Abstract
OBJECTIVES:
Using longitudinal data from the multigenerational Youth Development Study (YDS), this article documents how parents’ long-term smoking trajectories are associated with adolescent children’s likelihood of smoking. Prospective data from the parents (from age 14–38 years) enable unique comparisons of the parents’ and children’s smoking behavior, as well as that of siblings.
METHODS:
Smoking trajectories are constructed using latent class analysis for the original YDS cohort (n = 1010). Multigenerational longitudinal data from 214 parents and 314 offspring ages 11 years and older are then analyzed by using logistic regression with cluster-corrected SEs.
RESULTS:
Four latent smoking trajectories emerged among the original cohort: stable nonsmokers (54%), early-onset light smokers who quit/reduce (16%), late-onset persistent smokers (14%), and early-onset persistent heavy smokers (16%). Although 8% of children of stable nonsmokers smoked in the last year, the other groups’ children had much higher percentages, ranging from 23% to 29%. Multivariate logistic regression models confirm that these significant differences were robust to the inclusion of myriad child- and parent-level measures (for which child age and grade point average [GPA] are significant predictors). Older sibling smoking, however, mediated the link between parental heavy smoking and child smoking.
CONCLUSIONS:
Even in an era of declining rates of teenage cigarette use in the United States, children of current and former smokers face an elevated risk of smoking. Prevention efforts to weaken intergenerational associations should consider parents’ long-term cigarette use, as well as the smoking behavior of older siblings in the household.
Keywords: cigarette use, multigenerational effects, parent smoking, sibling smoking, socioeconomic background
What’s Known on This Subject:
Adolescents are likely to smoke if their parent(s) smoke. Little research uses prospective longitudinal data from parents and children to more confidently document these intergenerational associations, alongside potential confounders (parental education) and mediators (school achievement, mental health, older sibling smoking).
What This Study Adds:
Analyses of long-term multigenerational data show how diverse parental smoking trajectories influence child smoking, controlling for measured confounders. The risk of smoking is especially high among children residing with a persistent heavy smoking parent and an older sibling who smokes.
The rates of smoking among adolescents in the United States have declined dramatically since 1997, although 6% of 8th graders and 12% of 10th graders in 2011 reported smoking in the past month.1 Adolescent cigarette use is both heritable and influenced by environmental factors.2 In particular, adolescents have an elevated risk of smoking if their parent(s) smoke. This intergenerational association may reflect the relatively strong genetic influence on tobacco use compared with other substances or the modeling and reinforcement of parental smoking behavior by offspring.3,4 Parental smoking may also elevate the risk of offspring cigarette use through child school failure, psychological distress, or weakened attachment to parents, as well as factors such as low parental education or older sibling cigarette use.
Several studies have investigated these intergenerational influences on adolescents’ cigarette use.5 Although cross-sectional,6–11 follow-up,12–15 and longitudinal16–18 studies of adolescents have shown a relationship between parental and child smoking, the overall body of research remains equivocal.5 Previous studies have been limited by the use of retrospective reports of parent smoking, the use of offspring reports of parental smoking and other parent-level risk factors, and the lack of detailed measures encompassing the duration and intensity of parental cigarette use.5 Multigenerational, longitudinal research moves beyond this limitation, helping to establish a stronger link between parents’ and adolescents’ reports of smoking.18–21 An advantage of such studies is the ability to model changes in parental smoking prospectively, providing evidence that parental smoking cessation is associated with lower use and cessation among adolescents.22–26
Despite these advantages, few studies within the United States have used prospective parental data that was not exclusively concurrent with the adolescent data.19,21 In one of the most detailed studies to date using 8 waves of data, Chassin et al19 show that various parental smoking trajectories, beginning in adolescence, influenced whether their subsequently surveyed children had ever smoked. In particular, children of parents with early-onset and persistent smoking had the highest odds of ever smoking; these effects were robust to potentially confounding risk factors such as parental education and adolescents’ personality characteristics.
We add several innovations to this emerging line of research by examining the smoking behavior of 214 parents and 314 offspring in the multigenerational, longitudinal Youth Development Study (YDS). First, our dataset provides prospective measures of the intensity of parental cigarette use on 10 occasions over a 23-year period (age 14–38 years). This measurement design allows us to examine long-term trajectories of parental smoking patterns and the risk of their adolescent children’s cigarette use. Second, we test for several confounders, such as parental education, marital status, employment, and gender, as well as child depressive affect, self-esteem, closeness to parents, grade point average (GPA), age, race/ethnicity, and gender.1,2,11,15,17,19,27–33 In addition, the single cohort reduces any confounding effects that may be attributable to differing ages of the parents at the various survey waves. Third, data collected directly from siblings allows a unique examination of the influence of older-sibling smoking, which has emerged as an important consideration in intergenerational research.34,35 Finally, these intergenerational analyses examine current adolescent smoking, rather than lifetime smoking, to more fully establish temporal ordering in the intergenerational transmission of cigarette use.
Methods
Data
The YDS began in 1988 with a randomly selected sample of ninth graders enrolled in the St Paul Public School District in Minnesota (n = 1010).36 Those who provided consent (64%) did not differ from nonconsenters on numerous census tract characteristics.37 From 1988 to 2011, respondents completed up to 19 follow-up surveys, assessing changes in school, work, and family, as well as health and well-being. In 2009, a second-generation study began that continues to recruit and annually survey children of the original cohort who are aged 11 years and older. Since information gathering began for the second-generation study in 2004, 86% of the original YDS respondents completed at least 1 survey. Of those respondents, 50% had a child who was at least 11 years old, and thus eligible for the second-generation study. Approximately 59% of parents who had a child that was eligible provided signed consent, and 84% of these children participated in the study. Parents with higher levels of education and income were more likely to consent.38 Questionnaires were mailed to the child’s place of residence and replicated to a large degree the surveys that were asked of the original cohort when they were adolescents. To ensure temporal ordering in these analyses, we use the most recent wave of child data in 2011, giving us a total of 314 children from 214 parents of the original cohort. The University of Minnesota Institutional Review Board approved the study.
Measures
Child Data
The outcome measure is whether the child reported any tobacco smoking within the last year (2011). Descriptive statistics for all child and parent measures are shown in Table 1, with 16% of the children reporting smoking in the last year. Among the predictors, we include age (in years), race/ethnicity (1 = white non-Hispanic; 0 = other race/ethnicity), and gender (1 = boys; 0 = girls). We also include measures of depressive affect, self-esteem, closeness to parent, and GPA as potential mediators of intergenerational smoking behavior. GPA is a numeric version of the letter grade reported by the adolescent. Depressive affect is a 5-item additive scale (Cronbach α = 0.92), indicating how often the teenager felt downhearted and blue, in any strain, stress, or pressure, moody or brooded about things, in low spirits, or depressed.36 Self-esteem is a 3-item additive scale (Cronbach α = 0.72), consisting of agreement with having good qualities, taking a positive attitude toward oneself, and satisfaction with oneself as a whole.36 Closeness to the parent respondent is dichotomized as “not at all” (coded 0) versus all other responses (“extremely,” “quite,” “fairly” all coded 1). Finally, we test the influence of sibling smoking behavior by including the actual survey responses from older siblings in analyses.
TABLE 1.
Descriptive Statistics (2011)
| Variable | Percentage or Mean (SD) | Range | Child-Level Cases Imputed |
|---|---|---|---|
| Parent measures (n = 214) | |||
| Currently married | 54.8% | — | 11 (3.5%) |
| Education level | 11 (3.5%) | ||
| High school or less | 24.1% | — | — |
| Associates or vocational/technical | 30.0% | — | — |
| Some college | 30.4% | — | — |
| Bachelor’s or higher | 15.5% | — | — |
| Male gender | 25.2% | — | 0 (0.0%) |
| Currently employed | 73.9% | — | 11 (3.5%) |
| Smoking trajectories | 24 (7.6%) | ||
| Early-onset light smokers who quit/reduce | 18.3% | — | — |
| Late-onset persistent smokers | 9.7% | — | — |
| Early-onset persistent heavy smokers | 20.7% | — | — |
| Stable nonsmokers | 51.4% | — | — |
| Children measures (n = 314) | |||
| Smoking in last year | 16.2% | — | 0 (0.0%) |
| Age | 14.72 (2.79) | 11–21 | 2 (0.6%) |
| White, non-Hispanic race | 59.3% | — | 9 (2.9%) |
| Male gender | 44.1% | — | 1 (0.3%) |
| Depressive affect | 11.59 (4.88) | 5–25 | 5 (1.6%) |
| Grade point average | 2.98 (0.78) | 0–4 | 35 (11.1%) |
| Self-esteem | 9.36 (1.53) | 4–12 | 9 (2.9%) |
| Close to parent respondent | 92.0% | — | 38 (12.1%) |
| Older sibling smoker | 8.0% | — | 0 (0.0%) |
—, not applicable.
Parent Data
Across the 19 waves of parental data, cigarette smoking was assessed on 4 occasions during the teenage years (ages 14–18 years), 4 times in young adulthood (ages 21–27 years), and twice in adulthood (ages 35–38 years), with the most recent 2011 assessment overlapping with the survey of their children. Respondents indicated how often they had smoked cigarettes during the previous 30 days, with responses ranging on 4-point scales from “none at all” to “about 1 pack or more per day.” We use these 10 occasions to construct latent smoking trajectories.
From the 2011 parent survey, we also included measures of marital status, job holding, education attainment, and gender. Education attainment was measured by using 4 dummy variables: high school or less, associate’s degree or vocational/technical degree, some college but no degree, and bachelor’s degree or higher. Because early child-bearers typically have less post-secondary education than later child-bearers, relatively few parents had attained a bachelor’s degree or higher by 2011 (∼16%). For example, the parents of the youngest 11-year-old children in 2011 were approximately age 27 years at the child’s birth. Parents of 20-year-old children were 18 years old. Similarly, the lower percentage of men (25%) in our sample is attributable to women’s younger average age of parenthood.
Methods
We first constructed parental smoking trajectories via a nonparametric latent class trajectory analysis. The analysis models the probability of falling into any given smoking category, dependent only on time. We can write such a model as
 |
where the probability of the left-hand side is the joint probability over the observed smoking categories at each time and latent trajectory  . The right-hand side consists of the product of the set of conditional probabilities for the observed smoking categories given the latent trajectories (inside the bracket); and the unconditional probability of the latent trajectories (outside the bracket). Thus, estimates of the conditional probabilities
. The right-hand side consists of the product of the set of conditional probabilities for the observed smoking categories given the latent trajectories (inside the bracket); and the unconditional probability of the latent trajectories (outside the bracket). Thus, estimates of the conditional probabilities  give the probability of falling into a given smoking category by time (ie, age) within a trajectory, whereas
give the probability of falling into a given smoking category by time (ie, age) within a trajectory, whereas  gives the overall probability of each trajectory. Because missing data represent another discrete category, all 1010 original respondents are included. By exploiting the person-period nature of the data, we estimated the model in a single stage using a nonparametric latent class specification in Latent Gold.39,40 The Bayesian information criterion was used to guide model selection.41
gives the overall probability of each trajectory. Because missing data represent another discrete category, all 1010 original respondents are included. By exploiting the person-period nature of the data, we estimated the model in a single stage using a nonparametric latent class specification in Latent Gold.39,40 The Bayesian information criterion was used to guide model selection.41
After estimating the latent class model, each parent was assigned to her or his modal smoking trajectory. We then assessed how these trajectories, as well as other parent and child measures, related to child smoking using χ2 tests for categorical predictors and t tests for continuous predictors. For multivariate analyses, we used the “cluster” option within the “logit” procedure in Stata 12.0,42 which adjusts the standard errors to account for the clustering of siblings within parents.43 We use chained multiple imputation via the “mi” procedure within Stata to impute missing data for the predictors where valid data existed for the response variable. Table 1 shows the number of cases imputed for each variable, which is low. With 1 exception, in analyses not shown we found that the 4 potentially influential selection mechanisms discussed previously (original cohort retention from waves 15 to 19; having child(ren) ages 11 years or older; consenting to child(ren) participation; child(ren) participation) were unrelated to the 4 non-missing parental latent smoking trajectories discussed subsequently. Respondents in the heavy smoking trajectory were more likely to have child(ren) who were ages 11 years or older.
Results
Parental Smoking Trajectories
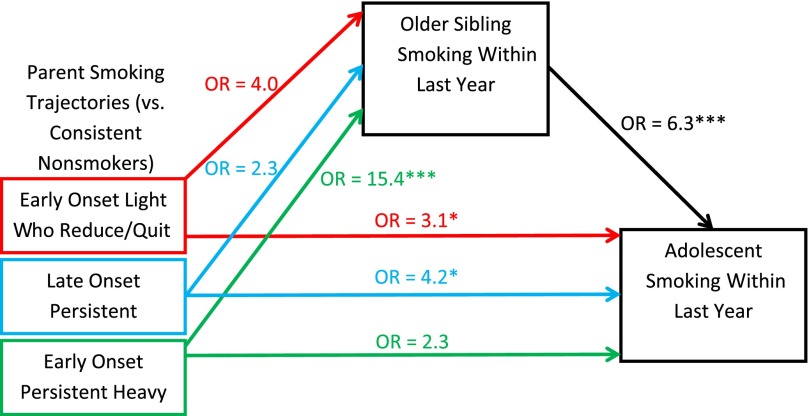
As shown in Table 2, the BIC statistic demonstrates that the best-fitting model has 5 latent trajectories and is acceptable according to the 2 measures of error. These parental smoking trajectories are depicted in Fig 1. Trajectory 1 consists of early-onset light smokers who quit or reduced use, constituting 16% of the original YDS cohort. By the end of high school, respondents in this trajectory had only a 14% probability of not smoking, with 1 to 5 cigarettes as the dominant category at 48% and a low chance of a pack daily throughout. By 2011, however, the “none” category increased to 60%, with major reductions in smoking. Trajectory 2 consists of late-onset persistent smokers, constituting 14% of the sample. Among this trajectory, the odds of not smoking in high school are very high (95% their junior year). By 1999 (age 25 years), this probability drops precipitously to as low as 9%. By 2011, all the categories are roughly of equal probability, although the smoking categories together make up 67%.
TABLE 2.
Fit Statistics for Latent Class Smoking Trajectories for Original Youth Development Study Cohort (1988–2011)
| Latent Classes | Log-likelihood | Parameters | BIC Statistic | Classification Errors | Reduction Errors |
|---|---|---|---|---|---|
| 1 | −12643.89 | 40 | 25656.60 | — | — |
| 2 | −10870.80 | 81 | 22488.43 | 0.02 | 0.95 |
| 3 | −10228.84 | 122 | 21582.56 | 0.03 | 0.95 |
| 4 | −9872.40 | 163 | 21247.70 | 0.05 | 0.92 |
| 5 | −9678.56 | 204 | 21238.07 | 0.04 | 0.92 |
| 6 | −9512.64 | 245 | 21284.26 | 0.04 | 0.92 |
| 7 | −9387.92 | 286 | 21412.85 | 0.05 | 0.92 |
BIC, Bayesian information criterion; —, not applicable.
FIGURE 1.
Smoking trajectories from latent class analysis for original YDS cohort (1988–2011).
Trajectory 3 represents early-onset persistent smokers, which are 16% of the original cohort. By the end of high school, the probability of smoking at least a half pack a day is 89% for respondents in this trajectory, with 54% smoking at least 1 pack daily. At its height in 1995, there is a 97% probability of smoking half a pack or more daily, with 71% smoking a pack daily. There is a noticeable reduction in the probability of smoking a pack daily, but the probability of not smoking only rises as high as 26% at the last observation in 2011. Finally, the majority of respondents fall into Trajectory 4 (54%), or stable nonsmokers. As shown in Fig 1, the probability of not smoking for this trajectory never falls below 92% during the period of observation.
The fifth trajectory (not shown in Fig 1) represents respondents who attritted from the study early, thus providing limited information on their smoking trajectory. In addition, the percentages reported previously are adjusted for missing values. Instead, we report the percentage who were missing by trajectory in Appendix Table. In the child-level analyses (described next), this trajectory is treated as missing, but attrition is built directly into the remaining trajectories.
Child-Level Analysis
Table 3 shows bivariate tests of independence of child’s smoking and the predictor variables. Children who reported smoking in the past year were significantly higher with regard to age and depressive affect, while lower on GPA and self-esteem. They were more likely to feel “not at all” close to their parents, as well as to have an older sibling who reported smoking. Among the parent measures, children of the stable nonsmokers are by far the lowest in terms of smoking in the last year (8%). The other 3 parental smoking trajectories are similar in terms of their children’s use, ranging from 23% to 29%. For the other parent-level measures, adolescent smoking is lowest among parents who are married, have a bachelor’s degree, or are male, although only marriage reaches the standard level of statistical significance (P < .05). Note that supplemental analyses (not shown) using alternate codings of parental education that distinguished high school dropouts from completers neither produced statistically significant results nor altered any of the results presented in Table 4.
TABLE 3.
Adolescent Last Year Smoking (2011) by Parent- and Child-Level Predictors
| Variable | Percentage Last Year Smoking | 95% CI |
|---|---|---|
| Parent measuresa | ||
| Currently married* | ||
| No | 21.9 | 15.7–29.6 |
| Yes | 12.7 | 8.4–18.7 |
| Education level | ||
| High school or less | 20.6 | 12.8–31.4 |
| Associate’s or vocational/technical | 17.6 | 11.0–26.9 |
| Some college | 16.3 | 10.1–25.4 |
| Bachelor’s degree or higher | 10.6 | 4.5–23.2 |
| Gender | ||
| Female | 17.9 | 13.5–23.3 |
| Male | 11.4 | 6.0–20.5 |
| Currently employed | ||
| No | 19.0 | 11.8–29.2 |
| Yes | 16.1 | 11.8–21.5 |
| Smoking trajectori*** | ||
| Early-onset light smokers who quit/reduce | 22.6 | 13.3–35.9 |
| Late-onset persistent smokers | 28.6 | 14.9–47.7 |
| Early-onset persistent heavy smokers | 25.0 | 15.6–37.5 |
| Stable nonsmokers | 8.1 | 4.6–13.7 |
| Children measures | ||
| Race | ||
| Non-white | 16.9 | 11.3–24.6 |
| White–non-Hispanic | 14.9 | 10.4–20.9 |
| Gender | ||
| Female | 16.0 | 11.3–22.2 |
| Male | 16.7 | 11.3–23.9 |
| Close to parent respondent* | ||
| No | 31.8 | 15.9–53.5 |
| Yes | 12.6 | 9.0–17.3 |
| Older sibling smoker*** | ||
| No | 14.2 | 10.6–18.7 |
| Yes | 40.0 | 23.0–59.9 |
| Last Year Nonsmokers: Average (95% CI) | Last Year Smokers: Average (95% CI) | |
| Age*** | 14.28 (13.96–14.61) | 16.92 (16.22–17.61) |
| Depressive affect*** | 11.16 (10.59–11.74) | 13.77 (12.31–15.22) |
| Grade point average*** | 3.07 (2.98–3.16) | 2.40 (2.11–2.69) |
| Self-esteem** | 9.46 (9.27–9.65) | 8.82 (8.42–9.22) |
CI, confidence interval.
Parent averages and tests are not adjusted for clustering of siblings within parent.
P < .05;
P < .01;
P < .001 (χ2 tests for categorical predictors; 2-tailed t tests for continuous predictors).
TABLE 4.
Logistic Regression Models of Adolescent Last Year Smoking (2011), with Multiple Imputation and Cluster-Corrected Standard Errors
| Model 1: Unadjusted Effects of Parental Smoking Trajectories | Model 2: Including Parent- and Child-Level Controls | Model 3: Including Indicator of Older Sibling Smoker | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Parent measures (n = 214) | ||||||
| Smoking trajectories (vs consistent nonsmoker) | ||||||
| Early-onset light smokers who quit/reduce | 3.24* | 1.28–8.17 | 3.50* | 1.12–10.95 | 3.14* | 1.07–9.21 |
| Late-onset persistent smokers | 4.63** | 1.60–13.39 | 4.34* | 1.32–14.32 | 4.24* | 1.36–13.22 |
| Early-onset persistent heavy smokers | 3.78** | 1.55–9.24 | 3.38* | 1.10–10.41 | 2.25 | 0.75–6.73 |
| Currently married | — | — | 1.01 | 0.43–2.36 | 1.01 | 0.47–2.15 |
| Education level (vs high school or less) | ||||||
| Associate’s degree or vocational/technical | — | — | 1.08 | 0.39–2.98 | 1.12 | 0.43–2.93 |
| Some college | — | — | 1.65 | 0.55–4.97 | 1.70 | 0.57–5.08 |
| Bachelor’s degree or higher | — | — | 1.55 | 0.30–8.02 | 1.52 | 0.30–7.70 |
| Male (vs female) | — | — | 0.85 | 0.31–2.32 | 1.09 | 0.40–3.00 |
| Currently employed (vs not employed) | — | — | 0.94 | 0.37–2.39 | 0.86 | 0.36–2.05 |
| Children measures (n = 314) | ||||||
| Age | — | — | 1.36*** | 1.15–1.60 | 1.45*** | 1.22–1.73 |
| White–non-Hispanic (vs non-White) | — | — | 1.22 | 0.53–2.81 | 1.36 | 0.59–3.12 |
| Male (vs female) | — | — | 1.19 | 0.47–2.97 | 1.30 | 0.50–3.33 |
| Depressive affect | — | — | 1.03 | 0.93–1.14 | 1.04 | 0.93–1.15 |
| Grade point average | — | — | 0.45* | 0.24–0.83 | 0.47* | 0.26–0.86 |
| Self-esteem | — | — | 0.93 | 0.71–1.22 | 0.90 | 0.69–1.18 |
| Close to parent respondent (vs not at all) | — | — | 0.36 | 0.07–1.70 | 0.44 | 0.10–1.99 |
| Older sibling smoker | — | — | — | — | 6.31*** | 2.39–16.66 |
Standard errors for significance tests and confidence intervals (CIs) are adjusted for clustering of siblings within parents. —, variable not included in model.
P < .05; ** P < .01; *** P < .001 (2-tailed t test).
Next, we examine multivariate logistic regression models predicting any smoking in the last year among the children, shown in Table 4. In Model 1, only parental smoking trajectories are included, with each category significantly more likely to have children smokers than the baseline stable nonsmoker trajectory. The odds ratios (ORs) are 3.2, 3.8, and 4.6 for the early-onset light smokers, early-onset heavy smokers, and late-onset smokers, respectively. When the parent-level and child-level controls are added in Model 2, the ORs only change slightly and remain statistically significant (P < .05). Younger children (P < .001) and those with higher GPA (P < .05) are less likely to have smoked in the last year.
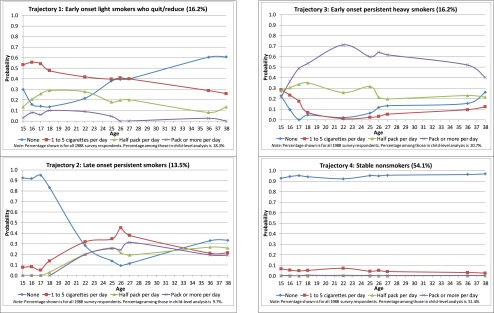
Model 3 adds the reported smoking from older siblings in the family, with such children having odds of smoking 6.3 times higher than those without an older sibling smoker. Although the other comparisons to stable nonsmokers are still significant, the comparison with early-onset persistent heavy smokers is reduced to non-significance. We depict this mediation graphically in Fig 2. The odds of an older sibling child reporting smoking are 15.4 times as high for parents who are early-onset persistent heavy smokers, relative to nonsmokers (P < .001), whereas this path is non-significant for the other parental trajectories. Instead, the significant effects for the other 2 parental trajectories operate through the direct effects of parental and sibling smoking. Thus, older sibling smoking appears to mediate some of the effect of parental consistent heavy smoking. In an alternate coding (not shown), we represented sibling smoking as 4 categories: older sibling smoker, older nonsmoking siblings, oldest sibling in family, and only child older than 11 years. With older nonsmoking siblings as the baseline, the comparison with oldest sibling in family (OR = 1.39, P = .57) and only child (OR = 1.24, P = .72) were very low in magnitude and non-significant, whereas the comparison with older sibling smoker was significant and similar in magnitude. Given that all the results hold and there is little magnitude difference in the 3 “no older sibling smoker” subcategories, we report the more parsimonious dichotomization.
FIGURE 2.
Mediation figure for the direct effect of parental smoking and indirect effect of parental smoking through older sibling smoking. ORs for the direct effects of parent smoking trajectories and older sibling smoking on adolescent smoking are from Table 4, Model 3. ORs for the indirect effects of parent smoking trajectories on older sibling smoking are adjusted for the child- and parent-level controls used in Table 4, Model 2. *p < .05, **p < .01, ***p < .001
Discussion
Using long-term multigenerational data, and latent class trajectory models capturing the duration and intensity of smoking behavior prospectively from adolescence (age 14 years) to adulthood (age 38 years), our results demonstrate that parental smoking trajectories significantly impact the smoking behavior of their children. Even after controlling for numerous potential child-, sibling-, and parent-level confounders, children of persistent smokers (whether early/late onset or heavy/light) have significantly higher odds of smoking in the past year than children of consistent nonsmokers. Even the children of “light” smokers who reduced or quit in later adulthood had 3.5 times higher odds than the trajectory of consistent nonsmokers. Our results show that parents who started smoking heavily in adolescence and remained a heavy smoker into adulthood were especially likely to have multiple children who smoked. In fact, older sibling cigarette use mediated the effect of parent use in heavy smoking households.
Although many studies have documented intergenerational influences on child smoking, our study extends this research in the following ways. First, we use 23 years of detailed prospective data to assess trajectories of smoking behavior from adolescence to adulthood. The smoking trajectories identified in our analyses are consistent with those found by other researchers using similar prospective datasets and methodologies, and further highlight the notion that parent smoking history matters.19 Second, we show that this intergenerational association is not fully explained by a variety of parent and child risk factors, particularly parent’s education and children’s achievement and adjustment. Third, consistent with recent research, we highlight the important role that older siblings play in the intergenerational transmission of smoking behaviors, especially for children who reside in households with long-term heavy smokers.34,35
We recognize limitations to the current study. The low percentage of parents with bachelor’s degrees (15%) is indicative of selection into relatively early parenthood; we only include those who select into parenthood by age 27 years, limiting our generalizability to such families. Thus, although implicated in past intergenerational smoking research,19 our non-significant education finding is likely because the sample overall has relatively low levels of education. Second, smoking information came from only 1 parent, which limits, among other possibilities, a detailed examination of parent and child gender (eg, father’s influence on sons, mother’s influence on daughters).44–46 Finally, we should interpret these nonexperimental results as associational, as parent-child smoking effects may be bidirectional.47
Conclusions
Consistent with previous research,5–20 parental smoking was strongly associated with adolescent smoking. Interestingly, children of both parents who were late-onset persistent smokers (ie, they had a low probability of smoking in their teenage years that increased in adulthood) or who had a history of light smoking in adolescence that declined in adulthood (ie, the early-onset light smokers who quit/reduced) had a significantly higher risk of smoking than children of parents who did not smoke in adolescence or adulthood. Although smoking as a teenager does not predetermine that one’s adolescent children will smoke,22–26 our longitudinal trajectories reveal that parental smoking at any age (even before the child is born) increases the chances that their children will smoke. Intervention efforts to heighten parental disapproval of smoking and weaken possible intergenerational influences45–50 should target parents who were smokers at any point from adolescence to adulthood. In addition to parents, the smoking behavior of older siblings should be targeted for prevention efforts.
Acknowledgments
We are grateful to Professor Jeylan Mortimer at the University of Minnesota for her role as the Principal Investigator of the Youth Development Study since its inception, her willingness for us to use the data, and her valuable feedback on this manuscript. We would also like to thank Brian Kelly for feedback and Jeanette Hussemann, Mayumi Uno, Chen-Yu Wu, and Frank Zhang for their role in data collection and preparation.
Glossary
- GPA
grade point average
- OR
odds ratio
- YDS
Youth Development Study
APPENDIX TABLE.
Probability of Missing by Original Youth Development Study Cohort Smoking Trajectories for Each Survey Year
| 1988 | 1989 | 1990 | 1991 | 1995 | 1998 | 1999 | 2000 | 2009 | 2011 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Trajectory 1: early-onset light smokers who quit/reduce | 0.022 | 0.053 | 0.028 | 0.062 | 0.223 | 0.153 | 0.192 | 0.171 | 0.261 | 0.278 |
| Trajectory 2: late-onset persistent smokers | 0.075 | 0.060 | 0.022 | 0.000 | 0.100 | 0.085 | 0.156 | 0.114 | 0.254 | 0.309 |
| Trajectory 3: early-onset persistent heavy smokers | 0.060 | 0.063 | 0.053 | 0.066 | 0.147 | 0.123 | 0.184 | 0.128 | 0.353 | 0.337 |
| Trajectory 4: stable-nonsmokers | 0.037 | 0.040 | 0.013 | 0.015 | 0.077 | 0.084 | 0.105 | 0.048 | 0.179 | 0.222 |
| Trajectory 5: high probability of attrition | 0.110 | 0.218 | 0.211 | 0.297 | 0.751 | 0.879 | 0.943 | 0.920 | 0.792 | 0.766 |
Footnotes
Dr Vuolo conducted the analyses, drafted the methods and results section, and approved the final manuscript as submitted; and Dr Staff drafted the abstract, introduction, and conclusion sections, and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This research was supported by grant HD44138 from the National Institute of Child Health and Human Development. It was previously supported by the National Institute of Mental Health (MH42843). Dr Staff is grateful for support from a Mentored Research Scientist Development Award in Population Research from the National Institute of Child Health and Human Development (HD054467). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2011. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2012 [Google Scholar]
- 2.U.S. Department of Health and Human Services How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010 [Google Scholar]
- 3.Chassin L, Hussong A, Beltran I. Adolescent substance use. In: Lerner RM, Steinberg L, eds. Handbook of Adolescent Psychology, 3rd ed. New York, NY: Wiley; 2009 [Google Scholar]
- 4.Hopfer CJ, Crowley TJ, Hewitt JK. Review of twin and adoption studies of adolescent substance use. J Am Acad Child Adolesc Psychiatry. 2003;42(6):710–719 [DOI] [PubMed] [Google Scholar]
- 5.Avenevoli S, Merikangas KR. Familial influences on adolescent smoking. Addiction. 2003;98(suppl 1):1–20 [DOI] [PubMed] [Google Scholar]
- 6.Bailey SL, Ennett ST, Ringwalt CL. Potential mediators, moderators, or independent effects in the relationship between parents’ former and current cigarette use and their children’s cigarette use. Addict Behav. 1993;18(6):601–621 [DOI] [PubMed] [Google Scholar]
- 7.Jackson C, Henriksen L. Do as I say: parent smoking, antismoking socialization, and smoking onset among children. Addict Behav. 1997;22(1):107–114 [DOI] [PubMed] [Google Scholar]
- 8.Tilson EC, McBride CM, Lipkus IM, Catalano RF. Testing the interaction between parent-child relationship factors and parent smoking to predict youth smoking. J Adolesc Health. 2004;35(3):182–189 [DOI] [PubMed] [Google Scholar]
- 9.Wilson DB, McClish DK, Heckman CJ, Obando CP, Dahman BA. Parental smoking, closeness to parents, and youth smoking. Am J Health Behav. 2007;31(3):261–271 [DOI] [PubMed] [Google Scholar]
- 10.Kelly AB, O’Flaherty M, Connor JP, et al. The influence of parents, siblings and peers on pre- and early-teen smoking: a multilevel model. Drug Alcohol Rev. 2011;30(4):381–387 [DOI] [PubMed] [Google Scholar]
- 11.Melotti R, Heron J, Hickman M, Macleod J, Araya R, Lewis G, ALSPAC Birth Cohort . Adolescent alcohol and tobacco use and early socioeconomic position: the ALSPAC birth cohort. Pediatrics. 2011;127(4). Available at: www.pediatrics.org/cgi/content/full/127/4/e948 [DOI] [PubMed] [Google Scholar]
- 12.Doherty WJ, Allen W. Family functioning and parental smoking as predictors of adolescent cigarettes use: a six-year prospective study. J Fam Psychol. 1994;8(3):347–353 [Google Scholar]
- 13.Li C, Pentz MA, Chou CP. Parental substance use as a modifier of adolescent substance use risk. Addiction. 2002;97(12):1537–1550 [DOI] [PubMed] [Google Scholar]
- 14.Harakeh Z, Scholte RHJ, Vermulst AA, de Vries H, Engels RC. Parental factors and adolescents’ smoking behavior: an extension of the theory of planned behavior. Prev Med. 2004;39(5):951–961 [DOI] [PubMed] [Google Scholar]
- 15.Otten R, Engels RCME, van de Ven MOM, Bricker JB. Parental smoking and adolescent smoking stages: the role of parents’ current and former smoking, and family structure. J Behav Med. 2007;30(2):143–154 [DOI] [PubMed] [Google Scholar]
- 16.Engels RCME, Knibbe RA, De Vries H, et al. Influences of parental and best friends’ smoking and drinking on adolescent use: a longitudinal study. J Appl Soc Psychol. 2006;29(2):337–361 [Google Scholar]
- 17.Hu MC, Davies M, Kandel DB. Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. Am J Public Health. 2006;96(2):299–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilman SE, Rende R, Boergers J, et al. Parental smoking and adolescent smoking initiation: an intergenerational perspective on tobacco control. Pediatrics. 2009;123(2). Available at: www.pediatrics.org/cgi/content/full/123/2/e274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chassin L, Presson C, Seo DC, et al. Multiple trajectories of cigarette smoking and the intergenerational transmission of smoking: a multigenerational, longitudinal study of a Midwestern community sample. Health Psychol. 2008;27(6):819–828 [DOI] [PubMed] [Google Scholar]
- 20.Melchior M, Chastang JF, Mackinnon D, Galéra C, Fombonne E. The intergenerational transmission of tobacco smoking—the role of parents’ long-term smoking trajectories. Drug Alcohol Depend. 2010;107(2-3):257–260 [DOI] [PubMed] [Google Scholar]
- 21.Weden MM, Miles JNV. Intergenerational relationships between the smoking patterns of a population-representative sample of US mothers and the smoking trajectories of their children. Am J Public Health. 2012;102(4):723–731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chassin L, Presson C, Rose J, Sherman SJ, Prost J. Parental smoking cessation and adolescent smoking. J Pediatr Psychol. 2002;27(6):485–496 [DOI] [PubMed] [Google Scholar]
- 23.Bricker JB, Leroux BG, Peterson AV, Jr, et al. Nine-year prospective relationship between parental smoking cessation and children’s daily smoking. Addiction. 2003;98(5):585–593 [DOI] [PubMed] [Google Scholar]
- 24.Bricker JB, Rajan KB, Andersen MR, Peterson AV, Jr. Does parental smoking cessation encourage their young adult children to quit smoking? A prospective study. Addiction. 2005;100(3):379–386 [DOI] [PubMed] [Google Scholar]
- 25.Bricker JB, Leroux BG, Robyn Andersen M, Rajan KB, Peterson AV, Jr. Parental smoking cessation and children’s smoking: mediation by antismoking actions. Nicotine Tob Res. 2005;7(4):501–509 [DOI] [PubMed] [Google Scholar]
- 26.Wyszynski CM, Bricker JB, Comstock BA. Parental smoking cessation and child daily smoking: A 9-year longitudinal study of mediation by child cognitions about smoking. Health Psychol. 2011;30(2):171–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Loughlin J, Karp I, Koulis T, Paradis G, Difranza J. Determinants of first puff and daily cigarette smoking in adolescents. Am J Epidemiol. 2009;170(5):585–597 [DOI] [PubMed] [Google Scholar]
- 28.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658 [DOI] [PubMed] [Google Scholar]
- 29.Ellickson PL, Orlando M, Tucker JS, Klein DJ. From adolescence to young adulthood: racial/ethnic disparities in smoking. Am J Public Health. 2004;94(2):293–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker TB, Brandon TH, Chassin L. Motivational influences on cigarette smoking. Annu Rev Psychol. 2004;55:463–491 [DOI] [PubMed] [Google Scholar]
- 31.Flay BR, Hu FB, Richardson J. Psychosocial predictors of different stages of cigarette smoking among high school students. Prev Med. 1998;27(5 Pt 3):A9–A18 [DOI] [PubMed] [Google Scholar]
- 32.Griffin KW, Botvin GJ, Doyle MM, Diaz T, Epstein JA. A six-year follow-up study of determinants of heavy cigarette smoking among high-school seniors. J Behav Med. 1999;22(3):271–284 [DOI] [PubMed] [Google Scholar]
- 33.Mayhew KP, Flay BR, Mott JA. Stages in the development of adolescent smoking. Drug Alcohol Depend. 2000;59(suppl 1):S61–S81 [DOI] [PubMed] [Google Scholar]
- 34.Slomkowski C, Rende R, Novak S, Lloyd-Richardson E, Niaura R. Sibling effects on smoking in adolescence: evidence for social influence from a genetically informative design. Addiction. 2005;100(4):430–438 [DOI] [PubMed] [Google Scholar]
- 35.Whiteman SD, Jensen AC, Maggs JL. Similarities in adolescent siblings’ substance use: testing competing pathways of influence. J Stud Alcohol Drugs. 2013;74(1):104–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mortimer JT. Working and Growing Up in America. Cambridge, MA: Harvard University Press; 2003 [Google Scholar]
- 37.Finch MD, Shanahan MJ, Mortimer JT, Ryu S. Work experience and control orientation in adolescence. Am Sociol Rev. 1991;56(5):597–611 [Google Scholar]
- 38.Hussemann JM, Mortimer JT, Zhang L. Exploring the correlates of parental consent for child survey participation: an intergenerational longitudinal study. Paper presented at: American Sociological Association Annual Meeting 2011; August 20, 2011; Las Vegas, NV. Available at: http://citation.allacademic.com/meta/p506110_index.html. Accessed May 3, 2013
- 39.Vermunt JK. Multilevel latent class models. Sociol Methodol. 2003;33(1):213–239 [Google Scholar]
- 40.Vermunt JK, Magidson J. Technical Guide for Latent GOLD 4.0: Basic and Advanced. Belmont, MA: Statistical Innovations; 2005 [Google Scholar]
- 41.Vuolo M, Staff J, Mortimer JT. Weathering the great recession: psychological and behavioral trajectories in the transition from school to work. Dev Psychol. 2012;48(6):1759–1773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.StataCorp Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011 [Google Scholar]
- 43.Hoechle D. Robust standard errors for panel regressions with cross-sectional dependence. Stata J. 2007;7(3):281–312 [Google Scholar]
- 44.Andrews JA, Hops H, Duncan SC. Adolescent modeling of parent substance use: the moderating effect of the relationship with the parent. J Fam Psychol. 1997;11(3):259–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ashley OS, Penne MA, Loomis KM, et al. Moderation of the association between parent and adolescent cigarette smoking by selected sociodemographic variables. Addict Behav. 2008;33(9):1227–1230 [DOI] [PubMed] [Google Scholar]
- 46.Sullivan KM, Bottorff J, Reid C. Does mother’s smoking influence girls’ smoking more than boys’ smoking? A 20-year review of the literature using a sex- and gender-based analysis. Subst Use Misuse. 2011;46(5):656–668 [DOI] [PubMed] [Google Scholar]
- 47.Schuck K, Otten R, Engels RCME, Barker ED, Kleinjan M. Bidirectional influences between parents and children in smoking behavior: a longitudinal full-family model. Nicotine Tob Res. 2013;15(1):44–51 [DOI] [PubMed] [Google Scholar]
- 48.Sargent JD, Dalton M. Does parental disapproval of smoking prevent adolescents from becoming established smokers? Pediatrics. 2001;108(6):1256–1262 [DOI] [PubMed] [Google Scholar]
- 49.Jackson CJ, Dickinson D. Enabling parents who smoke to prevent their children from initiating smoking: results from a 3-year intervention evaluation. Arch Pediatr Adolesc Med. 2006;160(1):56–62 [DOI] [PubMed] [Google Scholar]
- 50.Harakeh Z, Scholte RHJ, de Vries H, Engels RC. Parental rules and communication: their association with adolescent smoking. Addiction. 2005;100(6):862–870 [DOI] [PubMed] [Google Scholar]