Abstract
Down’s syndrome (DS) is a developmental disorder associated with intellectual disability (ID). We have previously shown that people with DS engage in very low levels of exercise compared to people with ID not due to DS. Many aspects of the DS phenotype, such as dementia, low activity levels and poor muscle tone, are shared with disorders of mitochondrial origin, and mitochondrial dysfunction has been demonstrated in cultured DS tissue. We undertook a phosphorus magnetic resonance spectroscopy (31P-MRS) study in the quadriceps muscle of 14 people with DS and 11 non-DS ID controls to investigate the post-exercise resynthesis kinetics of phosphocreatine (PCr), which relies on mitochondrial respiratory function and yields a measure of muscle mitochondrial function in vivo. We found that the PCr recovery rate constant was significantly decreased in adults with DS compared to non-DS ID controls (1.7±0.1 min−1 vs 2.1±0.1 min−1 respectively) who were matched for physical activity levels, indicating that muscle mitochondrial function in vivo is impaired in DS. This is the first study to investigate mitochondrial function in vivo in DS using 31P-MRS. Our study is consistent with previous in vitro studies, supporting a theory of a global mitochondrial defect in DS.
Introduction
Down’s syndrome (DS) is a developmental disorder associated with triplication of chromosome 21, and affects 1 in 700–1000 live births [1], [2]. The clinical phenotype in DS is variable and multi-faceted and includes specific physical characteristics and an increased risk for developing sensory deficits, congenital heart defects, early onset Alzheimer’s disease (AD), and hypothyroidism [3]. DS is also associated with obesity and reduced exercise capacity [4]. We have recently reported reduced physical activity levels in DS compared to people with intellectual disability (ID) not due to DS, with the older people with DS being less active than their younger counterparts [5]. As this use of an ID control group eliminates a number of general (social and environmental) factors that might explain this observation, we postulated an underlying age-related pathophysiology which limits activity in people with DS, an obvious candidate for which is mitochondrial dysfunction [5].
Mitochondrial generation of adenosine triphosphate (ATP) is fundamental to cellular energy turnover, and defects of mitochondrial function manifest in a variety of ways in specific clinical syndromes and in chronic diseases. In general defective mitochondrial function in vivo results in limited capacity for ATP synthesis, and may be associated with increased intracellular levels of toxic reactive oxygen species (ROS). In vitro studies in DS have demonstrated mitochondrial abnormalities including mtDNA mutations [6], global dysregulation of genes associated with mitochondrial function in the foetus [7], and mitochondrial enzyme deficiency [8]. However, we are aware of no studies that have assessed mitochondrial function in vivo in DS. We therefore undertook a study of DS mitochondrial function in vivo in skeletal muscle using 31P magnetic resonance spectroscopy (31P-MRS), which offers a non-invasive method for measuring mitochondrial function in vivo by analysing the post-exercise recovery kinetics of phosphocreatine (PCr), a process which relies on mitochondrial production of ATP [9]. We postulated that participants with DS would demonstrate a slowed recovery of PCr, indicating a defect of mitochondrial function in vivo, compared to control participants with similar levels of ID but not due to DS.
Methods
Ethics Statement
Ethical approval for the study was granted by the Cambridgeshire 3 Research Ethics Committee and all studies were conducted in accordance with the principles of the Declaration of Helsinki. Only participants judged to have the capacity to consent in accordance with the Mental Capacity Act (2005) were recruited. Written consent was obtained from all participants.
Recruitment, Screening and Familiarisation
Participants with ID not due to DS were deliberately chosen as controls for the DS group in an attempt to match for level of intellectual disability, environmental factors and fitness levels. Participants were recruited from a database of participants in a previous study [5] and were initially selected to match as far as possible age, gender, BMI and physical activity levels between groups. We scanned 29 individuals, but after detailed consideration when matching activity levels of the two groups, selected for analysis 14 DS and 11 ID participants. Inclusion criteria were: mild to moderate ID; known to ID services; aged ≥12 y; able to walk unaided; and able to understand protocol instructions. Exclusion criteria were: smoking; autism spectrum disorder; diabetes mellitus, cardiovascular disease; medication known to effect energy metabolism; and standard magnet contraindications. Prior to inclusion, participants underwent a preliminary screening at their home residence to determine whether they would be able to understand and complete the study protocol, and to assess their capacity to consent. Two weeks prior to the experimental measurements participants were shown a video and underwent at least two familiarisation sessions at their home residence to ensure they were comfortable with the in-scanner exercise protocol. All participants underwent at least four separate practice trials.
Measurements of Height, Weight, and Body Fat
Weight was measured to the nearest 0.1 kg with the participant dressed in lightweight clothing and without shoes, using a calibrated electronic scale (Seca 813, Seca Ltd, UK). Height was measured by the stretch stature method to the nearest 0.5 cm using a portable stadiometer (Seca Leicester Height Measure, Invicta Plastics, UK). Percentage body fat was assessed by bioelectrical impedance using a TBF−521 analyser (Tanita Corp., Japan) in accordance with the manufacturer's instructions.
Measurement of Leg Strength
Two weeks prior to the experimental measurements isometric leg strength was measured at the participants’ home residence using a portable back and leg dynamometer (Takei, model T.K.K. 5162, Japan) according to a protocol [10] which has been validated in both adolescents and adults [10], [11].
Assessment of Total Physical Activity
Habitual physical activity was assessed using an Actigraph GT1M accelerometer (Actigraph LLC, Pensacola, FL, USA) for seven consecutive days. Accelerometers have been used previously to assess physical activity in a number of studies in DS [12]–[14]. The total physical activity measure was used as a measure of habitual physical activity in these participants and not used to make inferences on energy expenditure [14]. These participants formed part of a previous report on activity in these cohorts and the methodology and analysis were as previously described in that study [5].
31P-MRS Measurement of Post-exercise PCr Recovery Kinetics
31P-MRS data were acquired on a Siemens MAGNETOM 3T Verio scanner. Participants were asked to arrive having refrained from strenuous exercise for at least 24 h and having abstained from alcohol, caffeine, and food for the preceding 24 h, 6 h, and 2 h respectively. The volunteers were placed supine and a 9 cm diameter surface coil attached to the right quadriceps (1/3 distal). An MR-compatible weight was attached to the right ankle that was proportional to their previously-determined leg strength, such that the PCr concentration after exercise was targeted to fall by 20–30% of basal levels, thereby avoiding any significant lowering of pH which is known to complicate interpretation of PCr recovery kinetics. The exercise paradigm consisted of 1 min rest, 1 min knee extensions (0.5 Hz), then 4 min rest. This was then repeated to permit two measurements of post-exercise PCr recovery, results from the analysis of which were averaged. Spectra were acquired with a TR of 2s and as previously described [15]. The PCr recovery rate constant, k, was found using a two parameter monoexponential fit to the equation: PCr(t) = PCrinitial+(PCrend – PCrinitial)(1-exp(-k.t)), where t is the time from the start of recovery, PCrinitial and PCrend are the PCr content at the initial and end of recovery phases respectively. MATLAB software (The MathWorks, Natick, MA, USA) was used to calculate PCrend from the mean end-recovery PCr values and then to obtain k and PCrinitial by the Levenberg Marquardt fitting algorithm. All spectra were analysed in jMRUI [16] and fitted using the AMARES [17] algorithm with prior knowledge. The intracellular pH was determined from the chemical shift of inorganic phosphate relative to PCr. A fully relaxed spectrum with 8 averages was also obtained for the calculation of metabolite ratios and concentrations. The conventional assumption was made that the intracellular concentration of ATP was 8.2 mM, and the free concentration of adenosine diphosphate (ADP) was calculated using established methods [18] with the conventional assumption (in the absence of any reported data in DS) of total creatine = 42.5 mM. The signal-to-noise ratio (SNR) of the PCr recovery sequence was defined as the (mean signal)/SD of the recovered PCr values (20 points, TR = 2s). High subcutaneous adipose tissue thicknesses can result in a low SNR and uncertainty in the accuracy of the PCr recovery rate constant, and hence a cut off value of SNR <35 was chosen for exclusion of k values.
Statistics
Statistical analysis was performed in IBM SPSS Statistics 21 (IBM Inc., Armonk, NY, USA), with significance set at p<0.05. A two-tailed independent samples t-test was performed to detect significant differences between groups.
Results
Participants with ID not due to DS and participants with DS were matched for age, gender, BMI and physical activity levels, and were found to have similar percentage body fat (Table 1). However, the DS were significantly shorter than the ID controls (p = 0.001). No significant correlation of total physical activity with age was found in either group, or altogether.
Table 1. Characteristics of the participants with Down’s syndrome (DS) and those with a non Down’s syndrome related intellectual disability (ID).
| DS (n = 14) | ID (n = 11) | p-value | |
| Age (yrs) | 32.7 (2.2) | 29.8 (2.7) | 0.410 |
| Gender | 8 M, 6 F | 5 M, 6F | 0.580 |
| Weight (kg) | 72.2 (3.2) | 80.0 (4.9) | 0.175 |
| Height (m) | 1.55 (0.03) | 1.72 (0.04) | 0.001 |
| BMI (kg/m2) | 30.4 (1.7) | 26.9 (1.1) | 0.100 |
| Percentage body fat (%) | 27.5 (2.7) | 27.5 (3.1) | 0.991 |
Data presented are mean (SEM).
M, Male; F, Female; BMI, body mass index.
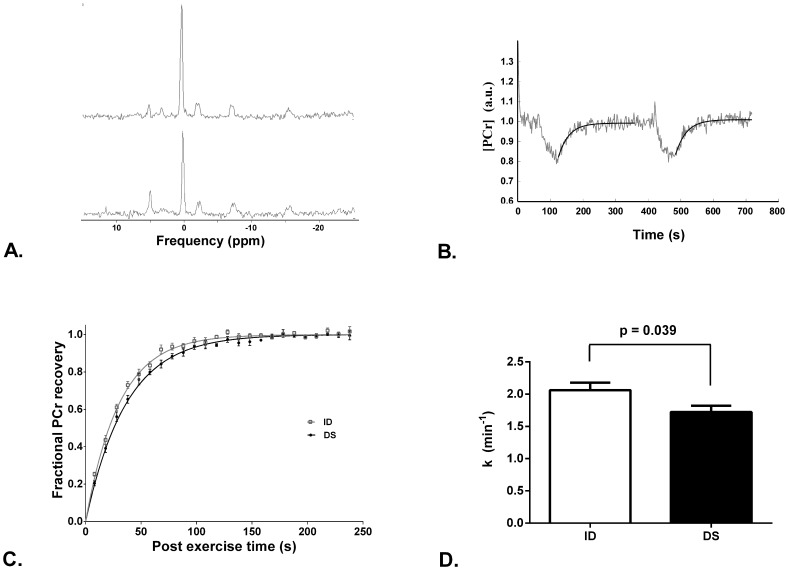
Four participants with DS were eliminated from the calculation of k due to not meeting the SNR requirements described in the Methods section, and hence the 31P-MRS and accelerometry results in Table 2 represent the DS group with n = 10. Post-exercise PCr recovery was significantly slowed in the DS group compared with ID (p = 0.039, Figure 1). Neither the resting nor end-exercise intracellular pH (pHi) differed significantly between those with DS and those with ID without DS (Table 2), and end-exercise pHi was not significantly lower than resting pHi in either group. No differences in resting metabolite concentrations nor their ratios were found between the groups (Table 2). There was no significant correlation between total physical activity and the PCr recovery rate constant, k in either group, or altogether.
Table 2. Accelerometry and 31P-MRS measurements for the participants with Down’s syndrome (DS) and those with a non Down’s syndrome related intellectual disability (ID).
| Category | Subcategory | DS (n = 10) | ID (n = 11) | p-value |
| Accelerometry | Total physical activity (counts/min) | 542.5 (25.3) | 611.6 (35.1) | 0.133 |
| 31P-MRS | Exercise weight (kg) | 2.03 (0.10) | 2.77 (0.29) | 0.031 |
| k (min−1) | 1.72 (0.10) | 2.06 (0.12) | 0.039 | |
| Resting Pi:PCr | 0.086 (0.005) | 0.096 (0.006) | 0.216 | |
| Resting PDE:PCr | 0.123 (0.011) | 0.115 (0.007) | 0.567 | |
| Resting Pi:PDE | 0.73 (0.06) | 0.86 (0.07) | 0.213 | |
| Resting [Pi] (mM) | 2.85 (0.16) | 2.96 (0.17) | 0.633 | |
| Resting [PDE] (mM) | 4.07 (0.35) | 3.58 (0.22) | 0.244 | |
| Resting [PCr] (mM) | 33.4 (0.7) | 31.2 (0.9) | 0.073 | |
| End exercise [PCr] (mM) | 26.5 (1.5) | 24.3 (0.9) | 0.211 | |
| Resting [ADP] (µM) | 14.7 (1.8) | 20.2 (2.3) | 0.078 | |
| End exercise [ADP] (µM) | 36.8 (4.9) | 45.2 (4.6) | 0.227 | |
| Resting pHi | 7.017 (0.015) | 7.036 (0.007) | 0.281 | |
| End exercise pHi | 7.061 (0.010) | 7.068 (0.009) | 0.648 |
Data presented are mean (SEM).
k, PCr recovery rate constant; [Pi], concentration of inorganic phosphate; [PCr], concentration of phosphocreatine; [PDE], concentration of phosphodiester; [ADP], concentration of adenosine diphosphate; pHi, intracellular pH.
Figure 1. 31P-MRS measures of mitochondrial function.
(A) Representative single spectra (NA = 1) at rest (upper) and near end exercise (lower), with 2 Hz line broadening applied for illustrative purposes. (B) Corresponding PCr timecourse to the spectra in A, which illustrates the typical [PCr] end-exercise depletion in this study. The SNR of this timecourse was 46, significantly below average. The black line represents the monoexponential fit to both PCr recoveries. The recovery time constant, k, was 1.87 min−1 and 1.83 min−1 for recovery from exercise bouts 1 and 2 respectively. (C) Mean fractional PCr recovery curves for physical activity matched ID (grey squares; n = 11) and DS (black circles; n = 10). Five spectra were averaged to give a time resolution of 10 seconds for clarity in this figure. The monoexponential fit using the mean recovery rate constant is shown for ID (grey line) and DS (black line). (D) Recovery rate constant (k) for matched physical activity groups of ID (white bars; n = 11) and for DS (black bars; n = 10). In C–D, data are mean +/− SEM.
Discussion
We found significantly slower post-exercise PCr recovery in skeletal muscle of the participants with DS compared with the non-DS ID control participants. Post-exercise PCr recovery, conveniently measured as the recovery rate constant, which was 16% lower in the DS participants, is a measure of mitochondrial function in vivo which integrates the contributions of muscle mitochondrial numbers, the mitochondrial content of enzymes, transporters and respiratory chain complexes, the activity of relevant cytosolic enzymes, and the whole-body cardiorespiratory physiology affecting substrate and oxygen supply to active muscle [19]. In exercise of the kind used here the exercising muscle mass is very small (compared e.g. to bicycle ergometry [20]), and cardiovascular limitations to this measure are normally negligible. Our participants with DS had no clinical evidence of cardiovascular or pulmonary disease, and therefore no reason to suppose that the defect we identified lies ‘upstream’ of the mitochondrion. The likeliest explanation is either a lower mitochondrial content, or a defect in intrinsic mitochondrial metabolism.
There are various lines of in vitro evidence to support, or at least parallel, our findings of mitochondrial dysfunction in vivo in DS. Previous in vitro studies in DS have shown mtDNA mutations or mitochondrial dysfunction in brain [6], [21]–[23] and dysregulation of genes associated with mitochondrial function in foetal heart tissue [7]. More specifically lower mRNA levels of complex I and decreased protein levels in complex I subunits [21] as well as decreased levels of complex V [24] have been identified in the brains of people with DS. Levels of mitochondrial enzymes in platelets, including cytochrome oxidase (COX), have been shown to be significantly lower in people with DS compared with controls [8]. There is also evidence of compensation for mitochondrial inefficiency, including a 25% increase in mitochondrial mass of fibroblasts in people with DS [25]. A recent study by Helguera et.al. [26] has shown that mitochondria move more slowly in DS neurons compared with controls, although there were higher numbers of moving mitochondria in DS at any given time that may be a compensatory mechanism. Collectively the results from these studies suggest a systemic long standing dysfunction of mitochondria in DS. To our knowledge, there have been no such studies in DS investigating skeletal muscle, which for practical reasons is the only tissue in which mitochondrial function in vivo (i.e. the capacity for mitochondrial ATP synthesis) can be quantified non-invasively [19]. The results of our in vivo study in skeletal muscle support this theory of a global mitochondrial defect.
We have previously shown that people with DS have highly sedentary lifestyles compared to their non-DS ID peers [5]. Similarly low levels of habitual physical activity have recently been reported in people with mitochondrial disease [27]. In addition, the authors of that study found a high prevalence of obesity, and a moderate negative correlation between steps walked per day and disease severity. We suggest that low levels of activity, the reduced capacity for exercise [4] and high rates of obesity [28] in DS could be accounted for in part by reduced mitochondrial ability of skeletal muscle to generate ATP.
However, any cross-sectional study relating habitual activity to muscle energetics (in this case, muscle mitochondrial capacity) must address the issue of causal direction; whilst mitochondrial dysfunction in vivo can certainly contribute to reduced habitual activity, it is also possible that reduced activity may lead to impaired muscle mitochondrial function. In the present study we have tried to address this by matching the DS and non-DS ID groups for physical activity. The data does not exist to say how much a ‘primary’ reduction in habitual activity would be necessary to yield the 16% defect we observed in mitochondrial function in vivo in DS compared to non-DS ID, nor conversely how much a primary mitochondrial defect (in mitochondrial numbers or intrinsic mitochondrial activity) of this size would be expected, on its own, to limit activity. We do know that the ‘slope’ of the relationship between these two measures is steep, in the sense that symptomatic primary mitochondrial myopathy is associated with on average a 40–50% defect in skeletal muscle mitochondrial capacity as measured by 31P-MRS [29]. The defect we have identified here is therefore likely to be functionally significant, even if we cannot be sure whether it is cause or effect (or both).
Precocious ageing and Alzheimer’s disease (AD) are strikingly common in DS, with almost 100% of people with DS eventually developing the neuropathology of AD [30], which is likely to be linked to the overexpression of the amyloid precursor protein gene (APP) resulting in a lifelong excess of beta-amyloid (Aβ). The role of mitochondrial dysfunction in neurodegenerative diseases is well-established [31]. Aβ has been shown to be imported into mitochondria where it inhibits function [32], [33], and data indicate that mitochondrial dysfunction contributes to the development of DSAD [34]. Aβ deposits have been seen in non-brain tissue of people with AD, DS and in normal ageing [35]. Further, transfer of the βAPP gene into cultured normal human muscle leads to decreased mitochondrial enzyme activity and structural abnormalities [36]. This demonstrates that mitochondrial interaction with Aβ is not limited to brain, and suggests, further, that mitochondrial dysfunction quantified in muscle in vivo, as in the current study, may provide insight into Aβ and mitochondria in brain. Mitochondrial dysfunction and mutations of mtDNA are a major hallmark of human ageing [37], suggesting that mitochondria may underlie the precocious biological ageing that is characteristic of DS. In the current study, there was no significant correlation with age in the DS group (p = 0.165, data not shown) although the eldest person in the group was only 44 y.
Low activity levels in DS are associated with reduced life expectancy, irrespective of heart disease [38]. Increasing mobility of people with DS should therefore improve well-being as well as mortality. Furthermore, high levels of exercise in people over 65 y in the general population has been shown to be protective against cognitive decline [39], adding further support to the notion that reduced habitual activity in DS may impact on the rate and severity of dementia, although mitochondrial dysfunction may underlie both these aspects of the phenotype. Understanding reasons for reduced habitual activity in DS, including the role of mitochondrial dysfunction and accumulation of mtDNA mutations, may be key to a number of health issues associated with the syndrome.
Acknowledgments
We are grateful to Louise McGrath for help in acquiring the data. We thank all the participants who took part in the study and the support workers and parents for supporting the participants during the study. We acknowledge Dr Dan Gordon, Anglia Ruskin University, for helpful discussions and the loan of the portable back and leg dynamometer.
Funding Statement
The study was funded by grants from the DS Association, the Special Olympics and the Health Foundation. ACP was supported by a grant from the DS Association, AS by core staff funding from the National Institute for Health Research (NIHR)/Wellcome Trust Cambridge Clinical Research Facility, and AJH by funding from the Health Foundation and the NIHR Collaborations in Leadership for Applied Health Research (CLAHRC) for Cambridgeshire and Peterborough. The authors are grateful for their support. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Frid C, Drott P, Lundell B, Rasmussen F, Anneren G (1999) Mortality in Down's syndrome in relation to congenital malformations. J Intellect Disabil Res 43 (Pt 3): 234–241. [DOI] [PubMed] [Google Scholar]
- 2. Stoll C, Alembik Y, Dott B, Roth MP (1998) Study of Down syndrome in 238,942 consecutive births. Ann Genet 41: 44–51. [PubMed] [Google Scholar]
- 3. Roizen NJ, Patterson D (2003) Down's syndrome. Lancet 361: 1281–1289. [DOI] [PubMed] [Google Scholar]
- 4. Mendonca GV, Pereira FD, Fernhall B (2010) Reduced exercise capacity in persons with Down syndrome: cause, effect, and management. Ther Clin Risk Manag 6: 601–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Phillips AC, Holland AJ (2011) Assessment of objectively measured physical activity levels in individuals with intellectual disabilities with and without Down's syndrome. PLoS One 6: e28618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Coskun PE, Wyrembak J, Derbereva O, Melkonian G, Doran E, et al. (2010) Systemic mitochondrial dysfunction and the etiology of Alzheimer's disease and down syndrome dementia. J Alzheimers Dis 20 Suppl 2S293–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Conti A, Fabbrini F, D'Agostino P, Negri R, Greco D, et al. (2007) Altered expression of mitochondrial and extracellular matrix genes in the heart of human fetuses with chromosome 21 trisomy. BMC Genomics 8: 268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Prince J, Jia S, Bave U, Anneren G, Oreland L (1994) Mitochondrial enzyme deficiencies in Down's syndrome. J Neural Transm Park Dis Dement Sect 8: 171–181. [DOI] [PubMed] [Google Scholar]
- 9. Larson-Meyer DE, Newcomer BR, Hunter GR, McLean JE, Hetherington HP, et al. (2000) Effect of weight reduction, obesity predisposition, and aerobic fitness on skeletal muscle mitochondrial function. Am J Physiol Endocrinol Metab 278: E153–161. [DOI] [PubMed] [Google Scholar]
- 10. Coldwells A, Atkinson G, Reilly T (1994) Sources of variation in back and leg dynamometry. Ergonomics 37: 79–86. [DOI] [PubMed] [Google Scholar]
- 11. Jawis MN, Singh R, Singh HJ, Yassin MN (2005) Anthropometric and physiological profiles of sepak takraw players. Br J Sports Med 39: 825–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Whitt-Glover MC, O'Neill KL, Stettler N (2006) Physical activity patterns in children with and without Down syndrome. Pediatr Rehabil 9: 158–164. [DOI] [PubMed] [Google Scholar]
- 13. Shields N, Dodd KJ, Abblitt C (2009) Do children with Down syndrome perform sufficient physical activity to maintain good health? A pilot study. Adapt Phys Activ Q 26: 307–320. [DOI] [PubMed] [Google Scholar]
- 14. Agiovlasitis S, Motl RW, Fahs CA, Ranadive SM, Yan H, et al. (2011) Metabolic rate and accelerometer output during walking in people with Down syndrome. Med Sci Sports Exerc 43: 1322–1327. [DOI] [PubMed] [Google Scholar]
- 15. Sleigh A, Raymond-Barker P, Thackray K, Porter D, Hatunic M, et al. (2011) Mitochondrial dysfunction in patients with primary congenital insulin resistance. J Clin Invest 121: 2457–2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Naressi A, Couturier C, Devos JM, Janssen M, Mangeat C, et al. (2001) Java-based graphical user interface for the MRUI quantitation package. MAGMA 12: 141–152. [DOI] [PubMed] [Google Scholar]
- 17. Vanhamme L, van den Boogaart A, Van Huffel S (1997) Improved method for accurate and efficient quantification of MRS data with use of prior knowledge. J Magn Reson 129: 35–43. [DOI] [PubMed] [Google Scholar]
- 18. Arnold DL, Matthews PM, Radda GK (1984) Metabolic recovery after exercise and the assessment of mitochondrial function in vivo in human skeletal muscle by means of 31P NMR. Magn Reson Med 1: 307–315. [DOI] [PubMed] [Google Scholar]
- 19. Kemp GJ, Brindle KM (2012) What do magnetic resonance-based measurements of Pi->ATP flux tell us about skeletal muscle metabolism? Diabetes 61: 1927–1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mortensen SP, Damsgaard R, Dawson EA, Secher NH, Gonzalez-Alonso J (2008) Restrictions in systemic and locomotor skeletal muscle perfusion, oxygen supply and VO2 during high-intensity whole-body exercise in humans. J Physiol 586: 2621–2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim SH, Fountoulakis M, Dierssen M, Lubec G (2001) Decreased protein levels of complex I 30-kDa subunit in fetal Down syndrome brains. J Neural Transm Suppl: 109–116. [DOI] [PubMed]
- 22. Busciglio J, Pelsman A, Wong C, Pigino G, Yuan M, et al. (2002) Altered metabolism of the amyloid beta precursor protein is associated with mitochondrial dysfunction in Down's syndrome. Neuron 33: 677–688. [DOI] [PubMed] [Google Scholar]
- 23. Kim SH, Vlkolinsky R, Cairns N, Lubec G (2000) Decreased levels of complex III core protein 1 and complex V beta chain in brains from patients with Alzheimer's disease and Down syndrome. Cell Mol Life Sci 57: 1810–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee SH, Lee S, Jun HS, Jeong HJ, Cha WT, et al. (2003) Expression of the mitochondrial ATPase6 gene and Tfam in Down syndrome. Mol Cells 15: 181–185. [PubMed] [Google Scholar]
- 25. Valenti D, Tullo A, Caratozzolo MF, Merafina RS, Scartezzini P, et al. (2010) Impairment of F1F0-ATPase, adenine nucleotide translocator and adenylate kinase causes mitochondrial energy deficit in human skin fibroblasts with chromosome 21 trisomy. Biochem J 431: 299–310. [DOI] [PubMed] [Google Scholar]
- 26. Helguera P, Seiglie J, Rodriguez J, Hanna M, Helguera G, et al. (2013) Adaptive downregulation of mitochondrial function in down syndrome. Cell Metab 17: 132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Apabhai S, Gorman GS, Sutton L, Elson JL, Plotz T, et al. (2011) Habitual physical activity in mitochondrial disease. PLoS One 6: e22294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bell AJ, Bhate MS (1992) Prevalence of overweight and obesity in Down's syndrome and other mentally handicapped adults living in the community. J Intellect Disabil Res 36 (Pt 4): 359–364. [DOI] [PubMed] [Google Scholar]
- 29. Taylor DJ, Kemp GJ, Radda GK (1994) Bioenergetics of skeletal muscle in mitochondrial myopathy. J Neurol Sci 127: 198–206. [DOI] [PubMed] [Google Scholar]
- 30. Lai F, Williams RS (1989) A prospective study of Alzheimer disease in Down syndrome. Arch Neurol 46: 849–853. [DOI] [PubMed] [Google Scholar]
- 31. Moreira PI, Cardoso SM, Santos MS, Oliveira CR (2006) The key role of mitochondria in Alzheimer's disease. J Alzheimers Dis 9: 101–110. [DOI] [PubMed] [Google Scholar]
- 32. Devi L, Anandatheerthavarada HK (2010) Mitochondrial trafficking of APP and alpha synuclein: Relevance to mitochondrial Dysfunction in Alzheimer’s and Parkinson’s diseases. Biochim Biophys Acta 1802: 11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hansson Petersen CA, Alikhani N, Behbahani H, Wiehager B, Pavlov PF, et al. (2008) The amyloid beta-peptide is imported into mitochondria via the TOM import machinery and localized to mitochondrial cristae. Proc Natl Acad Sci U S A 105: 13145–13150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Coskun PE, Busciglio J (2012) Oxidative Stress and Mitochondrial Dysfunction in Down's Syndrome: Relevance to Aging and Dementia. Curr Gerontol Geriatr Res 2012: 383170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Joachim CL, Mori H, Selkoe DJ (1989) Amyloid beta-protein deposition in tissues other than brain in Alzheimer's disease. Nature 341: 226–230. [DOI] [PubMed] [Google Scholar]
- 36. Askanas V, McFerrin J, Baque S, Alvarez RB, Sarkozi E, et al. (1996) Transfer of beta-amyloid precursor protein gene using adenovirus vector causes mitochondrial abnormalities in cultured normal human muscle. Proc Natl Acad Sci U S A 93: 1314–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lopez-Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013) The hallmarks of aging. Cell 153: 1194–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Eyman RK, Call TL (1991) Life expectancy of persons with Down syndrome. Am J Ment Retard 95: 603–612. [PubMed] [Google Scholar]
- 39. Lytle ME, Vander Bilt J, Pandav RS, Dodge HH, Ganguli M (2004) Exercise level and cognitive decline: the MoVIES project. Alzheimer Dis Assoc Disord 18: 57–64. [DOI] [PubMed] [Google Scholar]