Abstract
The aim of this meta-analysis was to summarise data from neuropsychological studies on inhibitory control to general and disease-salient (i.e., food/eating, body/shape) stimuli in bulimic-type eating disorders (EDs). A systematic literature search was conducted to identify eligible experimental studies. The outcome measures studied included the performance on established inhibitory control tasks in bulimic-type EDs. Effect sizes (Hedges' g) were pooled using random-effects models. For inhibitory control to general stimuli, 24 studies were included with a total of 563 bulimic-type ED patients: 439 had bulimia nervosa (BN), 42 had anorexia nervosa of the binge/purge subtype (AN-b), and 82 had binge eating disorder (BED). With respect to inhibitory control to disease-salient stimuli, 12 studies were included, representing a total of 218 BN patients. A meta-analysis of these studies showed decreased inhibitory control to general stimuli in bulimic-type EDs (g = −0.32). Subgroup analysis revealed impairments with a large effect in the AN-b group (g = −0.91), impairments with a small effect in the BN group (g = −0.26), and a non-significant effect in the BED group (g = −0.16). Greater impairments in inhibitory control were observed in BN patients when confronted with disease-salient stimuli (food/eating: g = −0.67; body/shape: g = −0.61). In conclusion, bulimic-type EDs showed impairments in inhibitory control to general stimuli with a small effect size. There was a significantly larger impairment in inhibitory control to disease salient stimuli observed in BN patients, constituting a medium effect size.
Introduction
The spectrum of bulimic-type eating disorders (EDs) includes anorexia nervosa of the binge/purge subtype (AN-b), bulimia nervosa (BN), and binge eating disorder (BED). These conditions share the common characteristic of recurrent episodes of binge eating (i.e., overeating of large amounts of food) with (AN-b and BN) or without (BED) compensatory behaviours, e.g., self-induced vomiting. Binge eating is associated with a ‘definite sense of loss of control’ [1]. Although the bulimic-type EDs are mental disorders associated with increased morbidity and all-cause mortality [2], [3], the mechanisms underlying bulimic behaviours are largely unknown.
In addition to the categorical classification of EDs, in recent years and with the upcoming fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a renewed interest in dimensional concepts and trans-diagnostic theories in EDs (AN, BN, BED) can be observed [4]–[6]. Recurrent episodes of binge eating are considered to be a common phenomenon in purging spectrum disorders and are evident in various ED pathologies, including AN (binge/purge subtype), BN and BED. Furthermore, impaired inhibitory control in bulimic-type ED patients does not appear to be restricted to food intake but may extend to general behaviours, e.g., excessive drinking, substance abuse, sexual disinhibition, and bullying, suggesting a more general dysregulation of inhibitory control in bulimic-type EDs [7], [8].
Neurocognitive tasks have been developed to investigate inhibitory control in and across different psychopathologies. However, there is a lack of systematic evidence from neuropsychological studies assessing and comparing inhibitory control capacities across different ED diagnoses. Because studies using subjective ratings of impulse control capacities and neuropsychological data generally fail to show strong associations (e.g., [9]–[11]), the assessment of inhibitory control with more objective and well-defined behavioural and cognitive tasks is of great importance.
Inhibition is a broad term that describes a wealth of phenomena. The present review is concerned with voluntary inhibition, as a subcomponent of cognitive control functions. Inhibitory control refers to the ability to suppress, interrupt, or delay an activated behaviour or cognitive course of action [12]–[15]. Inhibitory control is not a unitary construct, but consists of several subcomponents. These share a common underlying neural network but the degree of regional involvement seem to differ between the subcomponents [16]. A more basic distinction may exist between inhibitory mechanisms that control overt behaviors (i.e., behavioural inhibition) and those that control mental and attentional processes (i.e. cognitive inhibition). Based on the review of Bari et al. [16], the concept of behavioural inhibition encompasses the subdivision of response inhibition, reversal learning and delayed gratification. In the present meta-analysis, we limit our analysis to response inhibition and disinhibition, as reversal learning and delayed gratification depend on several additional factors (i.e. set-shifting, learning, reward sensitivity, decision making) for successful performance. Furthermore, compulsivity and reversal learning have been addressed in previous meta-analysis of ED patients (e.g., [17]). The concept of cognitive inhibition instead encompasses cognitive and attentional processes such as when during attentional processing task-irrelevant information has to be suppressed (i.e., interference control) [13].
Response inhibition tasks have been most commonly used in ED studies to investigate inhibitory control (behavioral inhibition). The most prominent examples are the No-go task [18] and the Stop Signal Task [12], which measures an overt, effortful expression of inhibitory control involving the suppression of an activated behavioural response [13]. In the classical No-go task, participants must respond to a frequently presented target and to inhibit their responses to an infrequently presented non-target [19]. The SST differs from the No-go task in that participants must inhibit an already initiated motor response [12]. The number of inhibitory control failures (e.g., failure to stop a pre-potent response when required during the No-go task) or the speed of the inhibitory process (i.e., the stop signal reaction time for the SST) is typically the main outcome measure.
Cognitive inhibition was investigated in ED patients with interference control tasks. These require effortful inhibitory control at a covert cognitive level to suppress the competing automatic response in favour of an alternative response [13]. The most prominent representative of these interference control tasks is the Stroop task. The classical Stroop task elicits a conflict between automatically reading the colour word and naming the incongruent colour of the ink (e.g., the word ‘blue’ is written in green ink colour). Furthermore, modified versions of the Stroop task have been used in ED patients to assess interference control to disease-salient stimuli [20]. Furthermore, the Simon task, which is based on the Simon spatial incompatibility effect (i.e., reaction times are faster and more accurate when the source of stimulation is in the same relative location as the response), also belongs to the group of interference control measures and has been employed in previous studies with bulimic-type ED patients [21], [22].
Other inhibitory control tasks have also been used in previous ED studies to assess primarily response disinhibition. Examples include the Hayling Sentence Completion Test (HSCT), Excluded Letter Fluency task (ELF), and Matching Familiar Figures Test (MFFT) (for further details of these tasks see study concerning [23]).
Previous studies on inhibitory control have reported ambiguous findings with respect to inhibitory control in bulimic-type EDs. Several studies have used the No-go task to assess inhibitory control in bulimic-type EDs [18], [24]–[28]. However, only two of them have reported impaired inhibitory control: one in BN patients (subgroup of BN patients with laxative misuse) [24] and the other in AN-b patients [18]. For the SST, three reports were found, and each included two subtypes of bulimic-type EDs ([9]: in AN-b and BN; [29]: in AN-b and BN; [11]: in BN and BED). However, only one of these studies found significant group differences between BN patients and controls [11], and another reported impairments in AN-b patients [29]. With respect to interference control, the Stroop task has been used most commonly, with inconsistent findings in bulimic-type EDs [28], [30]–[32]. Thus, despite the clinical features and evidence from self- report measures, the current findings from neurocognitive tasks are ambiguous and have not been able to clearly demonstrate impaired inhibitory control in bulimic-type EDs. Furthermore, previous independent studies have frequently used very small sample sizes without reporting effect sizes (ESs). Therefore, it remains unclear whether and to what extent inhibitory control impairment exists in bulimic-type EDs.
Several authors have summarised neurocognitive findings noted in EDs. However, these reviews a) have not conducted meta-analyses to estimate ESs [33], [34]; b) have not included the complete spectrum of bulimic-type EDs [20], [35], [36]; c) have combined currently ill and recovered ED patients [20], [35]; d) have not differentiated between AN-b and AN of the restricting subtype (AN-r) [35], [36]; and e) have only focused on a single type of inhibitory control measure [20], [35].
The aim of the present review with meta-analysis was to summarise the current evidence from multiple neuropsychological studies across the complete spectrum of bulimic-type EDs and across different task categories of inhibitory control to estimate the ES of impaired inhibitory control in patients with binge eating. More specifically, the following questions have been addressed: a) Do bulimic-type EDs (compared to controls) show poorer performance in neurocognitive tasks that address inhibitory control function? b) If so, is this impairment specific to neurocognitive mechanisms of response inhibition (behavioral inhibition) or interference control (cognitive inhibition)? c) Is impaired inhibitory control in bulimic-type EDs greater for disease-salient stimuli (e.g., food) or independent of the type of stimuli? d) Do the effect sizes of impaired inhibitory control differ within the spectrum of bulimic-type ED diagnoses?
Materials and Methods
Search strategy and study selection
We searched for published experimental studies on inhibitory control using the following electronic databases: PubMed, PsycINFO, PSYNDEX, and Web of Science. In addition, the reference lists of relevant articles were carefully searched.
The search strategy was based on the following keyword terms: impulsive, impulsivity, inhibitory control, inhibition, disinhibition, attention, executive function, motor control, cognitive control, reward, decision making, neurocognitive, neurocognition, neuropsychology, eating disorder, bulimia nervosa, binge eating disorder, anorexia nervosa, binge/purge, binge eating, purging disorder, and obesity. Searches were limited to human studies, including adults and adolescents of both genders. No date restrictions were applied to the selection of literature, and articles were searched up to March 2013. In addition, we reviewed all studies included in previously published meta-analyses or systematic reviews.
The retrieved titles and abstracts from the literature search were screened for relevance independently by two of the authors (MW, HCF). For every abstract that was identified as potentially relevant by at least one of the two review authors, the full text article was retrieved for evaluation by both reviewers independently. Discrepancies were resolved by discussion. The classification of tasks as inhibitory control measures was based on the information provided in the publications and through discussion among all the authors.
Studies were considered to be acceptable and comparable if they met the following eligibility criteria for inclusion: a) studies had to compare at least one clinical ED group to a healthy control group; b) patients included in the study had to fulfil diagnostic criteria based on the DSM-III, DSM-IV or ICD-10, and results had to be differentiated for current AN of the binge/purge subtype, current BN or current BED; c) studies had to include a detailed description of sociodemographic variables from the healthy control group; d) studies had to include at least one neurocognitive task that investigated inhibitory control; and e) studies had to include sufficient statistical information to allow for the calculations of ESs.
Data extraction and quality assessment
For data extraction (study characteristics, study results and quality assessment), we used a standardised form developed prior to the search. All discrepancies were rechecked, and disagreements were resolved by discussion with the other authors. Descriptive statistics (means, standard deviations and sample sizes) for the main outcome measures of relevant tasks in bulimic-type ED patients and healthy controls were extracted for the calculation of ESs. When articles did not report means and/or standard deviations, p values and sample sizes were used to calculate ESs.
Because no standardized criteria have been established to assess the quality of neuropsychological studies, we developed a priori a standardized checklist of risk of bias which was based on domains of the Newcastle-Ottawa Scale (NOS: www.ohri.ca/programs/clinical_epidemiology/oxford.htm) for evaluating risk of bias in case- control and cohort studies. The NOS consists of the three sub-domains ‘selection of subjects’, ‘comparability of subjects’ and ‘ascertainment of outcome’. We developed for each domain three to four quality items (e.g., inclusion/exclusion criteria, comparability of samples regarding diagnoses, age, educational level, and adequacy of outcome analysis). Each included study was assessed using this ten-item checklist where items were answered either as ‘quality criterion fulfilled (1)’ or as ‘not fulfilled (2)’. Ratings were summed-up to a total score with a maximum value of 10. Quality levels of evidence for each study were defined as high (> = 8), medium (6–8), and low ( = <5). Any discrepancies in quality assessment between the two authors (MW and HCF) were resolved by a third author (MH) who served as an arbiter.
Quantitative data synthesis
We classified reported outcomes into two categories: a) inhibitory control to general stimuli and b) inhibitory control to disease-salient stimuli (i.e., food/eating and weight/shape stimuli). For articles that included different subtypes of bulimic-type EDs (e.g., AN-b and BN), ESs were calculated separately for each patient group and were treated as separate studies (marked as ‘a’, ‘b’, etc). Separate ESs were calculated for the main outcome of every inhibitory control task in all studies. For studies using more than one neurocognitive measure of inhibitory control [23], [28], a mean ES was computed by averaging ESs across all measures within one study and was included in the calculation of the overall ES.
The ES was calculated as Hedges' g (a variation of Cohen's d that corrects for biases due to small sample sizes) and reported this value with its 95% confidence interval (CI95). The magnitude of Hedges' g was interpreted using Cohen's recommendations for small (>0.2), medium (>0.5) and large (>0.8) effect size. A negative ES indicates poorer inhibitory control in patients than in controls. Given the variety of neurocognitive tasks and outcomes, we used the more conservative random-effects model rather than a fixed-effect model to estimate a pooled ES. Heterogeneity among the studies was assessed using the Q test. In addition, the I2 statistic values were reported [I2 = (Q−df)/Q]. As a sample-size independent measure of the inconsistency of ESs across studies, I2 is more powerful with small sample sizes when compared to Cochran's Q test. I2>50% indicates medium heterogeneity, and I2>75% indicates large heterogeneity [37].
Small study effects as an indication of publication bias were assessed informally by visual inspection of the funnel plot (a plot of effect estimates against its standard error) and using the Egger's test [38].
All analyses were calculated using the software package ‘Comprehensive Meta-Analysis’ (version 2: www.Meta-Analysis.com).
Moderator analysis and sensitivity analysis
Subgroup analyses of the subtypes of bulimic-type EDs (i.e., AN-b, BN, and BED) and types of inhibitory control measures (e.g., Stroop, No-go, SST) were conducted to identify potential moderators that could explain potential sources of heterogeneity between studies. In addition, sensitivity analyses were conducted to explore the influence of study quality on the pooled overall ES.
Results
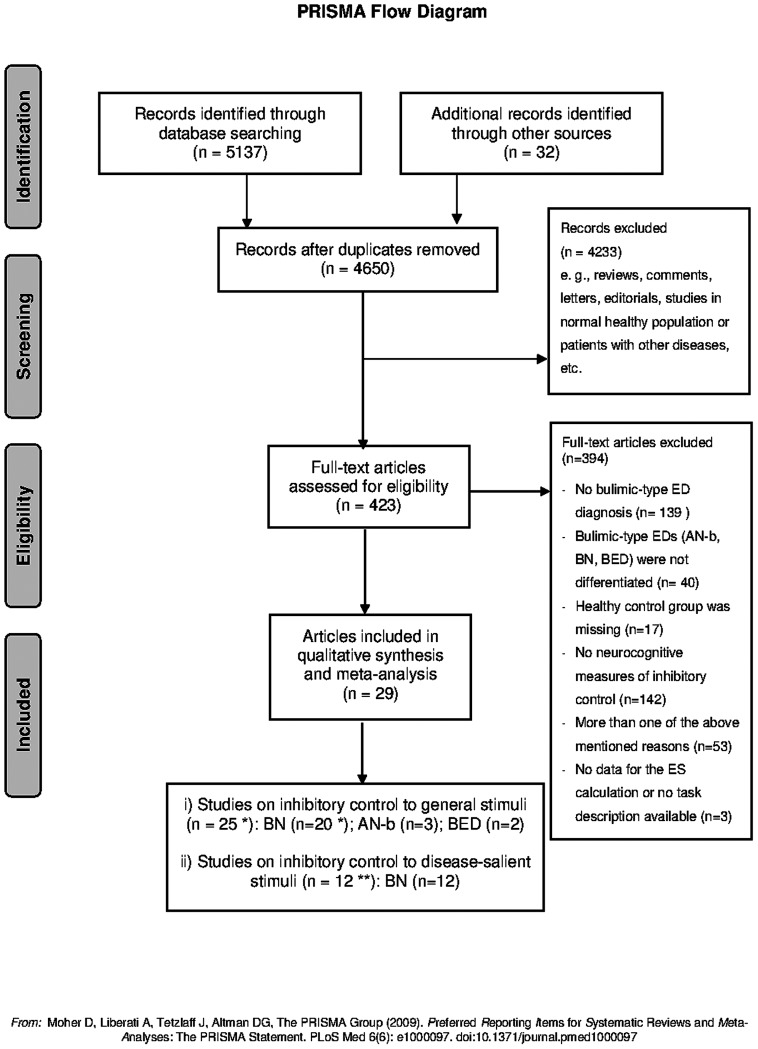
The ‘PRISMA statement’ [39] for reporting a systematic review and meta-analyses was followed (see: Checklist S1 for PRISMA items). This PRISMA Flow chart highlights the number of articles found at each stage of the search and the final number of studies that were included in the review (see Figure 1).
Figure 1. PRISMA Flow Chart.
The flow chart highlights the number of articles found at each stage of the search and the final number of studies that were included in the review; *: the number of studies includes one outlier study; **: four articles reported data for inhibitory control to general stimuli and disease-salient stimuli.
Our search resulted in 4650 potentially eligible articles after the exclusion of duplicates. A total of 423 articles appeared to be potentially relevant and were retrieved as full text manuscripts. Of these, 394 articles were excluded because they did not fulfill the inclusion criteria. The reasons for exclusion were as follows: no bulimic-type ED diagnoses (n = 139), no differentiation of subtypes of bulimic-type EDs (n = 40), no healthy control group (n = 17), no neurocognitive tasks or neurocognitive tasks that addressed other cognitive domains (n = 142), or more than one of the above mentioned reasons (n = 53). In addition, three articles were excluded from the meta-analysis due to a) the lack of appropriate data available for the calculation of ESs [25], [40] or b) insufficient information about neurocognitive task and analysis methods [26]. The qualitative synthesis and meta-analysis were based on the remaining 29 articles that addressed inhibitory control to general and disease-salient stimuli.
Inhibitory control to general stimuli
Study characteristics
Overall, 21 articles, which consisted of 25 studies conducted among bulimic-type ED patients (total of patients: n = 583), were included in the meta-analysis. The mean quality score of all included studies was 7.0. The characteristics of the study sample are shown in Table 1.
Table 1. Description of studies on general inhibitory control in bulimic-type eating disorders.
| Study | Subject | Female (percentage) | Age (years) mean (SD) | BMI (kg/m2) mean (SD) | Educational level | Co-morbidity/Treatment/Medication | Task/Outcome variable | Findings | Qualityscore (x/10) |
| Alvarez-Moya et al. 2009 | BN (15) | 100% | 33.6 (8.8) | 26.3 (6) | ns | NO/YES/YES | Stroop/colour-word interference index | ns | 7 |
| HC (15) | 100% | 35.5 (13.8) | NR | ||||||
| Ben-Tovim et al. 1989 | BN(19) | 100% | 26.9 (10) | 22.61 (4.7) | NR | NR/YES/NR | Stroop/colour-word interference index | ns | 6 |
| HC (38) | 100% | 22.8 (4.5) | 21.31 (2.5) | ||||||
| Ben-Tovim et al. 1991 | BN (27) | NR | 26.8 (9.1)* | 23.3 (4.6)* | NR | NR/YES/NR | Stroop/colour-word interference index | ns | 4 |
| HC-h (29) | 100% | 13.6 (1.1) | 21.8 (5.7) | ||||||
| HC-l (37) | 100% | 14.0 (1.3) | 19.7 (3.5)* | ||||||
| Black et al. 1997 | BN (16) | 100% | 23.8 (NR) | 23 (NR) | NR | NR/NO/NR | Stroop/colour-word time | ns | 6 |
| HC (29) | 100% | 21.2 (NR) | 22.6 (NR) | ||||||
| Brand et al. 2007 | BN (14) | 100% | 21.9 (3.3) | 21.6 (3.8) | ns | NO/NO/NO | Stroop/colour-word interference index | ns | 9 |
| HC (14) | 100% | 21.6 (2.9) | 21.3 (2.3) | ||||||
| Bruce et al. 2003 (a) | BN (12) | 100% | 25.6 (5.9) | 21.7 (2.3) | NR | YES/YES/NR | No-go/commission errors | BN≠HC* | 5 |
| HC (25) | 100% | 24.6 (7.1) | 22.0 (1.9) | ||||||
| Bruce et al. 2003 (b) | BN (33) | 100% | 24.5 (6.7) | 22.1 (3.2) | NR | YES/YES/NR | No-go/commission errors | ns | 5 |
| HC (25) | 100% | 24.6 (7.1) | 22.0 (1.9) | ||||||
| Claes et al. 2006 (a) | AN-b (14) | 100% | 21.7 (6.8) | NR | NR | NR/YES/NR | Stop signal/SSRT | ns | 5 |
| HC (83) | 100% | 20.1 (3.1) | NR | ||||||
| Claes et al. 2006 (b) | BN (22) | 100% | 22.7 (5.8) | NR | NR | NR/YES/NR | Stop signal/SSRT | ns | 5 |
| HC (83) | 100% | 20.1 (3.1) | NR | ||||||
| Cooper et al. 1992 | BN (36) | 100% | 24.3 (6.2) | 21.8 (2.2) | NR | NR/YES/NR | Stroop/colour-word interference index | ns | 6 |
| HC (18) | 100% | 22.1 (3.5) | 20.9 (1.5) | ||||||
| Darcy et al. 2012 | BN (23) | 100% | 16.3(1.2) | 109.1(18.2) # | BN<HC* | YES/NR/YES | Stroop/color-word interference index | ns | 7 |
| HC (22) | 100% | 15.4(1.9) | 105.7(12.8) # | ||||||
| Davidson et al. 2002 | BN (17) | 100% | 25.5 (6.4) | 21.2 (3.2) | NR | NR/YES/NR | Stroop/colour-word interference index | ns | 6 |
| HC (18) | 100% | 24.9 (6.1) | 21.1 (2) | ||||||
| Duchesne et al. 2010 | BED (38) | 76.3% | 33.3 (5.0) | 35.9 (2.9) | ns | YES/YES/NO | Stroop/colour-word time | ns | 7 |
| HC (38) | 89.5% | 35.4 (7.9) | 36.6 (3.8) | ||||||
| Fairburn et al. 1991 | BN (24) | 100% | 21.3 (3.8) | 22.6 (3.1) | NR | NR/NR/NR | Stroop/colour-word interference index | BN≠HC* | 6 |
| HC (50) | 100% | 20.0 (1.1) | 20.9 (1.6) | ||||||
| Galimberti et al. 2012 (a) | AN-b (12) | 100% | 27.1 (8.9) | 15.1 (1.6)* | ns | NO/YES/YES | Stop signal/SSRT | AN-b≠HC* | 7 |
| HC (29) | 100% | 26.0 (8.4) | 19.2 (1.6) | ||||||
| Galimberti et al. 2012 (b) | BN (16) | 100% | 25.3 (5.8) | 20.4 (3.7) | ns | NO/YES/YES | Stop signal/SSRT | ns | 8 |
| HC (29) | 100% | 26.0 (8.4) | 19.2(1.6) | ||||||
| Kemps et al. 2010 | BN (13) | 100% | 22.2 (3.9) | 23.6 (2.6) | ns | NO/YES/YES | Stroop/colour-word interference index | BN≠HC* | 9 |
| HC (13) | 100% | 20.8 (3.4) | 22.4 (3.4) | HSCT/total score | BN≠HC* | ||||
| ELF/total score | BN≠HC* | ||||||||
| MFFT/impulsivity score | BN≠HC* | ||||||||
| Marsh et al. 2009 | BN (20) | 100% | 25.7 (7.0) | 22.9 (2.3) | ns | NO/YES/YES | SSIT/RT interference | BN≠HC* | 8 |
| (outlier) | HC (20) | 100% | 26.4 (5.7) | 22.2 (2.2) | |||||
| Marsh et al. 2011 | BN (18) | 100% | 18.4 (2.1) | 22.0 (2.0) | ns | YES/NO/YES | SSIT/RT interference | ns | 7 |
| HC (18) | 100% | 17.3 (2.4) | 22.0 (1.9) | ||||||
| Rosval et al. 2006 (a) | AN-b (16) | 100% | 25.6 (7.7) | 16.7 (1.7)* | NR | NR/YES/NR | No-go/commission errors | AN-b≠HC* | 5 |
| HC (58) | 100% | 24.3 (6.2) | 21.9 (2.2) | ||||||
| Rosval et al. 2006 (b) | BN (65) | 100% | 25.0 (6.4) | 21.3 (1.9) | NR | NR/YES/NR | No-go/commission errors | ns | 6 |
| HC (58) | 100% | 24.3 (6.2) | 21.9 (2.2) | ||||||
| Southgate et al. 2008 | BN (14) | 100% | 25.7 (4.9) | 21.1 (6.7) | ns | NO/YES/NO | MFFT/impulsivity score | ns | 8 |
| HC (26) | 100% | 27.3 (11.5) | 22.0 (3.4) | ||||||
| Van den Eynde et al. 2012 | BN (40) | 100% | 28.3 (8.1) * | 25.2 (7.2) * | BN≠HC * | NR/YES/YES | Stroop/colour-word interference index | ns | 6 |
| HC (65) | 100% | 24.0 (2.6) | 22.2 (3.3) | No-go/commission errors | ns | ||||
| Wu et al. 2013 (a) | BN (16) | 93.8% | 27.1 (10.2) | 22.2 (2.9) | ns | YES/YES/YES | Stop signal/SSRT | BN≠HC* | 8 |
| HC (25) | 96.0% | 26.3 (5.4) | 22.1(2.0) | ||||||
| Wu et al. 2013 (b) | BED (44) | 90.9% | 40.1 (11.6) | 34.0 (5.0) | BED≠HC * | YES/YES/YES | Stop signal/SSRT | ns | 8 |
| HC (39) | 97.4% | 39.8 (11.3) | 35.1 (5.1) |
BN: bulimia nervosa; BED: binge eating disorder; AN-b: anorexia nervosa from the binge/purge subtype; HC: healthy controls; BMI: body mass index;
# : ideal body weight (percentage);
ns: no significant difference between patients and healthy controls;
significant group difference; NR: not reported; SSRT: stop signal reaction time; MFFT: Matching Familiar Figure Test; HSCT: Hayling Sentence Completion Test; ELF: Excluded Letter Fluency test; SSIT: Simon Spatial Incompatibility Task; RT: reaction time.
Twenty studies were conducted in BN patients (total of patients: n = 459, sample sizes ranging from 12 to 65), three studies in AN-b patients (total of patients: n = 42, sample sizes ranging from 12 to 16) and two studies in BED patients (patients: n = 38, and 44). Most participants in the included studies were female, with the exception of two articles that had a few male participants [11], [32] (see Table 1). The mean age of the entire sample was 26.4 years and ranged from 16.3 to 40.1 years (two articles [22], [41] included adolescent BN patients). The mean ages for the ED subtypes were 24.7, 24.6, and 36.9 years for the AN-b, BN, and BED subgroups, respectively. The mean BMI of the entire sample was 24.0 kg/m2, ranging from 15.1 to 35.9 kg/m2. The mean BMI for the ED subtypes were 17.9, 22.5, and 34.9 kg/m2 for the AN-b, BN, and BED subgroups, respectively. Approximately half of the studies provided information about educational levels or IQ scores (see Table 1). Two studies did not mention whether the patients were currently under treatment [42], [43]. Eleven studies did not provide data concerning comorbidity, while seven studies excluded participants with comorbid diagnoses, e.g., obsessive-compulsive disorder, substance abuse or dependence, psychotic disorder, bipolar disorder, etc. (see Table 1). Three studies reported the exclusive inclusion of medication-free participants [31], [32], [44], however, half of the studies did not mention or specify the usage of medication (see Table 1).
Of note, of the individual studies, 17 of the 25 (sample sizes of patients range from 14 to 65) failed to identify significant impairments in general inhibitory control in bulimic-type ED patients (see Table 1).
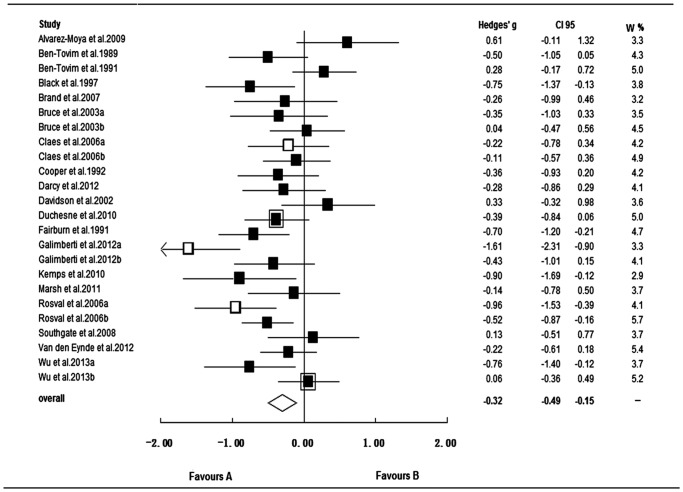
Small study effects and overall effect size
Visual inspection of the funnel plot suggested no small study effects, which was confirmed by a non-significant result on the Egger's test (p = 0.457). However, visual inspection of the funnel plot suggested a potential outlier (see Figure S1). The ES of the study [21] (20 BN patients compared to 20 controls) was −2.9 (SE = 0.45, CI95 = [−3.77; −2.02]). The pooled overall ES including the study was −0.40 (SE = 0.11, CI95 = [−0.61; −0.19], p<0.001), Q (24) = 86.0, p<0.001, I2 = 72.1%. After excluding the outlier study, the overall ES of the remaining studies on general inhibitory control was −0.32 (SE = 0.09, CI95 = [−0.49; −0.15], p = 0.001), and the heterogeneity between studies remained significant, Q (23) = 53.1, p<0.001 (see Figure 2); however, the ESs across studies decreased to medium inconsistency (I2 = 56.7%). Thus, we excluded the outlier study from the following analysis.
Figure 2. Forest plot for studies on inhibitory control to general stimuli in bulimic-type eating disorders.
▪: bulimia nervosa; ▪ with frame: binge eating disorder; □ anorexia nervosa from the binge/purge subtype; CI95: 95% confidence interval; W %: relative weight (percentage); Favours A/B: lower/higher inhibitory control in bulimic-type EDs than in controls.
Moderator analysis and sensitivity analysis
Subgroup analyses for the subtypes of bulimic-type EDs revealed significant negative effects in AN-b and BN, indicating impaired inhibitory control in this patient subpopulation. The ES for AN-b (Hedges' g = −0.91) was higher than that for BN (Hedges' g = −0.26), although this difference did not reach statistical significance. In addition, the ESs across the three AN-b studies was inconsistent to a larger extent (I2 = 78.7%) than that across the 19 BN studies (I2 = 42.7%). The pooled ES for two BED studies was non-significant (Hedges' g = −0.16, p = 0.485) (see Table 2).
Table 2. Moderator analysis of studies on general inhibitory control in bulimic-type eating disorders.
| Number of studies | Number of patients | Effect size | Heterogeneity | Small study effects | |||||
| Hedges' g | CI95 | SE | p value | p value (Egger's test) | |||||
| subtype of eating disorders | |||||||||
| BN | 19 | 439 | −0.26 | −0.43, −0.09 | 0.09 | 0.003 | Q (18) = 31.4, p = 0.026 | I2 = 42.7% | 0.878 |
| AN-b | 3 | 42 | −0.91 | −1.67, −0.14 | 0.39 | 0.020 | Q (2) = 9.38, p = 0.009 | I2 = 78.7% | 0.375 |
| BED | 2 | 82 | −0.16 | −0.60, +0.28 | 0.22 | 0.485 | Q (1) = 2.0, p = 0.156 | I2 = 50.3% | — |
| tasks | |||||||||
| Stroop | 12 | 282 | −0.25 | −0.47, −0.02 | 0.12 | 0.035 | Q (11) = 22.0, p = 0.025 | I2 = 49.9% | 0.957 |
| SST | 6 | 124 | −0.46 | −0.90, −0.03 | 0.22 | 0.036 | Q (5) = 18.6, p = 0.002 | I2 = 73.2% | 0.009 |
| No-go | 5 | 165 | −0.39 | −0.69,−0.09 | 0.15 | 0.010 | Q (4) = 7.72, p = 0.102 | I2 = 48.2% | 0.905 |
| MFFT | 2 | 27 | −0.35 | −1.34, +0.64 | 0.50 | 0.488 | Q (1) = 3.86, p = 0.05 | I2 = 74.1% | — |
| HSCT | 1 | 13 | −1.09 | −1.89, −0.29 | 0.41 | 0.008 | — | — | — |
| SSIT | 1 | 18 | −0.14 | −0.78, +0.50 | 0.33 | 0.662 | — | — | — |
| ELF | 1 | 13 | −1.02 | −1.81, −0.23 | 0.41 | 0.012 | — | — | — |
CI95: 95% confidence interval, SE: standard error; BN: bulimia nervosa; BED: binge eating disorder; AN-b: anorexia nervosa from the binge/purge subtype; SST: Stop Signal Task; MFFT: Matching Familiar Figure Test; HSCT: Hayling Sentence Completion Test; SSIT: Simon Spatial Incompatibility Task; ELF: Excluded Letter Fluency test.
Various tasks were used to investigate general inhibitory control in the retrieved studies, with the Stroop, SST, and No-go tasks being the most commonly used. The ESs for the individual task categories are presented in Table 2. Differences in ESs across task categories did not reach significance (p = 0.276). The pooled ES for studies of cognitive interference control (i.e., 12 studies using the Stroop task and one study using the Simon task) was −0.24 (SE = 0.11, CI95 = [−0.45; −0.03], p = 0.027). The pooled ES for studies on response inhibition (i.e., six studies using the SST and five studies using the No-go task) was −0.42 (SE = 0.13, CI95 = [−0.67; −0.17], p = 0.001). With respect to disinhibition, only two studies were available. In one of these studies, the MFFT was used in a sample of 14 BN patients and showed a non-significant ES (Hedges' g = 0.13, SE = 0.33, CI95 = [−0.51, 0.77], p = 0.692) [44], while in the other study, the MFFT, HSCT, and ELT were used in 13 BN patients and revealed ESs with Hedges' g of −0.88 for MFFT, −1.09 for HSCT, −1.02 for ELT (all p values <0.03) [23]. There were not enough studies on disinhibition to calculate a pooled ES.
The sensitivity analysis, which included only studies of medium to high quality (18 of 24 studies), yielded a comparable overall ES (Hedges' g = −0.36, CI95 = [−0.56; −0.16]), showing that the study quality did not influence the pooled ES in a significant way.
Inhibitory control to disease-salient stimuli
Study characteristics
A total of 12 studies in bulimic-type ED patients (total n = 218, sample size ranging from 10 to 30) using neurocognitive tasks on inhibitory control to disease-salient stimuli (food/eating, shape/weight) were included in the meta-analysis. The mean quality score of all included studies was 6.2. The characteristics of the study sample are shown in Table 3.
Table 3. Description of studies on disease-related inhibitory control in bulimic-type eating disorders.
| Study | Subject | Female (percentage) | Age (years) mean (SD) | BMI (kg/m2) mean (SD) | Educational level | Co-morbidity/Treatment/Medication | Task/Outcome variable | Findings | Quality score (x/10) |
| Ben-Tovim et al. 1989 | BN(19) | 100% | 26.9 (10) | 22.6 (4.7) | NR | NR/YES/NR | Stroop/interference index (food) | BN≠HC * | 6 |
| HC (38) | 100% | 22.8 (4.5) | 21.3 (2.5) | Stroop/interference index (shape) | BN≠HC * | ||||
| Ben-Tovim et al. 1991 | BN (27) | NR | 26.8 (9.1)* | 23.3 (4.6)* | NR | NR/YES/NR | Stroop/interference index (food) | BN≠HC * | 4 |
| HC-h (29) | 100% | 13.6 (1.1) | 21.8 (5.7) | Stroop/interference index (shape) | BN≠HC * | ||||
| HC-l (37) | 100% | 14.0 (1.3) | 19.7 (3.5)* | ||||||
| Black et al.1997 | BN (16) | 100% | 23.8 (NR) | 23 (NR) | NR | NR/NO/NR | Stroop/interference index (food) | ns | 6 |
| HC (29) | 100% | 21.2 (NR) | 22.6 (NR) | Stroop/interference index (shape) | ns | ||||
| Cooper et al. 1997 | BN (12) | 100% | NR | NR | NR | NR/YES/NR | Stroop/interference index (eating) | BN≠HC * | 6 |
| HC (18) | 100% | NR | NR | Stroop/interference index (weight/shape) | BN≠HC * | ||||
| Davidson et al. 2002 | BN (17) | 100% | 25.5 (6.4) | 21.2 (3.2) | NR | NR/YES/NR | Stroop/interference index (food) | BN≠HC * | 6 |
| HC (18) | 100% | 24.9 (6.1) | 21.1 (2.0) | Stroop/interference index (shape) | BN≠HC * | ||||
| Flynn et al. 1999 | BN (15) | 100% | 27.1 (7.0)* | 98.2 (7.1)# | ns | NR/YES/NR | Stroop/interference index (food) | ns | 6 |
| HC (13) | 100% | 22.3 (4.7) | 95.2 (7.2)# | Stroop/interference index (body) | BN≠HC * | ||||
| Jones-Chesters et al. 1998 | BN (16) | 100% | 25.6 (7.7) | 23.8 (3.0) | ns | NR/YES/NR | Stroop/RT (food/eating) | BN≠HC * | 7 |
| HC (16) | 100% | 26.6 (7.5) | 22.1 (2.8) | Stroop/RT (weight/shape) | BN≠HC * | ||||
| Lokken et al. 2006 | BN (30) | 100% | 19.1 (1.4) | 22.1 (4.3) | ns | NR/NR/NR | Stroop/interference index (eating) | BN≠HC * | 7 |
| HC (30) | 100% | 19.5 (1.0) | 22.2 (2.5) | Stroop/interference index (weight/shape) | BN≠HC * | ||||
| Lovell et al. 1997 | BN (24) | 100% | 26.9 (11.1) | 21.8 (3.5) | ns | NR/YES/NR | Stroop/RT (food) | ns | 6 |
| HC (33) | 100% | 24.7 (8.1) | 22.9 (3.6) | Stroop/RT (shape) | BN≠HC * | ||||
| Mobbs et al. 2008 | BN (18) | 100% | 25.1 (3.9) | 20.4 (2.6) | ns | YES/YES/NR | No-go/decision bias (food) | BN≠HC * | 8 |
| HC (18) | 100% | 24.3 (3.4) | 21.0 (1.6) | No-go/decision bias (body) | ns | ||||
| Perpiná et al. 1993 | BN (14) | 100% | 26.4 (4.9) | 26.6 (8.3) | ns | NR/YES/NR | Stroop/RT (food) | ns | 7 |
| HC (32) | 100% | 26.9 (6.0) | 23.4 (3.5) | Stroop/RT (body) | BN≠HC * | ||||
| Perpiná et al. 1998 | BN (10) | 100% | 27.8 (8.2) | 21.1 (2.2) | NR | NR/YES/NR | Stroop/interference index (food) | NR | 5 |
| HC (18) | 100% | 29.3 (9.7) | 21.1 (2.7) | Stroop/interference index (shape) | NR |
BN: bulimia nervosa; BED: binge eating disorder; AN-b: anorexia nervosa of the binge/purge subtype; HC: healthy controls; BMI: body mass index;
# : ideal body weight (percentage);
ns: no significant difference between patients and healthy controls;
significant group difference;
NR: not reported; RT: reaction time.
All the studies were conducted in BN patients. With the exception of one study, which did not report the gender of participants [45], samples tended to be exclusively female. The mean age of patients was 25.5 years, with a range from 19.1 to 27.8 years, and the mean BMI was 22.3 kg/m2, with a range from 20.4 to 26.6 kg/m2. Approximately half of the studies provided information about educational levels or IQ scores. Only one study included data on co-morbid diagnoses [46], and none of the studies provided information about the usage of psychotropic medication.
Four out of the 12 studies (sample sizes of patients ranging from 14 to 24) failed to identify significant impairments in inhibitory control to food/eating stimuli in BN patients, and two out of the 12 studies (sample sizes of patients were 16 and 18) failed to identify significant impairments in inhibitory control to body/shape stimuli in BN patients (see Table 3).
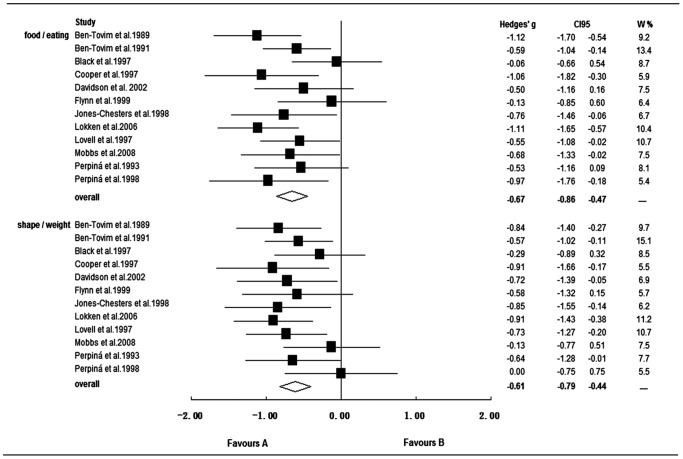
Small study effects and overall effect size
Visual inspection of funnel plots suggested no small study effects for inhibitory control to food/eating or to shape/weight, which were confirmed by the results of the Egger's test (p = 0.933; p = 0.532).
The overall ES for studies on inhibitory control to food/eating stimuli was medium (Hedges' g = −0.67, SE = 0.10, CI95 = [−0.86; −0.47], p<0.001). No significant evidence of heterogeneity was found, Q (11) = 13.4, p = 0.266, I2 = 18.1%. Studies on inhibitory control to shape/weight stimuli in BN patients also showed impairments with a medium ES (Hedges' g = −0.61, SE = 0.09, CI95 = [−0.79; −0.44], p<0.001), with no indication for heterogeneity, Q (11) = 9.1, p = 0.616, I2 = 0. There was no significant difference between ESs for food/eating and shape/weight (see Figure 3). However, the overall ES for inhibitory control to disease-salient stimuli was significantly larger than that for general inhibitory control (p = 0.014).
Figure 3. Forest plot for studies on inhibitory control to disease-salient stimuli in bulimia nervosa patients.
▪: bulimia nervosa; CI95: 95% confidence interval; W %: relative weight (percentage); food/eating: study used food/eating related stimuli; shape/weight: study used shape/weight related stimuli; Favours A/B: lower/higher inhibitory control in bulimic-type EDs than in controls.
Moderator analysis and sensitivity analysis
As Table 4 shows, all studies were run in BN patients, therefore, no comparison between subtypes of bulimic-type EDs was possible.
Table 4. Moderator analysis of studies on inhibitory control to disease-salient stimuli in BN patients.
| Number of studies | Number of patients | Effect size | Heterogeneity | Small study effects | |||||
| Hedges' g | CI95 | SE | p value | p value (Egger's test) | |||||
| a) Food/eating | |||||||||
| BN | 12 | 218 | −0.67 | −0.86, −0.47 | 0.10 | <0.001 | Q (11) = 13.4, p = 0.266 | I2 = 18.1% | 0.933 |
| Tasks | |||||||||
| Stroop | 11 | 200 | −0.67 | −0.88, −0.45 | 0.11 | <0.001 | Q (10) = 13.4, p = 0.201 | I2 = 25.5% | 0.938 |
| No-go | 1 | 18 | −0.68 | −1.34, −0.02 | 0.34 | 0.042 | — | — | — |
| b) Shape/weight | |||||||||
| BN | 12 | 218 | −0.61 | −0.79, −0.44 | 0.09 | <0.001 | Q (11) = 9.1, p = 0.616 | I2 = 0 | 0.532 |
| Tasks | |||||||||
| Stroop | 11 | 200 | −0.65 | −0.84, −0.47 | 0.09 | <0.001 | Q (10) = 6.65, p = 0.758 | I2 = 0 | 0.628 |
| No-go | 1 | 18 | −0.13 | −0.77, +0.51 | 0.33 | 0.699 | — | — | — |
CI95: 95% confidence interval, SE: standard error; BN: bulimia nervosa.
The Stroop task was used most frequently (11 out of the 12 studies), showing significant negative ESs for cognitive interference control to food/eating and shape/weight stimuli in BN patients (Hedges' g = −0.67, −0.65, respectively). There was only one study in which an alternative task (i.e., No-go task) was used to measure response inhibition [46]. The ES for the No-go study showed a significant effect for impaired inhibitory control to food/eating stimuli (Hedges' g = −0.68, p = 0.042) but not to shape/weight stimuli (p = 0.699) in BN patients (see Table 4).
Sensitivity analyses including only studies of medium to high quality (10 of the 12 studies) yielded comparable overall ESs (food/eating: Hedges' g = −0.66, CI95 = [−0.90; −0.41]; shape/weight: Hedges' g = −0.67, CI95 = [−0.86; −0.47]), demonstrating that the study quality did not influence the pooled ESs in a significant manner.
Discussion
The present systematic review and meta-analysis is the first to quantitatively synthesise the neuropsychological findings of inhibitory control in bulimic-type EDs, which consist of AN-b, BN and BED. Publications were searched up to March 2013, and 24 studies assessing inhibitory control to general stimuli and 12 studies focusing on inhibitory control to disease- salient stimuli were included in the meta-analysis.
The main finding of the meta-analysis is that bulimic-type ED patients have impaired general inhibitory control with a small ES when compared to healthy controls. The two main task categories of response inhibition (i.e., No-go task, SST) and effortful cognitive interference control (i.e., Stroop task, Simon task) showed a similar level of impairment. Notably, there was a significantly greater impairment (medium ES) to disease-salient stimuli than general stimuli, indicating that disease-salient stimuli worsen the general impairment of inhibitory control in BN patients. The comparison of inhibitory control to general and disease-salient stimuli was restricted to BN patients due to a lack of studies in AN-b and BED patients. Furthermore, the findings were largely based on cognitive interference control tasks (i.e., the Stroop task). Further research is needed to investigate whether greater impairment to disease-salient stimuli is also found in AN-b and BED and whether greater impairment is task- category independent and may also be found in response inhibition tasks. Differentiating the spectrum of bulimic-type EDs using diagnostic categories, preliminary findings indicate a large ES of AN-b, a small ES for BN, and a non-significant ES for BED with respect to impaired inhibitory control to general stimuli. However, these findings should be treated with caution, as most of the studies were conducted with BN populations, while only three studies were conducted in AN-b patients, and only two studies in BED patients were available.
As an extension of findings from previous studies, the present meta-analysis is the first to show significantly greater impairments of inhibitory control to disease-salient stimuli compared to general stimuli in BN patients. This finding indicates that attentional bias and approach motivation to disease-salient stimuli in BN patients may potentiate the generally impaired inhibitory control in this population, thus facilitating binge eating (releasing feeding behaviours from regulatory control). In comparison to previous meta-analyses, the enlarged meta-analysis of the present study showed a slightly smaller ES for impaired general inhibitory control in BN when compared to previous reviews [20], [36]. In contrast, slightly higher effects were found in BN patients to disease-salient stimuli in the present meta-analysis when compared to previous reports [20], [35]. However, the inclusion of recovered patients in previous meta-analyses [20], [35] may have also contributed to the mentioned differences in ESs.
Furthermore, with respect to a dimensional approach, the present findings support a decrease in inhibitory control from BED over BN to AN-b patients. This finding has clinical implications for the ED psychopathology, as it suggests that in BED patients, decreased inhibitory control seems to be of less importance than for AN-b and BN patients. These differences in inhibitory control may be relevant to behavioural distinctions for binge eating between BN and BED patients [11]. However, further research is needed to support the preliminary findings in BED patients.
The present review has progressed findings from previous reviews in a number of ways. First, this review has included a larger sample of bulimic-type ED patients (a total of 563 patients), thus covering the broad spectrum of bulimic-type EDs (i.e., AN-b, BN, and BED). Second, the methodological quality of this review was systematically assessed and included in sensitivity analyses, showing that there was no evidence that studies of lower methodological quality confounded the estimated ESs. In addition, in comparison to previous meta-analyses that focused on one specific inhibitory control task (i.e., Stroop task) [20], [35], we included different inhibitory control tasks to calculate a more comprehensive ES of impaired inhibitory control in bulimic-type EDs. This methodological approach was justified, as heterogeneity (I 2 value) was acceptable in the face of rather different tasks and patient populations. The stability of ESs over different inhibitory control tasks suggests a common underlying mechanism that seems independent from the specific task. Of note, for general inhibitory control, more than half of clinical studies failed to identify significant impairments in bulimic-type ED patients. In contrast, the meta-analysis with higher statistical power uncovered a small but significant impaired inhibitory control in bulimic-type ED patients.
It was not until recently that researchers began to investigate the underlying neural circuits of impaired inhibitory control in bulimic-type EDs [21], [22], [47], [48]. These neuroimaging studies suggest altered brain activation within frontostriatal circuits during the execution of inhibitory control tasks. More specifically, BN patients failed to activate frontostriatal circuits to the same degree as healthy comparison subjects during the execution of a cognitive inhibitory control task (Simon task: [21], [22]; No-go task: [47]). Further evidence for dysfunctional lateral prefrontal cortex activity comes from a study using transcranial magnetic stimulation [49]. These altered brain activations within frontostriatal circuits may contribute to deficits in inhibitory control at a neurocognitive level in bulimic- type EDs. Given the findings of the present meta-analysis, determining the neural mechanisms that contribute to deterioration in inhibitory control to disease-salient stimuli in BN patients may be a promising avenue for future neuroimaging research.
Limitations and implications for future work
First, the fact that we excluded studies that did not provide data for ES calculations [25], [40] and the lack of a direct search for unpublished data and grey literature may have resulted in a potential bias, which might have influenced the stability of pooled overall ES for inhibitory control. However, in the current review, the funnel plot and the Egger's test did not show small study effects, which is an indicator of the publication bias. Second, as common to all meta-analyses, findings from the current meta-analyses are to some extent influenced by the quality of primary studies, although the sensitivity analyses demonstrated that the quality levels of the included studies did not significantly affect the overall ES. We developed a priori a standardized checklist of risk of bias which was based on the domains of the Newcastle-Ottawa Scale, as no standardized criteria have been developed to assess the quality of neuropsychological studies. Third, for some studies, the data for the main outcome measures were not available (e.g., interference index for Stroop task), and the secondary outcome measure had to be used (e.g., score from colour-word conflict trial). This may have increased the heterogeneity across studies. However, the statistical testing for heterogeneity across studies showed acceptable inconsistencies (after excluding one potential outlier study). Fourth, our findings of impaired inhibitory control are valid for bulimic-type ED patients in the acute phase. We did not include patients who had recovered from bulimic-type EDs and did not consider whether patients were in treatment during investigation. Further research in ED patients after recovery or rather longitudinal studies are needed to differentiate whether inhibitory impairments are a state or rather a trait or a ‘scar’ after recovery of bulimic-type eating disorders. Fifth, we have not considered emotional interference on inhibitory control performance that may be of relevance in ED patients. However, at present the number of studies is too small to calculate a quantitative meta-analysis across ED diagnoses. Finally, the estimated ESs for AN-b and BED patients should be treated with caution given the limited sample sizes.
These findings have significant clinical implications, as dimensional measures of neurocognitive functioning related to inhibitory control may help to select specific psychological (e.g., cognitive remediation), as well as pharmacological interventions (e.g. selective serotonin reuptake inhibitors) that are designed to target basic neurobiological processes involved in inhibitory control functions. A better understanding of the neurocognitive profiles of bulimic-type EDs may help to provide a more fine-grained diagnostic classification, and refine existing treatment approaches as well as inform the development of new interventions.
Given the impaired inhibitory control noted in the studies, especially to disease-salient stimuli, these findings support the use of impulse control techniques in the current treatment regimens. In addition, cognitive training to address inhibitory control (i.e., cognitive remediation therapy) may improve treatment outcome and may represent a promising treatment modality for future research [50]. With respect to experimental research, future studies should consider more complex paradigms that would allow for the further exploration of the interactions between inhibitory control and other cognitive domains (e.g., set-shifting, decision-making) as well as emotional interference. Given the high comorbidity of depression and anxiety disorders in EDs, future studies should consider to a greater extent the impact of mood states on the performance in inhibitory control tasks or to use paradigms that systematically differentiate between with and without emotional interference.
Conclusions
The primary finding of the present review is that bulimic-type ED patients show an impairment in inhibitory control to general stimuli with a small ES. This rather low general impairment in BN patients was enlarged by disease-salient stimuli, suggesting a greater impairment of inhibitory control specifically to disorder related stimuli, which may underlie recurrent episodes of binge eating. For AN-b and BED patients, further clinical studies are needed to validate the preliminary findings.
Supporting Information
PRIMSA Checklist.
(DOC)
Funnel plot for all studies on general inhibitory control in bulimic-type eating disorders. The arrow indicates one outlier study.
(TIF)
Acknowledgments
We are grateful to all the authors of the included studies, particularly those who sent us the necessary data for our review and meta-analysis.
Funding Statement
MW was supported by a travelling fellowship from the China Scholarship Council, which is affiliated with the Ministry of Education, P. R. China. MS was supported by a grant from the German Research Foundation (FR2626/3-1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.APA (1994) Diagnostic and statistical manual of mental disorders (fourth edition). Washington, DC: American Psychiatric Association. [Google Scholar]
- 2. Arcelus J, Mitchell AJ, Wales J, Nielsen S (2011) Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry 68: 724–731. [DOI] [PubMed] [Google Scholar]
- 3. Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, et al. (2009) Increased mortality in bulimia nervosa and other eating disorders. Am J Psychiatry 166: 1342–1346. [DOI] [PubMed] [Google Scholar]
- 4. Fairburn CG, Cooper Z, Shafran R (2003) Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther 41: 509–528. [DOI] [PubMed] [Google Scholar]
- 5. Wildes JE, Marcus MD (2013) Incorporating dimensions into the classification of eating disorders: three models and their implications for research and clinical practice. Int J Eat Disord 46: 396–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Robbins TW, Gillan CM, Smith DG, de Wit S, Ersche KD (2012) Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cogn Sci 16: 81–91. [DOI] [PubMed] [Google Scholar]
- 7. Dansky BS, Brewerton TD, Kilpatrick DG (2000) Comorbidity of bulimia nervosa and alcohol use disorders: results from the National Women's Study. Int J Eat Disord 27: 180–190. [DOI] [PubMed] [Google Scholar]
- 8. Grilo CM, White MA, Masheb RM (2009) DSM-IV psychiatric disorder comorbidity and its correlates in binge eating disorder. Int J Eat Disord 42: 228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Claes L, Nederkoorn C, Vandereycken W, Guerrieri R, Vertommen H (2006) Impulsiveness and lack of inhibitory control in eating disorders. Eat Behav 7: 196–203. [DOI] [PubMed] [Google Scholar]
- 10. Lijffijt M, Bekker EM, Quik EH, Bakker J, Kenemans JL, et al. (2004) Differences between low and high trait impulsivity are not associated with differences in inhibitory motor control. J Atten Disord 8: 25–32. [DOI] [PubMed] [Google Scholar]
- 11. Wu M, Giel KE, Skunde M, Schag K, Rudofsky G, et al. (2013) Inhibitory control and decision making under risk in bulimia nervosa and binge-eating disorder. Int J Eat Disord 46: 721–728. [DOI] [PubMed] [Google Scholar]
- 12. Logan GD, Schachar RJ, Tannock R (1997) Impulsivity and inhibitory control. Psychol Sci 8: 60–64. [Google Scholar]
- 13. Nigg JT (2000) On inhibition/disinhibition in developmental psychopathology: views from cognitive and personality psychology and a working inhibition taxonomy. Psychol Bull 126: 220–246. [DOI] [PubMed] [Google Scholar]
- 14. Starkstein SE, Robinson RG (1997) Mechanism of disinhibition after brain lesions. J Nerv Ment Dis 185: 108–114. [DOI] [PubMed] [Google Scholar]
- 15. Aron AR, Robbins TW, Poldrack RA (2004) Inhibition and the right inferior frontal cortex. Trends Cogn Sci 8: 170–177. [DOI] [PubMed] [Google Scholar]
- 16. Bari A, Robbins TW (2013) Inhibition and impulsivity: Behavioral and neural basis of response control. Prog Neurobiol 108: 44–79. [DOI] [PubMed] [Google Scholar]
- 17. Tchanturia K, Davies H, Roberts M, Harrison A, Nakazato M, et al. (2012) Poor cognitive flexibility in eating disorders: examining the evidence using the Wisconsin Card Sorting Task. PLoS One 7: e28331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rosval L, Steiger H, Bruce K, Israel M, Richardson J, et al. (2006) Impulsivity in women with eating disorders: problem of response inhibition, planning, or attention? Int J Eat Disord 39: 590–593. [DOI] [PubMed] [Google Scholar]
- 19. Casey BJ, Trainor RJ, Orendi JL, Schubert AB, Nystrom LE, et al. (1997) A developmental functional MRI study of prefrontal activation during performance of a Go-No-Go task. J Cogn Neurosci 9: 835–847. [DOI] [PubMed] [Google Scholar]
- 20. Dobson KS, Dozois DJ (2004) Attentional biases in eating disorders: a meta-analytic review of Stroop performance. Clin Psychol Rev 23: 1001–1022. [DOI] [PubMed] [Google Scholar]
- 21. Marsh R, Steinglass JE, Gerber AJ, Graziano O'Leary K, Wang Z, et al. (2009) Deficient activity in the neural systems that mediate self-regulatory control in bulimia nervosa. Arch Gen Psychiatry 66: 51–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marsh R, Horga G, Wang Z, Wang P, Klahr KW, et al. (2011) An FMRI study of self-regulatory control and conflict resolution in adolescents with bulimia nervosa. Am J Psychiatry 168: 1210–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kemps E, Wilsdon A (2010) Preliminary evidence for a role for impulsivity in cognitive disinhibition in bulimia nervosa. J Clin Exp Neuropsychol 32: 515–521. [DOI] [PubMed] [Google Scholar]
- 24. Bruce KR, Koerner NM, Steiger H, Young SN (2003) Laxative misuse and behavioral disinhibition in bulimia nervosa. Int J Eat Disord 33: 92–97. [DOI] [PubMed] [Google Scholar]
- 25. Bruce KR, Steiger H, Koerner NM, Israel M, Young SN (2004) Bulimia nervosa with co-morbid avoidant personality disorder: behavioural characteristics and serotonergic function. Psychol Med 34: 113–124. [DOI] [PubMed] [Google Scholar]
- 26. Celone KA, Thompson-Brenner H, Ross RS, Pratt EM, Stern CE (2011) An fMRI investigation of the fronto-striatal learning system in women who exhibit eating disorder behaviors. Neuroimage 56: 1749–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Claes L, Mitchell JE, Vandereycken W (2012) Out of control? Inhibition processes in eating disorders from a personality and cognitive perspective. Int J Eat Disord 45: 407–414. [DOI] [PubMed] [Google Scholar]
- 28. Van den Eynde F, Samarawickrema N, Kenyon M, DeJong H, Lavender A, et al. (2012) A study of neurocognition in bulimia nervosa and eating disorder not otherwise specified-bulimia type. J Clin Exp Neuropsychol 34: 67–77. [DOI] [PubMed] [Google Scholar]
- 29. Galimberti E, Martoni RM, Cavallini MC, Erzegovesi S, Bellodi L (2012) Motor inhibition and cognitive flexibility in eating disorder subtypes. Prog Neuropsychopharmacol Biol Psychiatry 36: 307–312. [DOI] [PubMed] [Google Scholar]
- 30. Alvarez-Moya EM, Jimenez-Murcia S, Moragas L, Gomez-Pena M, Aymami MN, et al. (2009) Executive functioning among female pathological gambling and bulimia nervosa patients: preliminary findings. J Int Neuropsychol Soc 15: 302–306. [DOI] [PubMed] [Google Scholar]
- 31. Brand M, Franke-Sievert C, Jacoby GE, Markowitsch HJ, Tuschen-Caffier B (2007) Neuropsychological correlates of decision making in patients with bulimia nervosa. Neuropsychology 21: 742–750. [DOI] [PubMed] [Google Scholar]
- 32. Duchesne M, Mattos P, Appolinario JC, Freitas SR, Coutinho G, et al. (2010) Assessment of executive functions in obese individuals with binge eating disorder. Rev Bras Psiquiatr 32: 381–388. [DOI] [PubMed] [Google Scholar]
- 33. Duchesne M, Mattos P, Fontenelle LF, Veiga H, Rizo L, et al. (2004) [Neuropsychology of eating disorders: a systematic review of the literature]. Rev Bras Psiquiatr 26: 107–117. [DOI] [PubMed] [Google Scholar]
- 34. Van den Eynde F, Guillaume S, Broadbent H, Stahl D, Campbell IC, et al. (2011) Neurocognition in bulimic eating disorders: a systematic review. Acta Psychiatr Scand 124: 120–140. [DOI] [PubMed] [Google Scholar]
- 35. Brooks S, Prince A, Stahl D, Campbell IC, Treasure J (2011) A systematic review and meta-analysis of cognitive bias to food stimuli in people with disordered eating behaviour. Clin Psychol Rev 31: 37–51. [DOI] [PubMed] [Google Scholar]
- 36. Zakzanis KK, Campbell Z, Polsinelli A (2010) Quantitative evidence for distinct cognitive impairment in anorexia nervosa and bulimia nervosa. J Neuropsychol 4: 89–106. [DOI] [PubMed] [Google Scholar]
- 37. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, et al. (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343: d4002. [DOI] [PubMed] [Google Scholar]
- 39. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mobbs O, Iglesias K, Golay A, Van der Linden M (2011) Cognitive deficits in obese persons with and without binge eating disorder. Investigation using a mental flexibility task. Appetite 57: 263–271. [DOI] [PubMed] [Google Scholar]
- 41. Darcy AM, Fitzpatrick KK, Colborn D, Manasse S, Datta N, et al. (2012) Set-shifting among adolescents with bulimic spectrum eating disorders. Psychosom Med 74: 869–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cooper MJ, Anastasiades P, Fairburn CG (1992) Selective processing of eating-, shape-, and weight-related words in persons with bulimia nervosa. J Abnorm Psychol 101: 352–355. [DOI] [PubMed] [Google Scholar]
- 43. Fairburn CG, Cooper PJ, Cooper MJ, Mckenna FP, Anastasiades P (1991) Selective information processing in bulimia nervosa. Int J Eat Disord 10: 415–422. [Google Scholar]
- 44. Southgate L, Tchanturia K, Treasure J (2008) Information processing bias in anorexia nervosa. Psychiatry Res 160: 221–227. [DOI] [PubMed] [Google Scholar]
- 45. Ben-Tovim DI, Walker MK (1991) Further evidence for the Stroop test as a quantitative measure of psychopathology in eating disorders. Int J Eat Disord 10: 609–613. [Google Scholar]
- 46. Mobbs O, Van der Linden M, d'Acremont M, Perroud A (2008) Cognitive deficits and biases for food and body in bulimia: investigation using an affective shifting task. Eat Behav 9: 455–461. [DOI] [PubMed] [Google Scholar]
- 47. Lock J, Garrett A, Beenhakker J, Reiss AL (2011) Aberrant brain activation during a response inhibition task in adolescent eating disorder subtypes. Am J Psychiatry 168: 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Friederich HC, Wu M, Simon JJ, Herzog W (2013) Neurocircuit function in eating disorders. Int J Eat Disord 46: 425–432. [DOI] [PubMed] [Google Scholar]
- 49. Van den Eynde F, Claudino AM, Mogg A, Horrell L, Stahl D, et al. (2010) Repetitive transcranial magnetic stimulation reduces cue-induced food craving in bulimic disorders. Biol Psychiatry 67: 793–795. [DOI] [PubMed] [Google Scholar]
- 50. Sofuoglu M, DeVito EE, Waters AJ, Carroll KM (2013) Cognitive enhancement as a treatment for drug addictions. Neuropharmacology 64: 452–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRIMSA Checklist.
(DOC)
Funnel plot for all studies on general inhibitory control in bulimic-type eating disorders. The arrow indicates one outlier study.
(TIF)