Abstract
Patients with lung cancer are often misdiagnosed as pulmonary tuberculosis leading to delay in the correct diagnosis as well as exposure to inappropriate medication. Several factors are responsible for this situation in developing countries, including lack of awareness, inadequate infrastructure and socio-economic factors. This article outlines the differences between the two diseases as well as features that would make a clinician suspect the right diagnosis early.
Keywords: misdiagnosis, biopsy confirmation, ATT
Introduction
Tuberculosis continues to be a major cause of morbidity and mortality worldwide. There are an estimated 8.8 million incident cases of tuberculosis globally.[1] An estimated 1.61 million people across the world are diagnosed with lung cancer annually.[2] Lung cancer is the most common cause of death from cancer in men all over the world.[3] In India, lung cancer was considered to be rare in the beginning of the century[4] but has now reached almost epidemic proportions.
A steady increase in the number of admissions to the tuberculosis hospitals of malignant disease associated with or simulating tuberculosis has accentuated the problem of accurate diagnosis of tuberculosis and malignancy. There are many similarities between both diseases like they both are very common, have high prevalence, involve lung parenchyma and above all, characterised by similar symptoms. But, there are many differences between these two entities like they have different etiologies (pulmonary tuberculosis is infectious while lung cancer is non-infectious disease), different consequences, and altogether different management. Delay in the diagnosis and treatment of lung cancer results in poorer outcome and lower survival.
Symptoms such as fever, cough, expectoration, hemoptysis, weight loss and anorexia are common to both tuberculosis and lung cancer. In India, where tuberculosis is spreading in an uncontrolled way, it is not uncommon to find a lung cancer patient being treated for tuberculosis initially. However, age of the patient, history of smoking, mediastinal symptoms such as hoarseness of voice, Superior Vena Cava (SVC) obstruction, and dysphagia favor the diagnosis of lung cancer. On examination, there may be signs of collapse or mass, clubbing and metastatic and non-metastatic complications of lung cancer.
Etiology and risk factors
Tuberculosis is caused by infection of lung with small aerobic non-motile bacillus Mycobacterium tuberculosis (MTB). It spreads through the air when people who have an active MTB infection cough, sneeze, or otherwise transmit their saliva through the air. Lung cancer is an etiologically complex disease in which multiple genes are involved in the pathogenesis via different pathways.[5] When these genes interact with the environmental factors, individual may develop lung cancer.
There are some common risk factors like smoking for both pulmonary tuberculosis and lung cancer. Smoking can facilitate the manifestation or detrimental effects of tuberculosis through a variety of mechanisms. First, because smokers tend to have a chronic cough which is also the hallmark symptom of tuberculosis. Diagnosis of tuberculosis may then be delayed leading to a worse prognosis and perhaps higher probability for relapse. Second, smoking is a cause for co-morbidities, such as chronic bronchitis, chronic airway obstruction, pulmonary emphysema as well as coronary heart disease, that may facilitate progression of TB-infection to disease, but also impair lung function in addition to that of tuberculosis alone leading to worse prognosis. Third, iron overload of macrophages in pulmonary tissue is discussed as a direct effect impairing cellular response to micro-organisms. And finally, one could speculate that smokers are less likely to adhere to therapy, at least in certain settings or in certain areas although this may not be a problem in areas that use directly observed therapy for the majority or all of the patients. Cigarette smoking is single most important risk factor for lung cancer. In patients with lung cancer, a history of active tobacco smoking is present in 87% of males and in 85% of females.[6] There is 10-fold increased risk of lung cancer in smokers and 20 times more risk in heavy smokers (< 20 cig/day). The relative risk of developing lung cancer is 2.64 for bidi smokers and 2.23 for cigarette smokers with 2.45 as the overall relative risk.[7]
Other risk factors for pulmonary tuberculosis include:
History of known close contact with someone who has active tuberculosis. Inhalation of airborne nuclei from an infected person is proportional to the amount of time spent in the same air space, the proximity of the person, and the degree of ventilation.
Immunocompromised status (e.g. those with an HIV infection, cancer, transplanted organs, and prolonged high-dose corticosteroid therapy)
Substance abuse (IV or injection drug users and alcoholics).
Any person without an adequate health care (the homeless, particularly children under age 15 years and young adults between ages 15 and 44 yrs)
Pre-existing medical conditions or special treatment (e.g. diabetes mellitus, chronic renal failure, malnourishment, hemodialysis, or transplanted organ)
Institutionalization (e.g. long-term care facilities, psychiatric institutions, prisons)
Living in overcrowded, substandard housing
Being a health care worker performing high-risk activities: Administration of aerosolized pentamidine and other medications, sputum induction procedures, bronchoscopy, suctioning, coughing procedures, caring for the immunosuppressed patient and administering anesthesia and related procedures (e.g. intubation, suctioning)
Other risk factors for lung cancer are
Passive smoking
Exposure to certain metals (chromium, cadmium, arsenic), some organic chemicals, radiation, air pollution.
Atmospheric and occupational agents known as carcinogens like Radon (well-established lung carcinogen), asbestos, arsenic, bischloromethyl ether, chromium, nickel, polycyclic aromatic compounds.
Some viruses like HPV and CMV.
Medical history of tuberculosis
Personal traits (such as having a family history of lung cancer).
Cytogenetic studies have identified many chromosomal changes in lung cancer with numerical abnormalities, and structural aberrations including deletions and translocations. Small cell lung cancer is associated with oncogenes, like c-myc, L-myc, N-myc, c-raf and tumor suppressor genes, like p53 and Rb. Non-small cell lung cancer is associated with K-ras, N-ras, H-ras, c-myc, c-raf and tumor suppressor genes like p16 and Rb genes
Clinical features
Pulmonary tuberculosis and lung cancer have common symptoms like cough, expectoration, fever, hemoptysis, weight loss, and breathlessness. However, careful history and examination can help clinician to suspect lung cancer.
History of tobacco smoking is generally present in cases of lung cancer while it may be present or absent in tuberculosis. Fever in tuberculosis is low grade with evening rise, whereas in lung cancer, it is non-specific. If the weight loss is sudden, it indicates malignancy rather than pulmonary tuberculosis in which weight loss is gradual. The commonest symptom of lung cancer at presentation are change in character of chronic cough (a cough that does not go away), hemoptysis, dyspnea, hoarseness of voice, chest pain (aggravated by deep breathing), unexplained weight loss and loss of appetite, non-resolving pneumonia and superior vena cava syndrome (localized edema of face and upper extremities, facial plethora, distended neck and chest veins).
Cough is by far the most common symptom at presentation in lung cancer, and any “new” cough that persists longer than 2 weeks in patients over the age of 40 years who are tobacco smokers should be regarded with suspicion of lung cancer. Hemoptysis, which is usually in the form of streaking of blood in sputum, is an alarming symptom that should always be thoroughly investigated. Dyspnea may arise due to central airway narrowing or because of partial or complete collapse of a distal segment of lung. Poorly localized chest discomfort occurs in up to 60% of patients at diagnosis. These symptoms usually occur with centrally-placed neoplasms like squamous cell variety, whereas peripheral neoplasm, commonly adenocarcinoma may cause no respiratory symptom at the time of diagnosis, which may follow a chest radiograph taken for some other reason or as a part of non-specific symptoms. Sometimes, hoarseness of voice is the only complaint, and it is due to vocal cord paralysis due to involvement of left recurrent laryngeal nerve. When these patients are asked to cough, they produce relative ineffectual expiratory noise so called “bovine cough,” lacking an explosive quality of normal cough. Clubbing of fingers and toes is frequently seen. Lymphatic spread is common and scalene and supraclavicular lymph glands are usually the first to be involved.
Approximately 1/3rd patients with lung cancer present with symptoms due to metastatic spread, like skeletal metastasis, which are commonly seen in small cell and large cell types. These may present with bone pain or even pathological fractures. Cerebral metastasis may present with progressive neurological symptoms. These symptoms can be present in case of tuberculosis also if there is involvement of spine known as Pott ’s disease.
Diagnosis
The diagnosis of tuberculosis and lung cancer can be difficult as symptoms of both diseases are similar. Currently, as the incidence of tuberculosis in the elderly tends to increase due to an increase in immune compromised status (diabetes, HIV etc.) and lung cancer is not rare in the youth, patient’s age is no more a good reference in differential diagnosis.[8] However, diagnosis of lung cancer in patients with tuberculosis or with residual effects of tuberculosis possesses some peculiarities. These depend on variety of clinical symptoms, clinical course, and site of cancer. In case of ineffective specific treatment of tuberculosis, existence of lung cancer should be presumed.[9] Proper clinical examination and investigative workup is needed to reach the correct diagnosis.
Radiology
Due to high TB prevalence and radiological similarities, a large number of lung cancer patients initially get wrongly treated for tuberculosis based on radiological picture alone.
At chest skiagram, tuberculosis may manifests as 5 main entities: Parenchymal disease, lymphadenopathy, miliary disease (evenly distributed diffuse small 2-3-mm nodules, with slight lower lobe predominance), pleural effusion, and cavitation. Parenchymal lesions are characterized by dense, homogeneous, or non-homogenous parenchymal consolidation in any lobe (mostly upper lobe predilection) and fibrotic changes. Mass with or without collapse is the commonest radiological finding in lung cancer.[10] Malignant lesions have irregular margins with radiating strands. Lung cancer may also reveal as hilar prominence (in case of central tumors), pulmonary nodule (in case of peripheral tumors), widening of the mediastinum (suggestive of spread to lymph nodes), total or partial atelectasis of a segment, lobe or lung (mechanical effect causing obstructive collapse), unresolving consolidation (pneumonia), cavitation (eccentric, irregular margin with nodularity), elevated diaphragm (caused by phrenic nerve palsy) or pleural effusion (25.1%). Other findings include rib erosion in 4.8% and lymphangitis in 2.8%. A normal chest x-ray is found in 0.4% of cases of lung cancer.[10]
A CT scan is frequently the second step either to follow-up on an abnormal chest X-ray finding, or to evaluate troublesome symptoms in those with a normal chest x-ray. Centrilobular densities in and around the small airways and “tree-in-bud” appearances were the most characteristic CT features of pulmonary tuberculosis. It is best non-invasive method for lung cancer. Lung mass is not visible on conventional X-rays unless they are larger than 5-6 mm in diameter. In the CT images, however, modern CT machines can detect lesions up to 1-2 mm in diameter, hence CT is more sensitive than chest radiography and it can accurately tell tumor site, size and invasion to adjoining structures such as mediastinum, chest wall etc. There are many features on CT scan, which suggest the diagnosis of lung cancer [Figures 1–2]:
Figure 1.
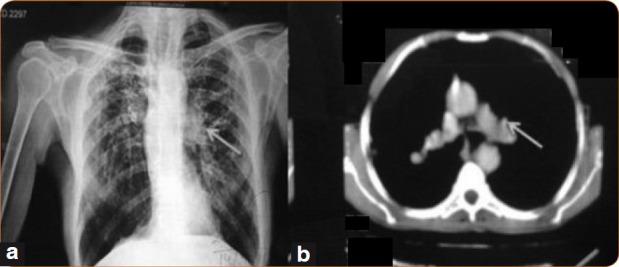
(a) CXR showing left hilar enlargement, (b) CT scan of same patient shows mass which on biopsy came out to be Squamous cell carcinoma
Figure 2.
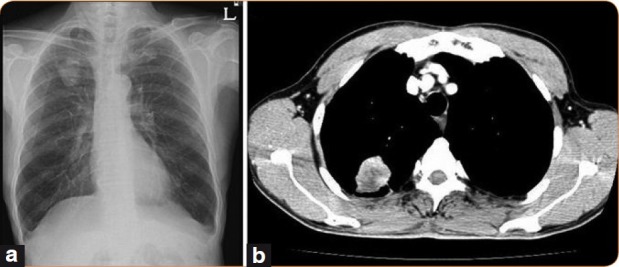
(a) Showing solitary pulmonary nodule on chest x-ray. (b) CT scan of same patient showing the mass posteriorly in right lower lobe.
Size
The larger the nodule, the more likely it is to be malignant.[11,12]
Margins
Lung cancers have irregular or speculated margins.[11,13,14] This feature cannot be used to exclude lung cancer as about 20% of malignant nodules have smooth margins.[15] Also, pulmonary tuberculosis in lung may present like nodule [Figure 3].
Figure 3.
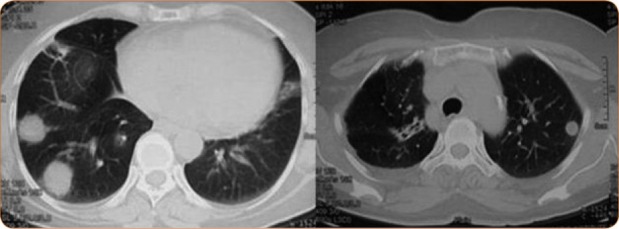
CT scan of a 62 years non-smoker female showing multiple and bilateral nodular opacities in right lower and left upper lobe which turned out to be pulmonary tuberculosis on histopathological examination done on CT guided biopsy
Internal morphology
Except for fat (attenuation, - 40 to - 120 Hounsfield units [HU]) and calcification within a nodule, an internal morphology is unreliable in distinguishing lung cancer. Calcification occurs in up to 14% of lung cancers and may be detected by CT. Cavitation can occur in lung cancer.
Growth
Lung cancers typically double in volume (an increase of 26% in diameter) between 30 and 400 days (average, 240 days). The use of CT scan thorax can improve the accuracy of growth assessment. It has been reported that growth can be detected in lung cancers as small as 5 mm when CT imaging is repeated within 30 days.
CT scan can very well assess the size of lymph node but cannot distinguish between neoplastic and reactive lymph nodes. CT guided FNAC or biopsy can be taken for histological diagnosis.
As pulmonary tuberculosis can present with any radiological appearance in countries like India where tuberculosis is rampant, sometime tuberculoma on CT scan can be misdiagnosed as lung cancer or metastasis due to its appearance resembling mass [Figures 3 and 4].
Figure 4.
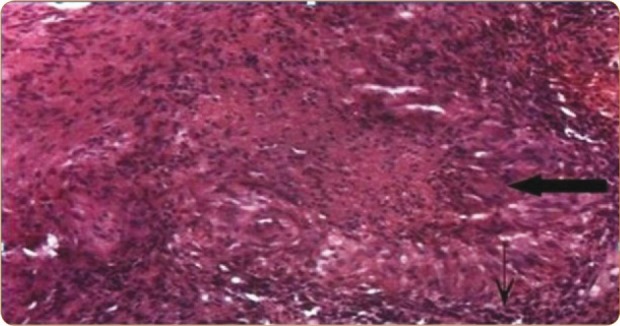
CT guided biopsy of right lower lobe nodule of same patient (Figure 3) showing epitheloid granuloma with langhan’s giant cell (thick arrow) and wall of epitheloid cells (small arrow) around a central area of necrosis
Therefore, cytohistopathological evidence is of utmost importance to reach definite diagnosis of lung cancer.
Sputum examination
Sputum smear staining is most widely applied diagnostic technique for active tuberculosis. It is key test in both establishing diagnosis and infectiousness of disease. The test is based on the high lipid content of the cell wall of the mycobacteria, which makes them resistant to decolorization by acid-alcohol after the primary staining. Its advantage is being inexpensive, rapid to perform and of being specific. Turnaround time is usually less than 2 hrs.
Sputum culture for AFB is gold standard for lab diagnosis of tuberculosis. It provides definitive diagnosis by establishing the viability and identity of the organism. Its most important benefit is drug susceptibility test, which can be done and also, it can identify the organism up to species level. The disadvantage of sputum culture for acid fast bacilli is being very slow, taking several weeks for growth of Mycobacterium tuberculosis, thereby delaying the treatment.
Diagnosis of lung cancer by examination of induced sputum specimens for malignant cells may be a valuable alternative to diagnosis by bronchoscopy.[16] Sputum cytology have many advantages over other methods used for diagnosis of lung cancer as it is quick, devoid of any trauma, non-invasive and most likely to give positive results in case of centrally-placed cancers. The best benefit is that it provides cytological diagnosis, which is important to decide the treatment for lung cancer.
Bronchoscopy
Bronchoscopy is important test for diagnosis of both pulmonary tuberculosis as well as lung cancer.
Bronchoscopy is indicated in case of tuberculosis in whom sputum is non-productive or smear examination is negative.[17] Various findings in case of tuberculosis on bronchoscopy include granulomatous ulcer (most common), solitary ulcer, hyperplastic lesion (including tuberculoma) and fibrostenotic lesions.[18] Performing Fiber Optic Bronchoscopy (FOB), and subjecting the bronchoscopic secretions (BAL, brushing)/TBLB material to conventional diagnostic methods of AFB smear, mycobacterial culture and histopathology is helpful in the diagnosis of sputum smear negative pulmonary tuberculosis. Application of the molecular methods such as Polymerase Chain Reaction (PCR) may be helpful as an adjunctive method for the confirmation of the diagnosis of tuberculosis in individual patient in the appropriate clinical setting. However, FOB is a costly test, is an invasive procedure, and is not widely available in the developing countries and resource poor settings. In developed countries with no limitations on resources/diagnostic facilities, an early use of FOB seems to be the best course of action in a patient with suspected sputum smear negative pulmonary tuberculosis.[19]
Bronchoscopy is most useful test for lung cancer as the entire tracheobronchial tree can be examined and lesions can be seen under direct vision as well as it can provide histological confirmation. The various abnormalities include growth, abnormal mucosa with areas of inflammation, easy bleeding, granularity, nodularity and areas of bronchial stenosis. Location of tumor with extension to carina or trachea is helpful for staging of lung cancer. It also suggests operability as tumor confined to lobar bronchus may be removed by lobectomy but if within 1 cm of carina, then pneumonectomy is procedure of choice.
Through bronchoscope we can have;
Broncho-alveolar lavage
Here, fluid is squirted into a small part of the lung and then recollected for examination.
Transbronchial biopsy
Here, a small piece of tissue is taken out with the help of biopsy forceps and sent for histopathological examination.
Transbronchial needle aspiration
This is done in the cases of larger lesions where with the help of transbronchial needle, the tissue material is aspirated and sent for an examination.
Bronchial brush biopsy
Bronchial brush smears are taken adjacent to the site of the tumor, and the slides are made from the material taken with the help of brush and sent for examination.
ELISA for tuberculosis is not reliable test for diagnosing pulmonary tuberculosis
Antibody detection by enzyme-linked immunosorbent assay (ELISA) for diagnosis of pulmonary tuberculosis is of limited use since less than 70% of patients produce specific antibodies in high levels.[20] ELISA test has sensitivity varying from 50% to 92% and specificity of 95%.[21] The limitations of test are:
The presence of antibodies to M. tuberculosis is not a definite evidence of active disease. Individuals who were previously exposed to mycobacteria and those residing in high prevalent area will show positive results.
In patients with active disease, there is wide variation in the antibody response.
Effects of antitubercular treatment on antibody levels are conflicting.
Different laboratories use different mycobacterial antigen like glycolipids from BCG, antigen 5 and 6 from M. tuberculosis, 64 kDa protein of BCG, 12 kD protein of M. tuberculosis and antigen 60 (A60). Thus, there is wide variation in the ELISA results from same sample.
Henceforth, ELISA for tuberculosis cannot be recommended for distinguishing pulmonary tuberculosis from lung cancer.
Conclusion
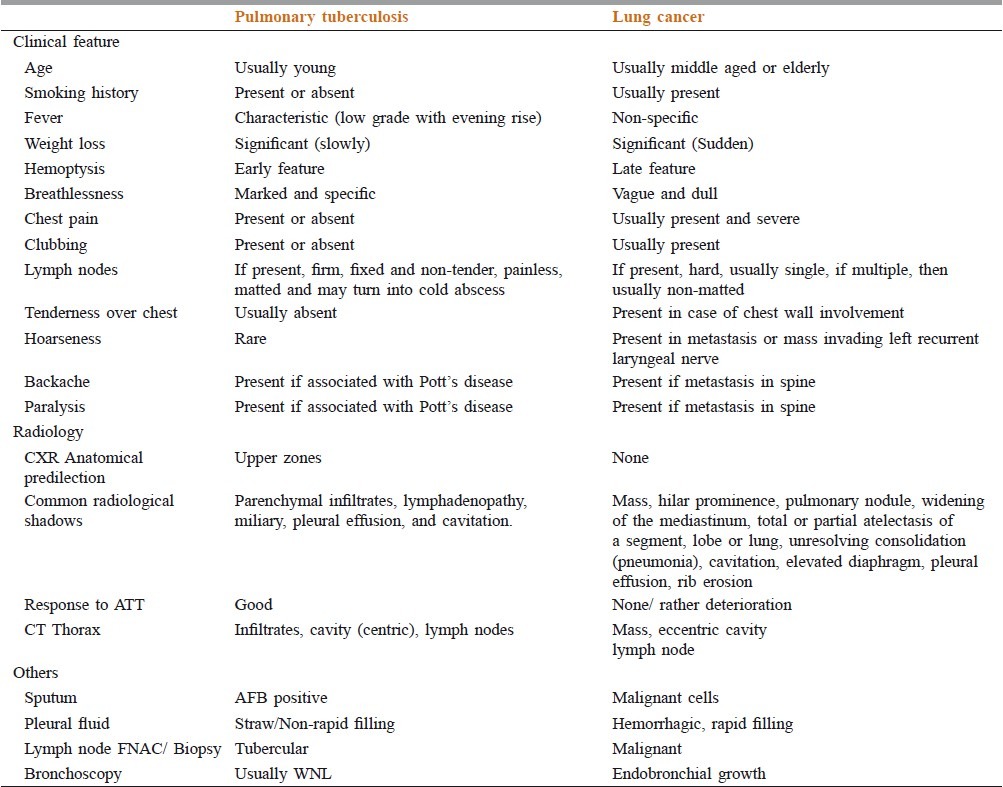
A missed or wrong diagnosis of lung cancer by clinician or general practitioner can lead to delays in treatment, wrong treatments, or no treatments at all. In developing countries like India, the main delay is accounted by patient’s ignorance in reporting to general practitioners, misinterpretation of chest radiograph findings and starting anti-tubercular treatment for suspicious opacities on chest radiograph without proper evaluation using appropriate investigative modalities like CT scan, sputum cytology, and bronchoscopy. The high cost and inaccessibility of diagnostic investigations such as CT scan, and bronchoscopy may contribute to their inadequate utilization early enough. In tertiary centers, waiting period for these investigations is often unacceptably long, further adding to the delay. Many a times, clinicians start ATT without detailed investigations. According to studies, delay in diagnosis of lung cancer was significantly high in patients who had received anti-tubercular treatment for current symptoms compared with those who did not receive anti-tubercular treatment.[22] An additional disturbing fact was that only a small proportion of these patients had a conclusive microbiological diagnosis of tuberculosis. Altogether, these lead to delay in diagnosis and progression of disease. This indicates that lung cancer is often misdiagnosed as pulmonary tuberculosis, and these patients are presumptively given ATT, hence causing significant delay in diagnosing cancer. The majority of lung cancers (< 80%) are diagnosed at an advanced stage, i.e. stage IIIB and IV, by that time, they are beyond the scope of curative resection.[23] Table 1 shows Differences between pulmonary tuberculosis and lung cancer.[24,37]
Table 1.
Differences between pulmonary tuberculosis and lung cancer
To conclude, due to high tuberculosis prevalence in India and radiological similarities, a large number of lung cancer patients initially get wrongly treated for pulmonary tuberculosis and there appears to be an unacceptable delay during the diagnosis and treatment of lung cancer. These may be due to both pre-hospital and hospital-related factors and may contribute, at least partly, to the poor prognosis of this disease even after treatment. Attempts are needed to minimize this lag period by maintaining a high index of suspicion, low threshold for referral and aggressive as well as appropriate investigative workup and prompt initiation of treatment. This is of major concern as early diagnosis of lung cancer can increase the chance of tumor resectability, and timely chemo-radiotherapy may provide better quality of life. If the clinicians including general practitioners are aware of the predisposing factors and the effect of the bronchogenic carcinoma, this may lead to an early diagnosis of lung cancer and better treatment outcome in patients suffering from this dreaded disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.World health organization. Global tuberculosis control. 2011 [Google Scholar]
- 2.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v1.2, Cancer Incidence and Mortality Worldwide: IARC CancerBase No 10 [Internet] Lyon, France: International Agency for Research on Cancer; 2010. [Last Accessed 2011 May]. Available from: http://globocan.iarc.fr . [Google Scholar]
- 3.GLOBOCAN 2002, 2008 database, International Agency for Research on Cancer, World Health Organization. [Last Accessed 2011 May]. Available from: http://globocan.iarc.fr/
- 4.Parkin DM, Muir CS. Cancer incidence in five continents: Comparability and quality of data. IARC Sci Publ. 1992;120:45–173. [PubMed] [Google Scholar]
- 5.Pesut DP, Marinkovic DM. Lung cancer and pulmonary tuberculosis-A comparative population-genetic study British. J Med Genetics. 2009;12:45–52. [Google Scholar]
- 6.Behera D, Balamugesh T. Lung cancer in India. Indian J Chest Dis Allied Sci. 2004;46:269–81. [PubMed] [Google Scholar]
- 7.Notani P, Sanghavi LD. A retrospective study of lung cancer in Bombay. Br J Cancer. 1974;29:477–82. doi: 10.1038/bjc.1974.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohan A, Sharma SK. Fibreoptic bronchoscopy in the diagnosis of sputum smear-negative pulmonary tuberculosis: Current status. Indian J Chest Dis Allied Sci. 2008;50:67–78. [PubMed] [Google Scholar]
- 9.Singh VK, Chandra S, Kumar S, Pangtey G, Mohan A, Guleria R. A common medical error: Lung cancer misdiagnosed as sputum negative tuberculosis. Asian Pac J Cancer Prev. 2009;10:335–8. [PubMed] [Google Scholar]
- 10.Wig KL, Lazaro EJ, Gadekar NG, Guleria JS. Bronchogenic carcinoma: Clinical features and diagnosis. Indian J Chest Dis. 1961;3:209–18. [Google Scholar]
- 11.Gurney JW. Determining the likelihood of malignancy in solitary pulmonary nodules with Bayesian analysis. Radiology. 1993;186:405–13. doi: 10.1148/radiology.186.2.8421743. [DOI] [PubMed] [Google Scholar]
- 12.Higgins GA, Shields TW, Keehn RI. The solitary pulmonary nodule. Arch Surg. 1975;110:570–5. doi: 10.1001/archsurg.1975.01360110116019. [DOI] [PubMed] [Google Scholar]
- 13.Sider L. Radiographic manifestations of primary bronchogenic carcinoma. Radiol Clin North Am. 1990;28:583–97. [PubMed] [Google Scholar]
- 14.Theros EG. Varying manifestations of peripheral pulmonary neoplasms. A radiologic-pathologic correlative study. Am J Roentgenol. 1977;128:893–914. doi: 10.2214/ajr.128.6.893. [DOI] [PubMed] [Google Scholar]
- 15.Siegelman SS, Zerhouni EA, Leo FP, Khouri NF, Stitik FP. CT of the solitary pulmonary nodule. Am J Roentgenol. 1980;135:l–13. doi: 10.2214/ajr.135.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Oswald NC, Hinson KF, Canti G, Miller AB. The diagnosis of primary lung cancer with special reference to sputum cytology. Thorax. 1971;26:623. doi: 10.1136/thx.26.6.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khajotia RR, Mohn A, Vetter N, Pokieser L, Schalleschak J. Induced sputum and cytological diagnosis of lung cancer. Lancet. 1991;338:976–7. doi: 10.1016/0140-6736(91)91839-m. [DOI] [PubMed] [Google Scholar]
- 18.Jalleh RD, Kuppusamy I, Parameswary V, Yeow CS. Fibreoptic bronchoscopy in the diagnosis of pulmonary tuberculosis - A Malaysian experience. Singapore Med J. 1993;34:55–7. [PubMed] [Google Scholar]
- 19.Tapia Acuna R. Bronchoscopy in pulmonary tuberculosis. Dis Chest. 1945;11:392–7. [PubMed] [Google Scholar]
- 20.Fergusson RJ. Crofton and Douglas’s Respiratory Diseases. 5th ed. New Delhi: Wiley India (P) Ltd.; 2008. Lung Cancer; pp. 1077–122. [Google Scholar]
- 21.Bhatia R. Laboratory Diagnosis. In: Sharma SK, editor. Tuberculosis. 2nd ed. New Delhi: JAYPEE Brothers Medical Publishers (P) Ltd; 2009. p. 168. [Google Scholar]
- 22.Singh VK, Chandra S, Kumar S, Pangtey G, Mohan A, Guleria R. A common medical error: Lung cancer misdiagnosed as sputum negative tuberculosis. Asian Pac J Cancer Prev. 2009;10:335–8. [PubMed] [Google Scholar]
- 23.Mountain CF. Revisions in the international system for staging lung cancer. Chest. 1997;111:1710–7. doi: 10.1378/chest.111.6.1710. [DOI] [PubMed] [Google Scholar]
- 24.Burrill J, Williams CJ, Bain G, Conder G, Hine AL, Misra RR. Tuberculosis: A radiologic review. RadioGraphics. 2007;27:1255–73. doi: 10.1148/rg.275065176. [DOI] [PubMed] [Google Scholar]
- 25.Alberts WM. Diagnosis and management of lung cancer: ACCP guidelines. Chest. 2007;132:1S–19. doi: 10.1378/chest.07-1860. [DOI] [PubMed] [Google Scholar]
- 26.Williams WR, Thompson JR. Differential diagnosis of Pulmonary Tuberculosis and Lung Cancer - Are cytologic studies of blood and bone marrow of value? Chest. 1965;47:70–6. doi: 10.1378/chest.47.1.70. [DOI] [PubMed] [Google Scholar]
- 27.Khuri FR, Herbst RS, Fossella FV. Emerging therapies in non-small cell lung cancer. Ann Oncol. 2001;12:739–44. doi: 10.1023/a:1011197500223. [DOI] [PubMed] [Google Scholar]
- 28.Sharma CP, Behera D, Aggarwal AN, Gupta D, Jindal SK. Radiographic patterns in lung cancer. Indian J Chest Dis Allied Sci. 2002;44:25–30. [PubMed] [Google Scholar]
- 29.Wu AH, Fontham ET, Reynolds P, Greenberg RS, Butfler P, Liff J, et al. Previous lung diseases and risk of lung cancer among lifetime non smoking women in the United States. Am J Epidemiol. 1995;141:1023–32. doi: 10.1093/oxfordjournals.aje.a117366. [DOI] [PubMed] [Google Scholar]
- 30.Cicenas S, Vencevicius V. Lung cancer in patients with tuberculosis. World J Surg Oncol. 2007;5:22. doi: 10.1186/1477-7819-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Danek SJ, Bower JS. Diagnosis of pulmonary tuberculosis by flexible fiberoptic bronchoscopy. Am Rev Respir Dis. 1979;119:677–9. doi: 10.1164/arrd.1979.119.4.677. [DOI] [PubMed] [Google Scholar]
- 32.Feng TC. Analysis of 27 patients with lung cancer misdiagnosed as tuberculosis. Zhonghua Zhong Liu Za Zhi. 1989;11:458–60. [PubMed] [Google Scholar]
- 33.Gould MK, Maclean CC, Kuschner WG, Rydzak CE, Owens DK. Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: A meta-analysis. JAMA. 2001;285:914–24. doi: 10.1001/jama.285.7.914. [DOI] [PubMed] [Google Scholar]
- 34.Kant S, Saheer S, Prakash V, Hasan G, Jabeed P, Husain N. Bilateral nodular pulmonary tuberculomas simulating metastatic disease. BMJ Case Rep. 2011;11:35–9. doi: 10.1136/bcr.11.2010.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kant S, Kushwaha RA, Verma SK, Sanjay Bilateral nodular pulmonary tuberculosis simulating metastatic lung cancer. Internet J Pulm Med. 2007;8:1531. [Google Scholar]
- 36.Kant S, Garg R, Tripathi AK. Approach to a solitary pulmonary nodule. J of Internal Medicine of India. 2000;3:131–6. [Google Scholar]
- 37.Behera D. Tuberculosis. In: Behera D, editor. Textbook of Pulmonary Medicine. 2nd ed. New Delhi: JAYPEE Brothers Medical Publishers (P) Ltd; 2010. pp. 521–2. [Google Scholar]


