Abstract
Introduction
The purpose of this study was to assess the severity of dissociation reported by borderline patients and axis II comparison subjects over 10 years of prospective follow-up.
Method
The Dissociative Experiences Scale (DES)—a 28-item self-report measure—was administered to 290 borderline inpatients and 72 axis II comparison subjects during their index admission. It was also re-administered at five contiguous two-year follow-up periods.
Results
The overall severity of dissociative experiences of those in both study groups decreased significantly over time but was discernibly greater in borderline patients (61% vs. 43%). The same pattern emerged for the sub-types of dissociation that were studied: absorption, depersonalization, and amnesia.
Conclusion
The severity of dissociation declines significantly over time for even severely ill borderline patients. However, it remains a recurring problem for over a third of those with DES scores that initially were in the range associated with trauma-spectrum disorders.
Keywords: borderline personality disorder, dissociation, longitudinal course
An early review of the clinical literature suggested that three areas of cognitive disturbance were particularly associated with the diagnosis of borderline personality disorder (BPD): experiences of depersonalization and derealization, feelings of distrust and suspiciousness, and stress-related micropsychotic episodes (1). Twelve studies were subsequently published that assessed the presence of the dissociative experiences reported by borderline patients (2-13). Taken together, it was found that these experiences were both common and discriminating for those with BPD.
More recently, studies have focused on the severity of the dissociative symptoms of borderline patients using the Dissociative Experiences Scale (DES) (14-18)—a 28-item self-report measure with proven psychometric properties. In general, they have found that borderline patients have a mean DES score of 17.8-27.4. This range is similar to mean scores achieved by late adolescents and eating-disordered patients but substantially lower than mean DES scores achieved by patients meeting criteria for PTSD or dissociative disorders, including dissociative identity disorder (DID) (19-22). It was also found that borderline patients had a significantly higher mean score on the DES than comparison subjects with other forms of personality disorder (16-18). Additionally, it was found that borderline patients had higher mean scores than axis II comparison subjects on the three factors that underlie the DES: absorption, depersonalization, and amnesia (16-18).
The current study is the first study, to the best of our knowledge, to assess the severity of the dissociative experiences of borderline patients and axis II comparison subjects over time. More specifically, the DES was administered at baseline and at five contiguous two-year follow-up periods to a large sample of carefully diagnosed borderline patients and comparison subjects with other forms of personality disorder. Over the ten years of follow-up, retention was high in both study groups.
The study had three aims. The first was to determine the course of the overall severity of dissociation as well as the severity of the three subtypes of dissociation assessed by the DES—absorption, depersonalization, and amnesia —among borderline patients and axis II comparison subjects. The second aim was to examine the overall severity of dissociation over time of borderline patients who had low levels, moderate levels, and high levels of overall dissociation at baseline. The third aim was to examine time to remission and time to recurrence for those borderline patients who had a mean DES score in the high range at baseline. In addition, we assessed time to new onset of a high score for those borderline patients with a mean DES score in the low-moderate range at baseline.
Methods
The current study is part of the McLean Study of Adult Development (MSAD), a multifaceted longitudinal study of the course of borderline personality disorder. The methodology of this study has been described in detail elsewhere (23). Briefly, all subjects were initially inpatients at McLean Hospital in Belmont, Massachusetts. Each patient was screened to determine that he or she: 1) was between the ages of 18-35; 2) had a known or estimated IQ of 71 or higher; 3) had no history or current symptomatology of schizophrenia, schizoaffective disorder, bipolar I disorder, or an organic condition that could cause psychiatric symptoms; and 4) was fluent in English.
After the study procedures were explained, written informed consent was obtained. Each patient then met with a masters-level interviewer blind to the patient’s clinical diagnoses for a thorough diagnostic assessment. Three semistructured interviews were administered: 1) the Structured Clinical Interview for DSM-III-R Axis I Disorders (SCID-I) (24), 2) the Revised Diagnostic Interview for Borderlines (DIB-R) (25), and 3) the Diagnostic Interview for DSM-III-R Personality Disorders (DIPD-R) (26). The inter-rater and test-retest reliability of all three of these measures have been found to be good-excellent (27, 28).
The dissociative experiences of borderline patients were assessed using the DES at each of the study’s six assessment periods (19-22). Each item within the DES is rated according to the percentage of time that the patient has experienced that particular type of dissociative experience. For example, a score of 30 on the depersonalizarion sub-scale of the DES suggests that the patient has spent 30% of his or her waking time struggling with feelings of unreality. The DES has been found to have good test-retest and split-half reliability. It has also been found to have construct and criterion validity. The DES provides an overall score that has been normed in various patient populations. In addition, the DES provides three factor scores that have been found to be internally consistent: absorption, depersonalization, and amnesia. According to guidelines extrapolated from the developers of the DES (19-22), scores of 10 or less are considered to be in the low dissociation range, and scores between 10 and 29.9 are considered to be in the mid-range, similar to the range achieved by late adolescents and eating-disordered patients. Scores of 30 or above are considered to be in the high range, which is consistent with those of individuals meeting criteria for PTSD or DID.
Data obtained from the DES were assembled in panel format (i.e., multiple records per patient, with one record for each follow-up period for which data were available). Random effects regression modeling methods assessing the role of group (BPD vs. OPD; high, moderate, or low baseline DES score among borderline patients), time, and their interaction, and controlling for gender (BPD vs. OPD analyses as there was a between-group difference in gender) were used in analyses of mean DES score data. As total DES and sub-scores were skewed, continuous measures were logarithmically transformed prior to modeling analyses in order to achieve distributions that were more symmetric. Alpha was set at the p<0.05 level, two-tailed.
We defined time-to-remission of a high DES score (30 or higher) as the follow-up period at which remission was first achieved. Thus, possible values for this time-to-remission measure were 2, 4, 6, 8, or 10 years, with time=2 years for persons first achieving a lower DES score during the first follow-up period, time=4 years for persons first achieving a lower DES score during the second follow-up period, etc. We defined time-to-new onset in a like manner. We defined time-to-recurrence in a somewhat different manner (i.e., the number of years after a remission had been achieved that a high DES score first reoccurred). Thus, time-to-recurrences were 2, 4, 6, or 8 years after first remission.
Results
Two hundred and ninety patients met both DIB-R and DSM-III-R criteria for BPD and 72 met DSM-III-R criteria for at least one nonborderline axis II disorder (and neither criteria set for BPD). Of these 72 comparison subjects, 4% met DSM-III-R criteria for an odd cluster personality disorder, 33% met DSM-III-R criteria for an anxious cluster personality disorder, 18% met DSM-III-R criteria for a nonborderline dramatic cluster personality disorder, and 53% met DSM-III-R criteria for personality disorder not otherwise specified (which was operationally defined in the DIPD-R as meeting all but one of the required number of criteria for at least two of the 13 axis II disorders described in DSM-III-R).
Baseline demographic data have been reported before (23). Briefly, 77.1% (N=279) of the subjects were female and 87% (N=315) were white. The average age of the subjects was 27 years (SD=6.3), the mean socioeconomic status was 3.3 (SD=1.5) (where 1=highest and 5=lowest) (29), and their mean GAF score was 39.8 (SD=7.8) (indicating major impairment in several areas, such as work or school, family relations, judgment, thinking, or mood).
In terms of continuing participation, 90.1% (N=309) of surviving patients were reinterviewed at all five follow-up waves. More specifically, 91.5% of surviving borderline patients (249/272) and 84.5% of surviving axis II comparison subjects (60/71) were evaluated six times (baseline and five follow-up periods).
Table 1 details mean total DES scores and mean absorption, depersonalization, and amnesia sub-scores over time for both study groups. As the relative differences for diagnosis and time in the table contain much fine-grained information, we believe that an example would be useful. As can be seen, borderline patients reported a mean total DES score of 21.8 (SD=18.6) at baseline (and axis II comparison subjects reported a mean score of 7.5 [SD=7.9]). By the time of their 10-year follow-up, the mean total DES score reported by borderline patients had declined to 8.5 (SD=12.1) (and that of axis II comparison subjects had declined to 3.9 [SD=5.6]). The relative difference of 2.58 for diagnosis indicates that the mean total DES score reported by borderline patients at baseline is approximately 2½ times larger than the corresponding mean for axis II comparison subjects. The relative difference of 0.57 for time indicates that the relative change from baseline to 10-year follow-up resulted in an approximately 43% (or [1 – 0.57]×100%) decline for axis II comparison subjects. In contrast, the significant interaction between diagnosis and time for the total DES score indicates that the relative decline from baseline to 10-year follow-up is approximately 61% (or [1 – 0.57×0.69]×100%) for borderline patients.
Table 1.
Random Effects Regression Modeling of Mean Scores of Patients with Borderline Personality Disorder and Axis II Comparison Subjects over Ten Years of Prospective Follow-Up
| Mean Score | Borderline Personality Disorder (Mean/Standard Deviation) | Axis II Comparison Subjects (Mean/Standard Deviation) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| BL (N=290) | 2 Yr FU (N=275) | 4 Yr FU (N=269) | 6 Yr FU (N=264) | 8 Yr FU (N=255) | 10 Yr FU (N=249) | BL (N=72) | 2 Yr FU (N=67) | 4Yr FU (N=64) | 6Yr FU (N=63) | 8 Yr FU (N=61) | 10 Yr FU (N=60) | Relative Difference Diagnosis Time Interaction | 95%CI Diagnosis Diagnosis Time Interaction | |
|
| ||||||||||||||
| DES | 21.8 (18.6) | 15.6 (16.5) | 13.0 (14.9) | 10.9 (13.8) | 10.4 (13.6) | 8.5 (12.1) | 7.5 (7.9) | 6.1 (7.8) | 4.4 (5.3) | 4.5 (5.8) | 4.1 (6.4) | 3.9 (5.6) | 2.58 | 2.04, 3.25 |
| .57 | .47, .66 | |||||||||||||
| .69 | .57, .83 | |||||||||||||
|
| ||||||||||||||
| Absorption | 29.2 (21.0) | 21.1 (19.8) | 18.1 (18.2) | 15.1 (16.4) | 13.9 (16.2) | 11.2 (14.4) | 12.3 (11.5) | 9.8 (11.0) | 6.7 (8.3) | 7.1 (8.7) | 5.6 (7.7) | 5.1 (6.6) | 2.44 | 1.92, 3.10 |
| .45 | .37, .55 | |||||||||||||
| .78 | .63, .98 | |||||||||||||
|
| ||||||||||||||
| Depersonalization | 16.9 (21.5) | 12.0 (19.3) | 9.5 (16.9) | 8.1 (16.6) | 8.2 (16.2) | 6.6 (15.1) | 2.0 (4.2) | 2.5 (7.6) | 1.2 (3.5) | 1.2 (3.8) | 0.9 (3.8) | 1.2 (4.2) | 3.36 | 2.46, 4.60 |
| .74 | .59, .93 | |||||||||||||
| .56 | .43, .72 | |||||||||||||
|
| ||||||||||||||
| Amnesia | 13.5 (18.8) | 8.3 (14.8) | 6.6 (13.0) | 5.0 (11.4) | 4.6 (10.7) | 3.6 (8.9) | 3.4 (7.0) | 1.7 (3.8) | 1.9 (4.3) | 1.5 (3.7) | 1.8 (5.8) | 1.4 (4.0) | 2.54 | 1.94, 3.31 |
| .68 | .55, .84 | |||||||||||||
| .56 | .44, .71 | |||||||||||||
P-values for diagnosis were all <0.001. P-values for time were all <0.001, except for depersonalization (0.011). P-values for interaction terms were all <0.001, except for absorption (0.031).
For all four analyses, gender was included as a model covariate.
As for the three sub-scale scores, the relative differences of 2.44, 3.36, and 2.54 for diagnosis indicate that the mean absorption, depersonalization, and amnesia scores reported by borderline patients at baseline were approximately 2½, 3, and 2½ times larger than the corresponding means for axis II comparison subjects. The relative differences of 0.45, .74, and .68 for time indicate that the relative change from baseline to 10-year follow-up resulted in an approximately 55%, 26%, and 32% decline among axis II comparison subjects for absorption, depersonalization, and amnesia respectively. In contrast, the significant interactions between diagnosis and time for the three sub-scale scores indicate that the relative decline from baseline to 10-year follow-up is approximately 65% (absorption), 59% (depersonalization), and 62% (amnesia) for borderline patients.
Figure 1 details the mean total DES scores of three sub-groups of borderline patients defined by their baseline mean total DES score. Those in the high (N=76) and moderate (N=122) baseline DES groups had a significantly faster rate of decline than those in the low DES group (N=92) (χ2 =80.4, df=2, p<0.001). It was also found that those in the high DES group had a significantly faster rate of decline than those in the moderate group (χ2 =4.6, df=1, p=0.0325). However, those in all three groups experienced a significant decline in mean total DES score from baseline to 10-year follow-up (with relative decline of 73% in the high group: χ2 =249.2, df=1, p<0.001; 66% in the moderate group: χ2 =306.2, df=1, p<0.001; 38% in the low group: χ2 =60.9, df=1, p<0.001).
Figure 1. Mean DES Scores (and standard errors) Attained by Baseline Groups of Bordeline Patients over Ten Years of Prospective Follow-up.
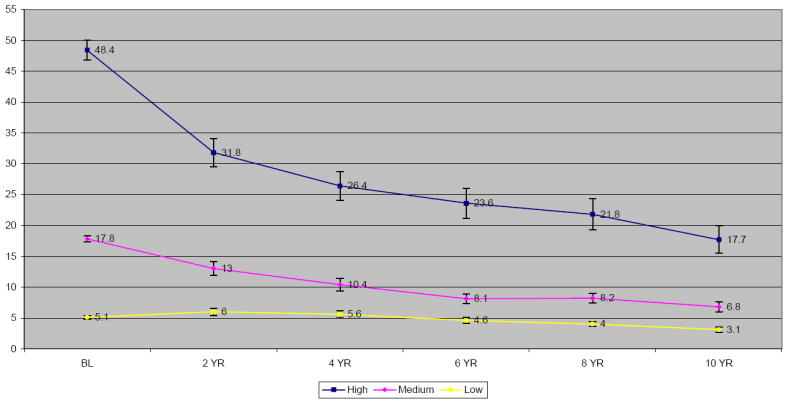
Ns for high DES group: 76, 72, 70, 68, 66, and 66; Ns for moderate group: 122, 114, 111, 109, 107, and 103; Ns for low group: 92, 89, 88, 87, 82, and 80.
Figure 2 details the rates of remission and recurrence of a mean DES score in the high range for the 76 borderline patients who scored in this range at baseline. As can be seen, over 90% of borderline patients reporting very high levels of dissociation at baseline experienced a remission of this high level of dissociation over time. However, slightly more than a third of borderline patients who experienced a remission later experienced a recurrence of severe dissociative symptoms. As for the 214 borderline patients who had a mean DES score in the low or moderate range at baseline, about 8% experienced a new onset of severe dissociative symptoms over the 10 years of prospective follow-up. (These analyses were limited to borderline patients as only two (2.8%) of axis II comparison subjects had mean DES scores of 30 or more at baseline, both had a remission, neither had a recurrence, and only one additional comparison subject had a new onset.)
Figure 2. Rates of Remission, Recurrence, and New Onsets of High DES Scores (30 or more) among Borderline Patients over Ten Years of Prospective Follow-up.
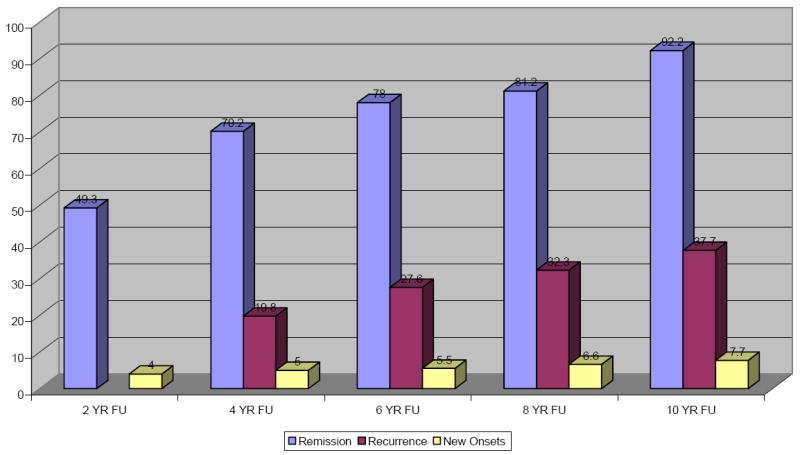
Note: Since a recurrence can only occur after a remission, there is no possibility of a recurrence occurring at the 2-year follow-up. Even though recurrences are displayed in this figure at the 4, 6, 8, and 10-year follow-up periods, these recurrences are actually occurring 2, 4, 6, and 8 years after the remission. All told, 61 borderline patients of the 76 who had a high DES score at baseline experienced a remission and 18 of those who remitted experienced a recurrence. Of the 214 with a low-moderate baseline score, 14 experienced a new onset of a high DES score.
Discussion
Two main findings have emerged from this study. The first is that the overall severity of dissociative experiences as assessed by the DES declined significantly over time for both borderline patients (61% relative decrease) and axis II comparison subjects (43% relative decrease). Similar declines were reported for both groups for the three main components of dissociation as assessed by the DES: absorption (65% vs. 55%), depersonalization (59% vs. 26%), and amnesia (62% vs. 32%). Taken together, this set of findings suggests that all types of dissociative experiences decline in severity for borderline patients (and axis II comparison subjects). However, these declines were significantly greater for borderline patients than axis II comparison subjects.
The second main finding is that borderline patients with high levels of dissociation at baseline were found to have less severe symptoms over time. This was so whether dissociation was studied as a continuous variable or as a series of categorical variables: time-to-remission of severe dissociation, time-to-recurrence, and time-to-new onset. In fact, these categorical variables suggest that even the most severely dissociated borderline patients are likely to report a clinically meaningful decline in the severity of their dissociation over time. These results also suggest that these declines are stable for two-thirds of those achieving a remission. In addition, they suggest that new occurrences of severe dissociation are quite rare. Taken together, these findings provide hope to both borderline patients suffering from serious dissociation and those treating them. In time, the suffering and disability associated with serious dissociation will decrease substantially for most and this lessening of severity will tend to be stable.
A caveat of comparing three levels of severity of dissociation over time is that those with more extreme scores (either particularly high or low) at baseline are expected to have less extreme scores at follow-up due to the statistical phenomena of regression to the mean. However, the fact that those with low scores did not increase over time indicates that the regression effect is likely modest for these data.
A limitation of this study is that all of the patients were seriously ill inpatients at the start of the study. Another limitation is that about 90% of those in both patient groups were in individual therapy and taking psychotropic medications at baseline and about 70% were participating in each of these outpatient modalities during each follow-up period (30). Thus, it is difficult to know if these results would generalize to a less disturbed group of patients or people meeting criteria for BPD who are not in treatment.
It is also unclear if the decline of dissociative experiences can be attributed to treatment, the passage of time, the support offered by family and friends, or some combination of these factors. Further research is needed to determine the reason or reasons for the substantial decline in dissociative symptomatology reported by even the most disturbed borderline patients.
Future research is also needed to determine the longitudinal relationship between dissociative experiences and other symptoms of BPD, such as episodes of self-mutilation, that have been found to have a cross-sectional relationship (14). Finally, further research of a longitudinal nature is needed to determine if the dissociative experiences of borderline patients are stress related in nature or more chronic (31).
Significant Outcomes.
92% of those borderline patients with a high DES score (30 or higher) at baseline had a remission of their severe dissociation during the10 years of follow-up.
38% of the borderline patients who had such a remission had a recurrence of a high DES score.
Only a low 8% of those with lower scores at baseline had a new onset of high levels of dissociation over the years of follow-up.
High levels of dissociation were rare at baseline among axis II comparison subjects and only emerged for one subject over time.
Limitations.
All subjects were initially inpatients and thus, the results of this study may not apply to less seriously ill outpatients.
The majority of the sample was in treatment and thus, the results may not generalize to untreated subjects.
The naturalistic design of the study makes it impossible to determine if the observed changes were due to treatment, the passage of time, the support offered by family and friends, or some admixture of the three.
Acknowledgments
This study was supported by NIMH grants MH47588 and MH62169.
References
- 1.Gunderson JG, Singer MT. Defining borderline patients: an overview. Am J Psychiatry. 1975;132:1–10. doi: 10.1176/ajp.132.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Chopra HD, Beatson JA. Psychotic symptoms in borderline personality disorder. Am J Psychiatry. 1986;143:1605–1607. doi: 10.1176/ajp.143.12.1605. [DOI] [PubMed] [Google Scholar]
- 3.Conte HR, Plutchik R, Karasu TB, Jerrett I. A self-report borderline scale: discriminative validity and preliminary norms. J Nerv Ment Dis. 1980;168:428–435. doi: 10.1097/00005053-198007000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Gunderson JG. In: Characteristics of borderlines, In Borderline Personality Disorders. Hartocollis P, editor. New York: International Universities Press; 1977. pp. 173–192. [Google Scholar]
- 5.Gunderson JG, Carpenter WT, Strauss JS. Borderline and schizophrenic patients: a comparative study. Am J Psychiatry. 1975;132:1257–1264. doi: 10.1176/ajp.132.12.1257. [DOI] [PubMed] [Google Scholar]
- 6.Koenigsberg HW. A comparison of hospitalized and nonhospitalized borderline patients. Am J Psychiatry. 1982;139:1292–1297. doi: 10.1176/ajp.139.10.1292. [DOI] [PubMed] [Google Scholar]
- 7.Links PS, Steiner M, Mitton J. Characteristics of psychosis in borderline personality disorder. Psychopathology. 1989;22:188–193. doi: 10.1159/000284595. [DOI] [PubMed] [Google Scholar]
- 8.Nurnberg HG, Hurt SW, Feldman A, Suh R. Evaluation of diagnostic criteria for borderline personality disorder. Am J Psychiatry. 1988;145:1280–1284. doi: 10.1176/ajp.145.10.1280. [DOI] [PubMed] [Google Scholar]
- 9.Perry JC, Klerman GL. Clinical features of the borderline personality disorder. Am J Psychiatry. 1980;137:165–173. doi: 10.1176/ajp.137.2.165. [DOI] [PubMed] [Google Scholar]
- 10.Sheehy M, Goldsmith L, Charles E. A comparative study of borderline patients in a psychiatric outpatient clinic. Am J Psychiatry. 1980;137:1374–1379. doi: 10.1176/ajp.137.11.1374. [DOI] [PubMed] [Google Scholar]
- 11.Silk KR, Lohr NE, Western D, Goodrich S. Psychosis in borderline patients with depression. J Personal Disord. 1989;3:92–100. [Google Scholar]
- 12.Soloff PH. A comparison of borderline with depressed and schizophrenic patients on a new diagnostic interview. Compr Psychiatry. 1981;22:291–300. doi: 10.1016/0010-440x(81)90087-0. [DOI] [PubMed] [Google Scholar]
- 13.Zanarini MC, Gunderson JG, Frankenburg FR. Cognitive features of borderline personality disorder. Am J Psychiatry. 1990;147:57–63. doi: 10.1176/ajp.147.1.57. [DOI] [PubMed] [Google Scholar]
- 14.Brodsky BS, Cloitre M, Dulit RA. Relationship of dissociation to self-mutilation and childhood abuse in borderline personality disorder. Am J Psychiatry. 1995;152:1788–1792. doi: 10.1176/ajp.152.12.1788. [DOI] [PubMed] [Google Scholar]
- 15.Shearer SL. Dissociative phenomena in women with borderline personality disorder. Am J Psychiatry. 1994;151:1324–1328. doi: 10.1176/ajp.151.9.1324. [DOI] [PubMed] [Google Scholar]
- 16.Zanarini MC, Ruser T, Frankenburg FR, Hennen JH. The dissociative experiences of borderline patients. Compr Psychiatry. 2000;41:223–227. doi: 10.1016/S0010-440X(00)90051-8. [DOI] [PubMed] [Google Scholar]
- 17.Zweig-Frank H, Paris J, Guzder J. Dissociation in female patients with borderline and non-borderline personality disorders. J Personal Disord. 1994;8:203–209. [Google Scholar]
- 18.Zweig-Frank H, Paris J, Guzder J. Dissociation in male patients with borderline and non-borderline personality disorders. J Personal Disord. 1994;8:210–218. [Google Scholar]
- 19.Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174:727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Bernstein EB, Putnam FW. An update on the dissociative experiences scale. Dissociation. 1993;6:16–27. [Google Scholar]
- 21.Putnam FW, Carlson EB, Ross CA, Anderson G, Clark P, Torem M, Bowman ES, Coons P, Chu JA, Dill DL, Lowenstein RJ, Braun BG. Patterns of dissociation in clinical and nonclinical samples. J Nerv Ment Dis. 1996;184:673–679. doi: 10.1097/00005053-199611000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Bernstein EB, Putnam FW, Ross CA, Torem M, Coons P, Dill DL, Loewenstein RJ, Braun BG. Validity of the Dissociative Experiences Scale in screening for multiple personality disorder: a multicenter study. Am J Psychiatry. 1993;150:1030–1036. doi: 10.1176/ajp.150.7.1030. [DOI] [PubMed] [Google Scholar]
- 23.Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry. 2003;160:274–283. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- 24.Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R (SCID) I: history, rational, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 25.Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The Revised Diagnostic Interview for Borderlines: discriminating BPD from other Axis II disorders. J Personal Disord. 1989;3:10–18. [Google Scholar]
- 26.Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG. The Diagnostic Interview for Personality Disorders: inter-rater and test-retest reliability. Compr Psychiatry. 1987;28:467–480. doi: 10.1016/0010-440x(87)90012-5. [DOI] [PubMed] [Google Scholar]
- 27.Zanarini MC, Frankenburg FR, Vujanovic AA. The inter-rater and test-retest reliability of the Revised Diagnostic Interview for Borderlines (DIB-R) J Personal Disord. 2002;16:270–276. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- 28.Zanarini MC, Frankenburg FR. Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Compr Psychiatry. 2001;42:369–374. doi: 10.1053/comp.2001.24556. [DOI] [PubMed] [Google Scholar]
- 29.Hollingshead AB. Two factor index of social position. New Haven, CT: Yale University; 1957. [Google Scholar]
- 30.Zanarini MC, Frankenburg FR, Hennen J, Silk KR. Mental health service utilization of borderline patients and axis II comparison subjects followed prospectively for six years. J Clin Psychiatry. 2004;65:28–36. doi: 10.4088/jcp.v65n0105. [DOI] [PubMed] [Google Scholar]
- 31.Stiglmayr CE, Ebner-Priemer UW, Bretz J, Behm R, Mohse M, Lammers CH, Anghelescu IG, Schmahl C, Schlotz W, Kleindienst N, Bohus M. Dissociative symptoms are positively related to stress in borderline personality disorder. Acta Psychiatr Scand. 2008;117:139–147. doi: 10.1111/j.1600-0447.2007.01126.x. [DOI] [PubMed] [Google Scholar]


