Abstract
BACKGROUND AND OBJECTIVES:
Home visiting is 1 strategy to improve child health and parenting. Since implementation of home visiting trials 2 decades ago, US preterm births (<37 weeks) have risen by 20%. The objective of this study was to review evidence regarding home visiting and outcomes of preterm infants
METHODS:
Searches of Medline, Cumulative Index to Nursing and Allied Health Literature, Cochrane Database of Systematic Reviews, Cochrane Controlled Trial Register, PsycINFO, and Embase were conducted. Criteria for inclusion were (1) cohort or controlled trial designs; (2) home-based, preventive services for infants at medical or social risk; and (3) outcomes reported for infants born preterm or low birth weight (<2500 g). Data from eligible reports were abstracted by 2 reviewers. Random effects meta-analysis was used to synthesize data for developmental and parent interaction measures.
RESULTS:
Seventeen studies (15 controlled trials, 2 cohort studies) were reviewed. Five outcome domains were identified: infant development, parent-infant interaction, morbidity, abuse/neglect, and growth/nutrition. Six studies (n = 336) demonstrated a pooled standardized mean difference of 0.79 (95% confidence interval 0.57 to 1.02) in Home Observation for Measurement of the Environment Inventory scores at 1 year in the home-visited groups versus control. Evidence for other outcomes was limited. Methodological limitations were common.
CONCLUSIONS:
Reviewed studies suggest that home visiting for preterm infants promotes improved parent-infant interaction. Further study of interventions targeting preterm infants within existing programs may strengthen the impact and cost benefits of home visiting in at-risk populations.
Keywords: home visiting, preterm infants, parent-child relationship, development, low birth weight
Currently in the United States, 12% of all infants are born preterm, or before 37 weeks of gestation.1 Compared with full-term infants (≥37 weeks), these infants are more likely to be hospitalized, to have poorer health, and to have cognitive and developmental delays in the first year of life. Preterm infants from disadvantaged backgrounds may be especially vulnerable to such outcomes because of factors such as inadequate social support, financial strain, and poorer access to health care services.2
Home visiting is 1 strategy to improve a range of maternal-child health outcomes, including preterm birth, in high-risk populations. Currently, an estimated 400 publicly and privately funded home visiting programs provide services for at least 500 000 families in the United States,3 and an investment of federal funding in this intervention has been made through the Patient Protection and Affordable Care Act (PPACA) to expand and implement programs.4 Although some previous studies have shown promise for prenatal home visiting to improve birth weight or preterm birth,5,6 recent reviews of the published literature on this topic have demonstrated inconsistent results, likely in part because of limitations in study approaches, lack of a theoretical framework specific to pregnancy outcomes, and variation in content and delivery of interventions.7–9
One understudied aspect of home visiting is the impact for infants born preterm who are enrolled in programs based on social risk factors either prenatally or after birth. Previous reviews suggesting that home visiting for preterm infants may improve outcomes were published ∼20 years ago.10,11 Since that time, the preterm birth rate in the United States has risen by 20%. Recent literature on the epidemiology of preterm birth has also revealed the public health impact of late preterm birth, or delivery between 34 and 36 weeks’ gestation, which affects 70% of all infants born preterm.12,13 Given the investment in home visiting through the PPACA and an increased understanding of preterm birth in recent years, an updated review of the existing literature on this topic is warranted.
The goal of the current review was to systematically evaluate published studies of home visiting initiated in pregnancy or early infancy to promote prevention and health promotion, with a specific focus on their impact for infants born preterm. A comprehensive review of the existing evidence for this vulnerable population will be useful in understanding the complex home-visiting literature, and may help provide a target for future interventions within existing home-visiting programs. In this review we explore the following 3 questions:
What is the evidence that enrollment in home visiting prenatally or in early infancy improves outcomes for preterm infants?
Are there characteristics of program implementation that are associated with differences in the impact of home visiting on outcomes for preterm infants?
Are there additional social risk factors (ie, maternal age or low income status) that are associated with differences in the impact of home visiting for preterm infants?
Methods
Study Selection
We conducted a comprehensive literature search of studies of home-visiting programs initiated in pregnancy or early infancy, with a specific focus on studies including preterm and/or low birth weight (LBW) infants. The sample was limited to published studies of home-based, preventive, and health promotion services to families with infants at high medical or social risk for adverse child outcomes. Studies including both preterm and full-term infants were included only if intervention effects were reported separately for preterm infants. Studies of home-visiting programs involving the use of professionals, including nurses and social workers, as well as trained paraprofessionals, were included. We also included studies in which other interventions, such as center-based meetings, were provided as additional components to home visiting. Further inclusion criteria were experimental or quasi-experimental design, published in 1980 or later, conducted in the United States or Canada, home visits initiated in pregnancy or early infancy, and reported early childhood and/or parenting outcomes for infants born preterm and/or LBW. Studies that met some but not all inclusion criteria were excluded. Also excluded were single-group designs, interventions limited to a single home visit or the first week of life, and studies of children primarily with chronic conditions other than prematurity or LBW.
Data Sources
A comprehensive literature search was undertaken to identify literature from January 1980 through November 2012. The search strategy involved searching electronic databases, inspecting bibliographies of retrieved articles, and hand-searching the published literature. We searched the Medline, Cumulative Index to Nursing and Allied Health Literature, Cochrane Database of Systematic Reviews and Cochrane Controlled Trial Register, and PsycINFO databases. Additionally, Embase was searched via SciVerse Scopus.
The search was undertaken by using the following search terms: home visiting, home visitation, early intervention, at-risk, infant, neonate, neonatal, low birth weight, preterm, premature. Reference lists of published review articles and meta-analyses were used to identify additional studies. Care was taken not to overrepresent a single study associated with multiple published reports. We abstracted data from across multiple published reports, thus yielding the most complete description possible of that particular study.
Data Collection and Analysis
All potential reports were reviewed and data from eligible reports were abstracted separately by 2 reviewers. Discrepancies were resolved by consensus. Study quality was assessed using the Consolidated Standards of Reporting Trials guidelines for the controlled trials, and the Strengthening the Reporting of Observational studies in Epidemiology guidelines for the cohort studies. Both sets of guidelines are made up of checklists against which the quality of studies should be assessed.
Because the studies covered a wide range of outcomes and it was not possible to combine results into 1 summary statistic, a primarily narrative analysis of the data was conducted. However, random effects meta-analysis was used to synthesize data for separate outcome domains on clinical determination of sufficient similarity between subjects and outcomes of included studies.14 Statistical heterogeneity was determined using I2 tests. A standardized mean difference was calculated for continuous data measures. All data analyses were performed with a random-effects model using Comprehensive Meta-Analysis, Version 2 (Biostat Inc, Englewood, NJ).
Results
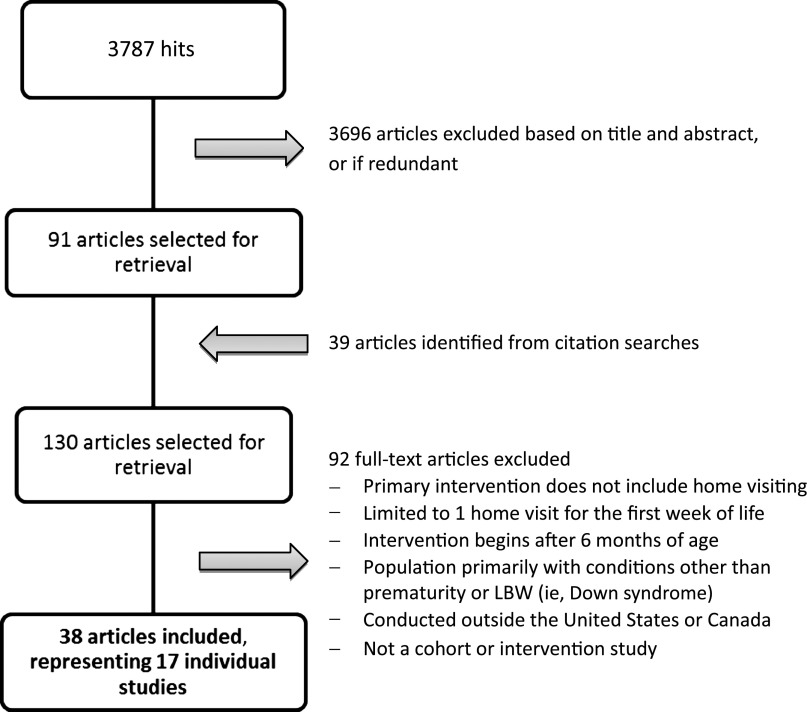
The search yielded 38 eligible publications, representing 17 individual studies evaluating a program of home visiting (see Fig 1). An additional 83 study reports were considered and excluded based on sampling criteria. The total of all samples in the included studies was 2983 infants, with a range of 45 to 985 and a median sample size of 100.
FIGURE 1.
Flow diagram showing selection of articles.
Program Descriptions
Table 1 describes each program with respect to targeted infant population, models of service delivery (when commenced and at what age concluded, number and length of home visits), home visitor background, and any additional program components.
TABLE 1.
Characteristics of Included Home-Visiting Programs
| Timing of Enrollment | Study Population | Additional Characteristics | Home Visitor | Frequency, Duration of Visits | Additional Interventions | Theory of Change | |
|---|---|---|---|---|---|---|---|
| Affleck et al45 (1989) | Before NICU discharge | NICU graduates, majority | none | Nurse | Weekly, 15 wk | — | Crisis theory associated with care of preterm infants |
| <36 wk and<1250 g | |||||||
| Barrera et al41,42 (1986) | 2 wk after discharge | Full-term and preterm infants | none | Infant development specialist | Weekly, first 3 mo | — | Transactional model focuses on parent-infant interactions |
| (<37 wk, <2000 g) | Biweekly, 6 mo | ||||||
| Monthly, until 1 y | |||||||
| Beckwith40 (1988) | Before NICU discharge | NICU graduates, <35 wk and <2000 g | Low socioeconomic status | RN or infant development specialist | Frequency not described, 12 mo | — | No specific theory reported |
| Brooten and colleages15,16 (1986, 1993) | Before NICU discharge | NICU graduates <1500 g | none | Nurse | Visits during first week home, then at 1, 9, 12, and 18 mo | Hospital-based intervention with parents during NICU stay. Weekly telephone contact for 2 mo after discharge. | No specific theory reported |
| Casiro et al27 (1993) | Before NICU discharge | NICU graduates <2000 g | none | Nurse | Individually determined over 8 wk, range 2–7 visits | Included trained homemakers to assist with childcare and housekeeping. | No specific theory reported |
| Field et al38,39 (1980, 1982) | After discharge | Full-term and preterm infants <37 wk, <2500 g | Teen moms, African American, low socioeconomic status | Graduate student with a teenaged work/study student. | Biweekly, first 4 mo Monthly, until 12 mo | — | Interaction effect of prematurity and maternal attributes |
| Finello et al46,47 (1998) | 1 wk after discharge | NICU graduates 750–1500 g | none | Not described | Frequency not described, over 2 y | Some also received home health nursing, providing critical care at home for first 1 to 4 wk. | No specific theory reported |
| Furuno et al35,37 (1985, 1986) | Before NICU discharge | NICU graduates <1500 g or <2000 g requiring mechanical ventilation | none | Nurse | Biweekly, 9 mo | Hospital-based intervention with parents during NICU stay. | Motor and sensory deficit model for preterm infants |
| Infant Health and Development Program17–24 (1990, 1992, 1994, 1995, 1997, 2003, 2009) | After discharge | Preterm infants <37 wk and <2500 g | none | Paraprofessional | Weekly, first year Biweekly, until 3 y | Center-based and group interventions after 1 y | Transactional model focuses on parent-infant interactions |
| Kang et al53 (1995) | Before NICU discharge | NICU graduates <36 wk | none | Nurse | 9 visits over 5 mo | Hospital-based intervention with parents during NICU stay. | Transactional model focuses on parent-infant interactions |
| Mother Infant Communication Project25,26 (1987, 1993) | After discharge | NICU graduates with LBW, prematurity, and other complications | Additional social risks (teen mom, child protective services, substance use, low income, child protective services) | Infant development specialist | Weekly then spaced to monthly for first year, then quarterly until 2 y | Some also participated in center-based groups and/or smaller local groups | Responsivity to infant cues important to development |
| Mother Infant Transaction Project34,36,43,44 (1984, 1988, 1990, 1993) | Before NICU discharge | NICU graduates <2250 g and <37 wk | none | Nurse | 4 visits: 3, 14, 30, and 90 d after discharge | Hospital-based intervention with parents and infant during NICU stay. | Transactional model focuses on parent-infant interactions |
| Neu and Robinson54 (2010) | Before NICU discharge | NICU graduates 32–34 wk | none | Nurse | Weekly, 8 wk | Some parents received part of intervention during NICU stay. | Coregulation |
| Resnick et al31–33 (1987, 1988) | Before NICU discharge | NICU graduates 500–1800 g | none | Infant development specialist | Biweekly, 2 y | Hospital-based intervention with parents during NICU stay. | No specific theory reported |
| Ross30 (1984) | After discharge | NICU graduates with LBW, prematurity, and other complications | Low socioeconomic status | Team of RN, occupational therapist | Biweekly, first 3 mo, then monthly up to 1 y | — | No specific theory reported |
| Teti et al29 (2009) | Before NICU discharge | NICU graduates <2500 g or <37 wk | African American | Master’s or doctoral student | 8 sessions over 20 wk | Hospital-based intervention with parents during NICU stay. Also infant massage therapy after discharge. | Transactional model focuses on parent-infant interactions |
| Zahr28 (2000) | Before NICU discharge | NICU graduates 800–2000 g | Hispanic, low socioeconomic status | Nurse | Two arms: “short” = 11 visits in 4 mo, “extended” = 19 visits in 12 mo | — | Transactional model focuses on parent-infant interactions |
RN, registered nurse.
Infant Population
All of the included programs enrolled infants either during birth hospitalization or soon after discharge. None of the studies meeting eligibility criteria for this review included participants enrolled prenatally in home visiting. Although 13 programs used specific enrollment criteria based either on gestational age, birth weight, or both, 4 programs instead targeted a more general population of infants requiring care in the NICU, most of whom were preterm and/or LBW.
Although most programs defined preterm as <37 weeks’ gestation, there was some variability; 2 programs defined preterm as <36 weeks’ gestation, 1 defined preterm as <35 weeks’ gestation, and 1 program included only infants at <34 weeks’ gestation. As seen in Table 1, 6 programs identified their study population primarily by birth weight instead of gestational age, with cutoff values for inclusion ranging from 1500 g to 2000 g. The targeted preterm infant populations varied in terms of severity of prematurity and LBW status, resulting in ranges in mean gestational age of 30 to 35 weeks, and mean birth weight of 1200 to 2400 g, across studies.
Intervention Details
Programs varied with respect to home visitor training background. Eight of the 17 programs used nurses, 3 used development specialists, 3 used trained paraprofessionals or graduate students, 2 used a mix of provider types, and 1 did not specify. Duration of home visiting ranged from 8 weeks to 3 years. As seen in Table 1, visit frequency also varied; whereas many programs provided visits weekly or biweekly early in infancy, some studies reported lower visit frequencies; for example, Brooten and colleagues, who reported visits through the first week home, then at 1, 9, 12, and 18 months.15,16 Seven studies implemented an additional intervention component during birth hospitalization, before the discharge home, focusing on parenting or infant development. In 2 programs, the Infant Health and Development Program (IHDP)17–24 and the Mother Infant Communication Project,25,26 the intervention also included attendance at center-based groups.
Reported Outcomes
We identified 5 general domains of outcomes: infant development, morbidity and health care utilization, abuse and neglect, parent-infant interaction, and growth and nutrition (see Table 2). Most reviewed studies, 13 of 17, assessed outcomes in more than 1 domain. The most common outcomes reported were in the domains of infant development (13 studies) and parent-infant interaction (14 studies). Child abuse/neglect was the least-reported outcome domain, with only 2 reviewed studies providing data.
TABLE 2.
Summary of Outcome Domains for Included Studies
| Age Assessed | Outcome Measure | Results | |
|---|---|---|---|
| Infant development | |||
| Barrera et al41,42 (1986) | 4, 8, 12, and 16 mo corrected age; | Cognitive and motor development (Bayley MDI and PDI; McCarthy Scales of Children's Abilities; MCDI; PIAT; VMI) | Little or no intervention effects on Bayley scores after 4 or 8 mo, but significant intervention effects at 12 mo (P < .05). |
| No significant intervention effect on temperament. | |||
| At 4.5 y, no significant treatment effects on PIAT or McCarthy scores. | |||
| 4.5 y of age | Infant temperament (Infant and Toddler Temperament Questionnaires) | At 4.5 y, significant treatment effect on VMI and MCDI, but only for infants with weight <1500 g. | |
| Beckwith40 (1988) | 13, 20 mo | Cognitive development (Bayley MDI) | No intervention effects on the Bayley scores at 13 mo, but significant intervention effects at 20 mo (P < .05). |
| Infant Health and Development Program17–24 (1990, 1992, 1994, 1995, 1997, 2003, 2009) | 2, 3, 5, 8, and 18 y | Cognitive development (Stanford-Binet Intelligence Scale, Wechsler Intelligence Scale for Children), Behavior problems (Child Behavior Checklist) | At 2 and 3 y, significant maternal education interaction effect, with higher Stanford-Binet scores for subgroups with high school education or less (P ≤ .001). At 3 y, significant intervention effect on Child Behavior Scores (P < .01). At 3, 5, and 8 y, significant birth weight interaction effect, with infants < 1500 g less influenced by intervention that infants 1500-2500 g. |
| Brooten and colleagues15,16(1986, 1993) | 18 mo | Cognitive and motor development (Bayley MDI and PDI) | No significant intervention effects on Bayley scores. |
| Casiro et al27 (1993) | 1 y corrected age | Cognitive and motor development (Bayley MDI and PDI) | No significant intervention effects on Bayley scores. |
| Field et al38,39 (1980, 1982) | 4, 8, and 12 mo postdischarge | Cognitive and motor development (Denver Developmental Screening Test; Bayley MDI and PDI), Infant temperament (Carey Infant Temperament Questionnaire) | Significant intervention effects at 4, 8, and 12 mo for infant temperament and cognitive development (P < .01). |
| Mother Infant Communication Project25,26(1987, 1993) | 18 mo | Language development (REEL) | Significant intervention effect for the expressive quotient on the REEL (P < .05); no significant intervention effect for receptive quotient. |
| Furuno et al35,37 (1985, 1986) | 3, 9 mo | Cognitive and motor development (Bayley MDI and PDI; Gesell Developmental Schedules) | No intervention effect on Gesell scores at 3 and 9 mo. At 9 mo, significant intervention effect on Bayley scores (P = .05), expressive and combined language quotients on REEL (P = .01). |
| Language development (REEL) | |||
| Mother Infant Transaction Project34,36,43,44 (1984, 1988, 1990, 1993) | 6, 12, 24, 36, 48 mo; 7, 9 y | Cognitive development (Bayley MDI; McCarthy Scales of Children's Abilities; Kaufman Assessment Battery for Children; PPVT) | At 6 mo, significant intervention effect on infant temperament (P < .01). |
| Infant temperament (Carey Infant Temperament Questionnaire) | No significant intervention effect on cognitive development measures at 6, 12, or 24 mo, but significant effect on McCarthy Scales at 3 y (P < .05) and 4 y (P < .01). Intervention effect persisted using Kaufman Assessment at 7 and 9 y (P < .01). | ||
| Resnick et al31–33 (1984, 1988, 1990, 1993) | 1, 2 y | Cognitive and motor development (Bayley MDI and PDI) | Significant intervention effect on percent with developmental delay at 1 and 2 y (P < .05). Also a significant intervention effect on Bayley scores at 1 and 2 y (P < .05). |
| Ross30 (1984) | 1 y | Cognitive and motor development (Bayley MDI and PDI; Amiel-Tison Neurologic Examination) | Significant intervention effects on Bayley Mental Scales (P < .001) but not on Bayley Motor Scales or Amiel-Tison examination. |
| Teti et al29 (2009) | 3–4 mo | Cognitive and motor development (Bayley MDI and PDI) | Significant birth weight interaction, with intervention effects only for infants <1000 g (P < .05), not for infants 1000–2500 g. |
| Zahr28 (2000) | 1, 4, 8, 12, 18, and 24 mo | Cognitive and motor development (Bayley MDI and PDI) | No consistent intervention effect. |
| Morbidity/Health care utilization | |||
| Infant Health and Development Program17–24(1990, 1992, 1994, 1995, 1997, 2003, 2009) | 3, 5, and 8 y | Morbidity Index (maternal report of hospitalizations, surgeries, injuries, and conditions) | At 3 y, a small, statistically significant increase in maternally reported minor illnesses for the infants < 1500 g only, with no intervention effect on serious health conditions. At 8 y, intervention groups received lower ratings on the Physical Functioning Scale. |
| Child health status (General Health Ratings Index) | |||
| Functional status (Functional Status Scale) | |||
| Brooten and colleagues15,16 (1986, 1993) | 18 mo | Rehospitalization and acute care visits | No significant intervention effects. |
| Casiro et al27 (1993) | 1 y | Rehospitalization and acute care visits | No significant intervention effects. |
| Finello et al46,47 (1998) | 6, 12 mo | Rehospitalization and emergency department visits, immunization status | At 6 mo, no intervention effects on ER visits or immunization status, but significant decrease in rehospitalization. At 12 mo, no effect on rehospitalization, but significant intervention on ER use and immunization status. |
| Abuse and neglect | |||
| Brooten and colleagues15,16(1986, 1993) | 18 mo | Reported abuse | No significant intervention effects. |
| Finello et al46,47 (1998) | 6, 12 mo | Reported abuse and neglect | No significant intervention effects. |
| Parent-infant interaction | |||
| Affleck et al45 (1989) | 6 mo | Maternal mood (Profile of Mood States) | No main intervention effects, but significant interaction effect with infant medical severity. |
| Maternal competence (Parenting Stress Index) | On maternal mood (P < .05). | ||
| Maternal perception of infant temperament (Infant Characteristics Questionnaire) | Significant interaction between treatment condition and maternal need for support on maternal sense of competence, maternal responsiveness, and perceived maternal control (P < .01). | ||
| Attachment, perceived maternal responsiveness (Attachment subscale of Parenting Stress Index and HOME Inventory) | No intervention effect on attachment or perception of temperament. | ||
| Maternal perceptions of control | |||
| Barrera et al41,42 (1986) | 4, 8, 12, and 16 mo | Parenting behavior and environment (HOME Inventory) | No significant intervention effect on HOME scores at 4 mo, but significant intervention effect by 16 mo (P < .05). At 4.5 y, significant intervention effect on HOME scores (P < .05). |
| 4.5 y | Maternal-infant interaction (coding of observed behavior) | ||
| Beckwith40 (1988) | 9, 13 mo | Maternal-infant interaction (coding of observed behavior), Maternal emotional stability | At 9 mo, significant intervention effect on observed level of reciprocal interactions. At 13 mo, significant intervention effect on emotional stability and realistic expectations of development, but no significant effect on attachment security. |
| Expectations of development | |||
| Attachment security | |||
| Casiro et al27 (1993) | 1 y | Parenting behavior and environment (HOME Inventory) | Significant intervention effects on total HOME score (P = .01). |
| Field et al38,39 (1980, 1982) | 4, 8, 12 mo | Maternal-infant interaction (coding of videotaped observed behavior) | At 4 mo, no intervention effect on feeding-interaction ratings, but significant effect on face-to-face interaction ratings (P < .01). At 8 mo, significant intervention effect on HOME scores (P < .01). At 12 mo, significant intervention effects on observed maternal-infant interaction (P < .01). |
| Parenting behavior and environment (HOME Inventory) | |||
| Finello et al46,47 (1998) | 6, 12 mo | Parenting behavior and environment (HOME Inventory; FACES) | At 6 and 12 mo, significant intervention effects on total HOME score (P < .05). No intervention effect on FACES score, parenting satisfaction, or maternal depression. |
| Satisfaction with parenting | |||
| Maternal depression (CES-D Scale) | |||
| Mother Infant Communication Project25,26 (1987, 1993) | 6, 12, and 18 mo | Parenting behavior and environment (HOME Inventory) | No significant intervention effects on HOME score at 6 or 12 mo, but significant effect at 18 mo (P < .01). |
| Furuno et al35,37 (1985, 1986) | 9 mo | Maternal-infant interaction (NCAFS and NCATS) | Significant intervention effect on NCAFS (P < .05), but not NCATS. |
| Kang et al53 (1995) | 1.5 and 5 mo corrected age | Maternal-infant interaction (NCAFS at 1.5 mo, NCATS at 5 mo) | At 1.5 mo, significant intervention effect on total NCAFS score (P < .05). |
| At 5 mo, significant intervention effect on total NCATS score (P < .05). | |||
| Neu and Robinson54 (2010) | 6 mo | Maternal-infant interaction (Still-Face Paradigm, Infant Regulatory Scoring System) | Significant intervention effect of kangaroo holding compared with control group (P < .05), but no intervention effect for treatment group with traditional blanket holding. No significant intervention effect on infant behavior. |
| Mother Infant Transaction Project34,36,43,44 (1984, 1988, 1990, 1993) | 4 mo | Maternal anxiety (Taylor Manifest Anxiety Scale) | At 4 mo, no intervention effect on maternal anxiety. At 6 mo, significant intervention effect on maternal confidence p < 0.01) and satisfaction (P < .05) but not on maternal attitude. |
| 6 mo | Maternal confidence, satisfaction, and perception of infant temperament (Seashore Self-Confidence Rating Paired Comparison Questionnaire; Satisfaction Scale) | ||
| Ross30 (1984) | 1 y | Parenting behavior and environment (HOME Inventory) | Significant intervention effects on HOME score (P < .001). No effect on maternal attitudes section of the MDECAS or maternal rating of infant temperament. |
| Maternal attitude (MDECAS) | No control for multiple comparisons or covariates. | ||
| Maternal perception of infant temperament (Toddler Temperament Scale) | |||
| Teti et al29 (2009) | 3–4 mo | Maternal self-efficacy (Maternal Self-Efficacy Scale) | Significant intervention effect on maternal self-efficacy (P < .05) but not on maternal sensitivity. |
| Maternal sensitivity (Maternal Behavioral Q-Set) | |||
| Zahr28 (2000) | 1, 4, 8, 12, 18, and 24 mo | Maternal Confidence (Maternal Confidence Questionnaire, Parenting Stress Index) | No consistent intervention effect on maternal confidence or parenting stress. Control group had significantly improved HOME scores, NCAFS and NCATS scores compared with intervention groups at multiple time periods (P < .001). |
| Maternal-infant interaction (NCAFS and NCATS) | |||
| Parenting behavior and environment (HOME Inventory) | |||
| Nutrition and growth | |||
| Infant Health and Development Program17–24 (1990, 1992, 1994, 1995, 1997, 2003, 2009) | 3, 5, and 8 y | Weight, height, head circumference | No significant intervention effect on growth outcomes at 3 y. At 8 y, infants < 1500 g were heaver (P = .02), taller (P = .05), and had larger head circumference (P = .001), compared with controls. |
| Brooten and colleagues15,16 (1986, 1993) | 18 mo | Failure to thrive | No significant intervention effects. |
| Casiro et al27 (1993) | 1 y | Weight, height, head circumference | No significant intervention effects. |
| Field et al38,39 (1980, 1982) | 4, 12 mo | Weight, height, head circumference | At 4 and 12 mo, significant intervention effects on weight and length, but not head circumference (P < .01). |
| Teti et al29 (2009) | 3–4 mo | Weight, height, head circumference | No significant intervention effects. |
Bayley PDI, Bayley Psychomotor Scales of Infant Development; CES-D, Center for Epidemiologic Studies Depression Scale; MCDI, Minnesota Child Development Inventory; PIAT, Peabody Individual Achievement Test; PPVT, Peabody Picture Vocabulary Test; REEL, Receptive Expressive Emergent Language Scale; VMI, Visual Motor Integration.
Infant Development
The 13 studies assessing infant development provide a wide range of effect sizes and study follow-up periods. Although most studies observed a significant difference between intervention and control groups on at least 1 developmental outcome measure, 3 studies (Brooten and colleagues,15,16 Casiro et al,27 and Zahr28) observed no significant differences at any of the assessment periods (18 months, 12 months, and throughout 24 months, respectively).
As shown in Table 2, multiple studies assessed infant development using the Bayley Mental Developmental Index (Bayley MDI). We therefore conducted a meta-analysis of effect sizes for Bayley MDI scores using studies with infant assessment data at or near 1 year of age. Although a total of 11 studies provided Bayley MDI data, 2 studies, Teti et al29 and Brooten and colleagues,15,16 were empirically omitted from the meta-analysis because of disparate follow-up ages (3–4 months and 18 months, respectively). The remaining 9 pooled studies27,28,30–44 (n = 516) demonstrate a statistically significant overall effect on the standardized mean difference (SMD) in Bayley MDI scores in the home-visited group versus the control group, with a pooled SMD of 0.50 (95% confidence interval [CI], 0.18 to 0.83) (Fig 2, Panel A). However, significant statistical heterogeneity was noted between the studies (I2 = 67.8%, P = .002). On further review of potential causes for study heterogeneity, we observed that when the 5 programs reporting weekly or biweekly initial visits were analyzed separately,30–33,35,37–39,41,42 the pooled SMD was 0.90 (95% CI 0.60 to 1.19) and there was no longer significant statistical heterogeneity (I2 = 8.8%, P = .36). In contrast, the remaining 4 programs with initial visit frequency that was not well defined or less than biweekly27,28,34,36,40,43,44 had a pooled SMD of 0.12 (95% CI –0.12 to 0.35) when analyzed separately, again with no statistical heterogeneity (I2 = 0.0%, P = .66).
FIGURE 2.
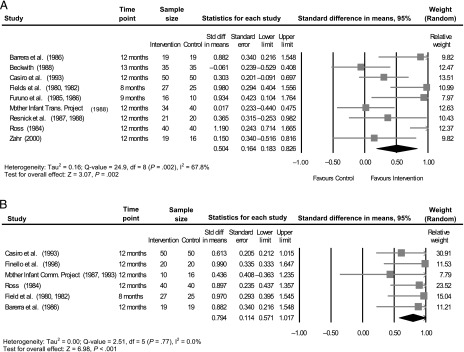
Meta-analysis of effects of home-visiting intervention on Bayley MDI scores and HOME Inventory scores at ∼1 year of age. A, Pooled effect on Bayley MDI scores. B, Pooled effect on HOME Inventory scores.
Parent-Infant Interaction
Outcomes in the domain of parent-infant interaction were reported in 14 of the 17 included studies. Of these, only 1 demonstrated an absence of positive intervention effect on any parent-infant interaction measures.28 As shown in Table 2, a range of these measures was used to assess parent-infant interaction across studies, including such diverse tools as the Maternal Developmental Expectations and Child-rearing Attitudes Survey (MDECAS), the Nursing Child Assessment Feeding Scales and Nursing Child Assessment Teaching Scales (NCAFS and NCATS), and the Family Adaptability and Cohesion Evaluation Scales (FACES).
Because 8 studies provided either a total score or subscale score for the Home Observation for Measurement of the Environment (HOME) Inventory, we conducted a meta-analysis of effect sizes for HOME Inventory scores using studies with data at or near 1 year of age. Of these, 2 studies, Affleck et al45 and Zahr28 were empirically omitted from the meta-analysis because of disparate follow-up ages (6 months and 18 months, respectively).The remaining 6 pooled studies25–27,30,38,39,41,42,46,47 (n = 336) demonstrate a statistically significant overall effect on the HOME Inventory scores in the home-visited group versus the control group, with a pooled SMD of 0.79 (95% CI 0.57–1.02) (Fig 2, Panel B). Given the lack of significant statistical heterogeneity between studies (I2 = 0.0%, P = .77), we also repeated this analysis using a fixed effects model, and results were identical.
Morbidity and Health Service Utilization
Four studies assessed the effect of home visiting on a range of morbidity and health service utilization outcomes. Finello et al46,47 found a significant decrease in the incidence of hospitalization among intervention infants at 6 months but not 12 months. Results of the IHDP demonstrated a small, statistically significant increase in maternally reported minor illnesses at 3 years of age, but only for infants weighing <1500 g, and no effect on serious health conditions.17–24 Neither Casiro et al nor Brooten and colleagues demonstrated significant intervention effects on rates of hospitalization or acute care visits.15,16,27
Nutrition and Growth
Five studies used anthropometric measures to assess physical growth, with follow-up periods ranging from 3 months to 8 years across studies. Only Field et al38,39 demonstrated a significant intervention effect on weight and length during infancy (at 4 and 12 months). Data from the IHDP at 8 years did demonstrate that intervention infants had higher weights, heights, and head circumferences compared with control infants, but only among those weighing <1500 g at birth.19
Child Abuse/Neglect
Brooten and colleagues15,16 and Finello et al46,47 measured the incidence of reported child abuse among study infants; neither observed a significant difference between intervention and control groups.
Program Design and Theory of Change
Program Intensity
As shown in Table 3, most studies did not provide information on whether participants received the full prescribed number of home visits. Only 1 study (Zahr28) evaluated a dosage effect of the intervention on observed outcomes (based on duration on home visiting received by the intervention group); no outcome difference was detected between 2 intervention arms with differing durations, 4 months and 12 months. Among 10 studies that demonstrated a significant intervention effect on developmental outcomes, duration of home visiting ranged from 3 months to 3 years. The Mother-Infant Transaction Program study in particular demonstrated sustained differences in developmental outcomes after 3 years, despite a home-visiting intervention limited to 4 visits over the first 90 days after NICU discharge.34,36,43,44 Of note, however, the Mother-Infant Transaction Program also used a hospital-based component for intervention infants and their families during NICU hospitalization.
TABLE 3.
Methodologic Descriptions of Included Studies
| Size | Study Design | Comparison Groups | Sample Size Calculation | Blinding of Observers | Participants Received Full Intervention? | Significant Differences at Baseline? | Loss to Follow-up | |
|---|---|---|---|---|---|---|---|---|
| Affleck et al45 (1989) | n = 100 | RCT | Home visiting vs non–home visiting | Not provided | Yes | Not provided | No | 6% attrition at 6 mo, no other information provided |
| Barrera et al41,42 (1986) | n = 83 | RCT, block randomization by infant and maternal characteristics | 2 home-visiting groups vs non–home visiting | Not provided | Yes | Not all families received all visits prescribed. | Not applicable | 19% attrition at 4.5 y, no other information provided |
| Beckwith40 (1988) | n = 92 | RCT | Home visiting vs non–home visiting | Not provided | Yes | Not provided | No | 36% attrition in control group, 5% in intervention group |
| Brooten and colleagues15,16 (1986, 1993) | n = 79 | RCT | Early discharge + home visiting versus standard care | Not provided | No | Not provided | No | 15% attrition at 18 mo, equal in both groups |
| Casiro et al27 (1993) | n = 100 | RCT, block randomization by birth wt | Early discharge + home visiting versus standard care | 85% power (P = .05, 1-tailed) | Yes | Variable treatment dose (no set number of visits prescribed) | Significantly more married mothers in intervention group | 8% attrition at 1 y, no other information provided |
| Field et al38,39 (1980, 1982) | n = 60 | RCT, block randomization by preterm status and maternal age | Home visiting vs non–home visiting in teen mom/preterm infant arm | Not provided | Yes | Not provided | No | 38% attrition at 12 mo, equivalent in both groups |
| Finello et al46,47 (1998) | n = 81 | RCT | Home visiting vs home health vs combined versus no intervention | Not provided | Not provided | Not provided | Significant group differences in infant complications | 10% attrition in control group vs 25% in home visiting group at 12 mo |
| Furuno et al35,37 (1985, 1986) | n = 100 | RCT | 2 home-visiting groups vs non–home visiting | Not provided | No | Not provided | No | 42% attrition at 9 mo, equivalent across groups |
| Infant Health and Development Program17–24 (1990, 1992, 1994, 1995, 1997, 2003, 2009) | n = 985 | RCT, block randomization by birth wt | Home visiting vs non–home visiting | 99% power (P = .05, 2-tailed) | Yes | Not provided | No | 7% attrition at 36 mo, equal in both groups |
| Kang et al53 (1995) | n = 327 | RCT, block randomization by maternal education status | Home visiting versus standard public health nursing | Not provided | Yes | Not provided | No | 24% attrition at 5 mo, equivalent across groups |
| Mother Infant Communication Project25,26 (1987, 1993) | n = 45 | Quasi-experimental design | 2 home-visiting intervention groups versus home-visiting control group | Not provided | No | Not provided | No | 29% attrition rate for intervention participants by 2 y |
| Mother Infant Transaction Project34,36,43,44 (1984, 1988, 1990, 1993) | n = 119 | RCT | Home visiting vs non–home visiting versus full-term control group | Not provided | Yes | Not provided | Higher maternal education and socioeconomic status in intervention group | 12% attrition in intervention group by 6 mo, none in control groups; by 48 mo, 32% attrition rate, similar across groups |
| Neu and Robinson54 (2010) | n = 87 | RCT | 2 home-visiting intervention groups (kangaroo vs blanket holding) vs home-visiting control group | <80% power (P = .05) | No | 82% and 87% of intervention groups received 8 visits | Higher depression scores in kangaroo intervention group | 18% attrition rate, equivalent across groups |
| Resnick et al31–33 (1984, 1988, 1990, 1993) | n = 221 | RCT | Home visiting vs non–home visiting | Not provided | Yes | Not provided | No | 76% attrition at 2 y, equivalent in both groups. |
| Ross30 (1984) | n = 84 | Matched cohort study | Home visiting vs non–home visiting | Not provided | Yes, but not for all measures | Not provided | Not applicable | 10% attrition in intervention group at 1 y, none in control |
| Teti et al29 (2009) | n = 173 | RCT, urn randomization to achieve balance on infant and maternal characteristics | Home-visiting intervention group vs home-visiting control group | 80% power (P < .05) | Yes | Variable delivery of massage component of intervention, otherwise not described | No | 21% attrition, equivalent in both groups |
| Zahr28(2000) | n = 123 | Pseudo-randomized trial: intervention group randomized into 2 study arms, but control group not randomized | 2 home-visiting groups vs standard public health nursing | <80% power (P < .05) | Yes | Not provided | No | 63% attrition in control group vs 42% and 48% in the intervention groups |
RCT, randomized controlled trial.
Additional Population Targets
Six studies25,26,28–30,38–40 targeted families of preterm infants with additional demographic characteristics, such as race or socioeconomic status. The study by Field et al38,39 was the only one included in this review to focus specifically on teenage mothers of preterm infants, reporting significant intervention effects in the outcome domains of infant development, parent-infant interactions, and nutrition and growth. Although the IHDP did not specifically target subpopulations of infants based on demographic characteristics, results of their analysis did demonstrate a significant interaction effect of maternal education, such that only the intervention subgroup with a high school education or less showed significant developmental differences at 2 and 3 years of age.17–24
Three studies described a significant interaction effect between birth weight and the home-visiting intervention, although the direction of this influence was not consistent between studies. Teti et al29 observed a significant difference between intervention and control groups when assessed at 3 to 4 months of age, but only among infants weighing <1000 g. Barrera et al41,42 also described significant differences in developmental outcomes at 4.5 years for infants weighing <1500 g but not for heavier infants. These results contrast with findings from the IHDP, in which significant cognitive differences were observed at 5 and 8 years of life among infants 1500 to 2500 g but not those weighing <1500 g at birth.17–24
Theory of Change
As seen in Table 1, 8 of the 13 studies measuring developmental outcomes described an explicit theory of change to support program development and key hypotheses, most of which demonstrated a significant intervention effect on at least 1 developmental outcome measure. Most commonly, studies cited a “transactional model,” focusing on the interaction between infants and parents as the primary target of intervention.
Study Quality
As seen in Table 3, 3 studies used nonrandom comparison groups; the remainder were randomized controlled trials. Most included studies compared an intervention including home visiting with a control population receiving no home visiting. However, control groups in 3 studies also received home visiting, whereas the intervention groups were given an enhanced or modified model of home visiting. Five of the 17 studies provided a calculation of statistical power, and 12 studies reported blinding observers to treatment group. Most studies demonstrated no significant differences in maternal or infant characteristics at baseline.
Overall, loss to follow-up was the weakest aspect of most studies, particularly those using a longer follow-up period, as this reduced sample size available for assessment of outcomes. Four studies did not report effect of group assignment on attrition, whereas 9 studies reported similar or equal loss to follow-up between groups, and 4 studies reported differential loss to follow-up based on group assignment.
Discussion
We identified 17 individual studies published in the literature since 1980 that evaluate the effectiveness of home visiting for preterm infants and their parents. As with much of the literature on home visiting, the reviewed studies vary in terms of design and implementation of the intervention, outcomes evaluated, and specific study population. Our pooled analysis of HOME Inventory scores supports a positive effect of home visiting on parenting outcomes for infants born preterm and/or LBW. Pooled analysis of Bayley MDI scores at 1 year demonstrates a statistically significant overall effect but with heterogeneity between programs potentially related to visit frequency. We found limited studies to support whether home visiting among this population reduces hospitalization or morbidity. We also found limited studies to support whether home visiting among preterm and/or LBW infants improves physical growth in infancy.
Only 2 reviewed studies measured child abuse as an outcome, and results are not sufficient to either support or refute the effect of home visiting in a preterm population. However, additional work by Bugental and Schwartz,48 not included in this review because of inclusion of a more heterogeneous, older infant sample, demonstrates the benefits of a home-visiting curriculum tailored to medically at-risk infants to prevent harsh parenting tactics. Further intervention research targeting a more specific population of preterm infants may be important, particularly given what is known about their increased risk of child abuse and neglect.49
Several reviewed studies used a well-defined theory of change to guide program implementation and demonstrated a positive intervention effect on developmental outcomes. Additionally, results of several studies suggested that additional characteristics, including birth weight and social risk factors, may moderate the impact of home visiting on developmental outcomes. This is consistent with recent literature on home visiting promoting the importance of aligning theory, implementation, target population, and outcomes.50 One notable exception to this pattern is the study by Zahr,28 which describes a population of low-income Hispanic families and their LBW infants. Despite a well-defined conceptual model and targeted population, no measurable intervention effects were observed. Although the lack of significantly positive findings may have resulted from methodological limitations, including a high sample attrition rate, the authors suggest that specific cultural factors may have contributed to a lack of alignment between program objectives and actual needs of the population.
Gaps in the Literature
Each of the reviewed studies enrolled infants and their parents into a program of home visiting after preterm delivery, either during or after discharge from the birth hospital. We were unable to find examples of home-visiting programs that enrolled families prenatally on the basis of social risk factors and reported specific outcome data for infants born preterm who continue to receive prevention services through the program. Further research would be useful in understanding the utility of a tailored curriculum for preterm infants within a larger program serving socially disadvantaged populations. Qualitative research may make an important contribution to this process by obtaining parents’ and home visitors’ views regarding the factors considered to be most important for the health and well-being of enrolled preterm infants.
Although previous studies of home visiting suggest that intensity of the intervention may be an important influence on program effectiveness,11,51 a subanalysis of data from the IHDP indicates that passive exposure to the intervention (ie, number of home visits) may not be as important as level of parental engagement.22 The current review demonstrates substantial heterogeneity in program implementation across studies as well as inclusion of non–home-based curriculum components. Future research in this area may focus on the effect of program intensity on outcomes for preterm infants enrolled in home visiting, with the goal of identifying a minimum duration and visit frequency to achieve improvements.
Finally, an important gap in interpretation of the current literature is the differential effect of home visiting on infants based on gestational age. Although 3 studies examine an interaction effect of birth weight for this intervention, stratification by birth weight alone may not sufficiently distinguish infants in terms of their true risk for complications.52 In light of the recent literature on neurodevelopmental and medical outcomes of late preterm infants, many of whom would not be classified as LBW, further research should focus on the effects of home visiting stratified by discrete gestational age ranges.
Strengths and Limitations of the Review
This is a comprehensive synthesis of recent evidence regarding the impact of home visiting on outcomes for preterm and LBW infants. Our review includes prospective studies only, thereby avoiding problems of reverse causality inherent in cross-sectional and case-control designs. Most studies included objective outcome measures assessed by examiners blinded to group status, minimizing the potential for reporting bias. In addition to assessing the methodological quality of included studies, our review evaluates the strength of program logic in relationship to its underpinning theory, which has been recently emphasized in the home-visiting literature. Last, our use of 2 independent reviewers to extract data is a strength of this review.
Although several included studies were well-designed and of sufficient size to detect clinically important intervention effects, many were of limited size, with attrition rates of a third or more contributing to findings that may have been biased. Additionally, because only published studies were included, this review may be subject to error because of publication bias. However, when the 9 studies contributing 1-year Bayley MDI score data were investigated with a funnel plot of SE, results did not appear to scatter asymmetrically (data not shown).
Conclusions
Many studies support that home visits in early infancy for preterm infants promote improved parent-infant interaction and infant development. The evidence regarding other infant outcomes, including morbidity, growth and nutrition, and child abuse or neglect, is more limited. Although few studies have evaluated the effectiveness of home visiting for preterm infants with additional social risk factors, the available literature suggests that targeted subgroups may confer benefit from these programs. Further studies are needed to examine the role of home visiting for preterm infants from socially disadvantaged backgrounds, including those who are enrolled in home visiting prenatally. Further evaluation of targeted interventions for this subgroup within larger home-visiting programs may strengthen their impact on health of high-risk communities and enhance the costs-benefits of home visiting, which has received a large public investment through the PPACA.
Acknowledgments
The authors thank Dr Rita Pickler for critical review of the manuscript and Dr Jareen Meinzen-Derr for biostatistical consultation.
Glossary
- Bayley MDI
Bayley Mental Developmental Index
- CI
confidence interval
- FACES
Family Adaptability and Cohesion Evaluation Scales
- HOME
Home Observation for Measurement of the Environment
- IHDP
Infant Health and Development Program
- LBW
low birth weight
- MDECAS
Maternal Developmental Expectations and Child-rearing Attitudes Survey
- NCAFS
Nursing Child Assessment Feeding Scales
- NCATS
Nursing Child Assessment Teaching Scales
- PPACA
Patient Protection and Affordable Care Act
- SMD
standardized mean difference
Footnotes
Dr Goyal conceptualized and designed the study, reviewed all included studies, and drafted the initial manuscript; Dr Teeters assisted with review of included studies and critically reviewed the manuscript; Dr Ammerman supervised conceptualization and design of the study, assisted with review of included studies, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of Mental Health, or the National Institutes of Health.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Goyal’s involvement in this project was supported by the Building Interdisciplinary Research Careers in Women’s Health program, cofunded by the Office of Research on Women’s Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, award 5K12HD051953-07. Dr Ammerman was supported by grant R01MH087499 from the National Institute of Mental Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary data for 2010. Natl Vital Stat Rep. 2011;60(2):1–26 [PubMed] [Google Scholar]
- 2.Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children’s health. Pediatrics. 2008;121(2):337–344 [DOI] [PubMed] [Google Scholar]
- 3.Astuto J, Allen L. Home visitation and young children: an approach worth investing in? Society for Research in Child Development. Soc Policy Rep. 2009;23:3–22 [Google Scholar]
- 4.Health Resources and Services Administration. Maternal, Infant, and Early Childhood Home Visiting program. 2010. Available at: http://mchb.hrsa.gov/programs/homevisiting/index.html. Accessed September 4, 2012
- 5.Olds DL, Henderson CR, Jr, Tatelbaum R, Chamberlin R. Improving the delivery of prenatal care and outcomes of pregnancy: a randomized trial of nurse home visitation. Pediatrics. 1986;77(1):16–28 [PubMed] [Google Scholar]
- 6.Lee E, Mitchell-Herzfeld SD, Lowenfels AA, Greene R, Dorabawila V, DuMont KA. Reducing low birth weight through home visitation: a randomized controlled trial. Am J Prev Med. 2009;36(2):154–160 [DOI] [PubMed] [Google Scholar]
- 7.McNaughton DB. Nurse home visits to maternal-child clients: a review of intervention research. Public Health Nurs. 2004;21(3):207–219 [DOI] [PubMed] [Google Scholar]
- 8.Issel LM, Forrestal SG, Slaughter J, Wiencrot A, Handler A. A review of prenatal home-visiting effectiveness for improving birth outcomes. J Obstet Gynecol Neonatal Nurs. 2011;40(2):157–165 [DOI] [PubMed]
- 9.Hollowell J, Oakley L, Kurinczuk JJ, Brocklehurst P, Gray R. The effectiveness of antenatal care programmes to reduce infant mortality and preterm birth in socially disadvantaged and vulnerable women in high-income countries: a systematic review. BMC Pregnancy Childbirth. 2011;11:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zahr L. An integrative research review of intervention studies with premature infants from disadvantaged backgrounds. Matern Child Nurs J. 1994;22(3):90–101 [PubMed] [Google Scholar]
- 11.Olds DL, Kitzman H. Review of research on home visiting for pregnant women and parents of young children. Future Child. 1993;3(3):53–92 [Google Scholar]
- 12.Martin JA, Kirmeyer S, Osterman M, Shepherd RA. Born a bit too early: recent trends in late preterm births. NCHS Data Brief. 2009(24):1–8 [PubMed]
- 13.Engle WA, Tomashek KM, Wallman C, Committee on Fetus and Newborn, American Academy of Pediatrics . “Late-preterm” infants: a population at risk. Pediatrics. 2007;120(6):1390–1401 [DOI] [PubMed] [Google Scholar]
- 14.Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available at: www.cochrane-handbook.org. Accessed September 4, 2012
- 15.Damato EG, Dill PZ, Gennaro S, Brown LP, York R, Brooten D. The association between CNS direct care time and total time and very low birth weight infant outcomes. Clin Nurse Spec. 1993;7(2):75–79 [DOI] [PubMed] [Google Scholar]
- 16.Brooten D, Kumar S, Brown LP, et al. A randomized clinical trial of early hospital discharge and home follow-up of very-low-birth-weight infants. N Engl J Med. 1986;315(15):934–939 [DOI] [PubMed] [Google Scholar]
- 17.Enhancing the outcomes of low-birth-weight, premature infants. A multisite, randomized trial. The Infant Health and Development Program. JAMA. 1990;263(22):3035–3042 [DOI] [PubMed] [Google Scholar]
- 18.Brooks-Gunn J, Gross RT, Kraemer HC, Spiker D, Shapiro S. Enhancing the cognitive outcomes of low birth weight, premature infants: for whom is the intervention most effective? Pediatrics. 1992;89(6 pt 2):1209–1215 [PubMed] [Google Scholar]
- 19.Casey PH, Bradley RH, Whiteside-Mansell L, Barrett K, Gossett JM, Simpson PM. Effect of early intervention on 8-year growth status of low-birth-weight preterm infants. Arch Pediatr Adolesc Med. 2009;163(11):1046–1053 [DOI] [PubMed] [Google Scholar]
- 20.Casey PH, Kelleher KJ, Bradley RH, Kellogg KW, Kirby RS, Whiteside L. A multifaceted intervention for infants with failure to thrive. A prospective study. Arch Pediatr Adolesc Med. 1994;148(10):1071–1077 [DOI] [PubMed] [Google Scholar]
- 21.Hill JL, Brooks-Gunn J, Waldfogel J. Sustained effects of high participation in an early intervention for low-birth-weight premature infants. Dev Psychol. 2003;39(4):730–744 [DOI] [PubMed] [Google Scholar]
- 22.Liaw FM, Meisels SJ, Brooks-Gunn J. The effects of experience of early intervention on low birth weight, premature children: The Infant Health and Development Program. Early Child Res Q. 1995;10:405–431 [Google Scholar]
- 23.McCarton CM, Brooks-Gunn J, Wallace IF, et al. Results at age 8 years of early intervention for low-birth-weight premature infants. The Infant Health and Development Program. JAMA. 1997;277(2):126–132 [PubMed] [Google Scholar]
- 24.Ramey CT, Bryant DM, Wasik BH, Sparling JJ, Fendt KH, LaVange LM. Infant Health and Development Program for low birth weight, premature infants: program elements, family participation, and child intelligence. Pediatrics. 1992;89(3):454–465 [PubMed] [Google Scholar]
- 25.Klein MD, Briggs MH. Facilitating mother-infant communicative interaction in mothers of high-risk infants. Commun Disord Q. 1987;10(2):95–106 [Google Scholar]
- 26.Haney M, Klein MD. Impact of a program to facilitate mother-infant communication in high-risk families of high-risk infants. Commun Disord Q. 1993;15(1):15–22 [Google Scholar]
- 27.Casiro OG, McKenzie ME, McFadyen L, et al. Earlier discharge with community-based intervention for low birth weight infants: a randomized trial. Pediatrics. 1993;92(1):128–134 [PubMed] [Google Scholar]
- 28.Zahr LK. Home-based intervention after discharge for Latino families of low-birth weight infants. Infant Ment Health J. 2000;21(6):448–463 [Google Scholar]
- 29.Teti D, Black MM, Viscardi R, et al. Intervention with African American premature infants: four-month results of an early intervention program. J Early Interv. 2009;31(2):146–164 [Google Scholar]
- 30.Ross GS. Home intervention for premature infants of low-income families. Am J Orthopsychiatry. 1984;54(2):263–270 [DOI] [PubMed] [Google Scholar]
- 31.Resnick MB, Reiss J, Eyler FD, Schauble P. Children's developmental services: a multidisciplinary program of psychological and educational services for neonatal intensive care. J Couns Dev. 1988;66:279–282 [Google Scholar]
- 32.Resnick MB, Eyler FD, Nelson RM, Eitzman DV, Bucciarelli RL. Developmental intervention for low birth weight infants: improved early development outcome. Pediatrics. 1987;80(1):68–74 [PubMed] [Google Scholar]
- 33.Resnick MB, Armstrong S, Carter RL. Developmental intervention program for high-risk premature infants: effects on development and parent-infant interactions. J Dev Behav Pediatr. 1988;9(2):73–78 [PubMed] [Google Scholar]
- 34.Rauh VA, Achenbach TM, Nurcombe B, Howell CT, Teti DM. Minimizing adverse effects of low birthweight: four-year results of an early intervention program. Child Dev. 1988;59(3):544–553 [PubMed] [Google Scholar]
- 35.O’Reilly KA, O’Reilly JP, Furuno S. Predicting to 9-month performance of premature infants. Phys Ther. 1986;66(4):508–515 [DOI] [PubMed] [Google Scholar]
- 36.Nurcombe B, Howell DC, Rauh VA, Teti DM, Ruoff P, Brennan J. An intervention program for mothers of low-birthweight infants: preliminary results. J Am Acad Child Psychiatry. 1984;23(3):319–325 [DOI] [PubMed] [Google Scholar]
- 37.Furuno S, O'Reilly KR, Ahern F. Transdisciplinary teamwork with parents of premature infants. In: Harel S, Anastasiow N, eds. The At-Risk Infant: Psycho/Social/Medical Aspects. Baltimore: Paul H. Brookes Publishing Co.; 1985:51–63 [Google Scholar]
- 38.Field TM, Widmayer SM, Stringer S, Ignatoff E. Teenage, lower-class, black mothers and their preterm infants: an intervention and developmental follow-up. Child Dev. 1980;51(2):426–436 [PubMed] [Google Scholar]
- 39.Field T, Widmayer S, Greenberg R, Stoller S. Effects of parent training on teenage mother and their infants. Pediatrics. 1982;69(6):703–707 [PubMed] [Google Scholar]
- 40.Beckwith L. Intervention with disadvantaged parents of sick preterm infants. Psychiatry. 1988;51(3):242–247 [DOI] [PubMed] [Google Scholar]
- 41.Barrera ME, Rosenbaum PL, Cunningham CE. Early home intervention with low-birth-weight infants and their parents. Child Dev. 1986;57(1):20–33 [DOI] [PubMed] [Google Scholar]
- 42.Barrera ME, Cunningham CE, Rosenbaum PL. Low birth weight and home intervention strategies: preterm infants. J Dev Behav Pediatr. 1986;7(6):361–366 [PubMed] [Google Scholar]
- 43.Achenbach TM, Phares V, Howell CT, Rauh VA, Nurcombe B. Seven-year outcome of the Vermont Intervention Program for Low-Birthweight Infants. Child Dev. 1990;61(6):1672–1681 [PubMed] [Google Scholar]
- 44.Achenbach TM, Howell CT, Aoki MF, Rauh VA. Nine-year outcome of the Vermont intervention program for low birth weight infants. Pediatrics. 1993;91(1):45–55 [PubMed] [Google Scholar]
- 45.Affleck G, Tennen H, Rowe J, Roscher B, Walker L. Effects of formal support on mothers’ adaptation to the hospital-to-home transition of high-risk infants: the benefits and costs of helping. Child Dev. 1989;60(2):488–501 [DOI] [PubMed] [Google Scholar]
- 46.Finello KM, Litton KM, deLemos R, Chan LS. Very low birth weight infants and their families during the first year of life: comparisons of psychosocial outcomes based on after-care services. J Perinatol. 1998;18(4):266–271 [PubMed] [Google Scholar]
- 47.Finello KM, Litton KM, deLemos R, Chan LS. Very low birth weight infants and their families during the first year of life: comparisons of medical outcomes based on after care services. J Perinatol. 1998;18(5):365–371 [PubMed] [Google Scholar]
- 48.Bugental DBS, Schwartz A. A cognitive approach to child mistreatment prevention among medically at-risk infants. Dev Psychol. 2009;45(1):284–288 [DOI] [PubMed] [Google Scholar]
- 49.Spencer N, Wallace A, Sundrum R, Bacchus C, Logan S. Child abuse registration, fetal growth, and preterm birth: a population based study. J Epidemiol Community Health. 2006;60(4):337–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Segal L, Sara Opie R, Dalziel K. Theory! The missing link in understanding the performance of neonate/infant home-visiting programs to prevent child maltreatment: a systematic review. Milbank Q. 2012;90(1):47–106 [DOI] [PMC free article] [PubMed]
- 51.Nievar MA, Van Egeren LA, Pollard S. A meta-analysis of home visiting programs: moderators of improvement in maternal behavior. Infant Ment Health J. 2010;31(5):499–520 [DOI] [PubMed] [Google Scholar]
- 52.Wilcox AJ. On the importance—and the unimportance—of birthweight. Int J Epidemiol. 2001;30(6):1233–1241 [DOI] [PubMed] [Google Scholar]
- 53.Kang R, Barnard K, Hammond M, et al. Preterm infant follow-up project: a multi-site field experiment of hospital and home intervention programs for mothers and preterm infants. Public Health Nurs. 1995;12(3):171–180 [DOI] [PubMed] [Google Scholar]
- 54.Neu M, Robinson J. Maternal holding of preterm infants during the early weeks after birth and dyad interaction at six months. J Obstet Gynecol Neonatal Nurs. 2010;39(4):401–414 [DOI] [PMC free article] [PubMed] [Google Scholar]