Abstract
Background
Long duration of untreated psychosis (DUP) is associated with poor treatment outcome. Whether or not DUP is related to brain gray matter volume abnormalities in antipsychotic medication treatment naïve schizophrenia remains unclear at this time.
Methods
Patients with treatment-naïve schizophrenia and healthy controls went through brain scan using high resolution Magnetic Resonance Imaging. DUP was evaluated using the Nottingham Onset Schedule (NOS), and dichotomized as short DUP (≤ 26 weeks) or long DUP (>26 weeks). Voxel-based methods were used for volumetric measure in the brain.
Results
Fifty-seven patients (27 short DUP and 30 long DUP) and 30 healthy controls were included in the analysis. There were significant gray matter volumetric differences among the 3 groups in bilateral parahippocampus gyri, right superior temporal gyrus, left fusiform gyrus, left middle temporal gyrus, and right superior frontal gyrus (p's<0.01). Compared with healthy controls, the long DUP group had significantly smaller volume in all these regions (p's <0.05). Compared with the short-DUP group, the long-DUP group had significantly smaller volume in right superior temporal gyrus, left fusiform gyrus, and left middle temporal gyrus (p's<0.01).
Conclusion
Our findings suggest that DUP is associated with temporal and occipitotemporal gray matter volume decrease in treatment naïve schizophrenia. The brain structural changes in untreated psychosis might contribute to poor treatment response and long-term prognosis in this patient population.
Introduction
Brain gray matter volume abnormalities, primarily in the frontal and temporal lobes, have been consistently reported in first episode of psychosis [1], [2]. The exact mechanisms for brain abnormalities early in the course of illness are still poorly understood. In particular, it remains unclear whether such abnormalities are influenced by the duration of untreated psychosis (DUP). DUP is defined as the time between onset of psychosis and the start of hospitalization or adequate antipsychotic drug treatment [3], [4]. Prolonged DUP has been associated with poor clinical and social outcomes [5], [6]. It has been suggested that DUP may have neurotoxic effect on the brain [7]–[9].
Previous studies have examined the association between DUP and brain structural changes in schizophrenia [10]–[15]. In region of interest based analyses, a longer DUP was associated with decreased volumes in caudate nucleus [10], left planum temporal [11], and left superior temporal gyri [12].
The voxel-based morphometry (VBM) method, which is an automated whole-brain magnetic resonance image measurement technique, is capable of assessing anatomical differences in the entire brain, and avoids operational bias toward particular brain structures. Previous studies using VBM analysis reported that DUP correlated with decreased temporal gray matter volume in first episode psychosis [13], [14]. A recent study showed that DUP was associated with orbital-frontal gray matter volume decrease in patients with first episode psychosis [15]. But most of subjects in previous studies were on antipsychotic treatment at the time of imaging scan.
The present study was to use the VBM approach to examine the relationship between DUP and gray matter volume in antipsychotic medication treatment naïve schizophrenia.
Methods
Subjects
Antipsychotic medication treatment naive patients with schizophrenia were recruited from the Third Affiliated Hospital of Sun Yat-sen University, China. The diagnosis of schizophrenia was confirmed using the Structured Clinical Interview for DSM-IV Axis I Disorders–Clinician Version administered by clinicians (QL and YS)[16]. Patients had never received antipsychotic or other psychotropic medication treatment prior to the study. Healthy individuals with no psychiatric history from the local community, matched with the patient group by age, gender, handedness, and education level, were recruited as controls. All subjects were within the age range 18 to 45 years old, right-handed, of Han Chinese ethnicity, and had more than 9 years of formal education. The exclusion criteria included neurological disorders, traumatic brain injury, substance-related disorders, history of electroconvulsive therapy, family history of mental illness, mental retardation, and contraindications for MRI scanning.
The study was approved by the Institutional Review Board at the Third Affiliated Hospital of Sun Yat-sen University. A written informed consent was obtained from each subject, or his or her legal guardians.
Clinical measures
The duration of untreated psychosis was evaluated using the Nottingham Onset Schedule (NOS) [17]. It was a short, guided interview and rating schedule to measure onset in psychosis. The NOS was completed based on medical records and the interview. The interview has explicit rules on how symptom onset and cessation should be rated, and if symptoms should be included. It also includes rules on choosing time frames when responses are unclear. The validity of the scale has been demonstrated in previous studies [18], [19].
The severity of psychopathology was assessed using the Positive and Negative Syndrome Scale (PANSS) [20].
Imaging acquisition and processing
Brain MRI scans were acquired using a 1.5-T GE Signa Twinspeed MRI scanner (General Electric Medical System, Milwaukee, WI, USA) located in the Magnetic Resonance Center of the Third Affiliated Hospital of Sun Yat-sen University. The first sequence was a transverse spin-echo scan, which acquired both T2- and proton-density weighted images of the brain. High-resolution whole brain volumetric T1-weighted images were acquired sagittally with an inversion-recovery prepared 3-D spoiled gradient echo (SPGR) pulse sequence (TI = 650 ms, TE = 9.6 ms, flip angle = 15°, field-of-view, FOV = 240×240 mm2, slice thickness = 1.8 mm, matrix = 256×256, TR = 7.47 ms, slices = 301).
All structural data were processed using the VBM toolbox (VBM8) (http://dbm.neuro.uni-jena.de/vbm) in the Statistical Parametric Mapping 8 software package (http://www.fil.ion.ucl.ac.uk/spm). First, all T1-weighted anatomical images were normalized to T1 template in SPM and then segmented into gray matter(GM), white matter(WM), and cerebrospinal fluid images(CSF). After this preprocessing, segmented images were checked to ensure all images were unabridged. Imaging data were smoothed with an 8 mm full width at half-maximum (FWHM) Gaussian kernel before the GM images were entered into a statistical model.
Statistical analysis
Clinical and demographic characteristics were compared among the groups using one-way analysis of variance (ANOVA) or chi-square test. A p value of 0.05 (two tailed) was used for statistical significance.
One-way analysis of covariance (ANCOVA) was used to compare VBM differences among the three groups controlling for gender, age and years of education, followed by post hoc t-tests for between group comparisons. The resulting statistical map obtained from ANCOVA test was corrected for multiple comparisons to a significant level of p< 0.01 by combining the individual voxel p <0.01 and cluster size >731 voxels using Monte Carlo simulations in the AFNI AlphaSim program.
To further examine the relationship between duration of untreated psychosis and the decreased gray volumes, we extracted the sum volumes of the clusters in the brain regions showed differences among 3 groups in VBM analysis. Multiple regression analysis in all patients was performed using SPM8 with gray matter volumes as dependent variable, DUP as a covariate of interest, and gender, age, years of education and PANSS total scores controlled as potential confounding variables.
Results
Demographic and clinical characteristics
A total of 61 patients and 32 healthy controls enrolled in the study. Four patients and 2 healthy controls withdrew from the study before any assessment procedures. Therefore 57 patients and 30 healthy controls completed the study.
According the previous study [15], patients were divided into two groups based on a DUP cutoff value of 26 weeks: the short DUP group (DUP≤26 weeks, n = 27) and the long DUP group (DUP>26 weeks, n = 30).
There were no significant differences in gender, age or years of education among the three groups (p's≥0.30). No significant differences were found between the two patient groups in the PANSS total or subscale scores (p's≥0.147; Table 1).
Table 1. Demographic and clinical characteristics of the study sample.
| Short-DUP(≤26 weeks) | Long-DUP(>26 weeks) | Healthy Controls | F/χ2 | p | |
| Age (years) | 25.1(6.3) | 25.7(6.7) | 25.6 (6.7) | 0.065 | 0.937 |
| Gender (M/F) | 16/11 | 16/14 | 16/14 | 0.264 | 0.876 |
| Education (years) | 11.3 (2.3) | 12.1(2.9) | 12.2(1.9) | 0.996 | 0.374 |
| DUP (weeks) | 7.1 (1.4) | 60.2 (11.0) | - | 66.113 | <0.001 |
| PANSS positive scores | 24.3 (4.9) | 23.0 (6.3) | - | 0.490 | 0.487 |
| PANSS negative scores | 13.8 (4.9) | 16.0 (6.9) | - | 2.165 | 0.147 |
| PANSS total scores | 73.7 (8.1) | 75.3 (11.9) | - | 1.642 | 0.205 |
Abbreviations: DUP = duration of untreated psychosis, PANSS = the Positive and Negative Syndrome Scale, values are expressed as mean (SD).
Gray matter volumetric measures
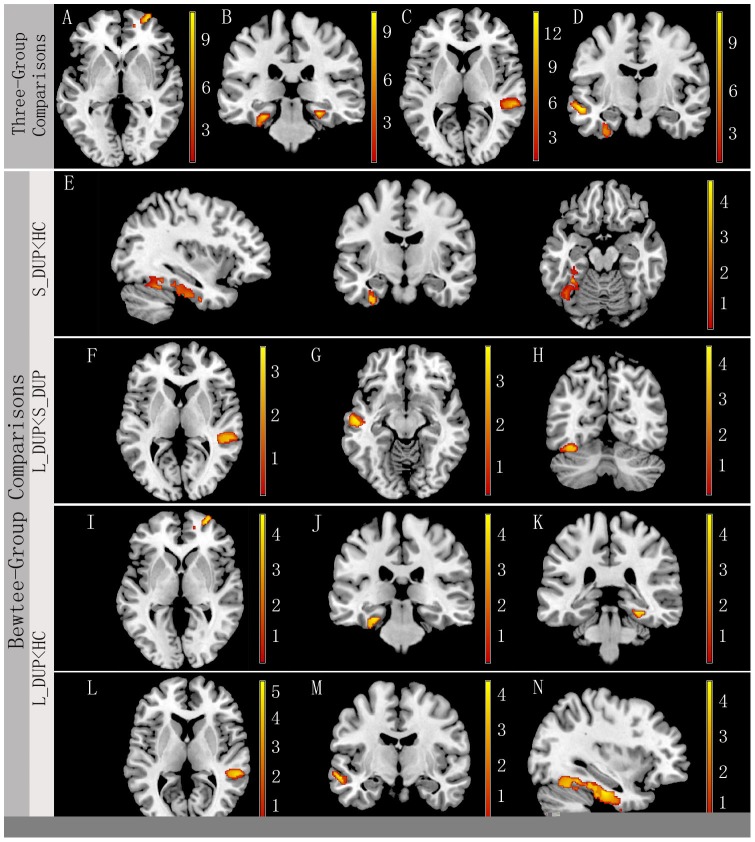
The VBM analysis showed significant differences among the three groups in gray matter volume in bilateral parahippocampus gyris, right superior temporal gyrus, left fusiform gyrus, left middle temporal gyrus, and right superior frontal gyrus (p's < 0.01).
Compared with healthy controls, long-DUP patients had significantly smaller gray matter volume in all these regions (p's <0.05, corrected). The gray matter volume was significantly smaller in right superior temporal gyrus, left fusiform gyrus, and left middle temporal gyrus in the long-DUP group compared with the short-DUP group(p's <0.01). Compared with healthy controls, the short-DUP group had a significantly smaller gray mater volume in left fusiform gyrus (p<0.01) (Fig. 1, Table 2).
Figure 1. Brain anatomical regions that showed significant difference in gray matter volume among the three groups (right is right).
A) right superior frontal gyrus, B) bilateral parahippocampus gyri, C) right superior temporal gyrus, and D) left fusiform and middle temporal gyri. Post-hoc analysis further suggested that the S-DUP group had significantly decreased gray matter volume in E) left fusiform gyrus compared with healthy control subjects, and significantly increased gray matter volume in F) right superior temporal gyrus, G) left middle temporal gyrus, and H) left fusiform compared with the L-DUP group. Compared with healthy control subjects, the L-DUP group had significantly decreased gray matter volume in I) right superior frontal gyrus, J) and K) bilateral parahippocampus gyrus, L) right superior temporal gyrus, M) left middle temporal gyrus, and N) left fusiform gyrus. Of note, statistical maps between L-DUP vs. Healthy control subjects were corrected for multiple comparisons using FDR (p<0.05), while those between L-DUP vs. S-DUP, and S-DUP vs. Healthy control subjects were corrected for multiple comparisons at the significant level of p<0.01 using AlphaSim Program (an extent threshold of p<0.01 with a minimum cluster size of 731 voxels).
Table 2. Comparison of gray matter volumes among the three groups.
| Comparison | ||||||
| Anatomical region | MNI Coordinate(x, y, z) | Cluster size | F a | S-DUP<HC b | L-DUP<HC c | L-DUP <S-DUP b |
| L parahippocampal | −28.5, −22, −20 | 1278d | 9.99 | 4.75 | ||
| R parahippocampal | 27, −27, −15 | 1106 | 10.25 | 4.52 | ||
| L Fusiform | −37.5, −60, −16.5 | 1278d | 11.67 | 4.33 | 4.57 | 4.28 |
| L middle temporal | −54, −4.5, 16.5 | 756 | 7.12 | 4.25 | 3.89 | |
| R superior temporal | 59, −31, 1 | 1323 | 13.90 | 5.26 | 3.78 | |
| R superior frontal | 30, 62, 0 | 807 | 11.22 | 4.59 | ||
Abbreviations: L = left, R = right, HC = Healthy Control subjects, S-DUP = short duration of untreated psychosis, L-DUP = long duration of untreated psychosis.
a All effects survived a voxel-wise statistical threshold using ANCOVA controlling for gender, age and years of education (p<0.01, AlphaSim corrected).
b All effects survived a voxel-wise statistical threshold using post-hoc test (p<0.01, AlphaSim corrected).
c All effects survived a voxel-wise statistical threshold using post-hoc test (p<0.05, FDR corrected).
d These peaks belong to the same cluster.
Relationship between DUP and gray matter volumetric measures
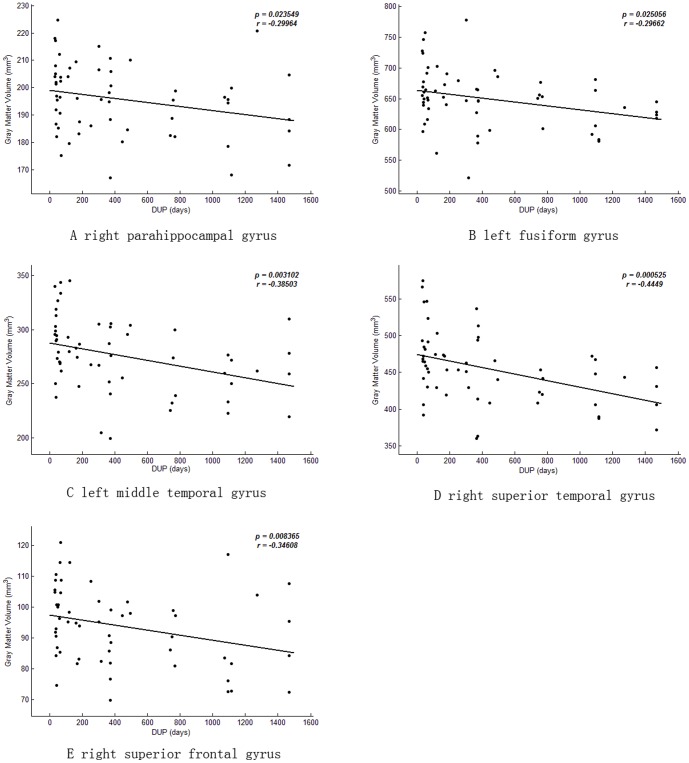
Significant inverse relationships were found between DUP and right parahippocampal gyrus, right superior temporal gyrus, left fusiform gyrus, left middle temporal gyrus, and right superior frontal gyrus after controlling for gender, age, years of education, and PANSS total scores, indicating a longer DUP was associated with decreased gray matter volume in these regions (r≤−0.30, p's≤0.025; Fig. 2).
Figure 2. Association between duration of untreated psychosis and gray matter volume.
Voxel-based multiple regression analysis was performed using SPM8 with gray matter volumes as dependent variable, DUP as a covariate of interest, and gender, age, years of education and PANSS total scores controlled as potential confounding variables.
Discussion
In this study, we examined the relationship between DUP and the brain gray matter volume in a sample of patients with antipsychotic medication treatment-naïve schizophrenia using voxel-based methods. Our results showed significantly smaller gray matter volume in right superior temporal gyrus, left fusiform gyrus, and left middle temporal gyrus in the long-DUP group compared with the short-DUP group. Our results are consistent with the findings from other studies [12]–[15], [21].
Several previous studies have shown that a prolonged DUP was associated with decreased superior temporal gyrus volume and left middle temporal gyrus volume [12], [15]. Superior temporal gyrus plays an important role, in thought and language processes, and is a major area of interest in schizophrenia research. One study has shown predominantly right-sided volumetric abnormalities in superior temporal gyrus in patients with early-onset schizophrenia [22].
Middle temporal gyrus is related to language and semantic memory processing, visual perception, and multimodal sensory integration. Previous studies have found middle temporal gyrus gray matter volume abnormalities in chronic and early-stage schizophrenia [23], [24]. A recent study has shown decreased left middle temporal gyrus volume in antipsychotic medication-naive, first-episode schizophrenia patients and their healthy unaffected siblings [25].
Lappin et al. [26] reported that a longer DUP was associated with poorer cognitive function in patients with schizophrenia. The temporal lobe has an integral role in language processing and semantic memory. The temporal gray matter volume abnormalities found in our study likely contributes to cognitive deficits in patients with untreated schizophrenia as reported in the literature. The fusiform gyrus, or occipitotemporal gyrus, is related to the processing and encoding of faces [27], which have been reported to be impaired in patients with schizophrenia [28]. Another prospective study has identified fusiform cortex reductions in individuals at high risk for psychosis [29]. A recent study found an inverse relationship between the volume of left fusiform gyrus and the duration of initial untreated period of first-episode psychosis [13]. The visual processing deficits observed in schizophrenia are associated with the abnormalities in this area [30]. Further, Chang et al. [31] found that a prolonged DUP was associated with more severe impairment in visual memory. Fusiform gyrus plays several essential roles in high-level visual processing and recognition. Our findings of fusiform abnormality are consistent with the functional impairment related to DUP as reported in previous studies [30], [31].
Increasing evidence suggests that the gray matter abnormalities associated with DUP may reflect the neurotoxic effect of untreated psychosis disease state [21]; gray matter volume continues to lose gradually throughout the course of illness if without intervention [32], [33]. As structural brain abnormalities are associated with poor treatment response and unfavorable long-term outcome [5], [6], early detection and intervention, therefore minimizing untreated time duration, become critically important in schizophrenia treatment.
In summary, our study examined the relationship between DUP and brain structure using an automated whole brain approach in a clinically well-characterized sample of treatment naive schizophrenia. We found that a prolonged DUP was associated with decreased temporal and occipitotemporal gray matter volumes. Our study has some limitations. The sample size was relative small. Since this was a cross-sectional study, a causal relationship between DUP and the brain abnormalities can’t be drawn. Future longitudinal studies are warranted to confirm our preliminary findings.
Funding Statement
This research was supported by the National Natural Science Foundation of China (grant No. 30900485 and 81270019); and by the National R&D Special Fund for Health Profession (grant No. 201002003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Bachmann S, Bottmer C, Pantel J, Schroder J, Amann M, et al. (2004) MRI-morphometric changes in first-episode schizophrenic patients at 14 months follow-up. Schizophr Res 67: 301–303. [DOI] [PubMed] [Google Scholar]
- 2. Nakamura M, Nestor PG, Levitt JJ, Cohen AS, Kawashima T, et al. (2008) Orbitofrontal volume deficit in schizophrenia and thought disorder. Brain 131: 180–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Selten JP, Veen ND, Hoek HW, Laan W, Schols D, et al. (2007) Early course of schizophrenia in a representative Dutch incidence cohort. Schizophr Res 97: 79–87. [DOI] [PubMed] [Google Scholar]
- 4. Emsley R, Chiliza B, Schoeman R (2008) Predictors of long-term outcome in schizophrenia. Curr Opin Psychiatry 21: 173–177. [DOI] [PubMed] [Google Scholar]
- 5. Crumlish N, Whitty P, Clarke M, Browne S, Kamali M, et al. (2009) Beyond the critical period: longitudinal study of 8-year outcome in first-episode non-affective psychosis. Br J Psychiatry 194: 18–24. [DOI] [PubMed] [Google Scholar]
- 6. Owens DC, Johnstone EC, Miller P, Macmillan JF, Crow TJ (2010) Duration of untreated illness and outcome in schizophrenia: test of predictions in relation to relapse risk. Br J Psychiatry 196: 296–301. [DOI] [PubMed] [Google Scholar]
- 7. Marshall M, Lewis S, Lockwood A, Drake R, Jones P, et al. (2005) Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry 62: 975–983. [DOI] [PubMed] [Google Scholar]
- 8. Perkins DO, Gu H, Boteva K, Lieberman JA (2005) Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry 162: 1785–1804. [DOI] [PubMed] [Google Scholar]
- 9. Angelopoulos EK, Markianos M, Daskalopoulou EG, Hatzimanolis J, Tzemos J (2002) Changes in central serotonergic function as a correlate of duration of illness in paranoid schizophrenia. Psychiatry Res 110: 9–17. [DOI] [PubMed] [Google Scholar]
- 10. Crespo-Facorro B, Roiz-Santianez R, Pelayo-Teran JM, Gonzalez-Blanch C, Perez-Iglesias R, et al. (2007) Caudate nucleus volume and its clinical and cognitive correlations in first episode schizophrenia. Schizophr Res 91: 87–96. [DOI] [PubMed] [Google Scholar]
- 11. Takahashi T, Suzuki M, Tanino R, Zhou SY, Hagino H, et al. (2007) Volume reduction of the left planum temporale gray matter associated with long duration of untreated psychosis in schizophrenia: a preliminary report. Psychiatry Res 154: 209–219. [DOI] [PubMed] [Google Scholar]
- 12. Keshavan MS, Haas GL, Kahn CE, Aguilar E, Dick EL, et al. (1998) Superior temporal gyrus and the course of early schizophrenia: progressive, static, or reversible? J Psychiatr Res 32: 161–167. [DOI] [PubMed] [Google Scholar]
- 13. Bangalore SS, Goradia DD, Nutche J, Diwadkar VA, Prasad KM, et al. (2009) Untreated illness duration correlates with gray matter loss in first-episode psychoses. Neuroreport 20: 729–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Malla AK, Bodnar M, Joober R, Lepage M (2011) Duration of untreated psychosis is associated with orbital-frontal grey matter volume reductions in first episode psychosis. Schizophr Res 125: 13–20. [DOI] [PubMed] [Google Scholar]
- 15. Lappin JM, Morgan K, Morgan C, Hutchison G, Chitnis X, et al. (2006) Gray matter abnormalities associated with duration of untreated psychosis. Schizophr Res 83: 145–153. [DOI] [PubMed] [Google Scholar]
- 16.First MB SRGM (1996) Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV). Washington, DC: American Psychiatric Press, Inc.
- 17. Singh SP, Cooper JE, Fisher HL, Tarrant CJ, Lloyd T, et al. (2005) Determining the chronology and components of psychosis onset: The Nottingham Onset Schedule (NOS). Schizophr Res 80: 117–130. [DOI] [PubMed] [Google Scholar]
- 18. Jackson HJ, McGorry PD, Dakis J, Harrigan S, Henry L, et al. (1996) The inter-rater and test-retest reliabilities of prodromal symptoms in first-episode psychosis. Aust N Z J Psychiatry 30: 498–504. [DOI] [PubMed] [Google Scholar]
- 19. Yung AR, McGorry PD (1996) The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull 22: 353–370. [DOI] [PubMed] [Google Scholar]
- 20. Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261–276. [DOI] [PubMed] [Google Scholar]
- 21.Haijma SV, Van Haren N, Cahn W, Koolschijn PC, Hulshoff PH, et al.. (2012) Brain Volumes in Schizophrenia: A Meta-Analysis in Over 18 000 Subjects. Schizophr Bull. [DOI] [PMC free article] [PubMed]
- 22. Matsumoto H, Simmons A, Williams S, Hadjulis M, Pipe R, et al. (2001) Superior temporal gyrus abnormalities in early-onset schizophrenia: similarities and differences with adult-onset schizophrenia.Am J. Psychiatry158: 1299–1304. [DOI] [PubMed] [Google Scholar]
- 23. Onitsuka T, Shenton ME, Salisbury DF, Dickey CC, Kasai K, et al. (2004) Middle and inferior temporal gyrus gray matter volume abnormalities in chronic schizophrenia: an MRI study. Am J Psychiatry161: 1603–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kuroki N, Shenton ME, Salisbury DF, Hirayasu Y, Onitsuka T, et al. (2006) Middle and inferior temporal gyrus gray matter volume abnormalities in first-episode schizophrenia: an MRI study. Am J Psychiatry163: 2103–2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hu M, Li J, Eyler L, Guo X, Wei Q, et al. (2013) Decreased left middle temporal gyrus volume in antipsychotic drug-naive, first-episode schizophrenia patients and their healthy unaffected siblings. Schizophr Res 144: 37–42. [DOI] [PubMed] [Google Scholar]
- 26.Lappin JM, Dazzan P, Morgan K, Morgan C, Chitnis X, et al.(2007). Duration of prodromal phase and severity of volumetric abnormalities in first-episode psychosis.Br J Psychiatry Suppl 51:s123–127 [DOI] [PubMed]
- 27. Hoffman EA, Haxby JV (2000) Distinct representations of eye gaze and identity in the distributed human neural system for face perception. Nat Neurosci 3: 80–84. [DOI] [PubMed] [Google Scholar]
- 28. Morris RW, Weickert CS, Loughland CM (2009) Emotional face processing in schizophrenia. Curr Opin Psychiatry 22: 140–146. [DOI] [PubMed] [Google Scholar]
- 29. Pantelis C, Yücel M, Wood SJ, McGorry PD, Velakoulis D (2003) Early and late neurodevelopmental disturbances in schizophrenia and their functional consequences. Aust N Z J Psychiatry 37: 399–406. [DOI] [PubMed] [Google Scholar]
- 30. Butler PD, Javitt DC (2005) Early-stage visual processing deficits in schizophrenia. Curr Opin Psychiatry18: 151–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chang WC, Hui CL, Tang JY, Wong GH, Chan SK, et al. (2012) Impacts of duration of untreated psychosis on cognition and negative symptoms in first-episode schizophrenia: a 3-year prospective follow-up study.Psychol Med. 7: 1–11. [DOI] [PubMed] [Google Scholar]
- 32. Vita A, De Peri L, Deste G, Sacchetti E (2012) Progressive loss of cortical gray matter in schizophrenia: a meta-analysis and meta-regression of longitudinal MRI studies.Transl Psychiatry. 2: e190 doi:10.1038/tp.2012.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Asami T, Bouix S, Whitford TJ, Shenton ME, Salisbury DF, et al. (2012) Longitudinal loss of gray matter volume in patients with first-episode schizophrenia: DARTEL automated analysis and ROI validation. Neuroimage 59: 986–996. [DOI] [PMC free article] [PubMed] [Google Scholar]