Abstract
BACKGROUND:
Cross-sectional studies link functional abdominal pain (FAP) to anxiety and depression in childhood, but no prospective study has evaluated psychiatric status in adulthood or its relation to pain persistence.
METHODS:
Pediatric patients with FAP (n = 332) and control subjects (n = 147) were tracked prospectively and evaluated for psychiatric disorders and functional gastrointestinal disorders (FGIDs) at follow-up in adolescence and young adulthood (mean age = 20.01 years). Participants were classified according to presence (FGID-POS) or absence (FGID-NEG) of FGIDs at follow-up.
RESULTS:
Lifetime and current risk of anxiety disorders was higher in FAP than controls (lifetime: 51% vs 20%; current: 30% vs 12%). Controlling for gender and age, the odds ratio was 4.9 (confidence interval = 2.83–7.43) for lifetime anxiety disorder and 3.57 (confidence interval = 2.00–6.36) for current anxiety disorder at follow-up for FAP versus controls. Lifetime risk of depressive disorder was significantly higher in FAP versus controls (40% vs. 16%); current risk did not differ. In most cases, initial onset of anxiety disorders was before pediatric FAP evaluation; onset of depressive disorders was subsequent to FAP evaluation. Within the FAP group, risk of current anxiety disorders at follow-up was significantly higher for FGID-POS versus FGID-NEG (40% vs 24%), and both were higher than controls (12%); current depressive disorders did not differ across FGID-POS, FGID-NEG, and controls.
CONCLUSIONS:
Patients with FAP carry long-term vulnerability to anxiety that begins in childhood and persists into late adolescence and early adulthood, even if abdominal pain resolves.
Keywords: functional gastrointestinal disorder, psychiatric disorders, anxiety, depression, pediatric, prospective
What’s Known on This Subject:
At the time of their pediatric medical evaluation, patients with functional abdominal pain (FAP) have higher levels of emotional symptoms compared with youth without FAP. No controlled prospective study has evaluated psychiatric outcomes for FAP patients in adulthood.
What This Study Adds:
This prospective study showed that pediatric FAP was associated with high risk of anxiety disorders in adolescence and young adulthood. Risk was highest if abdominal pain persisted, but was significantly higher than in controls even if pain resolved.
Chronic or recurrent abdominal pain affects 8% to 25% of school-age youth,1–3 is associated with frequent school absences,4–6 and accounts for 2% to 4% of pediatric clinic visits.7 Many patients, however, have no evidence of structural or biochemical abnormalities underlying their pain, and hence are considered to have medically unexplained or “functional” abdominal pain (FAP).8 The majority meet Rome III criteria for a functional gastrointestinal disorder (FGID) such as irritable bowel syndrome or functional dyspepsia.9 In addition, pediatric patients with FAP have high rates of anxiety and depression.10,11
Although several studies have evaluated the persistence of abdominal pain in patients with FAP,12 only 1 study evaluated diagnostic criteria for psychiatric disorders in these patients when they reached adulthood. In their seminal study, Campo et al13 identified 28 pediatric patients with medically unexplained recurrent abdominal pain by retrospective chart review and conducted telephone interviews with these patients when they were young adults. They found that, compared with a control group of patients without such history, those with recurrent abdominal pain in childhood were significantly more likely to meet diagnostic criteria for both lifetime and current anxiety disorders in adulthood. A decade later, this study remains the primary source of data on psychiatric outcomes into adulthood for pediatric patients with FAP. The small sample size, however, prohibited reliable evaluation of specific psychiatric diagnoses. Moreover, the study did not evaluate whether risk of psychiatric disorders in adulthood differed as a function of the persistence of abdominal pain. Thus, it is not known whether individuals with pediatric-onset FAP that resolves have rates of psychiatric disorders in adulthood comparable to those of individuals with no history of FAP; increased risk for psychiatric disorders might only characterize pediatric patients with FAP whose abdominal pain continues into adulthood.
This study prospectively followed pediatric patients with FAP and a control group of youth without FAP into adolescence and young adulthood. We hypothesized that individuals with a history of pediatric FAP would have significantly higher risk of anxiety and depressive disorders at follow-up compared with those without such history. We also evaluated rates of other psychiatric disorders, such as somatoform disorders, that have been linked to FGIDs.13,14 In addition, we evaluated whether risk of psychiatric disorders at follow-up in individuals with a history of FAP differed as a function of the persistence versus resolution of their abdominal pain, as defined by the Rome III criteria for FGIDs associated with abdominal pain.15 Finally, for those who met criteria for anxiety or depressive disorder, we evaluated the age of initial onset to determine whether the disorder preceded or followed the pediatric FAP evaluation.
Methods
Participants
Participants were drawn from databases of (1) FAP: consecutive new patients, aged 8 to 17 years, evaluated by the Vanderbilt Pediatric Gastroenterology Service for abdominal pain of ≥3 month’s duration and (2) control subjects: children recruited from area schools in the same age range but without abdominal pain who participated in a health survey at school during the same time period (1993–2007).16–18 Participants were eligible for the follow-up study if they had reached ≥12 years of age and at least 4 years had elapsed since the baseline evaluation. Participants in the FAP database were excluded if their baseline medical evaluation had yielded evidence of significant organic disease (eg, inflammatory bowel disease). In addition, participants in either database who reported onset of chronic disease (eg, inflammatory bowel disease, celiac disease, multiple sclerosis) during the follow-up interval were excluded.
The follow-up entailed a comprehensive evaluation of health outcomes, some of which have been presented elsewhere.19–21 The current study focused on mental health outcomes. Of the 577 individuals (391 with FAP; 186 controls) who were eligible for this study, 491 participated (332 with FAP; 159 controls). Within the FAP and control groups, participants did not differ significantly from nonparticipants regarding age, gender, or baseline levels of abdominal pain. For participants under age 18 years, a parent also participated.
Measures Administered at Follow-up
The Anxiety Disorders Interview Schedule—IV: Adult Lifetime and Child and Parent Versions (ADIS)22–24 is a psychiatric diagnostic interview designed to assess current and lifetime Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) anxiety, mood, and other psychiatric disorders. A Clinical Severity Rating (range 0–8) of ≥4 (indicating at least moderate severity/impairment) is required for assigning a diagnosis. The Anxiety Disorders Interview Schedule has excellent interrater reliability, test-retest reliability, and concurrent validity.25,26 The adult version was used for participants aged ≥18. The child version incorporates both parent and child report into a combined score. To evaluate reliability, 2 diagnosticians (J.E.B. and K.H.) independently rated randomly selected audiotapes of 20% of the interviews.25 Diagnostic disagreements were resolved by consensus or in consultation with the senior diagnostician (J.G.). The κ coefficient regarding presence/absence of disorder ranged from good to excellent (k = 0.76 for the presence of any anxiety disorder; k = 1.0 for other disorders).
The Rome III Diagnostic Questionnaire for Functional Gastrointestinal Disorders15 assesses symptoms associated with the diagnostic criteria for abdominal pain–related FGIDs (irritable bowel syndrome, functional dyspepsia, abdominal migraine, functional abdominal pain). Participants’ responses were scored according to the pediatric Rome III criteria (for participants aged <18 years) or the adult Rome III criteria (for participants aged ≥18 years).
Hollingshead Index of Socioeconomic Status27 was based on the occupation and educational level of the participant or, for those aged <18 years, their parents. Scores can range from 8 (unskilled laborer) to 69 (professional). Scores of both spouses were averaged for married adults and for parents of adolescents.
Procedure
The protocol was administered in a face-to-face interview at Vanderbilt University Medical Center or, for those who could not travel to the medical center, by telephone. Interviewers were unaware of participants’ group status. Procedures were approved by the institutional review board.
Data Analysis
Analyses used Statistics 18 statistical package (SPSS, Inc, Chicago, IL). All variables met assumptions of normality. Analyses of variance and χ2 tests were used to evaluate group differences by age and gender. Probability values were 2-tailed, P < .05. Logistic regression analyses compared categorical dependent variables by group, controlling for age and gender.
Results
Sample Characteristics
Of 332 previously identified patients with FAP who participated in the current study, 133 (40.1%) met criteria for an FGID associated with abdominal pain at follow-up (Table 1). Of the control group, 12 (7.5%) met criteria for a FGID at follow-up; they were excluded from further analysis because there were not enough of these cases to create a distinct comparison group on its own. Thus, the control sample comprised 147 individuals who did not report abdominal pain at baseline or at follow-up. The follow-up interval ranged from 4 to 16 years (M = 8.49; SD = 3.25) and age at follow-up ranged from 12 to 32 years (M = 20.01; SD = 3.79).
TABLE 1.
Sample Characteristics
| Demographic Variables | Participant Group | P | |
|---|---|---|---|
| FAP (n = 332) | Controls (n = 159) | ||
| Sex (% Female) | 63.8 | 54.4 | <.05 |
| Race/ethnicity (% white) | 89.7 | 94.5 | .09 |
| Age at initial evaluation (y) | 11.77 (2.59) | 10.82 (2.09) | <.001 |
| Follow-up interval (y) | 8.96 (3.49) | 7.43 (2.31) | <.001 |
| Age at follow-up (y) | 20.69 (3.94) | 18.46 (2.91) | <.001 |
| Socioeconomic status at follow-up | 39.60 (11.73) | 37.46 | .12 |
| FGIDs at follow-up | 40.1% | 7.5%a | <.001 |
| IBS only | 27.4 | 6.3% | <.001 |
| FD only | 17.8% | 1.9% | <.001 |
| Other FGID (abdominal migraine, FAP) | 5.4% | 0.6% | .01 |
| ≥2 FGIDs | 10.5% | 1.3% | <.001 |
Controls with FGIDs at follow-up were excluded from further analyses.
Lifetime and Current Risk of Psychiatric Disorders
Table 2 presents the lifetime and current risk of all major DSM-IV diagnoses for FAP and control groups. Table 3 presents odds ratios (ORs) and 95% confidence intervals (CIs) comparing the groups on the lifetime and current risk of any anxiety disorder and any depressive disorder, controlling for age and gender.
TABLE 2.
Risk of Lifetime and Current Psychiatric Disorders by Group
| Diagnosis | Lifetime | Current | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| FAP (n = 332) | Controls (n = 147) | P | FAP (n = 332) | Controls (n = 147) | P | |||||
| n | % | n | % | n | % | n | % | |||
| Anxiety disorders | ||||||||||
| Any anxiety disorder | 170 | 51.20% | 30 | 20.41% | <.001 | 101 | 30.42% | 17 | 11.56% | <.001 |
| Separation anxiety | 31 | 9.34% | 6 | 4.08% | .06 | 2 | 0.60% | 0 | 0.00% | 1.00 |
| Panic | 23 | 6.93% | 2 | 1.36% | .06 | 11 | 3.31% | 1 | 0.68% | .24 |
| Agoraphobia | 2 | 0.60% | 1 | 0.68% | .90 | 2 | 0.60% | 1 | 0.68% | .90 |
| Social anxiety | 86 | 25.90% | 9 | 6.12% | <.001 | 40 | 12.05% | 3 | 2.04% | .001 |
| Generalized anxiety | 59 | 17.77% | 9 | 6.12% | .001 | 44 | 13.25% | 6 | 4.08% | <.01 |
| Obsessive-compulsive disorder | 13 | 3.92% | 0 | 0.00% | 1.00 | 9 | 2.71% | 0 | 0.00% | 1.00 |
| Specific phobia | 46 | 13.86% | 11 | 7.48% | .02 | 27 | 8.13% | 6 | 4.08% | 1.00 |
| Posttraumatic stress disorder | 31 | 9.34% | 5 | 3.40% | .12 | 8 | 2.41% | 1 | 0.68% | .21 |
| Acute stress | 0 | 0.00% | 1 | 0.68% | .99 | 0 | 0.00% | 0 | 0.00% | .00 |
| Anxiety NOS | 7 | 2.11% | 2 | 1.36% | .91 | 4 | 1.20% | 1 | 0.68% | .95 |
| Depressive disorders | ||||||||||
| Any depressive disorder | 133 | 40.06% | 24 | 16.33% | <.001 | 20 | 6.02% | 4 | 2.72% | .23 |
| Major depressive disorder | 120 | 36.14% | 21 | 14.29% | <.001 | 17 | 5.12% | 4 | 2.72% | .50 |
| Dysthmia | 14 | 4.22% | 3 | 2.04% | .22 | 3 | 0.90% | 1 | 0.68% | .51 |
| Depression NOS | 4 | 1.20% | 1 | 0.68% | .84 | 0 | 0.00% | 0 | 0.00% | .00 |
| Other disorders | ||||||||||
| Mania | 5 | 1.51% | 0 | 0.00% | 1.00 | 1 | 0.30% | 0 | 0.00% | 1.00 |
| Somatoform | 14 | 4.22% | 0 | 0.00% | 1.00 | 12 | 3.61% | 0 | 0.00% | 1.00 |
| Substance abuse/dependence | 58 | 17.47% | 13 | 8.84% | .15 | 14 | 4.22% | 2 | 1.36% | .11 |
| Eating disorders | 17 | 5.12% | 6 | 4.08% | .97 | 2 | 0.60% | 1 | 0.68% | .89 |
| Disruptive behavior | 25 | 7.53% | 6 | 4.08% | .17 | 8 | 2.41% | 1 | 0.68% | .11 |
Significance level (P) is for logistic regression controlling for gender and age at follow-up. NOS, not otherwise specified.
TABLE 3.
ORs From Logistic Regression Analyses Comparing Risk of Lifetime and Current (at Follow-up) Diagnoses of Anxiety and Depressive Disorders for FAP Group (n = 332) Versus Control Group (n = 147)
| b | SE | Wald | OR | 95% CI | |
|---|---|---|---|---|---|
| Anxiety disorders | |||||
| Any anxiety disorder—lifetime | |||||
| FAP vs control subjects | 1.52*** | 0.25 | 23.91 | 4.59 | 2.83–7.43 |
| Any anxiety disorder—current at follow-up | |||||
| FAP vs control subjects | 1.27*** | 0.30 | 18.59 | 3.57 | 2.00–6.36 |
| Depressive disorders | |||||
| Any depressive disorder—lifetime | |||||
| FAP vs control subjects | 0.96*** | 0.26 | 13.33 | 2.62 | 1.56–4.40 |
| Any depressive disorder—Current at follow-up | |||||
| FAP vs control subjects | 0.68 | 0.58 | 1.41 | 1.98 | 0.64–6.12 |
P < .001.
Anxiety Disorders
A significantly higher proportion of the FAP group met criteria for ≥1 lifetime anxiety disorders compared with the control group (51.2% vs 20.4%). The OR for any lifetime anxiety disorder was 4.59 times greater for FAP compared with controls (CI: 2.83–7.43; P < .001). Similarly, a significantly higher proportion of the FAP group met criteria for ≥1 current anxiety disorders at follow-up compared with the control group (30.4% vs 11.6%). The OR for any current anxiety disorder was 3.57 times greater for FAP compared with controls (CI: 2.00–6.36; P < .001).
The most common anxiety disorder in the FAP group was social anxiety, with approximately one-quarter (25.9%) meeting criteria for social anxiety disorder during their lifetime. Indeed, the OR for social anxiety during their lifetime was 5.84 times greater for the FAP group compared with controls (CI: 2.81–12.15; P < .001). The OR for current social anxiety disorder at follow-up was 8.14 times greater for the FAP group compared with controls (CI: 2.44–27.12; P < .01).
Depressive Disorders
A significantly higher proportion of the FAP group met criteria for a depressive disorder during their lifetime compared with the control group (40.1% vs 16.3%). The OR for any lifetime depressive disorder was 2.62 times greater for FAP compared with controls (CI = 1.56–4.40; P < .001). Risk for current depressive disorder at follow-up was low and did not differ significantly between groups.
Other Psychiatric Disorders
A higher proportion of the FAP group met criteria for lifetime and current somatoform disorders compared with the control group (Lifetime: 4% vs 0%; Current: 3% vs 0%). Lifetime rates of substance abuse/dependence also were higher in FAP than in controls (17.5% vs 8.8%). However, group differences in somatoform and substance abuse/dependence were not significant in logistic regression analyses that controlled for age and gender. Rates of other disorders were low and did not differ significantly by group.
Age of Onset of Psychiatric Disorders and Temporal Relation to FAP Evaluation
Among participants who met criteria for a lifetime anxiety disorder (FAP, n = 170; control, n = 30), the age of onset was in childhood and did not differ significantly for FAP (M = 7.78 years, SD = 5.19) compared with controls (M = 8.97 years, SD = 5.98). The onset of depressive disorders was during adolescence and also did not differ by group (FAP, M = 15.96 years, SD = 4.61; control, M = 14.92 years, SD = 3.76).
Among FAP participants with a lifetime anxiety disorder, the majority (72.62%) reported onset before the age of their FAP evaluation. Among those with a lifetime depressive disorder, the majority (77.27%) reported onset after the age of their FAP evaluation.
Relation of Anxiety and Depressive Disorders to FGID at Follow-up
We subdivided participants in the FAP group into those who met Rome III criteria for an FGID at follow-up (FGID-POS; n = 133, 40.1%) and those who did not meet criteria at follow-up (FGID-NEG; n = 199; 59.9%). Figure 1 shows the risk of lifetime and current anxiety and depressive disorders in the FGID-POS, FGID-NEG, and control groups. Nearly two-thirds of the FGID-POS group (63.9%) met criteria for one or more lifetime anxiety disorders. The FGID-NEG group also had high rates of lifetime anxiety disorders (42.7%) compared with the control group (20.4%). ORs with 95% CIs are presented in Table 4. Controlling for age and gender, the OR for any lifetime anxiety disorder was 7.31 times greater for FGID-POS compared with controls and 3.36 times greater for FGID-NEG compared with controls (P’s < .001). Current anxiety disorders also were more common in the FGID-POS group (39.9%) at follow-up compared with the FGID-NEG (24.12%) and control (11.6%) groups. Specifically, the OR for any current anxiety disorder was 5.09 times greater for FGID-POS compared with controls (P < .001) and 2.68 times greater for FGID-NEG compared with controls (P < .05).
FIGURE 1.
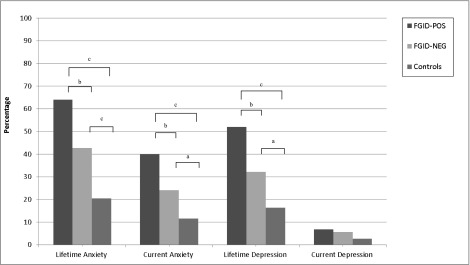
Risk of lifetime and current psychiatric disorders for pediatric patients with FAP who met criteria for FGID at follow-up (FGID-POS), pediatric patients with FAP who did not meet criteria for FGID at follow-up (FGID-NEG), and control subjects. aP < .05; bP < .01; cP < .001.
TABLE 4.
ORs From Logistic Regression Analyses Comparing Risk of Lifetime and Current Diagnoses of Anxiety and Depressive Disorders for FAP With FGID (FGID-POS; n = 133) and Without FGID (FGID-NEG; n = 199) at Follow-Up Versus Control Subjects (n = 147)
| b | SE | Wald | OR | 95% CI | |
|---|---|---|---|---|---|
| Anxiety disorders | |||||
| Any anxiety disorder—lifetime | |||||
| FGID-POS vs control subjects | 1.99*** | 0.29 | 48.31 | 7.31 | 4.17–12.81 |
| FGID-NEG vs control subjects | 1.21*** | 0.26 | 21.22 | 3.36 | 2.01–5.63 |
| Any anxiety disorder—current | |||||
| FGID-POS vs control subjects | 1.63*** | 0.32 | 25.32 | 5.09 | 2.70–9.59 |
| FGID-NEG vs control subjects | 0.99** | 0.32 | 9.68 | 2.68 | 1.44–4.99 |
| Depressive disorders | |||||
| Any Depressive Disorder - Lifetime | |||||
| FGID-POS vs control subjects | 1.42*** | 0.30 | 22.90 | 4.14 | 2.31–7.40 |
| FGID-NEG vs control subjects | 0.61* | 0.30 | 4.49 | 1.84 | 1.05–3.23 |
| Any depressive disorder—current | |||||
| FGID-POS vs control subjects | 0.76 | 0.63 | 1.44 | 2.13 | 0.62–7.34 |
| FGID-NEG vs control subjects | 0.63 | 0.61 | 1.05 | 1.87 | 0.57–6.22 |
Analyses adjusted for gender and age at follow-up. *P < .05; **P < .01; ***P < .001.
Regarding depressive disorders, approximately half of FGID-POS (51.9%) and a third of FGID-NEG (32.2%) met criteria for a lifetime depressive disorder compared with 16.3% of controls. Controlling for age and gender, the OR for a lifetime depressive disorder was 4.14 times greater for FGID-POS compared with controls (P < .001) and 1.84 times greater for FGID-NEG compared with controls (P < .05; Table 4). The risk for any current depressive disorder at follow-up was low and did not differ significantly across FGID-POS, FGID-NEG, and controls.
Discussion
We found a high risk for anxiety disorders at follow-up in pediatric patients with FAP followed prospectively from childhood into adolescence and young adulthood. The data are particularly compelling in that they reflect clinically significant disorders based on clinicians’ judgment that severity or impairment was moderate to high. By the time of follow-up in adolescence and young adulthood, half (51%) of those with a childhood history of FAP had met criteria for an anxiety disorder during their lifetime, and approximately one-third (30%) currently met criteria for an anxiety disorder. In contrast, only one-fifth (20%) of control participants met criteria for an anxiety disorder during their lifetime, and even fewer (12%) met criteria for current anxiety disorder at follow-up. Within the FAP group, risk for anxiety disorder was higher in those who met Rome III criteria at follow-up for FGID compared with those without FGID at follow-up. Nonetheless, even those without FGID at follow-up had significantly higher risk for anxiety disorder compared with controls. Thus, anxiety in patients with pediatric-onset FAP persisted over time even in the absence of abdominal pain associated with FGID.
For the majority of the FAP group, diagnostic interviews placed the onset of anxiety disorders before the pediatric gastroenterology evaluation that coincided with their enrollment in the study. Because they already had abdominal pain before their pediatric evaluation, the temporal relation between the onset of FAP and the onset of anxiety cannot be determined from these data. Nonetheless, both FAP and anxiety appear to have begun early in childhood. Interestingly, a recent study of children with anxiety disorders reported that 41% had symptoms of FGID compared with 6% of children without anxiety disorders.28 It is possible that FAP and anxiety share a common vulnerability such as a genetic variant that influences both pain sensitivity and psychological distress.29 Recent work also links low-grade inflammation to gastrointestinal symptoms as well as to anxiety.30–32 It also is possible that anxiety may arise secondary to pain in some individuals and yet serve a maintaining role in pain.
The association between FAP and anxiety can be understood within a biopsychosocial framework that recognizes the importance of emotional and social contextual processes in the experience of pain.33–36 Anxiety can alter pain sensitivity by increasing vigilance to potential threat, influencing pain coping,37 and disrupting endogenous opioid pain-control systems.37 Selective attention to pain-related information38–41 and a low threshold for alarm42 may lead patients with FAP to attend to minor discomfort and withdraw from activities, thereby potentially exacerbating their emotional distress. Abdominal pain also may legitimize children’s absence from school and other activities43; parents may try to protect their child with FAP from settings associated with pain. Without such exposure, however, children lack opportunities to learn to cope effectively with both pain and anxiety. Social anxiety, which was common in individuals with a history of FAP, may be particularly insidious in driving a fear-avoidance cycle of pain44,45 that can maintain withdrawal from social settings in which pain had been experienced previously.46
Regarding depressive disorders, lifetime risk was significantly higher in individuals with a history of FAP compared with controls (40% vs 16%), but, in contrast to anxiety disorders, depressive disorders were more likely to have developed subsequent to the medical evaluation for FAP. Current depressive disorders were rare at follow-up, however, and did not differ between individuals with a history of FAP and control subjects. Campo and colleagues13 similarly found that mood disorders were not significantly elevated in young adults with a history of FAP. Nonetheless, it is possible that pediatric FAP is associated with increased risk of depressive disorders, but because depression has a later onset and a more episodic course than anxiety disorders,47 we did not detect increased risk at the single, snapshot evaluation conducted in adolescence or early adulthood.
Risk of somatoform disorders was low and, after controlling for age and gender, did not differentiate the FAP and control groups. The DSM-IV criteria for somatoform disorders have shortcomings48 and may be replaced by a category of “somatic symptom disorders”;49 the proposed new diagnostic criteria may better distinguish individuals with and without a history of FAP.
Patients with FAP were enrolled in this study at the time of their evaluation at a tertiary care center. This ensured that all patients underwent a comprehensive subspecialty evaluation to rule out significant underlying organic disease but also represents a study limitation in that findings cannot generalize to children evaluated in primary care settings. A recent review reported that abdominal pain outcomes were similar in patients with and without a tertiary care evaluation,12 but no comparable data are available regarding psychological outcomes. It also should be noted that the age range at follow-up spanned adolescence and young adulthood and that the risk for some psychiatric disorders, such as depression, increases with age. This limitation was mitigated in part by controlling for age at follow-up in all analyses.
Conclusions
This study extends the literature linking pediatric FAP to anxiety disorders7,10,11,50 with prospective data showing that patients with FAP continue to experience high rates of anxiety disorders into adolescence and young adulthood. Patients with FAP also had high rates of depressive disorders during their lifetime, but few met criteria for a depressive disorder at the time of follow-up.
This is the first study of pediatric FAP to integrate mental health and abdominal pain outcomes. Notably, even individuals with a childhood history of FAP who did not meet FGID symptom criteria at follow-up still had significantly higher rates of anxiety disorders compared with controls. Social anxiety disorder was particularly common in the pediatric FAP patients and may contribute to school absence and withdrawal from social activities, thereby perpetuating pain-related disability.51
A decade after the seminal work by Campo et al,13 these data underscore the importance of a biopsychosocial approach to FAP that includes screening for anxiety and depression. Future research should evaluate whether interventions that treat mental health problems in FAP improve abdominal pain outcomes.
Acknowledgments
We thank those who served as psychiatric diagnostic interviewers for this study, including Hollister Trott, Mary Payne, and Shelly Ball.
Glossary
- CI
confidence interval
- DSM-IV
Diagnostic and Statistical Manual of Mental Disorders, 4th edition
- FAP
functional abdominal pain
- FGID
functional gastrointestinal disorder
- FGID-POS
positive for FGID
- FGID-NEG
negative for FGID
- OR
odds ratio
Footnotes
Dr Shelby conducted psychiatric diagnostic interviews, drafted the initial manuscript, conducted data analyses, and reviewed and revised the manuscript; Dr Shirkey and Ms Sherman conducted psychiatric diagnostic interviews and critically reviewed the manuscript; Dr Beck supervised and conducted psychiatric diagnostic interviews, conducted data analysis, and critically reviewed the manuscript; Dr Haman supervised psychiatric diagnostic interviews, conducted data analysis, and critically reviewed the manuscript; Ms Shears coordinated data collection and critically reviewed the manuscript; Dr Horst reviewed medical records, conducted data analysis, and critically reviewed the manuscript; Dr Smith contributed to conceptualizing and designing the study, supervised data analysis and critically reviewed the manuscript; Dr Garber contributed to conceptualizing and designing the study, provided oversight of psychiatric diagnostic interviewing, and critically reviewed the manuscript; Dr Walker contributed to conceptualizing and designing the study, supervised research activities, oversaw writing of the manuscript, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grant R01 HD23264 (L.S. Walker, principal investigator) from the National Institute on Child Health and Development and does not represent official views of the Institute. Support was also provided by Vanderbilt Kennedy Center (grant P30 HD15052), Vanderbilt Digestive Disease Research Center (grant DK058404), and the Vanderbilt CTSA (grant 1 UL1 RR024975) from the National Center for Research Resources, National Institutes of Health. Grace Shelby was supported in part by a training grant from the National Institutes of Mental Health (grant T32-MH18921). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Apley J, Hale B. Children with recurrent abdominal pain: how do they grow up? BMJ. 1973;3(5870):7–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chitkara DK, Rawat DJ, Talley NJ. The epidemiology of childhood recurrent abdominal pain in Western countries: a systematic review. Am J Gastroenterol. 2005;100(8):1868–1875 [DOI] [PubMed] [Google Scholar]
- 3.Saps M, Seshadri R, Sztainberg M, Schaffer G, Marshall BM, Di Lorenzo C. A prospective school-based study of abdominal pain and other common somatic complaints in children. J Pediatr. 2009;154(3):322–326 [DOI] [PubMed] [Google Scholar]
- 4.Hyams JS, Burke G, Davis PM, Rzepski B, Andrulonis PA. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr. 1996;129(2):220–226 [DOI] [PubMed] [Google Scholar]
- 5.Robinson JO, Alverez JH, Dodge JA. Life events and family history in children with recurrent abdominal pain. J Psychosom Res. 1990;34(2):171–181 [DOI] [PubMed] [Google Scholar]
- 6.Walker LS, Guite JW, Duke M, Barnard JA, Greene JW. Recurrent abdominal pain: a potential precursor of irritable bowel syndrome in adolescents and young adults. J Pediatr. 1998;132(6):1010–1015 [DOI] [PubMed] [Google Scholar]
- 7.Campo JV, Bridge J, Ehmann M, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004;113(4):817–824 [DOI] [PubMed] [Google Scholar]
- 8.Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130(5):1527–1537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baber KF, Anderson J, Puzanovova M, Walker LS. Rome II versus Rome III classification of functional gastrointestinal disorders in pediatric chronic abdominal pain. J Pediatr Gastroenterol Nutr. 2008;47(3):299–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garber J, Zeman J, Walker LS. Recurrent abdominal pain in children: psychiatric diagnoses and parental psychopathology. J Am Acad Child Adolesc Psychiatry. 1990;29(4):648–656 [DOI] [PubMed] [Google Scholar]
- 11.Dufton LM, Dunn MJ, Compas BE. Anxiety and somatic complaints in children with recurrent abdominal pain and anxiety disorders. J Pediatr Psychol. 2009;34(2):176–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gieteling MJ, Bierma-Zeinstra SM, Passchier J, Berger MY. Prognosis of chronic or recurrent abdominal pain in children. J Pediatr Gastroenterol Nutr. 2008;47(3):316–326 [DOI] [PubMed] [Google Scholar]
- 13.Campo JV, Di Lorenzo C, Chiappetta L, et al. Adult outcomes of pediatric recurrent abdominal pain: do they just grow out of it? Pediatrics. 2001;108(1). Available at: www.pediatrics.org/cgi/content/full/108/1/e1 [DOI] [PubMed] [Google Scholar]
- 14.Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002;122(4):1140–1156 [DOI] [PubMed] [Google Scholar]
- 15.Drossman DA, Dumitrascu DL. Rome III: new standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15(3):237–241 [PubMed] [Google Scholar]
- 16.Walker LS, Baber KF, Garber J, Smith CA. A typology of pain coping strategies in pediatric patients with chronic abdominal pain. Pain. 2008;137(2):266–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker LS, Garber J, Smith CA, Van Slyke DA, Claar RL. The relation of daily stressors to somatic and emotional symptoms in children with and without recurrent abdominal pain. J Consult Clin Psychol. 2001;69(1):85–91 [PMC free article] [PubMed] [Google Scholar]
- 18.Walker LS, Smith CA, Garber J, Claar RL. Testing a model of pain appraisal and coping in children with chronic abdominal pain. Health Psychol. 2005;24(4):364–374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dengler-Crish CM, Bruehl S, Walker LS. Increased wind-up to heat pain in women with a childhood history of functional abdominal pain. Pain. 2011;152(4):802–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walker LS, Dengler-Crish CM, Rippel S, Bruehl S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain. 2010;150(3):568–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain. 2012;153(9):1798–1806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DiNardo P, Brown T, Barlow D. Anxiety Disorders Interview Schedule for DSM-IV: Client Interview Schedule. San Antonio, TX: Psychological Corporation; 1994 [Google Scholar]
- 23.Silverman W, Albano A. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Child and Parent Versions. San Antonio, TX: Psychological Corporation; 1996 [Google Scholar]
- 24.Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: implications for the classification of emotional disorders. J Abnorm Psychol. 2001;110(1):49–58 [DOI] [PubMed] [Google Scholar]
- 25.Lyneham HJ, Abbott MJ, Rapee RM. Interrater reliability of the Anxiety Disorders Interview Schedule for DSM-IV: child and parent version. J Am Acad Child Adolesc Psychiatry. 2007;46(6):731–736 [DOI] [PubMed] [Google Scholar]
- 26.Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. J Am Acad Child Adolesc Psychiatry. 2001;40(8):937–944 [DOI] [PubMed] [Google Scholar]
- 27.Hollingshead A. Four Factor Index of Social Status. New Haven, CT: Yale University; 1975 [Google Scholar]
- 28.Waters A, Schilpzand E, Bell C, Walker L, Baber K. Functional gastrointestinal symptoms in children with anxiety disorders. J Abnorm Child Psychol. 2013;41(1):151–163 [DOI] [PubMed] [Google Scholar]
- 29.Diatchenko L, Nackley AG, Slade GD, Fillingim RB, Maixner W. Idiopathic pain disorders—pathways of vulnerability. Pain. 2006;123(3):226–230 [DOI] [PubMed] [Google Scholar]
- 30.O’Donovan A, Slavich GM, Epel ES, Neylan TC. Exaggerated neurobiological sensitivity to threat as a mechanism linking anxiety with increased risk for diseases of aging. Neurosci Biobehav Rev. 2013;37(1):96–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Öhman L, Simrén M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat Rev Gastroenterol Hepatol. 2010;7(3):163–173 [DOI] [PubMed] [Google Scholar]
- 32.Salim S, Chugh G, Asghar M. Inflammation in anxiety. In: Donev R, ed. Advances in Protein Chemistry and Structural Biology. Vol 88 Oxford, UK: Academic Press; 2012:1–25 [DOI] [PubMed] [Google Scholar]
- 33.Asmundson GJ, Katz J. Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety. 2009;26(10):888–901 [DOI] [PubMed] [Google Scholar]
- 34.Campbell CM, Edwards RR. Mind-body interactions in pain: the neurophysiology of anxious and catastrophic pain-related thoughts. Transl Res. 2009;153(3):97–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rhudy JL. The importance of emotional processes in the modulation of pain. Pain. 2009;146(3):233–234 [DOI] [PubMed] [Google Scholar]
- 36.Naliboff BD, Munakata J, Chang L, Mayer EA. Toward a biobehavioral model of visceral hypersensitivity in irritable bowel syndrome. J Psychosom Res. 1998;45(6):485–492 [DOI] [PubMed] [Google Scholar]
- 37.Naliboff BD, Rhudy JL. Anxiety in functional pain disorders In Mayer EA, Bushnell, MC, eds. Functional Pain Disorders: Presentation and Pathophysiology. Seattle: IASP Press; 2009:185–214 [Google Scholar]
- 38.Aldrich S, Eccleston C, Crombez G. Worrying about chronic pain: vigilance to threat and misdirected problem solving. Behav Res Ther. 2000;38(5):457–470 [DOI] [PubMed] [Google Scholar]
- 39.Beck JE, Lipani TA, Baber KF, et al. Attentional bias to pain and social threat in pediatric patients with functional abdominal pain and pain-free youth before and after performance evaluation. Pain. 2011;152(5):1061–1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boyer MC, Compas BE, Stanger C, et al. Attentional biases to pain and social threat in children with recurrent abdominal pain. J Pediatr Psychol. 2006;31(2):209–220 [DOI] [PubMed] [Google Scholar]
- 41.Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol Bull. 1999;125(3):356–366 [DOI] [PubMed] [Google Scholar]
- 42.Bakker M, Boer F, Benninga M, Koelman J, Tijssen M. Increased auditory startle reflex in children with functional abdominal pain. J Pediatr. 2010;156(2):285–291, e281 [DOI] [PubMed]
- 43.Simons LE, Logan DE, Chastain L, Stein M. The relation of social functioning to school impairment among adolescents with chronic pain. Clin J Pain. 2010;26(1):16–22 [DOI] [PubMed] [Google Scholar]
- 44.Lethem J, Slade PD, Troup JD, Bentley G. Outline of a fear-avoidance model of exaggerated pain perception—I. Behav Res Ther. 1983;21(4):401–408 [DOI] [PubMed] [Google Scholar]
- 45.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332 [DOI] [PubMed] [Google Scholar]
- 46.Labus JS, Mayer EA, Chang L, Bolus R, Naliboff BD. The central role of gastrointestinal-specific anxiety in irritable bowel syndrome: further validation of the visceral sensitivity index. Psychosom Med. 2007;69(1):89–98 [DOI] [PubMed] [Google Scholar]
- 47.Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J. Childhood and adolescent depression: a review of the past 10 years. Part II. J Am Acad Child Adolesc Psychiatry. 1996;35(12):1575–1583 [DOI] [PubMed] [Google Scholar]
- 48.Crombez G, Beirens K, Van Damme S, Eccleston C, Fontaine J. The unbearable lightness of somatisation: a systematic review of the concept of somatisation in empirical studies of pain. Pain. 2009;145(1–2):31–35 [DOI] [PubMed] [Google Scholar]
- 49.Voigt K, Wollburg E, Weinmann N, et al. Predictive validity and clinical utility of DSM-5 Somatic symptom disorder—comparison with DSM-IV somatoform disorders and additional criteria for consideration. J Psychosom Res. 2012;73(5):345–350 [DOI] [PubMed] [Google Scholar]
- 50.Knook LM, Konijnenberg AY, van der Hoeven J, et al. Psychiatric disorders in children and adolescents presenting with unexplained chronic pain: what is the prevalence and clinical relevancy? Eur Child Adolesc Psychiatry. 2011;20(1):39–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Logan DE, Simons LE, Carpino EA. Too sick for school? Parent influences on school functioning among children with chronic pain. Pain. 2012;153(2):437–443 [DOI] [PMC free article] [PubMed] [Google Scholar]


