Abstract
Background and aim: Cervical cancer is one of the most common causes of cancer mortality among women worldwide but it is one of the most preventable cancers due to the Pap smear test. The aim of this study was to estimate the participation rate of females in screening of cervical cancer with Pap smear test.
Methods: The study took place in a hospital in Rural Northern Greece during April and May 2007. Convenience sampling was performed and questionnaires were completed by 214 eligible females aged 20-64 years.
Results: One hundred and twenty four (57.9%) of the participants had had a Pap-test at some point in their lifetime. 72 of them (33.65%) had the test performed for the first time according to current guidelines. 13.6% were unaware about the recommended onset age of the test, 16.4% did not know the proper intervals, while 22.4% did not know the recommended upper age limit. 32.6% were informed by mass media, family members and friends. The take-up rates, the source of information and the setting where the examination was performed were related to age, origin, income, educational status, type of occupation and place of residence. Disparities in participation rates were detected.
Conclusions: Special efforts should be made by National Health Services towards enhancing secondary prevention of cervical cancer by increasing participation rates of older women, those with lower educational background, females with low income, Roma, retired or unemployed and residents of rural areas.
Keywords: secondary prevention, screening, participation rate, cervical cancer, Pap smear test
Cervical cancer is one of the most common causes of cancer mortality among women worldwide. Despite its high prevalence, it is one of the most preventable cancers due to the wide application of Pap smear test, an easy and cheap screening tool1. The disease affects mainly less developed countries where 83.1% of the cases and 85.55% of the deaths are registered2. Moreover, it causes more than 2.7 million years of life lost in women 25 to 64 years universally3 . In Europe (the 27 countries in the European Union) cervical cancer is the fourteenth cause of cancer related mortality in females. The incidence of the disease in Europe shows a peak in the age group of 45-50 years and one in the age group of 80-85 years4. Mortality of cervical cancer demonstrates decreasing trends from 1973 to 20012. This could be partially attributed to widespread screening with Pap-smear test. Its wide application as a screening tool for cervical cancer led to the decrease of the mortality of the disease up to 80% in countries with organized screening systems such as United Kingdom, Netherlands, Scandinavian countries5. In European countries that reduction was about 50-60% 6. In Greece 166 deaths/100.000 from cervical cancer were reported during 2008. Crude mortality rate was 5.5/100.000 and agespecific mortality rate 3.8/100.0007. In accordance with international data the disease affects mainly women over 40 years, while its incidence increases with age. Alike the situation in the European Union, mortality in Greece shows a decreasing trend from 1961 towards 20068.
Infection with Human Papilloma Virus (HPV) is a necessary condition for cervical cancer in combination with other causal factors. It is estimated that 99% of women suffering from cervical cancer were infected with HPV9 . Types 16 and 18 are most frequently detected. About 50-80% of sexually active women will be infected by HPV at some time throughout their life 10.
Other risk factors for cervical cancer include multiparity 11, use of per os contraceptives for more than five years12, smoking13, immunosuppression, concomitant infection with sexually transmitted virus other than HPV (e.g. Herpes simplex virus-2)14 , multiple sexual partners or sexual contact at an early age as well as low social class15 .
According to the recommendations of the Committee of the European Union for the screening of cancer, test-Pap is recommended the latest at the age of 30 and certainly not before the age of 20. The upper age limit depends on the available economic resources, but it should not be lower than 60 years old. The intervals should be 3 to 5 years16 .
Pap-test was introduced in clinical practice in the 1950's. Its specificity and sensitivity vary. In the literature two meta-analyses are referred. According to the first one, sensitivity varies from 11% to 99% and specificity from 14% to 97%17. The second meta-analysis describes sensitivity from 30 to 87% and specificity from 86 to 100% 6.
From the review in the literature, a 53.49% participation rate was reported in Greece, in a screening programme for cervical cancer in Chalkidiki (Ormilia) while in the municipality of Messinia and Ilia the participation rate was 58.4% 18. A second study about females' knowledge and their attitude towards family planning is referred19. In this study 29-30.1% of the participants had a Pap-test performed during the year before the study19 . Hellas Health I survey recorded that 59.4% of Greek women aged 21-69 years performed Pap-smear test within the past 3 years 20. In a study in a Greek province 79% of the female who participated had conducted Pap smear test at least once in their lifetime21.
The main purpose of the present study is to determine women's participation in screening of cervical cancer with Pap-test, in a rural area in Northern Greece, and the identification of the factors that affect compliance with current recommendations. Moreover, women's knowledge about present guidelines for the prevention of the disease and the source of information are being studied. Finally, the role of the National Health System in screening is being investigated.
Materials and Methods
A questionnaire was administered to females, who accompanied patients to the Emergency Department of General Hospital of Veria, Imathia, a rural area in Northern Greece, from April through May 2007. The target population was restricted to females 20-64 years old. Exclusion criteria were: a prior diagnosis of cervical cancer and history of total hysterectomy.
The questionnaire included 34 questions divided into 6 units. These questions recorded participants' demographic characteristics and were tailored to investigate the occurrence of the examination, their participation in other screening tests, knowledge about current guidelines for Pap-test and degree of adherence to them, information and source of information about Pap smear, as well as, confidence in Public Health Services.
In order to determine precisely the exact participation rate, according to the age of each participant, two new variables were computed: the ideal number of Pap-tests and compliance index. The first variable derives from the ratio of the difference between the age of each participant with the lower onset age of Pap-test (20 years), divided with the intervals of the examination (3 years):
Ideal number of Pap-tests=(age-20)/3
Compliance index is defined as the ratio between the total number of Pap-tests of each participant and the ideal number of them:
Compliance index=total number of Pap-tests/ideal number
Compliance index lower than one, indicates lower number of Pap-test than the proposed for the participant's age. The opposite stands for compliance index higher than one. Obviously index equal to one means that the proposed number of Pap-tests is the same with the actual one.
Statistical Analysis
All statistical analysis was performed using the statistical software SPSS for Windows22. Analysis of the sample's demographic characteristics, as well as the participants' answers, were conducted with descriptive statistics and the calculation of mean, standard deviation, range, minimum and maximum and frequency's analysis. The variables which deviated significantly from normality were analyzed through non-parametric tests. To investigate a statistical correlation between two qualitative variables x2 test was applied, in the case of one quantitative and one qualitative variable Kruskal-Wallis test for K-Independent samples was used, while Spearman correlation was applied for two consecutive quantitative variables. Mann-Whitney test for 2-Independent samples was used to help identify possible differences between groups. The level of statistical significance was set at 0.05. Linear regression modeling was used to investigate the relationship between the compliance index and certain demographic attributes of women sampled in order to assess the adjusted effect of those variables on compliance to cervical cancer screening guidelines.
Ethical approval was obtained by the Hospital's Scientific Council in order to conduct the field research, while all subjects were informed about the nature and the aim of the study before consenting to complete the questionnaire.
Results
From the 314 women initially interviewed, 214 (68.15%) completed the questionnaire, 39 (12.42%) refused to participate for various reasons and 61 (19.43%) fulfilled the exclusion criteria and weren't included in the study. Participants' demographic characteristics are summarized in Table 1. Women's attitudes about cervical cancer screening are described in Table 2.
Table 1. The demographic characteristics of the participants which were considered as independent variables of the statistical analysis.
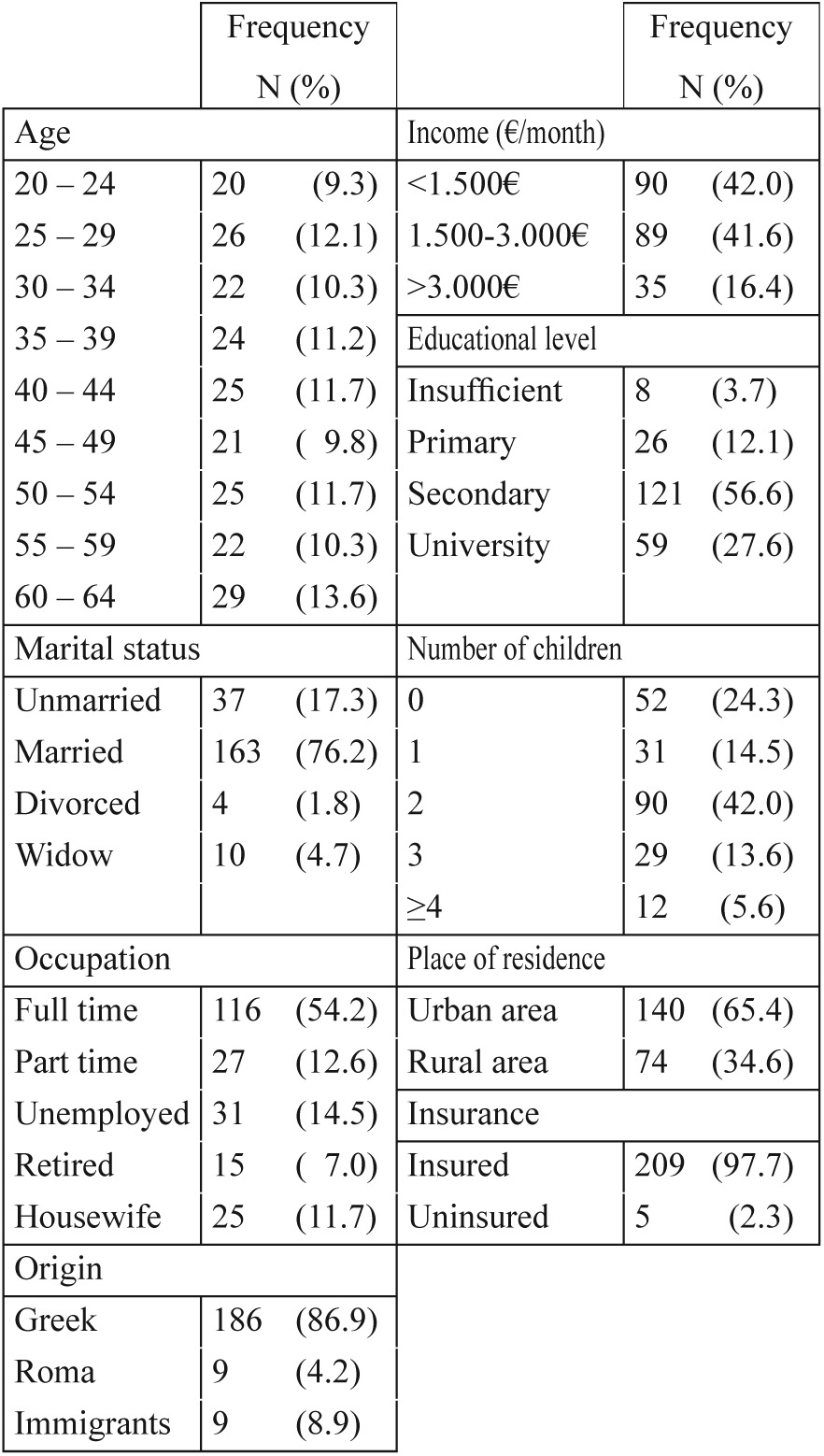
Table 2. Women's attitudes about cervical cancer screening (Pap smear test).
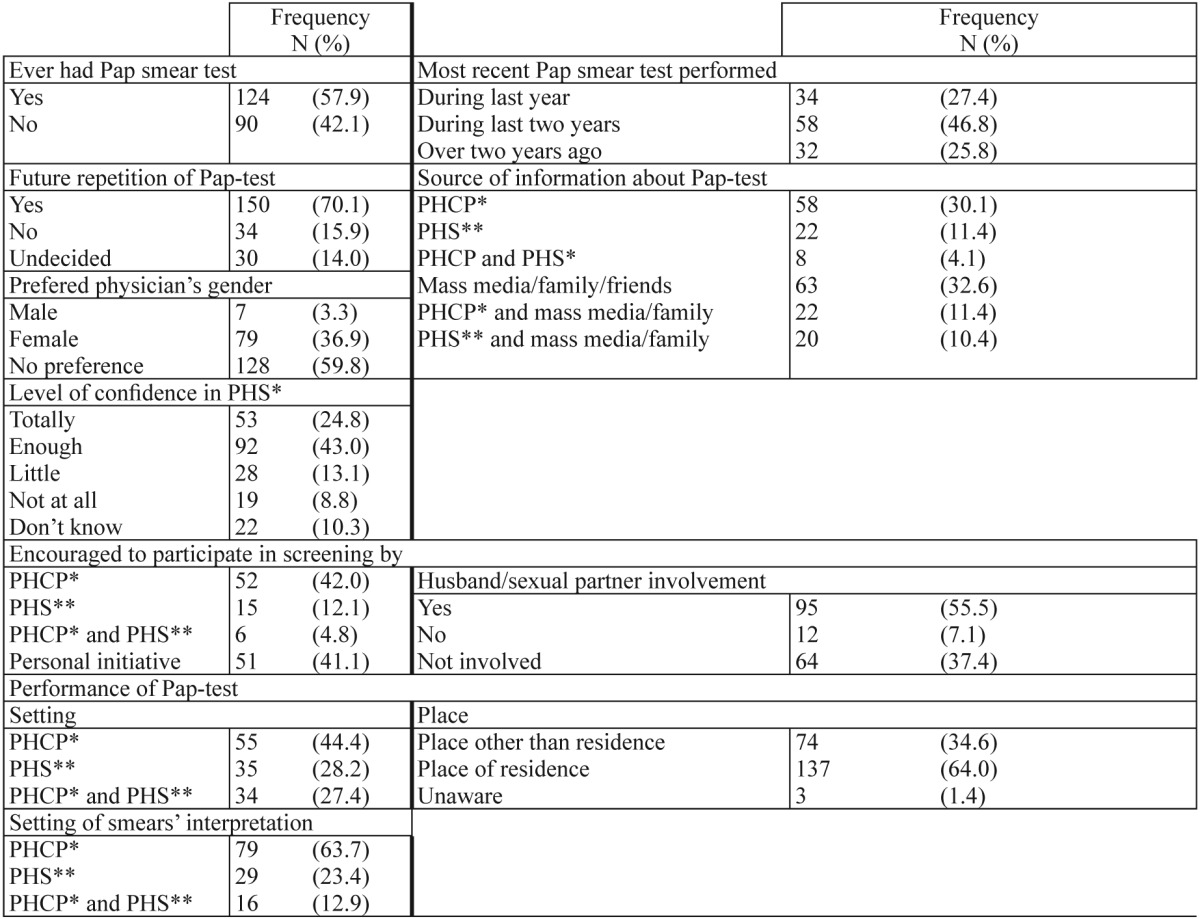
*PHCP: Private health care provider
**PHS: Public Health Services
Womens' participation and attitudes about cervical cancer screening with Pap smear test as well as source of Information about it and level of confidence in PHS for test's performance
47 (21.9%) of the participants trust little or not at all Public Health Services. The physician's gender was important for 79 (36.9%) women who preferred a female physician to perform the Pap-test. In our study 74 (34.6%) of the participants had to transport to a place other than their residence to participate in screening. A considerable proportion of the women who had conducted a Papsmear test (51 women, 41.1%) took part in a screening programme driven by personal initiative and 55.5% (95 women) were encouraged by their partner. Unfortunately only 12.1% of the sample (15 women) were encouraged by public health services to participate in a screening programme and less than one fourth (44 women, 21.8%) were even informed by health professionals working in the public services. Nevertheless, 67.8% of the women asked expressed their confidence in the Public Health System for the administration of cervical cancer screening. The role of social environment in providing information about the Pap smear test has also emerged with about one third of the women asked (32.6%) reporting that they received information from the mass media and family or friends.
Knowledge of women about Pap-test was investigated by means of three open-ended questions about the recommended onset age of the test, intervals and upper age limit. An important finding was that 178 (83.2%) and 126 (58.9%) women were incorrectly informed about the intervals between Pap-tests and the upper age limit of the examination respectively. Incorrectly informed about current recommendations were women aged 20- 24 (42.86%), those older than 55 years (21.43%), the group with income lower than 1.500€/month (20%), participants who didn't graduate from primary school (60%) and women of Roma origin (35.7%). Unemployed women and housewives were also incorrectly informed (57.1% and 59.5% respectively).
Statistically significant correlation between participants' age and their opinion about the onset age of Paptest was observed (f: 40.15, p<0.001) with 150 (70.1%) of them being aware about the proper onset age. 85 (87.63%) of the women aged 25-45 years knew the proper onset age, while 16 (20%) of those aged 50-64 years, as well as, 6 (30%) of the participants aged 20-24 years were uninformed (Table 3).
Table 3. Results of statistical analysis.
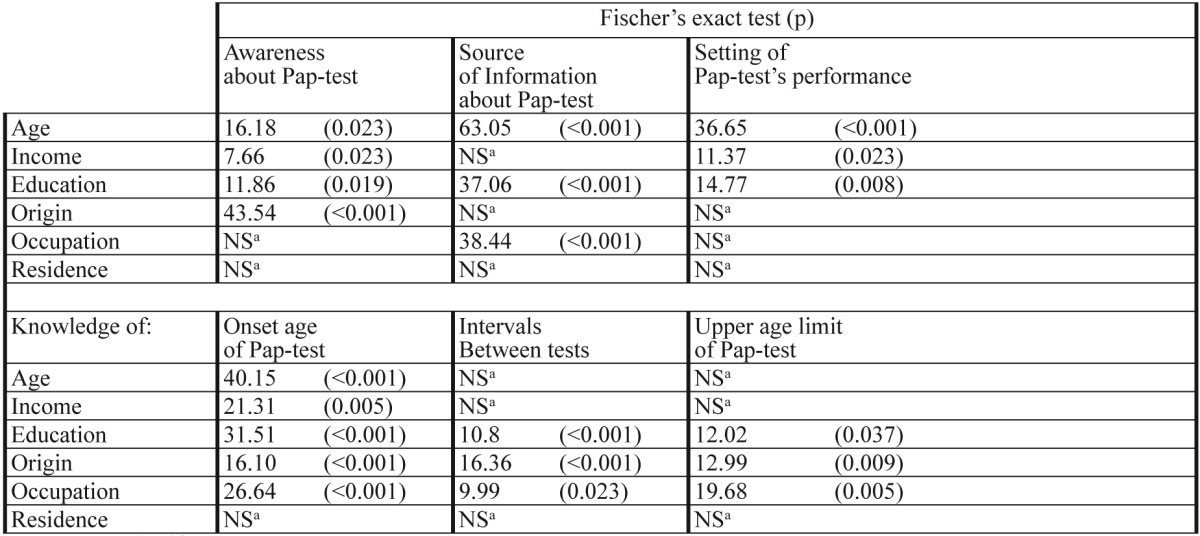
aNS:No Significant
Results of statistical association between women's awareness about current guidelines for cervical cancer screening with Paptest, source of information and setting of Pap-test's performance, as well as women's knowledge about current guidelines for cervical cancer screening with Pap-test with their demographic characteristics
Source of information about cervical cancer screening was statistically related with age (f: 63.05, p<0.001), education (f: 37.06, p<0.001) and occupation (f: 38.44, p<0.001) (Table 3). Participants younger than 44 years (38.46%), those with full time occupation (35.35%) and university graduates (45.76%) chose to be informed by a private health care provider, while those over the age of 44 years (39.17%) and graduates from primary/secondary level of education (34.7%) preferred the mass media and friends or family.
Selection of the setting where the test was performed was related to age (f: 36.65, p<0.001), income (f: 11.37, p=0.023) and education (f: 14.77, p=0.008) (Table 3). Private care providers were preferred by 41.17% of university graduates, 49.5% of those with income higher than 1.500€/month and 57% of women aged 20-49 years. On the other hand public health services were selected by 45.45% of women with income less than 1.500€/month, as well as 47.7% of those aged older than 50 years.
Finally as shown in Table 4 45.1% of the sample participated in cervical cancer screening programs as frequently (or even more) as it is recommended by current guidelines. A negative correlation between age and compliance index was recorded (r=-0.17, p=0.00), with younger women having a higher compliance index. Compliance increased linearly with income and level of education. Both Greek women (p=0.001) and immigrants (p=0.026) had higher compliance than Roma. Women with a full time occupation had a higher compliance index compared to unemployed (p=0.001), retired (p=0.005) and housewives (p=0.001).
Table 4. Compliance index to current Pap-test guidelines.
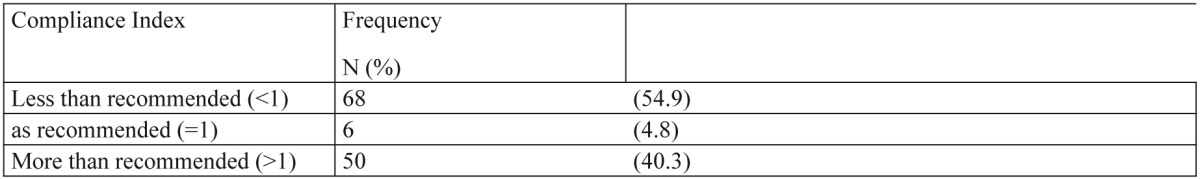
The observed frequency of compliance index to current Pap-test guidelines
A linear regression model depicting the association between the compliance index and demographic characteristics of women was applied as illustrated in Table 5. A negative association between age and compliance index was recorded (β= -0.184, p=0.011), with younger women having a higher compliance index. On the other hand compliance increased linearly with income (β= 0.281, p<0.001), meaning that women of higher income followed more closely current guidelines for cervical cancer screening. Greek women also showed higher compliance than immigrants or Roma (β= -0.214, p=0.001) even after adjusting for socioeconomic factors such as income and education.
Table 5. Association between compliance index and demographic characteristics of women.
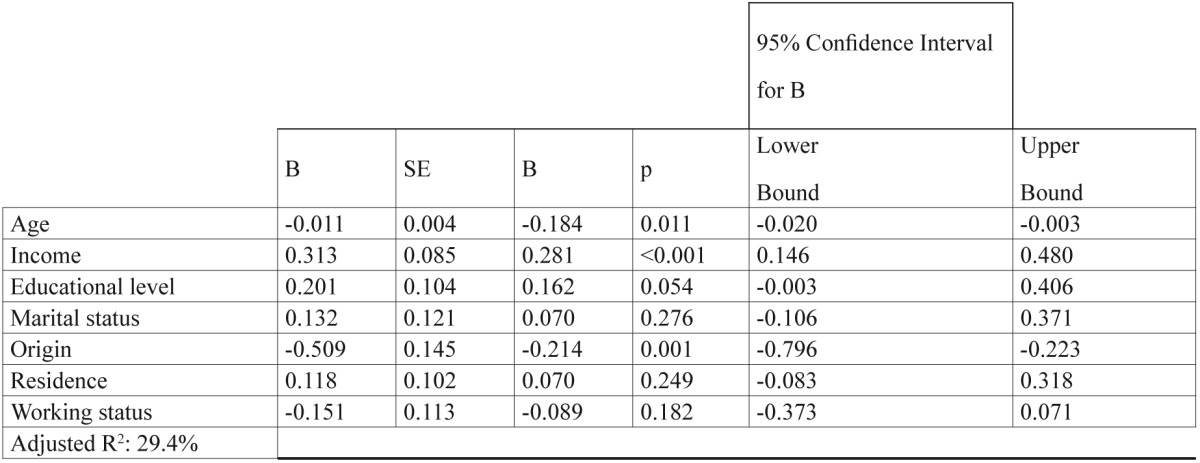
Linear regression model depicting the association between the compliance index to current Pap-test guidelines and demographic characteristics of women
Discussion
In our study age, income, educational level, type of occupation and origin were identified as significant factors associated with participation rates in Pap-test screening programs, women's source of information about them, their knowledge about guidelines and preferred setting of test performance. Women that do not usually comply with the guidelines for cervical cancer screening are older in age, uninsured and belong in minority groups23,24, of lower socioeconomic status24,25. In a study conducted in Spain participation rate in screening of cervical cancer with Pap-test was associated with educational level, family status, occupation, place of residence26.
With the application of the compliance index it was found that women's adherence to the established guidelines was unsatisfactory. More than half of the participants (54.84%, n=68) who have performed Pap-test did not comply with the current guidelines. Our finding that compliance decreased with age is concordant with existing literature23 and important, because younger women are at greater risk for contracting HPV than are their older counterparts27 and therefore in higher risk of developing cervical lesions (CIN) that can easily be identified by Pap smear testing 28,29.
The vast majority of the sample (90.2%, n=193) considered themselves informed about the Pap-test, a claim that was not supported by their actual answers. This discrepancy between the participants' opinion of their information status and their answers suggests that the way and the sources of information provided to the public need to be reconsidered. Information provided on cervical cancer screening need to be revised following precise and evidence-based guidelines.
Only a quarter of the participants were informed by Public Health Services (PHS), and a small proportion attended an organized public screening programme. Inefficiency and a partial absence of PHS in the field of dispersing public information about screening were clearly demonstrated. It is necessary to reorganize and reinforce the role of PHS in this field.
Less than one third of the sample chose the public health sector setting to have a Pap-test performed. A preference for a private physician was indicated. This fact could probably be attributed to other factors, such as the nature of the examination that provokes embarrassment when a proper physician-patient relationship is not assured30,31 and the fact that in Greece outpatient gynaecologic services are mainly private.
It is worth mentioning that, on the other hand, a significant percentage (43%) of the sample trust the public health services, even though only 28.2% of the sample selects them exclusively for having their cervical cancer screening.
Results from this study are in accordance with findings from both Chalkidiki and Messinia study18, and Hellas Health I survey20 which recorded participation rates of 53.49% and 59.4% respectively while a study in a Greek province reported that 79% of the participants had conducted the Pap-test at least once in their lifetime21. On the other hand in countries with organized screening programs such as Sweden, Finland, United Kingdom participation rates come up to 80% 32.
In Greece cancer screening is opportunistic and not systematic33. Such activities are mainly occasional and depend on every woman's personal initiative, in contrast to other countries such as the Scandinavian countries, United Kingdom or the Netherlands5. The organization and implementation of a nationwide system for screening population must become a high priority. Moreover, special efforts should be made by the Public Health Services towards increasing participation rates of older women, those with lower educational background, females with income of less than 1.500€/month, Roma, retired or unemployed women and residents of rural areas. The ways of informing sufficiently and properly these vulnerable populations could be the subject of another study.
The results of this study should be interpreted under the context of its limitations. Firstly, the women interviewed did not derive through stratified sampling. They were recruited from consecutive women accompanying patients at an emergency department. One could suggest that people who visit public hospitals represent a special group with specific social, economic and cultural characteristics. The selection of the sample from the emergency department, and not from outpatient clinics, aimed to counterbalance this bias. According to the data of the last census from the National Statistics Service (NSSG 2007)34, the representation of each age-group of the sample is comparable to the actual population of the prefecture of Imathia. Women aged 20-64 in Imathia, which is the target age group of the study, are 4338534. Finally, the response rate (68.15%) should be taken into consideration upon the interpretation of the results. Origin was used with caution because of the unequal representation of each subgroup at the sample (Greek, Roma and immigrants). However, its statistical correlation with the variables under study was considered important.
According to this study cervical cancer screening in the sample of women of this study is not accomplished within acceptable levels of population coverage, compliance and socioeconomic strata. Cervical cancer represents a substantial public health problem with economic and social dimensions, potentially life-threatening. Prompt detection at an early stage improves the prognosis of the disease, quality of life and in many cases reduces mortality. Cervical cancer screening should be part of organized screening programs that address the whole population recommended to participate1. Taking these factors into consideration, efforts must be made by the state for wide, organized and systematic application of screening population-based programs, promoting the application of current guidelines and providing equal opportunities for their implementation.
Conflict of interest: none
References
- 1.World Health Organization. National Cancer Control Programmes. Policies and Managerial Guidelines. 2nd edition. Geneva: WHO; 2002. [Google Scholar]
- 2.Parkin DM, Whelan S, Ferlay J, Raymond L, Young J. Cancer Incidence in Five Continents. Vol VIII. Lyon, France: IARC Press; 2002. (IARC Scientific Publications No. 155). [Google Scholar]
- 3.Yang BH, Bray FI, Parkin DM, Sellors JW, Zhang ZF. Cervical cancer as a priority for prevention in different world regions: an evaluation using years of life lost. IJC. 2004;109:418–424. doi: 10.1002/ijc.11719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arbyn M, Autier P, Ferlay J. Burden of cervical cancer in the 27 member states of the European Union: estimates for 2004. Ann Oncol. 2007;18:1425–1427. doi: 10.1093/annonc/mdm377. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Comprehensive cervical cancer control: a guide to essential practice. Geneva, Switzerland: World Health Organization; 2006. [PubMed] [Google Scholar]
- 6.Nanda K, Mc Crory DC, Myers ER, Bastian LA, Hasselblad V, Hickey JD, et al. Accuracy of the Papanicolaou test in screening for and follow-up of cervical cytologic abnormalities: a systematic review. Ann Intern Med. 2000;132:810–819. doi: 10.7326/0003-4819-132-10-200005160-00009. [DOI] [PubMed] [Google Scholar]
- 7.Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;4:765–781. doi: 10.1016/j.ejca.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 8.International Agency for Research on Cancer; World Health Organization. IARC Handbooks of Cancer Prevention. Vol 10. Lyon, France: IARC Press; 2006. Cervix Cancer Screening. [Google Scholar]
- 9.Planning and Implementing Cervical Cancer Prevention and Control Programs: A Manual for Managers. Seattle: Alliance for Cervical Cancer Prevention; 2004. Available from: http://www.alliance-cxca.org/english/publications. [Google Scholar]
- 10.Moscicki AB, Hills N, Shiboski S, Powell K, Jay N, Hanson E, et al. Risks for incident human papillomavirus infection and low grade squamous intraepithelial lesion development in young females. JAMA. 2001;285:2995–3002. doi: 10.1001/jama.285.23.2995. [DOI] [PubMed] [Google Scholar]
- 11.Munoz N, Franceschi S, Bosetti C, Moreno V, Herrero R, Smith JS, et al. Role of parity and human papillomavirus in cervical cancer: the IARC multicentric case-control study. The Lancet. 2002;359:1093–1101. doi: 10.1016/S0140-6736(02)08151-5. [DOI] [PubMed] [Google Scholar]
- 12.Moreno V, Bosch FX, Muñoz N, Meijer CM, Shah V, Walboomers JMM, et al. Effect of oral contraceptives on risk of cervical cancer in women with human papillomavirus infection: the IARC multicentric case-control study. The Lancet. 2002;359:1085–1092. doi: 10.1016/S0140-6736(02)08150-3. [DOI] [PubMed] [Google Scholar]
- 13.Lacey JJ, Frisch M, Brinton L, Abbas F, Barnes W, Gravitt P, et al. Associations between smoking and adenocarcinomas and squamous cell carcinomas of the uterine cervix (United States) Cancer Cause Control. 2001;12:153–161. doi: 10.1023/a:1008918310055. [DOI] [PubMed] [Google Scholar]
- 14.Smith JS, Herrero R, Bosetti C, Muñoz N, Bosch FX, Eluf-Neto J, et al. Herpes simplex virus-2 as a human papillomavirus cofactor in the etiology of invasive cervical cancer. JNCI. 2002;94:1604–1613. doi: 10.1093/jnci/94.21.1604. [DOI] [PubMed] [Google Scholar]
- 15.Dos Santos Silva I, Beral V. In Social inequalities and cancer. Lyon: IARC Scientific Publications; 1997. Socioeconomic differences in reproductive behaviour; pp. 285–308. (IARC Scientific Publications No. 138). [PubMed] [Google Scholar]
- 16.Advisory Committee on Cancer Prevention. Recommendations on cancer screening in the European Union. Eur J Cancer. 2000;36:1473–1478. doi: 10.1016/s0959-8049(00)00122-2. [DOI] [PubMed] [Google Scholar]
- 17.Fahey M, Irwig L, Macaskillet P. Meta-analysis of Pap Test Accuracy. American J Epidemiol. 1995;141:680–689. doi: 10.1093/oxfordjournals.aje.a117485. [DOI] [PubMed] [Google Scholar]
- 18.Riza E, Kyriakogianni-Psaropoulou P, Koumantakis E, Symiakaki H, Garas I, Linos A. Cervical cancer screening in Greece. Eur J Cancer. 2000;36:2227–2232. doi: 10.1016/s0959-8049(00)00314-2. [DOI] [PubMed] [Google Scholar]
- 19.Tsamandouraki K, Alamanos Y, Tountas Y. Knowledge of and attitudes towards family planning and early detection of breast and cervical cancer in two female populations in Greece. Social and Preventive Medicine. 1992;37:136–141. doi: 10.1007/BF01624624. [DOI] [PubMed] [Google Scholar]
- 20.Dimitrakaki C, Boulamatsis D, Mariolis A, Kontodimopoulos N, Niakas D, Tountas Y. Use of cancer screening services in Greece and associated social factors: results from the nation-wide Hellas Health I survey. Eur J Cancer Prev. 2009;18:248–257. doi: 10.1097/CEJ.0b013e32832405d6. [DOI] [PubMed] [Google Scholar]
- 21.Gesouli-Voltyraki E, Tsetsekou E, Metaxa A, Borsi A, Noula M. The knowledge of women in a Greek Province regarding the cervical cancer, its prevention capabilities and the Pap-test. HSJ. 2010;4:101–109. [Google Scholar]
- 22.Drive S Wacker. SPSS 16.0 for Windows. Chicago, Illinois: SPSS Inc; 2005. [Google Scholar]
- 23.Meissner HI, Breen N, Coyne C, Legler GM, Green DT, Edwards BK. Breast and Cervical Cancer Screening Intervention: An Assessment of the Literature. Cancer Epidemiol, Biomarkes Prev. 1998;7:951–961. [PubMed] [Google Scholar]
- 24.Robinson JM, Shavers V. The Role of Health Insurance Coverage in Cancer Screening Utilization. JHCPU. 2008;19:842–856. doi: 10.1353/hpu.0.0048. [DOI] [PubMed] [Google Scholar]
- 25.Eaker S, Adami HO, Sparen P. Attitudes to screening for cervical cancer: a population-based study in Sweden. Cancer Cause Control. 2001;12:519–528. doi: 10.1023/a:1011233007132. [DOI] [PubMed] [Google Scholar]
- 26.Luengo matos S, Mupoz Van Den Eynde A. Use of Pap Test For cervical Cancer Screening and Factors Related With Use in Spain. Aten Primaria. 2004;33:229–234. doi: 10.1016/S0212-6567(04)79407-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leinonen M, Nieminen P, Kotaniemi-Talonen L, Malila N, Tarkkanen J, Laurila P, et al. Age-specific Evaluation of Primary Human Papillomavirus Screening vs Conventional Cytology in a Randomized Setting. JNC. 2009;101:1612–1623. doi: 10.1093/jnci/djp367. [DOI] [PubMed] [Google Scholar]
- 28.Naucler P, Ryd W, Törnberg S, Strand A, Wadell G, Elfgren K, et al. Human papillomavirus and Papanicolaou tests to screen for cervical cancer. N Engl J Med. 2007;357:1589–1597. doi: 10.1056/NEJMoa073204. [DOI] [PubMed] [Google Scholar]
- 29.Dillner J, Rebolj M, Birembaut P, Petry KU, Szarewski A, Munk C, et al. Long term predictive values of cytology and human papillomavirus testing in cervical cancer screening: joint European cohort study. BMJ. 2008;377:a1754. doi: 10.1136/bmj.a1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buetow S, Janes R, Steed R, Ihimaera L, Elley CR. Why don't some women return for cervical smears? A hermeneutic phenomenological investigation. Health Care Women I. 2007;28:843–852. doi: 10.1080/07399330701563251. [DOI] [PubMed] [Google Scholar]
- 31.Markovic M, Kesic V, Topic L, Matejic B. Barriers to cervical cancer screening: A qualitative study with women in Serbia. Soc Sci Med. 2005;61:2528–2535. doi: 10.1016/j.socscimed.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Anttila A, Ronco G, Clifford G, Bray F, Hakama M, Arbyn M. Cervical cancer screening programmes and policies in 18 European countries. Br J Cancer. 2004;91:935–941. doi: 10.1038/sj.bjc.6602069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Linos A, Riza E. Comparison of cervical cancer screening programmes in the European Union. Eur J Cancer. 2000;36:2260–2265. doi: 10.1016/s0959-8049(00)00321-x. [DOI] [PubMed] [Google Scholar]
- 34.National Statistical Service of Greece, NSSG. Concise Statistical Yearbook 2006. Pireas, Greece: NSSG Press; 2007. Available at: http://www.statistics.gr. [Google Scholar]


