Abstract
Objective
In 2002 AMSA created a fourth year medical student elective known as HEART that provided the opportunity for students to explore humanism in medicine, self-care, complementary and alternative medicine modalities, communication, activism, and community building in a four week immersion experience. The educational effects of this elective, and whether it has met its stated goals, are unknown.
Method
The authors conducted a web-based, cross-sectional survey of the first eight cohorts of HEART graduates in 2010. Survey questions assessed respondents’ demographics and perspectives on the educational impact of the elective. Descriptive statistics were used to characterize the sample and qualitative analyses were guided by grounded theory.
Results
Of 168 eligible alumni, 122 (73%), completed the survey. The majority were female (70%), age ≤35 (77%), and trained in primary care specialties (66%). Half were attendings in practice. The majority of respondents felt the elective taught professionalism (89%) and communication skills (92%) well or very well. The majority highly agreed that the elective helped them better cope with stress during residency training (80%), taught them self-care skills (75%), and improved their ability to empathize and connect with patients (71%). Qualitative analysis of the personal and professional impact of the elective identified twelve common themes with self-discovery, self-care, and collegial development/community most frequently cited.
Conclusions
The majority of HEART graduates endorse learning important skills and benefiting from the experience both personally and professionally. Aspects of the HEART curriculum may help training programs teach professionalism and improve trainee well-being.
Introduction
Professionalism, humanism, effective communication, and the ability to collaborate with other allied health professionals as a team are valuable and important physician competencies. Organizations such as the Accreditation Council on Graduate Medical Education (ACGME), American Board of Internal Medicine (ABIM), American Association of Medical Colleges (AAMC), and the Institute of Medicine (IOM) have set guidelines around the inclusion of these topics in training curricula and their measurement(1–4). Nonetheless, formal training in these topics is often underemphasized in medical education in deference to acquiring medical knowledge and procedural skills. Moreover, the hidden curriculum(5), loss of empathy during medical training(6), and the high prevalence of burnout among medical students and residents(7, 8) adversely affect the development of these competencies. In short, many students complete medical school with a wealth of knowledge, but feel ill-prepared to engage in the human aspects of healing and have had little opportunity to reflect on their personal development during their training.
To address these concerns, a committee of medical students and faculty created a unique, fourth year medical student elective in 2002. The elective, known today as HEART (Humanistic Elective in alternative medicine, Activism, and Reflective Transformation), is sponsored by the American Medical Student Association (AMSA) and accredited by the University of Florida College of Medicine. HEART is organized and directed by a committee of five student leaders with oversight from core faculty. Information about the elective is largely spread by word of mouth and the AMSA listserve. Applications for the program are reviewed on a rolling basis, and most students who apply are accepted. Applicants generally consist of a self-selected group of highly motivated students who value community and the topics covered in the elective. Participants are responsible for transportation to the elective as well as a $1000 tuition fee.
Each year, approximately 20 medical students from across the country participate in HEART, spending 4 weeks in a cooperative living and learning environment at a retreat center in northern California. They explore a core curriculum consisting of humanism and relationship-centered medicine, spirituality in medicine, complementary and alternative medicine (CAM), activism and social justice, community building, communication skills, and self-care. Students spend their time in a combination of didactic and experiential sessions led by physician leaders in their respective fields, community chores that include cleaning and cooking healthy meals for each other, and activities promoting reflection and self-care. Further description of the elective and its goals can be found online(9).
While anecdotal reports from program graduates suggested that HEART was a profoundly meaningful experience for some participants, the lack of an evaluation component to this program inhibited any formal assessment of its outcomes. Thus, to begin to understand the effect of this unique medical education innovation on physicians’ personal and professional development, we surveyed past program participants about their experience with the elective. We sought to understand whether this elective achieved its stated goals, especially those focused on cultivating humanism and developing communication and self-care skills.
Method
We performed a retrospective cross-sectional survey of HEART program participants from the 2002–2009 cohorts during the spring of 2010. HEART participants were initially invited to participate in the study by email invitation. Email addresses were obtained from the HEART Advisory Committee Chair who maintains a database of past participants. Of 183 total program graduates at the time of the survey, we did not have contact information for 13 graduates. Additionally, two graduates (MLD and WN) were study authors who elected not to participate in the survey to avoid introducing bias. This left 168 eligible respondents. The survey was posted on the web using Survey Monkey(10). Upon completion of the survey, respondents were offered the opportunity to enter a raffle to win one of two $50 Amazon.com gift certificates as a token of appreciation for their participation through a separate survey link, in order to maintain participant anonymity. The study was approved by the Beth Israel Deaconess Medical Center Committee on Clinical Investigation.
Survey questions assessed participant demographics, training experiences, and participants’ experiences with the HEART program both quantitatively and qualitatively. The latter questions were developed de novo through an iterative process among the study authors using the program description and goals as a guide(9). We asked graduates to explain their numerical responses to the questions about the influence of HEART on their personal and professional development (items 8 and 9 in Table 2) and provided a text box in which they could type their responses. We also asked them to comment on the most important skill that they learned from HEART. Further details regarding specific questions are found in the respective figures and tables. The survey also assessed participant experiences with CAM, frequency and type of self-care practices, and included validated surveys assessing burnout(11), empathy(12), mindfulness(13), resilience(14), attitudes toward CAM(15), and self-rated quality of life(16). Analysis of these data will be reported separately. The entire survey was pre-tested with three internal medicine residents who had not participated in HEART.
Table 2.
Graduates’ Perspectives of What They Learned (n=122)
| “The HEART experience…” | % Highly Agree* |
|---|---|
| 1. Helped me to better cope with the stresses associated with residency training. | 80 |
| 2. Taught me skills that I used to help take better care of myself during residency training | 75 |
| 3. Improved my ability to empathize and connect with my patients. | 71 |
| 4. Increased my knowledge of complementary and alternative medicine. | 85 |
| 5. Increased my self-confidence in taking on leadership roles. | 57 |
| 6. Increased my ability to work collaboratively with colleagues as a team. | 66 |
| 7. Has made me more satisfied with my decision to be in medicine. | 73 |
| 8. Positively affected my personal development. | 89 |
| 9. Positively affected my professional development. | 77 |
Descriptive statistics were used to characterize the sample and were calculated using SAS version 9.2 (SAS Institute, Cary, North Carolina). We used grounded theory(17) and the program’s goals(9) to guide our qualitative analysis. Briefly, three study authors reviewed respondents’ comments, independently identified common themes and, using an iterative process, collectively created a codebook defining each theme. Two authors (WK and WN) subsequently reviewed and coded all of the responses based upon the codebook. A third author (MLD) compiled the codes from both reviewers and served as a tie-breaker or returned the comments back to the primary reviewers when additional consensus-building was necessary.
Results
Of 168 eligible survey respondents, 122 completed the survey for a response rate of 73%. Study participation was similar across all cohorts regardless of whether graduates were still residents in training or were attendings in practice at the time of the survey. Survey respondents were predominantly female, white, age 35 or younger, and practicing in primary care specialties (Table 1). Respondents had attended medical school in diverse locations across the U.S. These trends are similar to what we expected based upon our prior knowledge of the entire population of HEART graduates.
Table 1.
Respondent Demographics (n = 122)
| Characteristic | No. (%) |
|---|---|
| Female | 86 (70) |
| Race | |
| White | 99 (81) |
| Asian or Pacific Islander | 15 (12) |
| Other | 8 (7) |
| Age | |
| ≤30 | 37 (30) |
| 31–35 | 57 (47) |
| 36–40 | 19 (16) |
| ≥41 | 9 (7) |
| Region where attended Medical School | |
| Midwest | 38 (31) |
| Northeast, mid-Atlantic | 38 (31) |
| South | 17 (14) |
| West | 27 (22) |
| Other | 2 (2) |
| Degree | |
| MD | 101 (83) |
| DO | 19 (16) |
| ND | 2 (2) |
| Region where trained as a resident | |
| Midwest | 18 (15) |
| Northeast, mid-Atlantic | 37 (30) |
| South | 9 (7) |
| West | 56 (46) |
| Not yet started residency or no residency | 2 (2) |
| Type of residency program* | |
| University hospital or multiple sites | 61 (52) |
| Community hospital, university affiliated | 40 (34) |
| Community hospital, not university affiliated | 17 (14) |
| Specialty | |
| Family Medicine† | 60 (49) |
| Internal Medicine‡ | 9 (7) |
| Pediatrics | 12 (10) |
| Psychiatry | 21 (17) |
| Other§ | 20 (16) |
| Level of Training | |
| PGY-1 | 18 (15) |
| PGY-2 | 13 (11) |
| PGY-3 | 17 (14) |
| PGY-4 | 1 (1) |
| Fellow | 7 (6) |
| Attending | 62 (51) |
| Research/Other | 4 (3) |
Missing values (4) from those who have not done a residency or type of residency program was unclear
Includes 2 naturopathic doctors
Includes internal medicine subspecialties and primary care
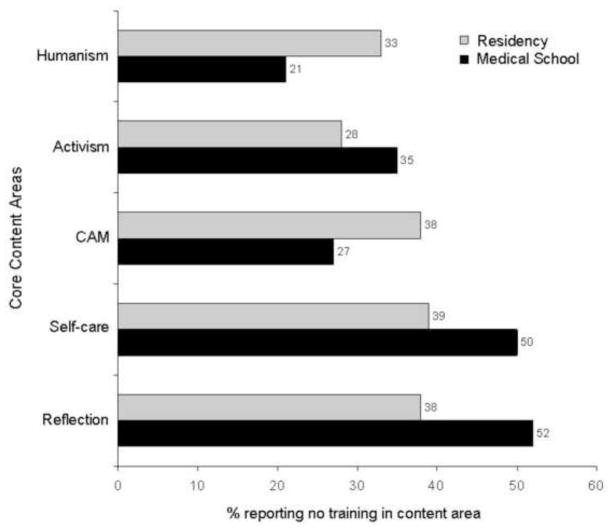
We asked program graduates about their exposure to the core content areas of the HEART curriculum as both medical students and residents (Figure 1). Twenty-one percent of respondents reported no training in humanism during their medical school training and 33% reported no such training during residency. Two aspects of the HEART curriculum most noted to be lacking in medical school and residency curricula were physician self-care (50% and 39%, respectively) and reflection on the medical education experience (52% and 38%, respectively).
Figure 1.
Frequency of graduates reporting lack of exposure to HEART curriculum core content areas in medical school and residency. Graduates were asked “how much exposure to the following subjects did you have as part of your medical school/residency curriculum?” and given three possible responses: none, some, extensive. Shown are the percent of HEART graduates reporting no training in humanism in medicine (e.g., narrative, the arts in medicine, medical humanities), activism and service (e.g., social justice, cultural humility, underserved populations), CAM, self-care (e.g., stress reduction techniques), and reflection (e.g., opportunities to reflect on medical education and life) during medical school (black bars) and residency (gray bars).
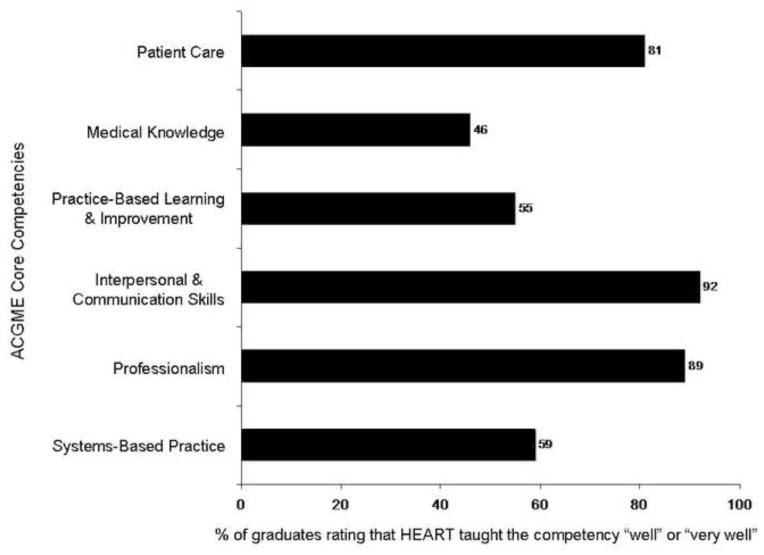
We also asked program graduates to rate how well the HEART curriculum taught each of the ACGME core competencies (Figure 2) using the ACGME definitions(1). The majority of respondents felt that HEART taught patient care (81%), interpersonal and communication skills (92%) and professionalism (89%) well or very well.
Figure 2.
Frequency of graduates reporting that HEART taught the ACGME core competencies well or very well. Graduates were given a list of the ACGME core competencies and definitions(1) and asked, “How well did HEART teach explicitly or implicitly, these ACGME core competencies that residencies are required to teach?” Answer choices were presented as a 5 point likert scale with the following options: not at all, a little, somewhat, well, very well. Shown are the percentage of respondents rating “well” or “very well” in response to the question.
We next asked graduates about the degree to which HEART taught them specific skills or affected their personal or professional development (Table 2). The majority of respondents highly agreed that the HEART experience helped them in each of the nine domains that were asked regarding their perspectives on the elective.
Finally, analysis of the responses to our qualitative questions about the personal and professional impact of the elective and the most important skill they learned yielded 12 distinct and recurring themes that fell into 3 broad categories: relationship to self (self-discovery, resilience, self-care, spirituality), relationship to others (effective communication, leadership, humanism, collegial development), and relationship to the profession of medicine (motivation, re-envisioning of medicine, power and responsibility in medicine, CAM knowledge; Table 3). Comments ranged in length from a short phrase to a long paragraph and included anywhere from one to seven distinct themes. Less than 10% of the comments did not fit into one of the 12 themes. Overall, the most frequently cited themes included self-discovery, self-care, and collegial development/community (Table 3).
Table 3.
How HEART affected graduates’ personal, professional, and skill development
| Theme | Personal Development (%) | Professional Development (%) | Most Important Skill (%) |
|---|---|---|---|
| 1. Self-discovery - personal growth, reflection, listening to or knowing oneself better | 38 | 21 | 17 |
| 2. Resilience - getting through training/difficult times, avoiding burnout | 25 | 18 | 5 |
| 3. Self-care – coping skills used to promote “balance”, “well-being”, or “self-healing” | 38 | 15 | 33 |
| 4. Spirituality - specific mention of spirituality or faith | 3 | 4 | 4 |
| 5. Effective communication - communication/conflict resolution skills, hearing others | 10 | 17 | 16 |
| 6. Leadership - development of one’s own leadership skills | 3 | 6 | 2 |
| 7. Humanism - kindness, compassion or empathy toward patients/others | 5 | 17 | 14 |
| 8. Collegial development - connecting with like-minded individuals, community | 43 | 37 | 17 |
| 9. Motivation - inspiration, validation, feeling good about one’s chosen career | 16 | 13 | 2 |
| 10. Re-envisioning of medicine - broader vision of medical practice, professional values, or comments about becoming a “healer” | 19 | 31 | 4 |
| 11. Power and responsibility in medicine - activism, social responsibility, hierarchy | 4 | 2 | 0 |
| 12. CAM knowledge - as related to patient care, other cultural views of health/illness | 11 | 23 | 12 |
Graduates were asked to explain how HEART had affected their personal development (n = 91 respondents), their professional development (n = 84), and “What one skill did you take away from HEART that has been most important to you?” (n = 122). Shown are the percent of those responding whose comments contained each of the designated themes. Themes fell into 3 main categories: relationship to self (1–4), relationship to others (5–8), and relationship to medicine (9–12).
The ways in which the elective promoted self-discovery and self-care were quite profound for some program graduates.
“I did a lot of exploring things which had held me back, whether they be personal shyness or assumptions about what was or wasn’t okay for a doctor to think or feel. It made me feel a lot more comfortable as a person who also happens to be a doctor. It gave me tools to become a healthier, better-balanced me.”
“HEART gave me the tools to implement my world view, my character, and my heart into my work as a doctor on a daily basis from how I interact with patients, how I view disease, how I view health and healing, and how I take care of my own body, soul, and family. I feel HEART just allowed me to re-learn and re-appreciate many things I already believed and knew before medical school that the dominant medical culture dulled or drilled out of me in some way.”
Many graduates commented on the value of community they discovered at HEART. This sense of community contributed not only to collegial development, but also provided inspiration, encouraged self-discovery, promoted resilience, and fostered humanism.
“Feeling connected w/ like-minded physicians was very comforting for me. Gives me hope.”
“I feel that I got to know myself better during that time because of the community and the experiences allowed in that space.”
“It helped me rally during severely stressful times in my internship, knowing that there was a community out there of physicians with whom I could connect, and on whom I could rely when I felt overwhelmed by my situation in residency.”
“Living in community with other future physicians and becoming close friends with them made me feel as though I was not alone in the struggle to maintain empathy as a provider.”
In addition to the 12 themes that we identified, several graduates commented on how the elective helped them transition from medical student to resident or helped them through residency training.
“HEART provided the forum to reflect on and heal from the process of medical school, as well as strengthen and recenter in preparation for residency.”
“HEART is strategically placed in our training that is immediately before we enter residency….HEART really helped to give me sustaining practices and community to fall back on in my mind and in daily life to get through residency training without burning out or treating my patients poorly.”
“Intern year, to start, has been so much more enriching and livable as a result of my experiences and lessons from HEART.”
Nearly all (96%) of the comments on the most important skill learned from HEART fit into one of the 12 themes (Table 3). These comments commonly reflected personal coping skills (“mindfulness, self-care”, “reflective journaling”), professional tools (“communication skills”, “empathy”), or specific attitudes (“open-mindedness”, “staying grounded in the midst of chaos”, “remembering Loving kindness daily”).
Discussion and Conclusions
This paper is the first to describe the HEART program and what graduates have gained from this experience. The majority of graduates agreed that the program supported the development of professionalism, empathy, and communication and self-care skills. The most frequently cited themes in our qualitative analysis were self-discovery, self-care, and collegial development/community. CAM was frequently mentioned within the context of both self-care and patient care. The overwhelming majority of respondents felt that they benefited both personally and professionally from the experience.
Our results support the notion that this elective achieves its stated goals of helping trainees develop skills in the areas of humanism, self-care, communication, and CAM(9). Promoting activism/social responsibility within medicine and developing leadership skills are also stated goals of the program. The qualitative analysis identified several comments related to these topics, and about half of the respondents felt more confident in taking on leadership roles. We did not quantitatively assess activism or social responsibility in our survey.
Although HEART was not designed specifically to address the ACGME core competencies(1), its structure and curriculum support reflection and skills development around patient care, professionalism, and interpersonal and communication skills. In addition, the HEART curriculum emphasizes physician self-care as an important prerequisite to proficiency in these competencies. Many of the graduates’ comments reflect how their self- and/or situational awareness improved their ability to care for patients. Indeed, previous work has linked physician well-being with professionalism(18) and suggested that CAM education may enhance professionalism and humanism by encouraging an openness to explore patient preferences and cultural views as well as use of self-care habits that may enhance self-awareness and reduce the effects of work-related stress and burnout(19–21).
Many survey respondents endorsed that curriculum around self-care and humanism in medicine was lacking from their medical school and/or residency training. While we are surprised by these numbers and recognize that recall bias may partially explain our results, the overall impression that these topics were lacking in training may suggest that presenting this material using traditional didactic approaches does not guarantee that learners absorb or recall it, let alone integrate it into their developing professional ethos. Dedicated time for dialogue and reflection on these topics may be necessary. Programs such as HEART and others(22–26) that create a safe environment to reflect upon professional values and meaning within a supportive community represent an alternative model to the traditional didactic and evaluation-based approach and have demonstrated effectiveness in accomplishing these goals.
The qualitative responses revealed that many participants took away memories, attitudes, and skills that they continue to value and cultivate years after completing the HEART program. Although the HEART curriculum is unique, some of the themes voiced by program graduates echo those from previously published reports of students’ reflections on professional values and the training environment(5, 22, 27). HEART is uniquely timed in April of the fourth year of medical school, offering trainees the opportunity to reflect on their medical school experiences and reconnect with what is personally and professionally meaningful as they transition from medical students to interns. The opportunity for self-reflection in an intentional and supportive environment during this transition period may augment the impact of HEART and facilitate personal healing, enhance the development of professional aspirations(28), and “immunize” trainees from some of the challenges they will face during residency training(29) by offering both immediate inspiration and validation while also teaching trainees valuable skills to use in their personal and professional lives. Whether a single skill or a particular skill set is critical to the maintenance of such immunity, and protecting trainees from burnout, is unclear.
Nonetheless, the HEART program serves as a unique model for its ability to teach and cultivate key competencies while enhancing the personal and professional growth of trainees. Expanding the program would permit more trainees to participate, but its length and cost may make it infeasible for many. Creating “mini-HEART” programs that combine similar elements within a shorter time frame, with or without a longitudinal component, may be more practical for both students and medical schools.
Limitations of our study include the self-selected nature of the population and potential for recall bias in answering some survey questions. While our survey respondents reported benefiting from participating in HEART, they likely already had interests in the topics covered and may be more open to exploring the humanistic aspects of medicine and integrative modalities congruent with self-care (e.g., meditation, yoga, journaling) and therefore evaluate the elective positively. Whether all fourth year medical students would similarly find the elective as valuable as our respondents is unclear. Notably, survey responses from HEART graduates still in training were not markedly different from graduates who had completed residency training, suggesting that length of time since taking the elective did not introduce marked bias. We did not include a comparison group in our study as our main aim was to understand what program graduates had gained from this experience. Additionally, it is unclear what a proper “control group” for this population would be.
In summary, the majority of HEART graduates endorse learning important skills and benefiting from the experience both personally and professionally. The program’s emphasis on intentional community and reflection may have mediated some of these benefits. Aspects of the HEART curriculum may help training programs teach the competencies of professionalism and communication skills while improving trainee well-being and promoting resiliency.
Acknowledgments
The authors thank Jake Donaldson, MD for his contributions to brainstorming sessions prior to the study’s commencement, Tamara Merritt, MD for access to the database of HEART graduates, Jan Walker, RN, MBA for critical reading of the manuscript, and all of the HEART graduates who participated.
Funding/Support: Dr. Dossett was supported by an institutional National Research Service Award #T32AT000051, a Katherine Swan-Ginsberg Humanism in Medicine Fellowship, and by the Division of General Medicine and Primary Care at Beth Israel Deaconess Medical Center.
Footnotes
Other disclosures: Drs. Dossett and Nunley are graduates of HEART. Dr. Nunley serves on the HEART board of directors. Dr. Kohatsu is a faculty facilitator for HEART.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Swing SR. The ACGME outcome project: Retrospective and prospective. Med Teach. 2007 Sep;29(7):648–54. doi: 10.1080/01421590701392903. [DOI] [PubMed] [Google Scholar]
- 2.Project professionalism [Internet] Philadelphia, PA: American Board of Internal Medicine; 2001. cited 3/29/12]. Available from: http://www.abimfoundation.org/en/ResourceCenter/Bibliography/~/media/Files/Resource%20Center/Project%20professionalism.ashx. [Google Scholar]
- 3.Assessment of professionalism project [Internet]. Association of American Medical Colleges; cited 03/30/12]. Available from: https://www.aamc.org/download/77168/data/professionalism.pdf. [Google Scholar]
- 4.Greiner AC, Knebel E. Health professions education: A bridge to quality. National Academies Press; 2003. [PubMed] [Google Scholar]
- 5.Gaufberg EH, Batalden M, Sands R, Bell SK. The hidden curriculum: What can we learn from third-year medical student narrative reflections? Acad Med. 2010 Nov;85(11):1709–16. doi: 10.1097/ACM.0b013e3181f57899. [DOI] [PubMed] [Google Scholar]
- 6.Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, et al. The devil is in the third year: A longitudinal study of erosion of empathy in medical school. Acad Med. 2009 Sep;84(9):1182–91. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002 Mar 5;136(5):358–67. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 8.Dyrbye LN, Massie FS, Jr, Eacker A, Harper W, Power D, Durning SJ, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010 Sep 15;304(11):1173–80. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 9.HEART program description [Internet] American Medical Student Association; cited 03/30/12]. Available from: http://www.amsa.org/AMSA/Homepage/EducationCareerDevelopment/AMSAAcademy/HEART/HEARTProgramDescription.aspx. [Google Scholar]
- 10.Survey monkey [Internet] Available from: http://www.surveymonkey.com/
- 11.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3. Mountain View, CA: Consulting Psychologists Press, Inc; 1996. [Google Scholar]
- 12.Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, et al. The jefferson scale of physician empathy: Development and preliminary psychometric data. Educational and Psychological Measurement. 2001;61(2):349–65. [Google Scholar]
- 13.Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008 Sep;15(3):329–42. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 14.Wagnild GM. The resilience scale user’s guide for the US english version of the resilience scale and the 14-item resilience scale. 2009 [Google Scholar]
- 15.Lie D, Boker J. Development and validation of the CAM health belief questionnaire (CHBQ) and CAM use and attitudes amongst medical students. BMC Med Educ. 2004 Jan 12;4:2. doi: 10.1186/1472-6920-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shanafelt TD, Novotny P, Johnson ME, Zhao X, Steensma DP, Lacy MQ, et al. The well-being and personal wellness promotion strategies of medical oncologists in the north central cancer treatment group. Oncology. 2005;68(1):23–32. doi: 10.1159/000084519. [DOI] [PubMed] [Google Scholar]
- 17.Glaser B, Strauss A. Discovery of grounded theory: Strategies for qualitative research. Sociology Press; 1967. [Google Scholar]
- 18.West CP, Shanafelt TD. Physician well-being and professionalism. Minn Med. 2007 Aug;90(8):44–6. [PubMed] [Google Scholar]
- 19.Elder WG, Hustedde C, Rakel D, Joyce J. CAM curriculum activities to enhance professionalism training in medical schools. Complement Health Pract Rev. 2008;13(2):127–33. doi: 10.1177/1533210107313917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009 Sep 23;302(12):1284–93. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 21.Beckman HB, Wendland M, Mooney C, Krasner MS, Quill TE, Suchman AL, et al. The impact of a program in mindful communication on primary care physicians. Acad Med. 2012 Jun;87(6):815–9. doi: 10.1097/ACM.0b013e318253d3b2. [DOI] [PubMed] [Google Scholar]
- 22.Rabow MW, Wrubel J, Remen RN. Authentic community as an educational strategy for advancing professionalism: A national evaluation of the healer’s art course. J Gen Intern Med. 2007 Oct;22(10):1422–8. doi: 10.1007/s11606-007-0274-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krupat E, Pelletier S, Alexander EK, Hirsh D, Ogur B, Schwartzstein R. Can changes in the principal clinical year prevent the erosion of students’ patient-centered beliefs? Acad Med. 2009 May;84(5):582–6. doi: 10.1097/ACM.0b013e31819fa92d. [DOI] [PubMed] [Google Scholar]
- 24.Sands SA, Stanley P, Charon R. Pediatric narrative oncology: Interprofessional training to promote empathy, build teams, and prevent burnout. J Support Oncol. 2008 Sep-Oct;6(7):307–12. [PubMed] [Google Scholar]
- 25.DasGupta S, Charon R. Personal illness narratives: Using reflective writing to teach empathy. Acad Med. 2004 Apr;79(4):351–6. doi: 10.1097/00001888-200404000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Rosenthal S, Howard B, Schlussel YR, Herrigel D, Smolarz BG, Gable B, et al. Humanism at heart: Preserving empathy in third-year medical students. Acad Med. 2011 Mar;86(3):350–8. doi: 10.1097/ACM.0b013e318209897f. [DOI] [PubMed] [Google Scholar]
- 27.Karnieli-Miller O, Vu TR, Holtman MC, Clyman SG, Inui TS. Medical students’ professionalism narratives: A window on the informal and hidden curriculum. Acad Med. 2010 Jan;85(1):124–33. doi: 10.1097/ACM.0b013e3181c42896. [DOI] [PubMed] [Google Scholar]
- 28.Rabow MW, Wrubel J, Remen RN. Promise of professionalism: Personal mission statements among a national cohort of medical students. Ann Fam Med. 2009 Jul-Aug;7(4):336–42. doi: 10.1370/afm.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coulehan J, Williams PC. Vanquishing virtue: The impact of medical education. Acad Med. 2001 Jun;76(6):598–605. doi: 10.1097/00001888-200106000-00008. [DOI] [PubMed] [Google Scholar]