Abstract
Osteosarcoma is the most common primary bone tumor in children and young adults arising from primitive mesenchymal bone-forming cells. The lung is the most common site of metastasis of osteosarcoma. Here, we report a case of a 14-year-old male patient having osteosarcoma of tibia presenting to us for evaluation of left-sided pleural effusion after 4 years of mid-thigh amputation. Contrast-enhanced computed tomography thorax revealed a large, heterogeneous, calcified mass (+277 H.U) at left upper and middle lobe along with massive left-sided pleural effusion. Thoracoscopy revealed a lung metastasis in the right upper and middle lobe along with 2-cm diameter mass found on the surface of parietal pleura. Lung tumor was resected and biopsy of the pleural mass was carried out. Histopathological examination from both the masses was suggestive of metastatic osteosarcoma. The case underlines the importance of performing thoracoscopy in patients of osteosarcoma who recur with lung metastasis.
Keywords: Metastasis, osteosarcoma, pleura, thoracoscopy
Introduction
Osteosarcoma is the most common primary bone tumor encountered in children and young adults.[1] It arises from primitive mesenchymal bone-forming cells and its histological hallmark is the presence of a malignant osteoid. Although osteosarcomas have dramatic response to treatment, approximately 25-30% of the patients eventually develop metastases.[2] Lung is the most common site of metastasis of osteosarcoma. Metastatic osteosarcoma presenting with pleural metastasis is very rare. Here, we report a case of a 14-year-old male patient presenting to us for evaluation of left-sided pleural effusion, after 4 years of mid-thigh amputation for osteosarcoma of the right tibia.
Case Report
A 14-year-old male patient with osteosarcoma of tibia received preoperative chemotherapy with cisplatin and doxorubicin. He had undergone mid-thigh amputation in November 2007. Histopathological examination from the lesion at the upper end of tibia was suggestive of osteogenic sarcoma. The patient then received 6 cycles of cisplatin and doxorubicin until June 2008. A computed tomography (CT) thorax done at that time revealed no abnormality. The patient presented to us in April 2012 with cough and pleuritic chest pain for the last 7 days. Clinical examination findings were suggestive of left-sided massive pleural effusion. Hematological examination showed normocytic, normochromic anemia (Hb 9.5 g/dl) with normal erythrocyte sedimentation rate. Pleural fluid was lymphocytic, exudative in nature with adenosine deaminase level 13.3 (normal <30 U/L). Pleural fluid cytology for malignant cells was negative on three successive occasions. Contrast-enhanced CT thorax revealed a large, heterogeneous, calcified mass (+277 H.U) at left upper and middle lobe extending to the hilum, partially encasing the left main pulmonary artery along with left-sided massive pleural effusion resulting in complete collapse consolidation of the left lung [Figure 1]. CT-guided fine needle aspiration cytology from the lung mass was inconclusive. Flexible bronchoscopy done after pleural aspiration revealed no other abnormality. Thoracoscopy revealed a lung metastasis in right upper and middle lobe exposed on the surface of visceral pleura. A tumor about 2 cm in diameter was found on the surface of parietal pleura. Lung tumor was resected and biopsy of the pleural mass was carried out. Both the sections showed tumor composed of polygonal and spindle-shaped cells with hyperchromatic nuclei. The tumor cells showed nuclear pleomorphism. Tumor giant cells with large hyperchromatic nuclei were present. The tumor cells showed osteoid formation. Extensive areas of the tumor exhibited chondroid differentiation along with mitotic figures. The features were compatible with metastatic osteogenic sarcoma [Figure 2]. The patient was administered three more cycles of chemotherapy consisting of cisplatin and doxorubicin and did not develop any cumulative toxicity post-chemotherapy, in spite of the same chemotherapy regimen pre-relapse and post-relapse.
Figure 1.
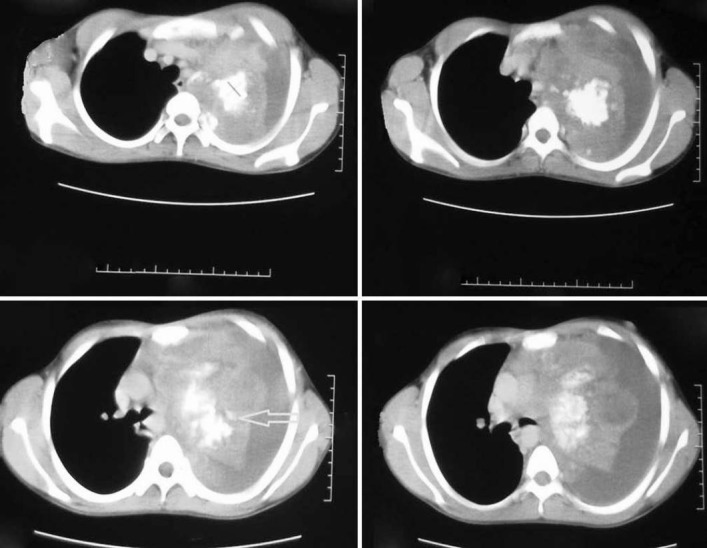
Contrast enhanced computed tomography scan of thorax showing a large, heterogeneous, calcified mass (arrow) with +277 H.U at left upper and middle lobe extending to the hilum, partially encasing the left main pulmonary artery along with left-sided massive pleural effusion
Figure 2.
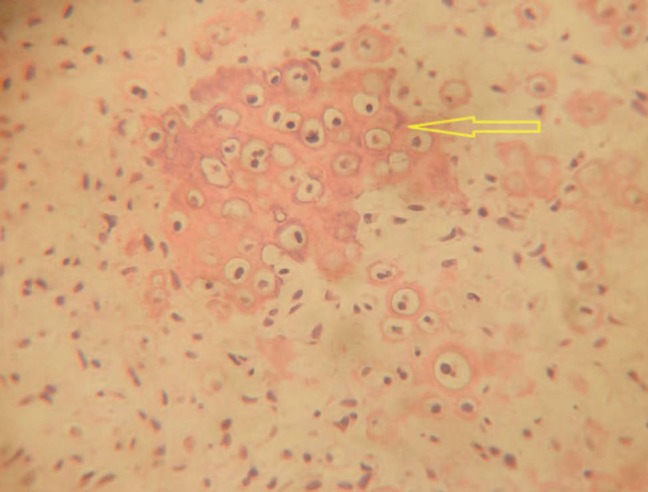
Pleural biopsy specimen showing polygonal and spindleshaped cells with hyperchromatic nuclei and osteoid formation (yellow arrow) along with mitotic figures, suggestive of metastatic osteogenic sarcoma
Discussion
Osteosarcoma is a deadly form of primary bone tumor thought to arise from primitive mesenchymal bone-forming cells. A number of variants of osteosarcoma occur, including conventional types (osteoblastic, chondroblastic, and fibroblastic), telangiectatic, multifocal, parosteal, and periosteal. At presentation, 80% of the patients with osteosarcoma have localized disease at presentation and 10% have distant metastasis.[3] The most common sites of metastases are lung and bone, respectively.[4] Osteosarcomas show a dramatic response to treatment. Approximately 25-30% of the tumors recur after treatment.[2] The lung is the most common site of initial recurrence after treatment. According to the Japan Autopsy Annual Database, 643 patients died of osteosarcoma between 1981 and 2002 in Japan. Of 643 patients, only 78 (12.1%) patients had pleural metastasis.[5] There are no conclusive data regarding the presence of pleural effusion in patients with osteosarcoma. Pleural metastasis in patients with osteosarcoma is rarely reported. Pleural metastasis in patients with osteosarcoma may occur due to two reasons: (1) Due to direct contact of pleura with the lungs and (2) hematogenous spread of osteosarcoma. Although lung is the most common site of hematogenous metastasis of osteosarcoma, pleural metastasis occurs rarely contrary to carcinoma of lung. It is difficult to give a definite opinion about the origin of pleural metastasis in our patient. The points in favor of the local spread of the tumor due to direct contact with pleural surface include (1) although both lung and pleural tumors were separated from each other, thepleural tumor came into contact with lung surface during ventilation as it was within the reach of lung tumor. (2) Absence of mesothelial covering in both lung and pleural surfaces.
The most common mode of metastasis of osteosarcoma patients is micrometastasis in the lungs, which is treatable with adjuvant chemotherapy. Overall management and prognosis is determined by the number, site, and size of the metastasis.[6] The volume of the tumor has been used to predict patient survival and the occurrence of lung metastasis on plain radiographs.[7] Recurrent osteosarcoma in general terms is considered to have a poor prognosis. A short time-interval between initial presentation and relapse, recurrences involving more than one site, and in the case of lung metastases, bilateral disease, and pleural involvement are negative prognostic factors. In recurrent osteosarcoma presenting with lung metastasis or pleural effusion; the pleural cavity must be thoroughly examined with a thoracoscope. After direct visualization of the pleural cavity if any metastatic parietal pleural lesion is found in contact with the lung lesion or isolated, it should be resected completely along with the lung tumor and free pleural margin. Complete surgery is a prerequisite for cure and improves the survival of the patient. Second-line chemotherapy, especially chemotherapy using more than one agent, seems to add little to improve the outcome. Patients with unresectable disease may benefit from radiotherapy.[8] The 5-year survival rate in patients with pulmonary metastasis of osteosarcoma was reported to be 41%.[9]
In our patient, metastasis to the parietal pleura resulted from kissing of the lung metastatic lesion to the parietal pleura. In the literature, only one case of kissing pleural metastasis had been reported; which was a 16-year-old boy who developed diaphragmatic pleural metastasis adjacent to the lung metastasis due to relapse of osteosarcoma after 1 year of resection of the right femoral osteosarcoma. After resection of his pleural metastasis by thoracoscopy, he was well and did not develop any recurrence during 81 months of follow-up.[10]
In conclusion, we want to report the case as pleural metastasis in osteosarcoma is rare. As localized pleural tumor can be removed surgically with better prognosis, pleural cavity should be looked into carefully in every patient of osteosarcoma. Thoracoscopy should be used in patients of osteosarcoma who recur with lung metastasis and in evaluation of undiagnosed pleural effusion.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Vander Griend RA. Osteosarcoma and its variants. Orthop Clin North Am. 1996;27:575–81. [PubMed] [Google Scholar]
- 2.Tabone MD, Kalifa C, Rodary C, Raquin M, Valteau-Couanet D, Lemerle J. Osteosarcoma recurrences in pediatric patients previously treated with intensive chemotherapy. J Clin Oncol. 1994;12:2614–20. doi: 10.1200/JCO.1994.12.12.2614. [DOI] [PubMed] [Google Scholar]
- 3.Marina NM, Pratt CB, Rao BN, Shema SJ, Meyer WH. Improved prognosis of children with osteosarcoma metastatic to the lung (s) at the time of diagnosis. Cancer. 1992;70:2722–7. doi: 10.1002/1097-0142(19921201)70:11<2722::aid-cncr2820701125>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 4.Jeffree GM, Price CH, Sissons HA. The metastatic patterns of osteosarcoma. Br J Cancer. 1975;32:87–107. doi: 10.1038/bjc.1975.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Japan Autopsy Annual Database. Tokyo: Japanese Society of Pathology; 1981-2002. Japanese Society of Pathology. In Japanese. [Google Scholar]
- 6.Pochanugool L, Subhadharaphandou T, Dhanachai M, Hathirat P, Sangthawan D, Pirabul R, et al. Prognostic factors among 130 patients with osteosarcoma. Clin Orthop Relat Res. 1997;345:206–14. [PubMed] [Google Scholar]
- 7.Bieling P, Rehan N, Winkler P, Helmke K, Maas R, Fuchs N, et al. Tumor size and prognosis in aggressively treated osteosarcoma. J Clin Oncol. 1996;14:848–58. doi: 10.1200/JCO.1996.14.3.848. [DOI] [PubMed] [Google Scholar]
- 8.Kempf-Bielack B, Bielack SS, Jürgens H, Branscheid D, Berdel WE, Exner GU, et al. Osteosarcoma relapse after combined modality therapy: An analysis of unselected patients in the Cooperative Osteosarcoma Study Group (COSS) J Clin Oncol. 2005;23:559–68. doi: 10.1200/JCO.2005.04.063. [DOI] [PubMed] [Google Scholar]
- 9.Skinner KA, Eilber FR, Holmes EC, Eckardt J, Rosen G. Surgical treatment and chemotherapy for pulmonary metastases from osteosarcoma. Arch Surg. 1992;127:1065–70. doi: 10.1001/archsurg.1992.01420090073010. [DOI] [PubMed] [Google Scholar]
- 10.Mori T, Yoshioka M, Iwatani K, Kobayashi H, Yoshimoto K, Nomori H. Kissing pleural metastases from metastatic osteosarcoma of the lung. Ann Thorac Cardiovasc Surg. 2006;12:129–32. [PubMed] [Google Scholar]


