Abstract
Brain metastasis is the most common intracranial tumor in adults. The incidence of brain metastasis is rising with the increase in survival of cancer patients. Magnetic resonance imaging with contrast enhancement is the imaging procedure of choice to diagnose and characterize brain metastases. Multiple lesions with marked vasogenic edema and mass effect are typically seen in patients with brain metastases. The classical appearance of a metastasis is a solid enhancing mass with well-defined margins and extensive edema. Occasionally, central necrosis produces a ring enhancing mass. Here, we report a case of Non Small Cell Lung Cancer with multiple ring enhancing lesions in brain, and the approach to diagnosis of such patients.
Keywords: Cystic brain metastases, magnetic resonance imaging, neurocysticercosis
Introduction
Brain metastasis is the most common intracranial tumor in adults. It presents clinically as headache, seizures or loss of cognitive or motor function. The incidence of brain metastasis is rising with the increase in survival of cancer patients. Approximately, 20%-40% patients with cancer will develop brain metastases in the course of their disease.[1] Presenting symptoms include headache (49%), focal weakness (30%), mental disturbances (32%), gait ataxia (21%), seizures (18%), speech difficulty (12%), visual disturbance (6%), sensory disturbance (6%), and limb ataxia (6%).[2] Lung, breast, melanoma, renal, and colon cancers are the most common primary tumors to metastasize to the brain.[3] Magnetic resonance imaging (MRI) with contrast enhancement is the imaging procedure of choice to diagnose and characterize brain metastases.
We report an unusual case of cystic brain lesions in a patient of non-small cell lung cancer, with the approach to the differential diagnosis.
Initial presentation and treatment
A 57-year-old gentleman was diagnosed in May 2011 with metastatic adenocarcinoma lung with pleural effusion and pericardial effusion. He received 6 cycles of pemetrexed and carboplatin based chemotherapy, completed in October 2011, with symptomatic improvement, and radiologically stable disease. Then, the patient was kept on observation. He presented in follow-up in September 2012 with 2-3 weeks complaints of heaviness in the head, not associated with giddiness, vomiting, altered behavior, seizures, cough, breathlessness or chest pain. Central Nervous System examination revealed bilateral extensor plantars and no other abnormality. His Eastern Co-operative Oncology Group (ECOG) performance status was well-preserved at 1. Contrast Enhanced Computerized Tomography (CECT) of the thorax showed no evidence of disease progression.
Imaging findings
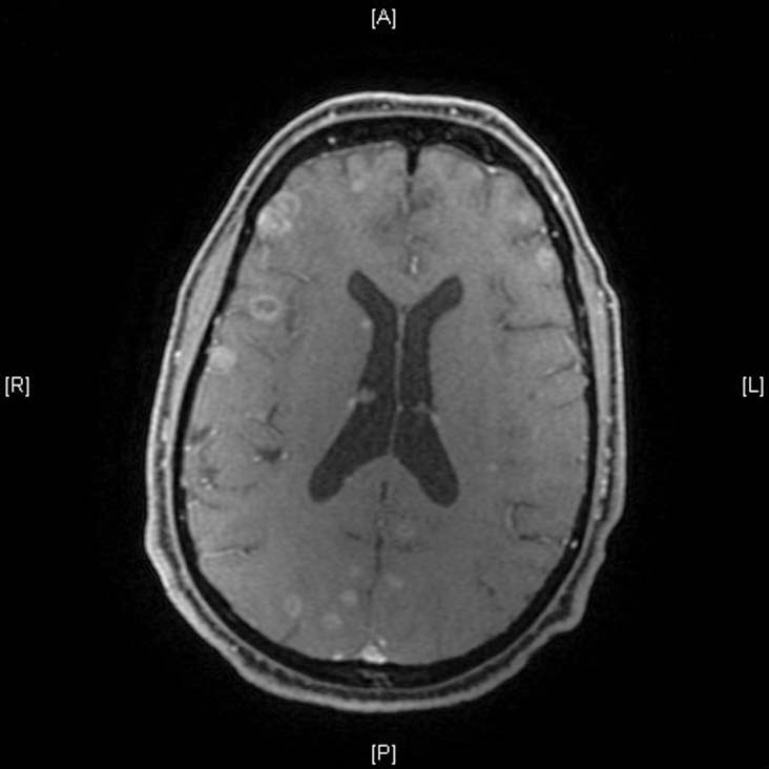
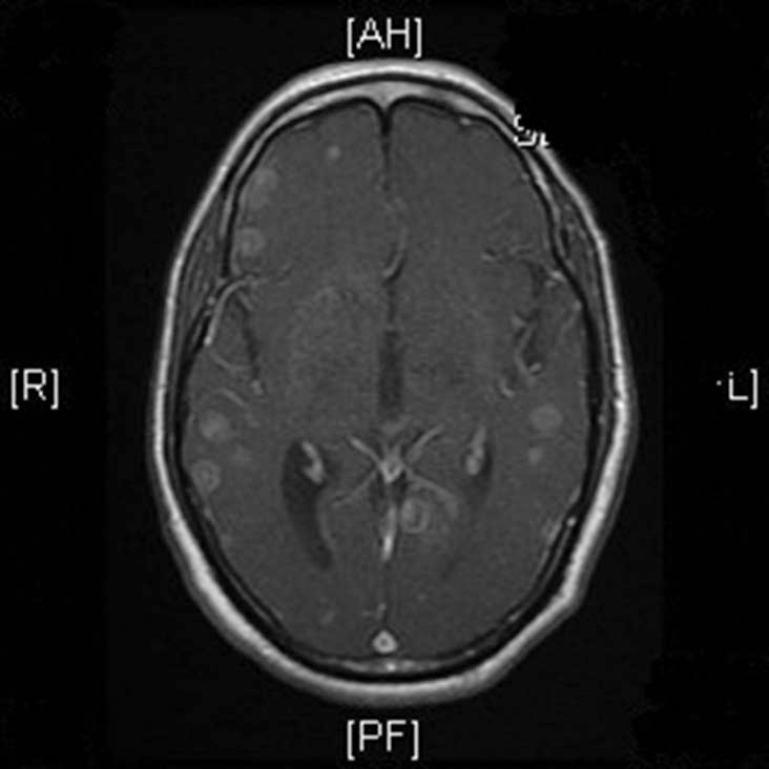
MRI Brain was ordered in view of new onset headache, which showed numerous rounded enhancing lesions of varying sizes in both cerebral and cerebellar hemispheres, involving the grey and white matter [Figures 1-3]. The lesions involved all the lobes in both cerebral hemispheres, with the largest measuring 1.2 cm in diameter. Most of the lesions showed thin enhancing walls together with eccentric punctate enhancing foci within. The lesions appeared hypointense on T1-weighted images, and hyperintense on T2-weighted and Fluid Attenuated Inversion Recovery (FLAIR) images. A few lesions showed areas of low signal intensity on gradient echo and Susceptibility weighted imaging sequences suggestive of calcification or hemorrhage. Mild to moderate perilesional edema was seen around the enhancing lesions. No evidence of restricted diffusion was seen in the brain on diffusion weighted images.
Figure 1.
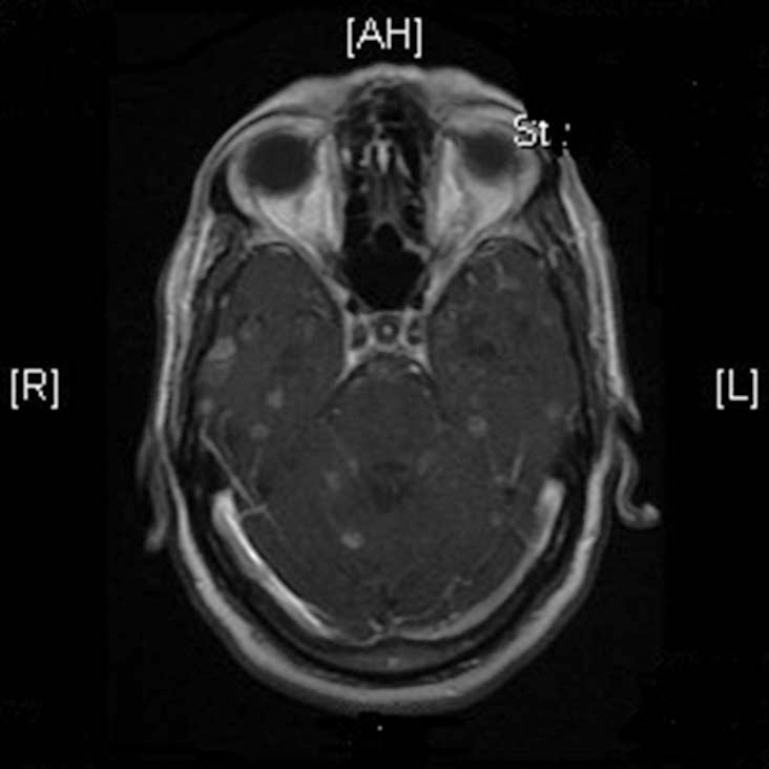
T1w post gad axial contrast enhanced magnetic resonance (CEMR) multiple ring and disc enhancing lesions noted in the bilateral cerebral and cerebellar hemispheres with surrounding perilesional edema
Figure 3.
T1w post gad axial – contrast enhanced magnetic resonance (CEMR) – multiple ring and disc like enhancing lesion noted in the bilateral cerebral hemisphere with surrounding perilesional edema
Figure 2.
T1w post gad axial – contrast enhanced magnetic resonance (CEMR) – multiple ring and disc like enhancing lesions noted in the bilateral cerebral hemisphere with surrounding perilesional edema
Differential diagnosis with approach to diagnosis
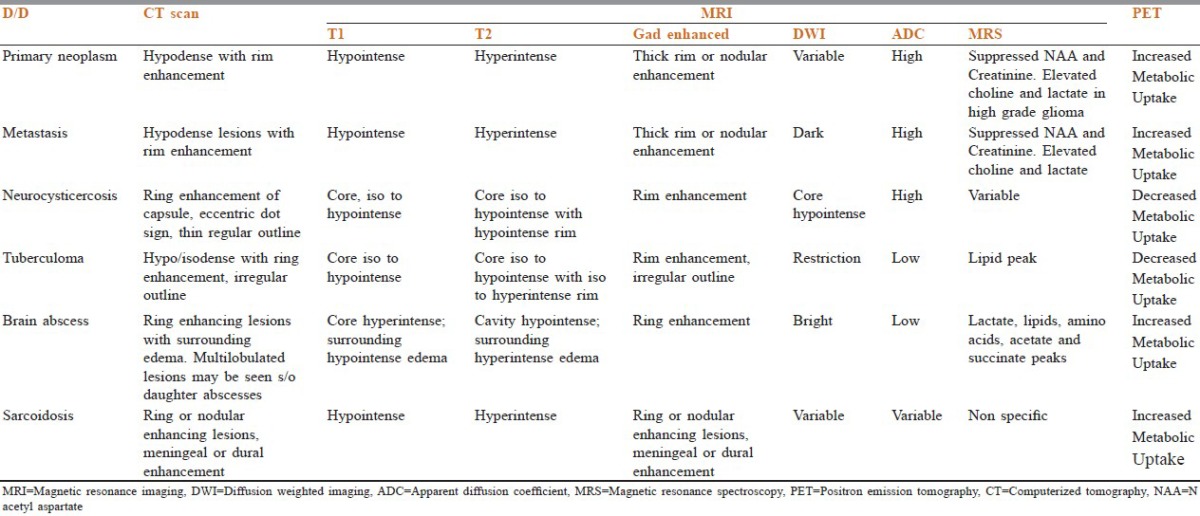
Cystic lesions are common findings on MRI and CT brain. The common differential diagnoses to be considered in case of cystic lesions in the brain in an immunocompetent individual include brain metastases, brain abscess, tuberculoma, neurocysticercosis, primary tumor of brain, and sarcoidosis. Differentiating these cysts on the basis of imaging findings alone is difficult [Table 1].
Table 1.
Differential diagnoses of ring enhancing lesions of the brain
Causes of multiple ring enhancing lesions of the brain
Bacterial
Pyogenic abscess
Tuberculous abscess
Mycobacterium aviumintracellulare
Listeriosis
Fungal
Nocardiois
Actinomycosis
Rhodococcosis
Zygormycosis
Coccidiomycosis
Paracoccidiomycosis
Mucormycosis
Aspergillosis
Cryptococcosis
Histoplasmosis
Parasitic
Neurocysticercosis
Amoebic abscess
Toxoplasmosis
Chagas disease
Inflammatory and demyelinating disorders
Multiple sclerosis
Acute disseminated encephalomyelitis
Sarcoidosis
Vasculitis and Behcet disease
Neoplastic
Metastases
Primary brain tumor
World Health Organization considers neurocysticercosis to be the most common parasitic disease of the brain.[4] Neurocysticercosis cysts are found in the subarachnoid spaces, typically the basal cisterns and deep within the sulci.[5] Other common locations include the hemispheric parenchyma at the gray matter – white matter interface and in the ventricles (fourth ventricle is most common).
Imaging findings in neurocysticercosis
Imaging findings in neurocysticercosis vary with the stage of cyst development. Multifocal lesions and lesions in different stages of development are common.
In the early vesicular stage of neurocysticercosis, MRI shows smooth thin-walled cysts[6,7] rarely with edema and contrast enhancement. A mural nodule representing the viable larval scolex is often present. Usually, the lesions are < 2 cm in diameter.[8] Cystic brain lesions with scolex is pathognomonic of neurocysticercosis.
With the beginning of cyst degeneration (colloidal-vesicular stage), pericystic edema and cyst wall enhancement appear,[7] due to host inflammatory response.
In the healing, or granular nodular stage, non-contrast CT scans show an isoattenuated cyst with a hyperattenuated calcified scolex. Surrounding edema and contrast enhancement persist. The residual cyst is isointense to brain on T1-weighted images and iso to hypointense on T2-weighted images. Occasionally, a target or bull's eye appearance is seen with the calcified scolex in the center of the mass.
In the quiescent or residual stage, small calcified nodules without mass effect and usually without enhancement are seen.[6,7]
Imaging findings in brain metastases
The classical appearance of a metastasis is a solid enhancing mass with well-defined margins and extensive edema. Occasionally, central necrosis produces a ring enhancing mass. Multiple lesions with marked vasogenic edema and mass effect are typically seen in patients with brain metastases. Lesions are isointense to mildly hypointense on T1-weighted images, hyperintense on T2-weighted images or with FLAIR. Surrounding edema is relatively hypointense on FLAIR and T1-weighted images and hyperintense on T2-weighted images. Following administration of a contrast agent, solid, nodular, or irregular ring patterns of enhancement are seen. It has been shown that treatment with dexamethasone leads to a reduction in evidence on MRI of peritumoral edema and occasionally, a lessening in the extent of contrast enhancement. Definitive diagnosis can be established on biopsy.
Final diagnosis
In our case, the multiple lesion-like “cyst with a dot” appearance of varying sizes, max1.2 cm and varying stages of development on MRI suggested the diagnosis of neurocysticercosis.
Treatment and further clinical course
The patient was initially thought to have cystic brain metastases and was given steroids and whole brain radiotherapy (WBRT) 20 Gy in 5 fractions. Post radiotherapy, non-contrast CT head showed no significant abnormality in the brain except for mild dilatation of the ventricular system [Figure 4]. Multiple enhancing nodules and perilesional edema seen in both cerebral and cerebellar hemispheres on the previous MRI appeared to have completely regressed and were not visualized in the post WBRT non-contrast CT Head. However, following WBRT, the condition of the patient deteriorated. In follow-up visits, he was found to have ECOG Performance Status-3. He complained of headache, giddiness, irritability, and weakness in both lower limbs. CNS examination showed power 3/5 in bilateral lower limbs and extensor plantars bilaterally. MRI spine showed disc desiccation at L5-S1 level. The possibility of brain edema was entertained and the patient was restarted on steroids, to which he showed marginal response. He was started on Tab Albendazole 15 mg/kg/d in two divided doses for 28 days presumptively for neurocysticercosis. During the last follow-up, he was still on Albendazole and his clinical condition had marginally improved.
Figure 4.
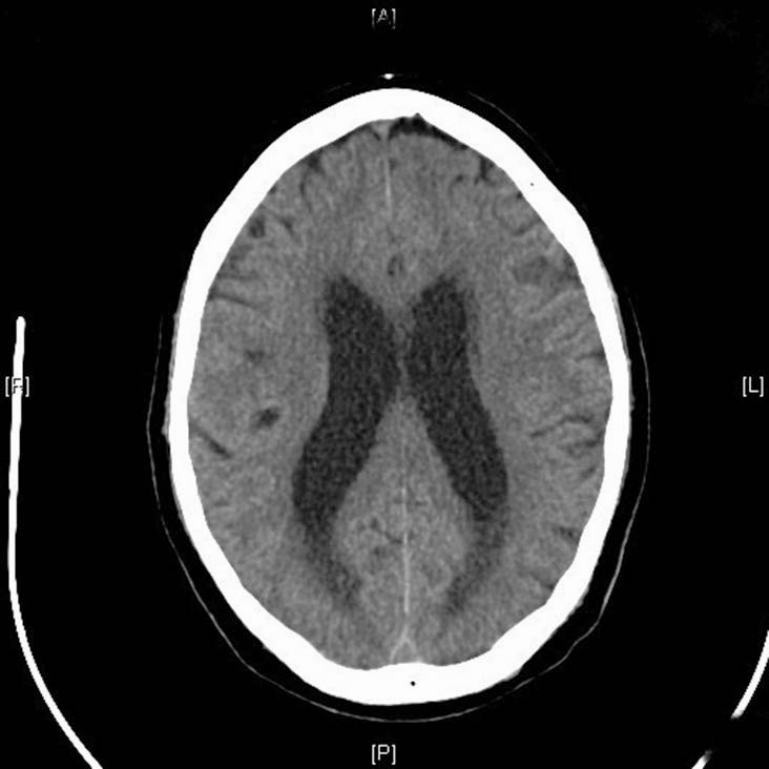
Post Whole Brain Radiotherapy (WBRT) Non Contrast Computerized Tomography (NCCT) head dated 18/10/12 showing mild dilatation of the ventricular system. Multiple enhancing nodules and perilesional edema seen in both cerebral and cerebellar hemispheres on the previous magnetic resonance imaging scan appears to have completely regressed
Figures 1-3: MRI brain dated 10/9/12 showing numerous rounded cystic lesions of varying sizes are seen in both cerebral and cerebellar hemispheres, showing thin enhancing walls together with eccentric punctate enhancing foci within the lesions. Mild to moderate perilesional edema is seen around the enhancing lesions. The lesions appear hypointense on T1-weighted images, and hyperintense on T2-weighted and FLAIR images.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Norden AD, Wen PY, Kesari S. Brain metastases. Curr Opin Neurol. 2005;18:654–661. doi: 10.1097/01.wco.0000191514.37498.2b. [DOI] [PubMed] [Google Scholar]
- 2.Posner JB. Neurologic Complications of Cancer. Vol. 37. Philadelphia: Davis FA; 1995. Paraneoplastic Syndromes; p. 311. [Google Scholar]
- 3.Burger PC, Scheithauer BW. Washington: American Registry of Pathology; 2007. Tumors of the Central Nervous System. Atlas of Tumor Pathology. [Google Scholar]
- 4.Colli BO, Carlotti CG, Jr, Assirati JA, Jr, Machado HR, Valença M, Amato MC. Surgical treatment of cerebral cysticercosis: Long-term results and prognostic factors. Neurosurg Focus. 2002;12:e3. [PubMed] [Google Scholar]
- 5.Osborn AG, Preece MT. Intracranial cysts: Radiologic-pathologic correlation and imaging approach. Radiology. 2006;239:650–64. doi: 10.1148/radiol.2393050823. [DOI] [PubMed] [Google Scholar]
- 6.Salzman KL. Diagnostic Imaging: Brain. Salt Lake City, Utah: Amirsys; 2004. Parasites, miscellaneous; pp. 8–53. [Google Scholar]
- 7.Osborn AG. Diagnostic Neuroradiology. St Louis, Mo: Mosby; 1994. Infections of the brain and its linings; pp. 709–13. [Google Scholar]
- 8.Garg RK, Sinha MK. Multiple ring-enhancing lesions of the brain. J Postgrad Med. 2010;56:307–16. doi: 10.4103/0022-3859.70939. [DOI] [PubMed] [Google Scholar]


