase permeases that were previously identified in plants and other lower eukaryotes. Furthermore, at least some of the parasite ENTs appear to function as active proton symporters rather than as the equilibrative transporters typified by mammalian ENTs. Nonetheless, many common features of sequence and secondary structure between mammalian and protozoan ENTs imply that much of what we learn regarding basic functional properties of ENTs from each type of organism will be useful for understanding the entire family of permeases.
Some of the parasitic protozoa appear to have relatively limited numbers of purine transporters, such as Cryptosporidium parvum, which has only one known ENT in its genome, and Leishmania species, for which three distinct permeases and one closely related isoform have been characterized to date and for which one additional uncharacterized ENT has been identified. In contrast, T. brucei cells contain at least 11 distinct ENT permeases or more, if closely related isoforms of TbNT8 and TbNT11 are considered. It is currently unclear why one genus of parasite should be able to thrive with a limited number of purine transporters while another parasite from a relatively closely related genus expresses a plethora of such carriers. It is equally unclear why parasite permeases differ so substantially in substrate specificities and affinities. However, significant differences in the physiological niches and life cycle stages of different parasites may ultimately provide at least part of the explanation. The multiplicity of purine transporters expressed even by a relatively “discrete” parasite, such as L. major, would appear to make daunting the challenge of designing therapeutic inhibitors that are specific for all of the parasite permeases but sparing of the homologous mammalian transporters. In fact, effective therapeutic regimens such as the application of allopurinol for the treatment of leishmaniasis and Chagas' disease (35) have relied upon these permeases to deliver subversive substrates rather than on the inhibition of their uptake activities. However, this consideration underscores the potential importance of parasite purine permeases as determinants of drug resistance. The scope of basic and applied problems in parasite biology that the purine permeases impact implies that the study of these transporters will continue to provide illuminating insights for some time to come.
Acknowledgments
This research was supported by grants AI44138 and AI25920 (to S.M.L.) as well as AI23682 and AI51507 (to B.U.) from the National Institutes of Health and by grant 0360022Z from the American Heart Association (to N.S.C.).
REFERENCES
- 1.Acimovic, Y., and I. R. Coe. 2002. Molecular evolution of the equilibrative nucleoside transporter family: identification of novel family members in prokaryotes and eukaryotes. Mol. Biol. E 19:2199-2210. [DOI] [PubMed] [Google Scholar]
- 2.Alleman, M. M., and M. Gottlieb. 1996. Enhanced acquisition of purine nucleosides and nucleobases by purine-starved Crithidia luciliae. Mol. Biochem. Parasitol. 76:279-287. [DOI] [PubMed] [Google Scholar]
- 3.Al-Salabi, M. I., L. J. M. Wallace, and H. P. de Koning. 2003. A Leishmania major nucleobase transporter responsible for allopurinol uptake is a functional homolog of the Trypanosoma brucei H2 transporter. Mol. Pharmacol. 63:814-820. [DOI] [PubMed] [Google Scholar]
- 4.Arastu-Kapur, S., E. Ford, B. Ullman, and N. S. Carter. 2003. Functional analysis of an inosine-guanosine transporter from Leishmania donovani: the role of conserved residues, aspartate 389 and arginine 393. J. Biol. Chem. 278:33327-33333. [DOI] [PubMed] [Google Scholar]
- 5.Aronow, B., K. Kaur, K. McCartan, and B. Ullman. 1987. Two high affinity nucleoside transporters in Leishmania donovani. Mol. Biochem. Parasitol. 22:29-37. [DOI] [PubMed] [Google Scholar]
- 6.Baldwin, S. A., J. R. Mackey, C. E. Cass, and J. D. Young. 1999. Nucleoside transporters: molecular biology and implications for therapeutic development. Mol. Med. Today 5:216-224. [DOI] [PubMed] [Google Scholar]
- 7.Berens, R. L., E. C. Krug, and J. J. Marr. 1995. Purine and pyrimidine metabolism, p. 89-117. In J. J. Marr and M. Müller (ed.), Biochemistry and molecular biology of parasites. Academic Press, New York, N.Y.
- 8.Burchmore, R. J. S., L. J. M. Wallace, D. Candlish, M. I. Al-Salabi, P. R. Beal, M. P. Barrett, S. A. Baldwin, and H. P. de Koning. 2003. Cloning, heterologous expression, and in situ characterization of the first high affinity nucleobase transporter from a protozoan. J. Biol. Chem. 278:23502-23507. [DOI] [PubMed] [Google Scholar]
- 9.Carter, N. S., M. P. Barrett, and H. P. de Koning. 1999. A drug resistance determinant in Trypanosoma brucei. Trends Microbiol. 7:469-471. [DOI] [PubMed] [Google Scholar]
- 10.Carter, N. S., C. Ben Mamoun, W. Liu, E. O. Silva, S. M. Landfear, D. E. Goldberg, and B. Ullman. 2000. Isolation and functional characterization of the PfNT1 nucleoside transporter gene from Plasmodium falciparum. J. Biol. Chem. 275:10683-10691. [DOI] [PubMed] [Google Scholar]
- 11.Carter, N. S., B. J. Berger, and A. H. Fairlamb. 1995. Uptake of diamidine drugs by the P2 transporter in melarsen-sensitive and -resistant Trypanosoma brucei brucei. J. Biol. Chem. 270:28153-28157. [DOI] [PubMed] [Google Scholar]
- 12.Carter, N. S., M. E. Drew, M. Sanchez, G. Vasudevan, S. M. Landfear, and B. Ullman. 2000. Cloning of a novel inosine-guanosine transporter gene from Leishmania donovani by functional rescue of a transport-deficient mutant. J. Biol. Chem. 275:20935-20941. [DOI] [PubMed] [Google Scholar]
- 13.Carter, N. S., and A. H. Fairlamb. 1993. Arsenical-resistant trypanosomes lack an unusual adenine/adenosine transporter. Nature 361:173-175. [DOI] [PubMed] [Google Scholar]
- 14.Carter, N. S., N. Rager, and B. Ullman. 2003. Purine and pyrimidine transport and metabolism, p. 197-223. In J. J. Marr, T. Nilsen, and R. Komuniecki (ed.), Molecular and medical parasitology. Academic Press, London, United Kingdom.
- 15.Chiang, C. W., N. Carter, W. J. Sullivan, Jr., R. G. Donald, D. S. Roos, F. N. Naguib, M. H. el Kouni, B. Ullman, and C. M. Wilson. 1999. The adenosine transporter of Toxoplasma gondii. Identification by insertional mutagenesis, cloning, and recombinant expression. J. Biol. Chem. 274:35255-35261. [DOI] [PubMed] [Google Scholar]
- 16.de Koning, H. P., and G. Diallinas. 2000. Nucleobase transporters. Mol. Membr. Biol. 75:75-94. [DOI] [PubMed] [Google Scholar]
- 17.de Koning, H. P., and S. M. Jarvis. 1998. A highly selective, high-affinity transporter for uracil in Trypanosoma brucei brucei: evidence for proton-dependent transport. Biochem. Cell Biol. 76:853-858. [DOI] [PubMed] [Google Scholar]
- 18.de Koning, H. P., and S. M. Jarvis. 1997. Hypoxanthine uptake through a purine-selective nucleobase transporter in Trypanosoma brucei brucei procyclic cells is driven by protomotive force. Eur. J. Biochem. 247:1102-1110. [DOI] [PubMed] [Google Scholar]
- 19.de Koning, H. P., and S. M. Jarvis. 1997. Purine nucleobase transport in bloodstream forms of Trypanosoma brucei brucei is mediated by two novel transporters. Mol. Biochem. Parasitol. 89:245-258. [DOI] [PubMed] [Google Scholar]
- 20.de Koning, H. P., C. J. Watson, and S. M. Jarvis. 1998. Characterization of a nucleoside/proton symporter in procyclic Trypanosoma brucei brucei. J. Biol. Chem. 273:9486-9494. [DOI] [PubMed] [Google Scholar]
- 21.de Koning, H. P., C. J. Watson, L. Sutcliffe, and S. M. Jarvis. 2000. Differential regulation of nucleoside and nucleobase transporters in Crithidia fasciculata and Trypanosoma brucei brucei. Mol. Biochem. Parasitol. 106:93-107. [DOI] [PubMed] [Google Scholar]
- 22.Finley, R. W., D. A. Cooney, and J. A. Dvorak. 1988. Nucleoside uptake in Trypanosoma cruzi: analysis of a mutant resistant to tubercidin. Mol. Biochem. Parasitol. 31:133-140. [DOI] [PubMed] [Google Scholar]
- 23.Ghosh, M., and T. Mukherjee. 2000. Stage-specific development of a novel adenosine transporter in Leishmania donovani amastigotes. Mol. Biochem. Parasitol. 108:93-99. [DOI] [PubMed] [Google Scholar]
- 24.Goldberg, B., N. Yarlett, J. Sufrin, D. Lloyd, and C. J. Bacchi. 1997. A unique transporter of S-adenosylmethionine in African trypanosomes. FASEB J. 11:256-260. [DOI] [PubMed] [Google Scholar]
- 25.Hall, S. T., C. J. Hillier, and A. M. Gero. 1996. Crithidia luciliae: regulation of purine nucleoside transport by extracellular purine concentrations. Exp. Parasitol. 83:314-321. [DOI] [PubMed] [Google Scholar]
- 26.Hall, S. T., J. I. Penny, A. M. Gero, and S. Krishna. 1998. Crithidia luciliae: functional expression of nucleoside and nucleobase transporters in Xenopus laevis oocytes. Exp. Parasitol. 90:181-188. [DOI] [PubMed] [Google Scholar]
- 27.Hansen, B. D., J. Perez-Arbelo, J. F. Wlakony, and L. D. Hendricks. 1982. The specificity of purine base and nucleoside uptake in promastigotes of Leishmania braziliensis panamensis. Parasitology 85:271-282. [DOI] [PubMed] [Google Scholar]
- 28.Henriques, C., M. Sanchez, R. Tryon, and S. M. Landfear. 2003. Molecular and functional characterization of the first nucleobase transporter gene from African trypanosomes. Mol. Biochem. Parasitol. 130:101-110. [DOI] [PubMed] [Google Scholar]
- 29.Hyde, R. J., C. E. Cass, J. D. Young, and S. A. Baldwin. 2001. The ENT family of eukaryote nucleoside and nucleobase transporters: recent advances in the investigation of structure/function relationships and the identification of novel isoforms. Mol. Membr. Biol. 18:53-63. [PubMed] [Google Scholar]
- 30.Iovannisci, D. M., K. Kaur, L. Young, and B. Ullman. 1984. Genetic analysis of nucleoside transport in Leishmania donovani. Mol. Cell. Biol. 4:1013-1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Javitch, J. A. 1998. Probing the structure of neurotransmitter transporters by substituted-cysteine accessibility method. Methods Enzymol. 296:331-346. [DOI] [PubMed] [Google Scholar]
- 32.Kaback, H. R., M. Sahin-Tóth, and A. B. Weinglass. 2001. The kamikaze approach to membrane transport. Nat. Rev. Mol. Cell. Biol. 2:610-620. [DOI] [PubMed] [Google Scholar]
- 33.Kavanaugh, M. P. 1998. Neurotransmitter transport: models in flux. Proc. Natl. Acad. Sci. USA 95:12737-12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kerby, D. R., and S. Detke. 1993. Reduced purine accumulation is encoded on an amplified DNA in Leishmania mexicana amazonensis resistant to toxic nucleosides. Mol. Biochem. Parasitol. 60:171-185. [DOI] [PubMed] [Google Scholar]
- 35.Marr, J. J. 1991. Purine analogs as chemotherapeutic agents in leishmaniasis and American trypanosomiasis. J. Lab. Clin. Med. 118:111-119. [PubMed] [Google Scholar]
- 36.Mäser, P., C. Sütterlin, A. Kralli, and R. Kaminsky. 1999. A nucleoside transporter from Trypanosoma brucei involved in drug resistance. Science 285:242-244. [DOI] [PubMed] [Google Scholar]
- 37.Matovu, E., F. Geiser, V. Schneider, P. Maser, J. C. K. Enyaru, R. Kaminsky, S. Gallati, and T. Seebeck. 2001. Genetic variants of the TbAT1 adenosine transporter from African trypanosomes in relapse infections following melarsoprol therapy. Mol. Biochem. Parasitol. 117:73-81. [DOI] [PubMed] [Google Scholar]
- 38.Matovu, E., M. L. Stewart, F. Geiser, R. Brun, P. Maser, L. J. M. Wallace, R. J. Burchmore, J. C. K. Enyaru, M. P. Barrett, R. Kaminsky, T. Seebeck, and H. P. de Koning. 2003. Mechanisms of arsenical and diamidine uptake and resistance in Trypanosoma brucei. Eukaryot. Cell 2:1003-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parker, M. D., R. J. Hyde, S. Y. M. Yao, L. McRobert, C. E. Cass, J. D. Young, G. A. McConkey, and S. A. Baldwin. 2000. Identification of a nucleoside/nucleobase transporter from Plasmodium falciparum, a novel target for anti-malarial chemotherapy. Biochem. J. 349:67-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phelouzat, M., M. Basselin, F. Lawrence, and M. Robert-Gero. 1995. Sinefungin shares AdoMet-uptake system to enter Leishmania donovani promastigotes. Biochem. J. 305:133-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rager, N., C. Ben Mamoun, N. S. Carter, D. E. Goldberg, and B. Ullman. 2001. Localization of the Plasmodium falciparum PfNT1 nucleoside transporter to the parasite plasma membrane. J. Biol. Chem. 276:41095-41099. [DOI] [PubMed] [Google Scholar]
- 42.Sanchez, M., R. Tryon, G. Vasudevan, and S. M. Landfear. 2004. Functional expression and characterisation of a purine nucleobase transporter gene from Leishmania major. Mol. Membr. Biol. 21:11-18. [DOI] [PubMed] [Google Scholar]
- 43.Sanchez, M. A., R. Tryon, J. Green, I. Boor, and S. M. Landfear. 2002. Six related nucleoside/nucleobase transporters from Trypanosoma brucei exhibit distinct biochemical functions. J. Biol. Chem. 277:21499-21504. [DOI] [PubMed] [Google Scholar]
- 44.Sanchez, M. A., B. Ullman, S. M. Landfear, and N. S. Carter. 1999. Cloning and functional expression of a gene encoding a P1 type nucleoside transporter from Trypanosoma brucei. J. Biol. Chem. 274:30244-30249. [DOI] [PubMed] [Google Scholar]
- 45.Seyfang, A., and S. M. Landfear. 1999. Substrate depletion upregulates uptake of myo-inositol, glucose and adenosine in Leishmania. Mol. Biochem. Parasitol. 104:121-130. [DOI] [PubMed] [Google Scholar]
- 46.Stein, A., G. Vasudevan, N. Carter, B. Ullman, S. M. Landfear, and M. P. Kavanaugh. 2003. Equilibrative nucleoside transporter family members from Leishmania donovani are electrogenic proton symporters. J. Biol. Chem. 278:35127-35134. [DOI] [PubMed] [Google Scholar]
- 47.Sundaram, M., S. Yao, A. M. L. Ng, M. Griffiths, C. E. Cass, S. A. Baldwin, and J. D. Young. 1998. Chimeric constructs between human and rat equilibrative nucleoside transporters (hENT1 and rENT1) reveal hENT1 structural domains interacting with coronary vasoactive drugs. J. Biol. Chem. 273:21519-21525. [DOI] [PubMed] [Google Scholar]
- 48.Sundaram, M., S. Y. M. Yao, J. C. Ingram, Z. A. Berry, F. Abidi, C. E. Cass, S. A. Baldwin, and J. D. Young. 2001. Topology of a human equilibrative, nitrobenzylthioinosine (NBMPR)-sensitive nucleoside transporter (hENT1) implicated in the cellular uptake of adenosine and anti-cancer drugs. J. Biol. Chem. 276:45270-45275. [DOI] [PubMed] [Google Scholar]
- 49.Ullman, B. 1984. Pyrazolopyrimidine metabolism in parasitic protozoa. Pharmaceut. Res. 1:194-203. [DOI] [PubMed] [Google Scholar]
- 50.van Deursen, F. J., S. K. Shahi, C. M. R. Turner, C. Hartmann, C. Guerra-Giraldez, K. R. Matthews, and C. E. Clayton. 2001. Characterisation of the growth and differentiation in vivo and in vitro of bloodstream-form Trypanosoma brucei strain TREU 927. Mol. Biochem. Parasitol. 112:163-171. [DOI] [PubMed] [Google Scholar]
- 51.Vasudevan, G., N. S. Carter, M. E. Drew, S. M. Beverley, M. A. Sanchez, A. Seyfang, B. Ullman, and S. M. Landfear. 1998. Cloning of Leishmania nucleoside transporter genes by rescue of a transport-deficient mutant. Proc. Natl. Acad. Sci. USA 95:9873-9878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vasudevan, G., B. Ullman, and S. M. Landfear. 2001. Point mutations in a nucleoside transporter gene from Leishmania donovani confer drug resistance and alter substrate selectivity. Proc. Natl. Acad. Sci. USA 98:6092-6097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Visser, F., M. F. Vickers, A. M. L. Ng, S. A. Baldwin, J. D. Young, and C. E. Cass. 2002. Mutation of residue 33 of human equilibrative nucleoside transporters 1 and 2 alters sensitivity to inhibition of transport by dilazep and dipyridamole. J. Biol. Chem. 277:395-401. [DOI] [PubMed] [Google Scholar]
- 54.Yao, D., M. Sundaram, E. G. Chomey, C. E. Cass, S. A. Baldwin, and J. D. Young. 2001. Identification of Cys140 in helix 4 as an exofacial cysteine residue within the substrate-translocation channel of rat equilibrative nitrobenzylthioinosine (NBMPR)-insensitive nucleoside transporter rENT2. Biochem. J. 353:387-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yao, S. Y. M., A. M. L. Ng, W. R. Muzyka, M. Griffiths, C. E. Cass, S. A. Baldwin, and J. D. Young. 1997. Molecular cloning and functional characterization of nitrobenzylthioinosine (NBMPR)-sensitive (es) and NBMPR-insensitive (ei) equilibrative nucleoside transporter proteins (rENT1 and rENT2) from rat tissues. J. Biol. Chem. 272:28423-28430. [DOI] [PubMed] [Google Scholar]