Abstract
Objective
To define long-term health state utility outcomes in patients undergoing endoscopic sinus surgery (ESS) for refractory chronic rhinosinusitis (CRS)
Study Design
Prospective, longitudinal cohort study
Methods
The SF-12 survey was issued to the 168 patients who were enrolled in an initial study evaluating short-term utility outcomes following ESS. SF-12 responses were converted into SF-6D utility scores using the University of Sheffield algorithm. The primary outcome was mean overall long-term utility level following ESS. Secondary outcomes evaluated annual utility level following ESS and utility outcomes for different subgroups of patients with CRS.
Results
A total of 83 patients provided long-term health state utility outcomes. The mean overall long-term utility level was 0.80 at a mean follow-up of 5.2 years after ESS. Compared to the baseline (0.67) and short-term follow-up (0.75) utility levels in this group, there was a significant improvement at the long-term period (p=0.002). 54% (45/83) of patients achieved long-term postoperative utility scores higher than the United States (US) norm of 0.81. There was a significant improvement in utility scores for all subsequent years after ESS compared to preoperative responses (all p<0.028). All subgroups of CRS received significant long-term utility improvements (all p<0.001), while those undergoing revision ESS demonstrated continued improvement past the short-term postoperative period.
Conclusion
This study has demonstrated that patients with refractory CRS achieve stable mean long-term utility levels following ESS and often return to a health state comparable to US population norms.
Keywords: Utility, quality of life, chronic rhinosinusitis, sinusitis, endoscopic sinus surgery
Introduction
Patient ‘utility’ level measures a person's preference for being in their current health state. A utility is a particularly informative clinical outcome since it provides a general quality of life metric that can be compared across several disease states. Utility scores are recorded between 1 [perfect health] and 0 [death] and can be obtained thru traditional gaming approaches (i.e. Standard gamble or Time trade-off) or generic surveys such as the EQ-5D1,2, Health Utilities Index (HUI)3,4, and Short-form 6D (SF-6D)5.
Cost-effectiveness analysis (CEA) is the evaluation of costs and consequences of alternative interventions using clinical outcomes in ‘natural units’. The natural units in a CEA tend to be disease-specific outcomes, such as symptom-free days, complications avoided, or cases diagnosed. When the CEA uses the generic utility level as the outcome, some authors have labeled this a cost-utility analysis (CUA). The major advantage of CUA over a CEA is that outcomes can be compared across different disease states and therefore can help elucidate the opportunity cost of shifting health care resources between interventions. The goal of a CUA is to inform policy makers who are attempting to maximize efficient allocation of health care resources while functioning within a constrained budget.
Chronic rhinosinusitis (CRS) is typically a non-life threatening condition and thus the detrimental health effects may influence a patient's quality of life until the time of death. The chronicity of disease creates an inherent challenge in performing a strong CUA for CRS, since it is not feasible to follow all patients until death. Therefore, assumptions, based on extrapolations from the best available utility data, are required to define long-term utility outcomes.
The purpose of this study was to evaluate long-term utility outcomes in patients undergoing ESS for CRS. When using the SF-6D minimally important difference (MID) of 0.036, we hypothesized that long-term utility scores would still show a durable improvement over baseline scores by at least one MID. When combined with short-term utility outcomes, the results from this study will provide a trend in utility outcomes over time that may be used to inform future cost utility analyses and ultimately patient, provider, and policy decision-making.
Methods
Patient Selection and Survey Distribution
We have previously reported short-term utility outcomes after ESS from a cohort of patients with CRS7. Each of these patients had CRS according to the 2007 Adult Sinusitis Guideline and was enrolled in an observational study between 2004-2009 to evaluate outcomes before and after ESS. All patients were adults (age > 18) at the time of entry into the cohort and had previously completed the Medical Outcomes Study Short-Form-36 version 1.0 (SF-36) prior to ESS and at least once following surgery.
The Medical Outcomes Study Short-Form-12 version 1.0 survey (SF-12) was mailed to all original cohort members from our initial utility outcomes study (n=168) along with an invitation to participate in the current study. Each patient was asked to complete the SF-12 survey with regard to their current overall state of health. Exclusion criteria included the inability to fully complete questionnaires or cooperate with study evaluations in English. A comparison of baseline characteristics of survey respondents to the initial cohort characteristics was performed to evaluate for potential selection bias. Study protocol was approved by the Institutional Review Board and informed consent was obtained from each study participant.
Utility Score Calculation
The SF-12 is an abbreviation of the SF-36 instrument which contains physical and mental health domain scores which are combined, scored, and weighted (standardized range: 0-100), with higher scores indicating a higher (better) level of health8. Health state utility scores (SF-6D) are derived from responses to 6 separate items indicated on both the SF-36 and SF-12 using a commercially available weighted algorithm derived by the Department of Health Economics and Decision Science at the University of Sheffield, Sheffield, United Kingdom9. This algorithm application is compatible with most commercially available statistical software packages and was used to calculate standardized health state utility values (range: 0.0= “death” − 1.0= “perfect health”) from long-term follow-up survey responses provided by each study subject. Baseline and short-term utility scores were previously calculated through responses originally provided on the SF-36survey done during the original study for each subject and calculated using the same methodology. This investigation provided health state utility scores associated with a third “long-term” follow-up time-point, which allowed for a long-term utility trend to be generated.
Data Compilation and Statistical Analysis
All returned survey data was collected, transcribed, and manually entered into a relational database by a trained study coordinator using standardized clinical research forms. Returned survey responses on the SF-12 instrument were de-identified and securely stored during the data collection period (Microsoft Excel; Microsoft Corp., Redmond, WA.). Statistical analysis was accomplished using commercially available statistical software (SPSS v. 19.0; SPSS Inc., Chicago, IL.). The main outcome of interest was operationalized by the mean change in long-term health state utility score (post-treatment score minus baseline score).
Descriptive statistics were provided for patient demographics including means, standard deviations (SD), frequencies, and ranges, where appropriate. Wilcoxon signed-rank and McNemars chi-square tests were used to assess improvement in health state utility over time between paired follow-up time points. Mann-Whitney U tests were used to evaluate differences in utility scores between subject comorbidity at each distinct time point. Repeated measures general linear models (GLM) were used to evaluate significant trends in utility scores over time and whether various comorbid conditions (nasal polyposis and history of prior ESS) were significant covariates of utility improvement while controlling for correlation between time points. Repeated measure GLM's were built using utility scores at each time point as within-subject factors (Level III) and evaluated potential interactive effects between time and cormobid factors using an exchangeable covariance matrix design. Greenhouse-Geisser corrected F-tests, with corresponding degrees of freedom, were reported if model sphericity was violated. A p-value < 0.05 was considered a statistically significant difference.
Results
Subject characteristics
In this prospective longitudinal study, we obtained preoperative/baseline, short-term postoperative, and long-term postoperative utility outcomes in a total 83 patients who received ESS for refractory CRS (83/168; response rate of 50%). Mean long-term follow-up was 5.2 years (62.5 (12.7) months/range: 37 – 91 months). The average subject age was 53.5(12.3) years old (range: 24-79) with a higher proportion of males (n=45; 54.2%) than females. Comorbid characteristics included 30 subjects with asthma (36.1%), 20 subjects with allergies (24.1%), and 7 subjects with acetylsalicylic acid intolerance (8.4%). There were no baseline differences detected between the original cohort (n=168) and the long-term response cohort (n=83).
Mean overall Long-term utility
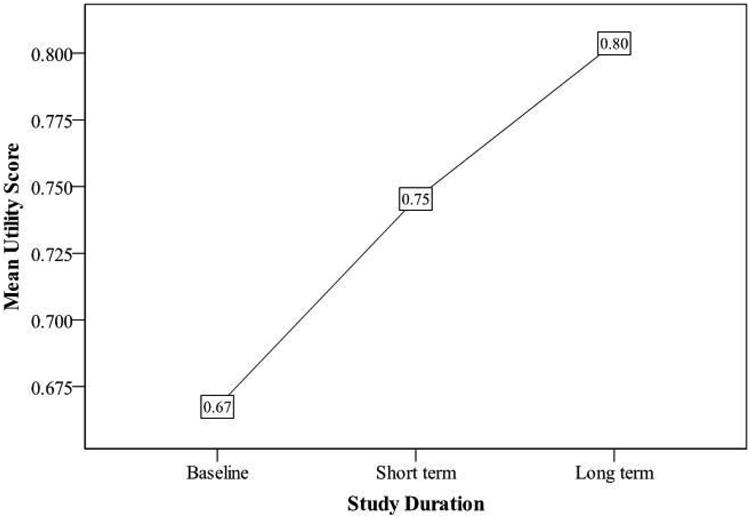
Preoperative utility assessments demonstrated an overall mean score of 0.67(0.11) (range: 0.49 – 0.96). At an average short-term postoperative follow-up of 1.5 years (17.5(6.3) months) the overall mean utility score was 0.75(0.13) which demonstrated a significant utility improvement of 0.08(0.12) (p<0.001). With an average long-term postoperative follow-up of 5.2 years (62.5(12.7) months) the mean utility score was 0.80(0.13) (range: 0.46 – 1.00) with an overall significant improvement from baseline (F(1.79, 141.04)=15.14; p<0.001). 54% (45/83 subjects) of all long-term respondents reported a utility score ≥ 0.81, which is the reported US utility population norm. The mean trend in utility scores for all 83 subjects with long-term follow-up is shown in Figure 1.
Figure 1. Overall long-term postoperative trend in health state utility level following ESS.
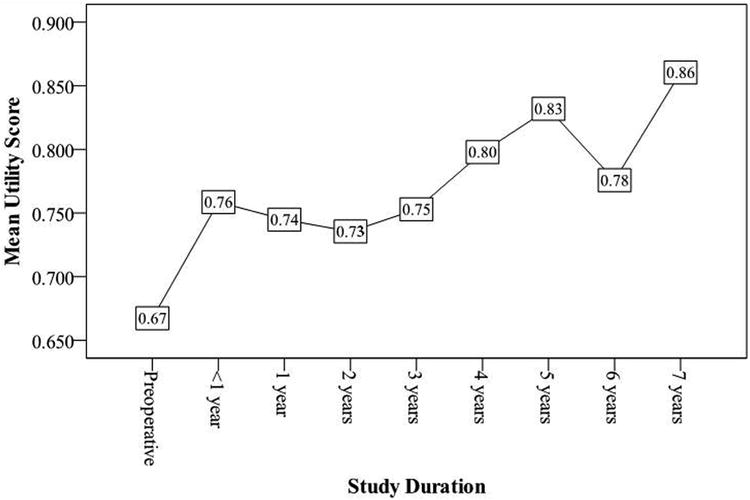
Mean utility values for each year after ESS
Following ESS, a trend in utility outcomes could be generated since study subjects completed the SF-6D evaluation at various times after surgery. The frequency of follow-up is described in Table 1 while the breakdown of mean utility scores for each year following ESS is outlined in Figure 2. Subjects with less than 1 year follow-up after ESS reported significant improvements in utility scores (p=0.008). Continued average improvements in utility scores were durable and significant for all subsequent years after ESS compared to preoperative responses (all p<0.028).
Table 1. Mean utility scores per year following ESS.
| Follow-up time: | Follow-up Term: | N | Utility Score Mean(SD) |
|---|---|---|---|
| < 1 year | Short | 9 | 0.76(0.15) |
| 1 year | Short | 62 | 0.74(0.13) |
| 2 years | Short | 10 | 0.73(0.11) |
| 3 years | Long | 10 | 0.75 (0.14) |
| 4 years | Long | 16 | 0.80 (0.11) |
| 5 years | Long | 29 | 0.83 (0.12) |
| 6 years | Long | 22 | 0.78 (0.14) |
| 7 years | Long | 6 | 0.86 (0.12) |
Figure 2. Annual postoperative utility trend following ESS.
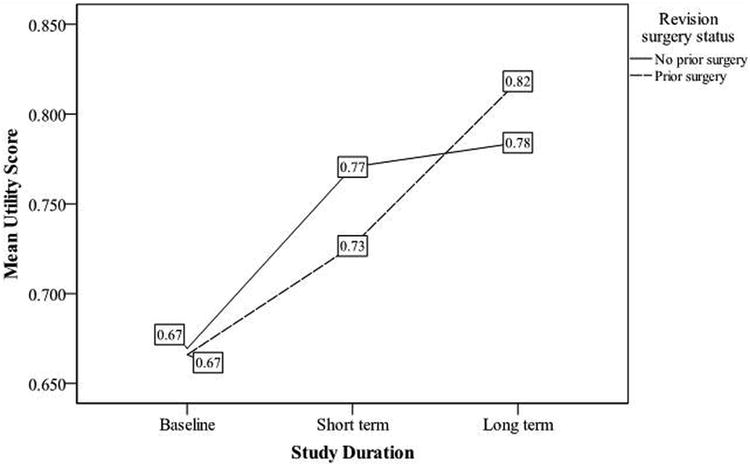
Mean overall long-term utility for Primary ESS and Revision ESS
Mean long-term utility scores were statistically similar between subjects with (n=47) and without (n=36) a history of prior ESS (0.82 (0.11) vs. 0.78(0.15), respectively, p=0.453; Figure 3). Both subject groups reported highly significant improvement in health state utility over time between baseline and long-term follow-up evaluations (both p<0.001). Primary ESS subjects reported similar mean utility scores between short-term (0.77(0.13)) and long-term (0.78(0.15)) follow-up (p=0.578), while revision ESS subjects reported significant improvement between short (0.73(0.13)) and long-term (0.82(0.11) follow-up periods (p<0.001).
Figure 3. Long-term postoperative utility trend following primary and revision ESS.
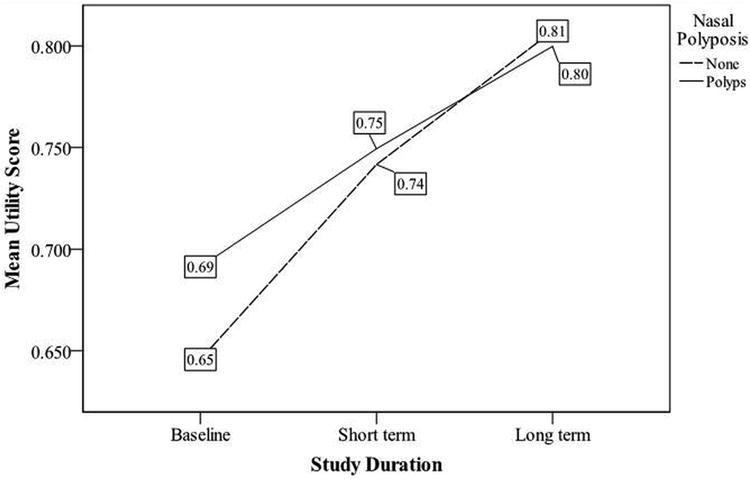
Mean overall long-term utility for Polyp and Non-polyp CRS after ESS
Mean long-term utility scores were also similar between subjects with nasal polyposis (CRSwNP; n=39) and without (CRSsNP; n=44) preoperative nasal polyposis (0.80(0.12) vs. 0.81(0.13), respectively, p=0.421; Figure 4). Both groups reported highly significant improvement in health state utility over time between baseline and long-term follow-up evaluations (both p<0.001). CRSwNP subjects reported similar mean utility values between short-term and long-term follow-up evaluations (p=0.086) while CRSsNP subjects were found to have further statistically significant improvement between short-term and long-term follow-up (p=0.010).
Figure 4. Long-term postoperative utility trend for patient with CRS with and without nasal polyposis following ESS.
Discussion
This study demonstrated that the utility improvements after ESS reported in the short-term (1.5 years) were maintained over time and often continued to improve. With a mean follow-up of 5.2 years, the overall mean long-term utility score was 0.80(0.13) which was similar to US population norm of 0.8110. Furthermore, there were continued average improvements in health state utility scores for all subsequent years following ESS compared to preoperative responses. Significant long-term improvements in utility scores were seen in both CRSwNP and CRSsNP patients and those with and without prior sinus surgery. Although ESS likely contributed to a portion of long-term utility improvement, it is important to recognize the potential for unmeasured confounding effects on long-term general health outcomes (such as subsequent revision ESS procedures, changes in medical therapy, chronic disease adaptation, or improvements in comorbid status).
Health care expenditure, in terms of GDP, is estimated to be increasing at a rate of 4% per year and thus there is a growing concern about the fiscal sustainability of health care systems around the globe11. A recent perspective article in the New England Journal of Medicine by Neumann outlines the following integral components for practicing physicians: 1) cost constraint consideration, 2) recognition that less care may be better care, and 3) a call for physicians to use health care resources wisely12. This highlights the need critically evaluate clinical interventions using economic evaluations to ensure resources are being allocated efficiently.
True economic evaluation seeks to define the costs and consequences of a clinical intervention on a patient though their entire life until the time of death. This creates an inherent challenge when studying chronic conditions, such as CRS, since it is typically not feasible to study the true long-term effects of clinical interventions. For example, in a large prospective, multi-institutional trial evaluating the outcomes following ESS for CRS, the mean age was 48.6 years13. Using the 2011 US national life expectancy age of 75.414, this would require a mean study follow-up of 26.8 years to clearly define the effect of ESS on patients with CRS. To overcome this inherent challenge of economic evaluation's requirement for true long-term outcomes, assumptions are generated using extrapolations from the best available data. Therefore, it is imperative to generate the best available long-term data possible to promote accurate long-term assumption development. This reasoning was the impetus behind this study.
Utility level is a generic quality of life outcome based on the patient's preference for being in a particular health state and forms the foundation for the quality adjusted life year (QALY), which is the preferred outcome during CEA/CUA15,16. The QALY is a product of the patient's life-expectancy and quality of life in those remaining years. Although there are several controversies surrounding the QALY, it provides valuable information to policy makers and can assist in the decision-making process for health care resource allocation.
In 2011, Soler et al. reported the first prospective study evaluating utility outcomes following ESS for patients with refractory CRS7. Using the SF-6Dhealth state utility question naire they demonstrated a baseline CRS utility value of 0.65 (95% CI: 0.63-0.66) which was lower than other chronic conditions such as congestive heart failure17 and chronic obstructive pulmonary disease18. With a mean follow-up of 1.5 years after ESS, the utility score increased by 0.087 (95% CI: 0.06 - 0.12) to provide a mean overall short-term post-ESS utility value of 0.74. This increase in utility was larger than other clinical interventions such as joint replacement19 and continuous positive airway pressure (CPAP) for sleep apnea20.
The purpose of this study was to build upon the initial results from Soler et al. and provide longer term utility outcomes following ESS for refractory CRS. In this prospective longitudinal study, we achieved a mean long-term follow-up of 5.2 years on 83 patients who underwent ESS for refractory CRS. The mean long-term utility level following ESS was 0.80(0.13) which demonstrated a significant improvement from the initial short-term postoperative follow-up utility of 0.75(p<0.001). This level of mean long-term health state utility is comparable to the U.S. population norm of 0.8110. Furthermore, 54% (45 of 83 subjects) of all long-term respondent's reported achieving what could be considered a ‘normal’ utility level (utility score ≥ 0.81). Due to the chronicity of QoL reductions associated with CRS, demonstrating that ESS commonly results in the reconstitution of long-term ‘normal’ health state utility has tremendous implications for disease management and future economic evaluations.
When health state utility levels were evaluated for each year after ESS, there were continued significant average utility improvements for all subsequent years of long-term follow-up compared to preoperative responses (all p<0.028). When we evaluated factors such as history of prior ESS and nasal polyposis status, we discovered significant long-term utility improvements compared to preoperative baseline status (both groups p<0.001). Patients undergoing revision ESS continued to experience utility level improvements after the initial short-term follow-up period (0.73 at 1.5 years to 0.82 at 5.2 years; p<0.001). Although reasons for this finding are unknown, one may hypothesize that patients undergoing revision ESS typically have more challenging disease, thus producing a clinical lag in utility improvement as medical therapy may take longer to control and stabilize postoperative mucosal inflammation.
It is important to recognize the potential for a confounding variable to contribute to long-term utility improvements. Although ESS likely contributed to a portion of long-term utility improvement identified in this study, we cannot conclude it was the sole contributor. Furthermore, there is a potential that patients adapt to their chronic disease state and gradually return to US utility norms. Despite the potential for confounding variables and patient adaptation, our study has demonstrated that ESS likely plays an important role in utility outcomes in patients with refractory CRS. Future long-term prospective cohort studies should confirm these findings and potentially elucidate the factors contributing to this continued utility improvement.
There are some limitations of this study to consider when evaluating these findings: First, there is a possibility of follow-up bias since patients who are feeling better and hold a more favorable view towards their surgical outcome may have a higher likelihood of completing and returning a postoperative survey. However, a proportion of long-term responses did report low patient utility (scores ranging 0.46-0.60) which does indicate some level of variability in patient outcomes and decreased postoperative utility. Furthermore, the average short-term utility of ‘non-responders (85/168)’ was 0.72(.013), which was no different than the short-term utility of the ‘long-term responder (83/168)’ group (p = 0.229). A second potential limitation is that there were small sample sizes available for some postoperative annual follow-up evaluations and each individual follow-up year involved different patient subgroups. Despite some groups having a low sample size, there was a general trend of improving utility level following ESS as demonstrated by long-term assessments compared to baseline and short-term levels. A third limitation is the survey based design of this study to define long-term utility outcomes. This method is not as robust as compared to a prospective longitudinal cohort study with regular scheduled follow-up intervals. This type of cohort study has the advantage of obtaining accurate follow-up data which can be used to elucidate confounding effects. However, prospective longitudinal cohort studies are very challenging to perform at tertiary referral centers due to patient referral patterns and migration, thus we attempted to use the best available methodology to define long-term utility results following ESS. Despite these limitations, we feel this study is strengthened by its prospective longitudinal design and use of stringent CRS diagnostic criteria. Data from this study will enable researchers to begin generating more accurate long-term assumptions for future economic evaluations of ESS in patients with CRS. Future studies should confirm our early findings and attempt to define potential confounding variables using a prospective cohort study design.
Conclusion
Long-term health state utility outcomes are important both to evaluate the effectiveness of our interventions for chronic disease and to generate accurate long-term utility assumptions for economic evaluations. This study has demonstrated that patients who undergo ESS for refractory CRS experience stable utility improvements over time and often continue to experience improvements past the initial short-term postoperative follow-up period. Furthermore, the mean long-term utility level following ESS approached US population norms and over half of the patients exceeded this ‘normal’ health state utility level. Future long-term cohort studies will need to confirm these findings and elucidate potential confounding variables.
Footnotes
Financial Disclosures: There are no financial disclosures for Luke Rudmik, MD, Jess Mace, MPH, Zachary M. Soler, MD, MSc, or Timothy L. Smith, MD, MPH.
Potential Conflicts of Interest: There are no conflicts of interests for Luke Rudmik. Jess C. Mace, Zachary M. Soler, and Timothy L. Smith receive grant funding from the National Institute on Deafness and Other Communication Disorders, one of the National Institutes of Health (Bethesda, MD); Public clinical registration (www.clinicaltrial.gov) #NCT00799097. Timothy L. Smith is also a consultant for Intersect ENT (Palo Alto, CA) which provided no financial or administrative support for this investigation.
References
- 1.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 2.Essink-Bot ML, Stouthard ME, Bonsel GJ. Generalizability of valuations on health states collected with the EuroQolc-questionnaire. Health economics. 1993;2:237–46. doi: 10.1002/hec.4730020307. [DOI] [PubMed] [Google Scholar]
- 3.Furlong WJ, Feeny DH, Torrance GW, Barr RD. The Health Utilities Index (HUI) system for assessing health-related quality of life in clinical studies. Annals of medicine. 2001;33:375–84. doi: 10.3109/07853890109002092. [DOI] [PubMed] [Google Scholar]
- 4.Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. Health and quality of life outcomes. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. Journal of health economics. 2002;21:271–92. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 6.Walters SJ, Brazier JE. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health and quality of life outcomes. 2003;1:4. doi: 10.1186/1477-7525-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soler ZM, Wittenberg E, Schlosser RJ, Mace JC, Smith TL. Health state utility values in patients undergoing endoscopic sinus surgery. The Laryngoscope. 2011;121:2672–8. doi: 10.1002/lary.21847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Brazier JE, Roberts J. The estimation of a preference-based measure of health from the SF-12. Medical care. 2004;42:851–9. doi: 10.1097/01.mlr.0000135827.18610.0d. [DOI] [PubMed] [Google Scholar]
- 10.Hanmer J, Lawrence WF, Anderson JP, Kaplan RM, Fryback DG. Report of nationally representative values for the noninstitutionalized US adult population for 7 health-related quality-of-life scores. Medical decision making: an international journal of the Society for Medical Decision Making. 2006;26:391–400. doi: 10.1177/0272989X06290497. [DOI] [PubMed] [Google Scholar]
- 11.OECD: Health Data. [Accessed Oct 2012];2011 at http://www.oecd.org/health/healthpoliciesanddata/49105858.pdf.
- 12.Neumann PJ. What we talk about when we talk about health care costs. The New England journal of medicine. 2012;366:585–6. doi: 10.1056/NEJMp1200390. [DOI] [PubMed] [Google Scholar]
- 13.Smith TL, Litvack JR, Hwang PH, et al. Determinants of outcomes of sinus surgery: a multi-institutional prospective cohort study. Otolaryngology--head and neck surgery: official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2010;142:55–63. doi: 10.1016/j.otohns.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arias E. United States life tables, 2007. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2011;59:1–60. [PubMed] [Google Scholar]
- 15.NICE. National Institute of Clinical Excellence: Guide to the methods of technology appraisal. 2008 http://wwwniceorguk/media/B52/A7/TAMethodsGuideUpdatedJune2008pdf.
- 16.Siegel JE, Weinstein MC, Russell LB, Gold MR. Recommendations for reporting cost-effectiveness analyses. Panel on Cost-Effectiveness in Health and Medicine. JAMA: the journal of the American Medical Association. 1996;276:1339–41. doi: 10.1001/jama.276.16.1339. [DOI] [PubMed] [Google Scholar]
- 17.Kontodimopoulos N, Argiriou M, Theakos N, Niakas D. The impact of disease severity on EQ-5D and SF-6D utility discrepancies in chronic heart failure. The European journal of health economics: HEPAC: health economics in prevention and care. 2011;12:383–91. doi: 10.1007/s10198-010-0252-4. [DOI] [PubMed] [Google Scholar]
- 18.Szende A, Leidy NK, Stahl E, Svensson K. Estimating health utilities in patients with asthma and COPD: evidence on the performance of EQ-5D and SF-6D. Quality of life research: an international journal of quality of life aspects of treatment, care and rehabilitation. 2009;18:267–72. doi: 10.1007/s11136-008-9429-z. [DOI] [PubMed] [Google Scholar]
- 19.Kvamme MK, Kristiansen IS, Lie E, Kvien TK. Identification of cutpoints for acceptable health status and important improvement in patient-reported outcomes, in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. The Journal of rheumatology. 2010;37:26–31. doi: 10.3899/jrheum.090449. [DOI] [PubMed] [Google Scholar]
- 20.Schmidlin M, Fritsch K, Matthews F, Thurnheer R, Senn O, Bloch KE. Utility indices in patients with the obstructive sleep apnea syndrome. Respiration; international review of thoracic diseases. 2010;79:200–8. doi: 10.1159/000222094. [DOI] [PubMed] [Google Scholar]


