Abstract
Background
Extensive patient and family education is required at the time of a new diagnosis of pediatric cancer yet ittle data exist regarding the availability and linguistic competency of new cancer diagnosis education provided by pediatric oncology institutions.
Procedure
Using the American Society of Pediatric Hematology/Oncology (ASPHO) membership list, a web-based survey was conducted among a cohort of pediatric oncologists to determine pediatric oncologists’ assessment of institutional resources for new cancer diagnosis education and the availability of linguistically appropriate education.
Results
Of 1,294 ASPHO members sent email survey invitations, 573 (44.3%) responded with 429 meeting eligibility criteria. Oncologists at academic institutions reported their institutions had more availability of resources for new diagnosis education compared with those from non-academic institutions (Mean 78.6 vs. 74.3; 0 [not at all] – 100 [well equipped]; p=0.05). The mean score increased with volume of new cancer diagnoses/year: small (<75) = 73.4; medium (75 – 149) = 76.7; large (≥ 150) = 84.5 (p <0.001). Oncologists at large volume institutions reported more availability of an established patient education protocol (50.8% vs. 38.1%, p <0.001) and increased use of dedicated non-physician staff (79.9% vs. 66.1%, p=0.02), but less use of websites for patient education (17.2% vs. 33.3%, p=0.001). Availability of linguistically appropriate education improved with increasing institution size: small (76.4), medium (82.3) and large (84.0) patient volume (p <0.011).
Conclusion
According to pediatric oncologists, a disparity in educational and linguistic resources for new pediatric cancer diagnosis education exists depending on institution type and size.
Keywords: language competency, patient education, new cancer diagnosis, psychosocial
INTRODUCTION
In the United States, around 12,000 children are diagnosed with cancer annually (1). Patients and families require extensive education on the disease, prognosis, treatment, side effects and care at home. There is a paucity of data on the methods and availability of education for childhood cancer patients and parents (2–5). Studies to date show parental stress negatively impacts comprehension (5), parents and oncologists can have discrepant impressions of the child’s prognosis (4) and discharge educational planning may decrease readmission rates (3). Before developing interventions to standardize educational resources at the time of new diagnosis, it is necessary to assess current practices and availability of resources in institutions treating children with cancer and identify resource gaps.
Therefore, we conducted a survey to assess pediatric oncologists’ report of the availability of teaching resources at their institutions for patients and parents at the time of a new childhood cancer diagnosis. Additionally, we investigated the perceived importance of linguistic competency at the institutions and the availability of language services, such as document translation and certified interpreters.
METHODS
Study Review
The Institutional Review Board at Vanderbilt University Medical Center (Nashville, TN) reviewed and approved the study.
Study Population
Using the online membership database from the American Society of Pediatric Hematology/Oncology (ASPHO), we identified currently practicing attending oncologists based on review of their membership profile.
Survey
The survey was constructed and delivered using REDCap, a secure, web-based application for building and managing online surveys and databases (6). The survey was developed by pediatric oncologists with guidance from experts in education and cultural competency. Two pilot surveys at a single institution were conducted with feedback considered for item clarification. The final survey consisted of 17 multiple choice questions including demographic information and assessments of resources available at the respondents’ institutions, two scale bar questions assessing the respondents’ impressions of the resources available for patient education and the importance of linguistic competency at their institutions, and three free text boxes to describe areas of success and areas for improvement at the respondents’ institutions as well as contact information if the respondent wished to share resources (Supplementary Material).
To provide protected anonymous web access to the survey, a series of three emails were sent through REDCap over a four-week period to potential study participants. Individual responses were de-identified by REDCap ensuring that the identity of the respondent was blinded to researchers.
Statistical Analysis
Primary data analysis focused on differences among respondents from small (<75 new cancer diagnoses/year), medium (75–150 new cancer diagnoses/year) and large (>150 new cancer diagnoses/year) institutions as well as those from academic versus non-academic (community/private/other) institutions. Survey responses to multiple choice questions were reported as percentages. Chi squared analysis was used to evaluate independent categorical responses. Responses to scale bar questions were reported as means with standard deviations. As the data did not exhibit a normal distribution, Kruskal-Wallis tests were performed on continuous outcomes of the scale responses when more than two groups (e.g. institution new diagnosis volume) were observed and Wilcoxon rank sum tests if there were only two groups (e.g. institution type). Statistical analyses were done using STATA™, version 11 (StataCorp LP, College Station, TX, USA).
RESULTS
Survey Population
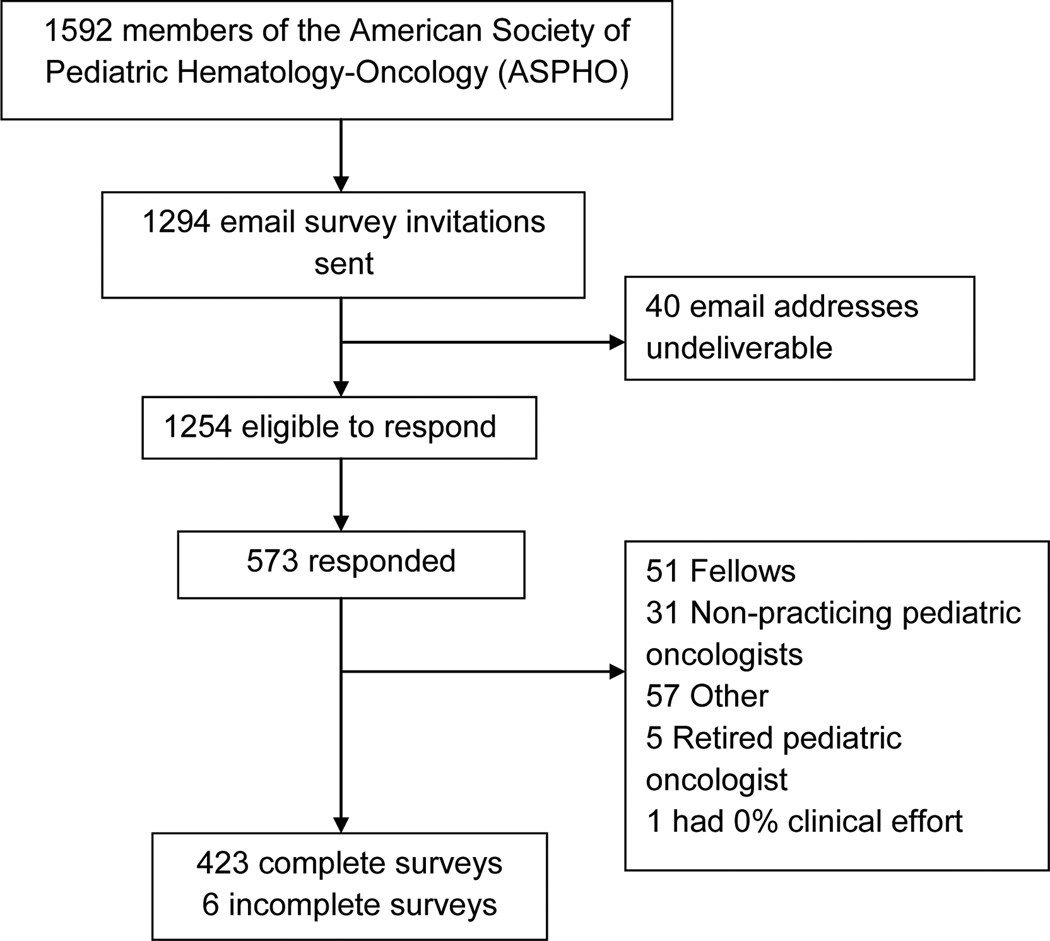
At the time of this study, there were 1592 members of ASPHO listed on their online membership roster. After review of profiles and eliminating those self-identified as not being an attending oncologist, 1294 ASPHO members were sent email survey invitations. Of those, 573 (44.3%) responded to the survey and 429 met eligibility criteria and were included in the study analysis (Figure 1).
Figure 1.
Consort Diagram
Of the respondents, 52.5% were male and 82.1% reported that > 30% of their time was dedicated to clinical practice. A broad range of experience was observed in this cohort with 30.2% less than 5 years from the completion of their fellowship training, 17.6% between 6–10 years, 23.4% between 11–20 years, and 28.8% with more than 20 years of post-fellowship experience. The majority of the respondents were employed at academic institutions compared to non-academic institutions (81.3% vs. 18.7%). There was a relatively even distribution of institutions represented based on annual new cancer diagnosis volume with small (<75), medium (75–149) and large (>150), 39.3%, 29.3% and 31.4%, respectively (Table I).
Table I.
Cohort
| Characteristic | N | % |
|---|---|---|
| Gender (n= 427) | ||
| Female | 203 | 47.5 |
| Male | 224 | 52.5 |
| Clinical Effort (n= 428) | ||
| 1–30% | 76 | 17.8 |
| 31–70% | 131 | 30.6 |
| >70% | 221 | 51.6 |
| Years since completing fellowship (n=428) | ||
| <5 years | 129 | 30.1 |
| 6–10 years | 76 | 17.8 |
| 11–20 years | 101 | 23.6 |
| >20 years | 122 | 28.5 |
| Institution (n=428) | ||
| Academic | 348 | 81.3 |
| Community/Private/Other | 80 | 18.7 |
| New Diagnoses/Year (n=427) | ||
| <75 | 168 | 39.3 |
| 75–149 | 125 | 29.3 |
| >150 | 134 | 31.4 |
| Patients from a minority group (n=426) | ||
| <10% | 32 | 7.5 |
| 10–24% | 141 | 33.1 |
| 25–49% | 160 | 37.6 |
| 50–74% | 78 | 18.3 |
| 75–100% | 15 | 3.5 |
| Patient’s primary language not English (n=427) | ||
| <10% | 142 | 33.3 |
| 10–24% | 166 | 38.9 |
| 25–49% | 94 | 22 |
| 50–74% | 20 | 4.7 |
| 75–100% | 5 | 1.2 |
Institutional Education Practices
When queried about how equipped their institutions were to provide new diagnosis patient/family education, on a scale bar with a range from 0 (Not At All) to 100 (Well Equipped), oncologists at academic institutions reported their institutions to be better equipped than those from non-academic institutions (Mean 78.6 vs. 74.3; p = 0.05). The mean score also increased with volume of new diagnoses/year: small (<75) = 73.4; medium (75 – 149) = 76.7; large (≥ 150) = 84.5 (p <0.001) (Table II).
Table II.
Subjective Responses to Institution Teaching Resources
| Equipped Score (Mean) |
Std | p value | |
|---|---|---|---|
| Institution | |||
| Academic (n=346) | 78.6 | 16.6 | 0.05 |
| Community/Private/Other (n=79) | 74.3 | 18.8 | |
| New Diagnoses/Year | |||
| <75 (n=167) | 73.4 | 17.2 | |
| 75–149 (n=123) | 76.7 | 17.5 | <0.001 |
| >150 (n=134) | 84.5 | 14.3 | |
A series of questions were then answered regarding available teaching methods for families of newly diagnosed pediatric oncology patients. Oncologists at large volume institutions, compared with the smallest volume institutions, reported more availability of an established patient education protocol (50.8% vs. 38.1%, p <0.001), increased utilization of dedicated non-physician education staff (79.9% vs. 66.1%, p=0.02) and less use of websites as an educational medium (17.2% vs. 33.3%, p=0.001) for patient and parent education. There were no significant differences in the reported use of the use of print or electronic resources (such as DVDs) or time spent with the oncologist by institution type or new diagnosis volume.
Assessment of Language Competency
With respect to education for non-English speaking families, on a scale from 0 (Not At All) to 100 (Very Important), the importance placed on linguistically appropriate education followed a similar pattern to the availability of teaching resources with a mean scaled value of 76.4 for small volume institutions, 82.3 for medium and 84.0 for large volume institutions (p <0.011). However, there was no difference between academic and non-academic institutions (Table III).
Table III.
Pediatric Oncologists’ Assessment of Importance of Linguistic Competency at Their Institution
| Language Competency Importance Score (Mean) |
Std | P Value | |
|---|---|---|---|
| Institution | |||
| Academic (n=346) | 81 | 20.3 | 0.91 |
| Community/Private/Other (n=79) | 78.6 | 27.5 | |
| New Diagnoses/Year | |||
| <75 (n=166) | 76.4 | 25.1 | |
| 75–149 (n=125) | 82.3 | 19.2 | 0.011 |
| >150 (n=133) | 84 | 18.7 | |
Regarding specialized language services for non-English speaking patients and families, survey respondents reported that certified interpreters were “always” used by 71.6% of oncologists at large volume institutions vs. 51.8% at the smallest volume institutions (p=0.002) and by 62.6% vs. 50.0% at academic compared with non-academic institutions (p=0.01). There was no difference in reported translation of documents into patients’ primary languages by either institution type or new diagnosis volume.
DISCUSSION
While limited assessments of patient and parent education for newly diagnosed children with cancer have been undertaken, this is the first large survey of pediatric oncologists on this topic across varied institutional types. These data, based on pediatric oncologists’ reporting of available educational resources, demonstrated significant differences between academic and non-academic institutions and smaller versus larger volume institutions, with the larger academic institutions having the greatest number of resources. Patterns of provision of education also varied, with larger academic institutions using more protocol-driven education delivered by non-physicians and smaller institutions using more web-based resources. Furthermore, contributing to these differences, the availability of resources for non-English speaking patients and families was more robust at larger institutions where certified translators appear to be more commonly utilized.
Most studies on the topic of patient education have been approached from the family’s perspective. Data from these studies, albeit limited by small sample size, should help to inform practice, as parental perception of the amount of information provided to them directly impacts their ability to make a treatment decision (7). In a survey of twelve families with acute lymphoblastic leukemia (ALL), Aburn and Gott found that families were generally satisfied with education, but wanted less medical jargon, more time with health professionals and an up-to-date and reliable list of websites (8. A multi-institution study including 77 families of children with all types of cancer found that greater than half of parents reported use of the internet for education about their child’s cancer (4). In our survey, smaller volume institutions reported utilizing web-based resources more than larger volume institutions, perhaps due to a lack of dedicated staff to provide one-on-one teaching and established printed teaching materials. The impact of this difference and use of websites requires additional study to see if website use in the educational process may better meet family needs and practices, even in larger institutions with other educational resources. Computer-based programming is in limited use to aid in patient and family education, but the availability, quality and use of electronic media designed for new pediatric cancer diagnosis education has not been extensively studied (9, 10). An optional section at the end of the survey asked respondents to provide examples of educational successes and areas for improvement in patient education at their institution. In addition to the use of institutional handbooks or webpages, some respondents reported the use of the Children’s Oncology Group Family Handbook and the American Cancer Society and the Leukemia/Lymphoma Society websites.
Multiple methods can be utilized by the medical team to aid the family in making important treatment-related decisions and caring for their child with cancer (11). In a narrative review of the literature regarding new diagnosis education with patients with acute lymphoblastic leukemia, Aburn and Gott reported 5 themes including: 1) identification of a key educator for discharge planning; 2) use of a multidisciplinary approach; 3) discussion of the caretakers’ responsibilities; 4) early initiation of education; 4) a tailored approach to family needs; and 5) creation of a child-focused plan of care while at home (2). In order for any communication with the family to be effective, it must be presented to them in comprehensible manner. A Canadian study of Asian immigrant parents of children with cancer found that more than a third had limited or no ability to communicate in English and often found language services inadequate or unavailable. The language barrier negatively impacted the parents’ understanding of their child’s care and limited their integration into the appropriate medical services (12). Our study quantified this barrier faced by non-English speaking patients as only two thirds of responding pediatric oncologists were aware if important documents were being translated into the family’s primary language. Additionally, resources for non-English speaking patients and parents appear less available in smaller volume and non-academic institutions, as compared with larger volume and academic institutions. Telephone interpretation services are available for institutions unable to employ full time interpreters and offer a broad range of language services for patients whose primary language may not be common in the institution’s community.
Our data suggest that there are significant differences in educational resources between small and large and academic and non-academic institutions, which require further investigation. However, an important study limitation is that data were collected from attending pediatric oncologists who may not be fully aware of all the resources available at their institution. Perspectives of other health professionals, patients or family members would clearly enhance these data and is an important area for follow-up study. A majority of the respondents were from academic institutions which likely represents the normal distribution of pediatric oncologists. Further limitations due to study design included the inability to validate resources available and the inability to examine differences in educational resources across geographic regions, including countries outside the United States and Canada. Finally, as only the email address was collected from the review of ASPHO members’ profiles, analysis could not be performed on those who did not respond.
The impact of differences we noted between academic and higher volume institutions, compared to non-academic or smaller volume institutions, on patient outcome has yet to be determined, but may inform the future development of standards for educational interventions. Differences in availability and method of educational resources by institution size and type highlight the need to create dialogue and share resources to ensure that all newly diagnosed pediatric cancer patients receive high quality, patient and family-centered, culturally and linguistically appropriate education. Aligning available educational resources with parental and patient needs is of paramount importance to the provision of quality education. Furthermore, all institutions should make language competency in patient education the highest of priorities. Centralization of shared resources, including linguistic and culturally competent material, may be one mechanism to standardize and improve care across institutions caring for children with cancer. With the goal of decreasing health disparities and providing the highest quality care for all patients regardless of institution or patient background, further research is therefore required to test potential strategies of standardizing educational methods and determining the impact on patient outcome.
Supplementary Material
ACKNOWLEDGEMENTS
Research reported in this publication was supported by of National Institutes of Health under Award Number NIH 5 T32 HD 60554-3. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. REDCap is supported by UL1TR000011 from NCATS/NIH.
Footnotes
None of the authors have conflicts of interest to disclose.
SUPPLEMENTARY MATERIAL
The survey tool developed and utilized for this study is included as Supplementary Material.
REFERENCES
- 1.Audet CM, Sidat M, Blevins M, Moon TD, Vergara A, Vermund SH. HIV knowledge and health-seeking behavior in Zambezia Province, Mozambique. SAHARA J : journal of Social Aspects of HIV/AIDS Research Alliance / SAHARA , Human Sciences Research Council. 2012;9(1):41–46. doi: 10.1080/17290376.2012.665257. Epub 2012/12/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aburn G, Gott M. Education given to parents of children newly diagnosed with acute lymphoblastic leukemia: a narrative review. Journal of pediatric oncology nursing : official journal of the Association of Pediatric Oncology Nurses. 2011;28(5):300–305. doi: 10.1177/1043454211409585. Epub 2011/09/29. [DOI] [PubMed] [Google Scholar]
- 3.Caliskan Yilmaz M, Ozsoy SA. Effectiveness of a discharge-planning program and home visits for meeting the physical care needs of children with cancer. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2010;18(2):243–253. doi: 10.1007/s00520-009-0650-2. Epub 2009/05/27. [DOI] [PubMed] [Google Scholar]
- 4.Miller KS, Vannatta K, Vasey M, Yeager N, Compas BE, Gerhardt CA. Health literacy variables related to parents' understanding of their child's cancer prognosis. Pediatric blood & cancer. 2012;59(5):914–918. doi: 10.1002/pbc.24146. Epub 2012/03/22. [DOI] [PubMed] [Google Scholar]
- 5.Sloper P. Needs and responses of parents following the diagnosis of childhood cancer. Child: care, health and development. 1996;22(3):187–202. doi: 10.1046/j.1365-2214.1996.788788.x. Epub 1996/05/01. [DOI] [PubMed] [Google Scholar]
- 6.Estopinal CB, van Dijk JH, Sitali S, Stewart H, Davidson MA, Spurrier J, et al. Availability of Volunteer-Led Home-Based Care System and Baseline Factors as Predictors of Clinical Outcomes in HIV-Infected Patients in Rural Zambia. PloS one. 2012;7(12):e49564. doi: 10.1371/journal.pone.0049564. Epub 2012/12/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller VA, Nelson RM. Factors related to voluntary parental decision-making in pediatric oncology. Pediatrics. 2012;129(5):903–909. doi: 10.1542/peds.2011-3056. Epub 2012/04/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aburn G, Gott M. Education Given To Parents of Children Newly Diagnosed with Acute Lymphoblastic Leukemia: The Parent's Perspective [Abstract O031] Pediatr Blood Cancer. 2011;52(5):715. [PubMed] [Google Scholar]
- 9.Dragone MA, Bush PJ, Jones JK, Bearison DJ, Kamani S. Development and evaluation of an interactive CD-ROM for children with leukemia and their families. Patient education and counseling. 2002;46(4):297–307. doi: 10.1016/s0738-3991(01)00166-5. Epub 2002/04/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones JK, Kamani SA, Bush PJ, Hennessy KA, Marfatia A, Shad AT. Development and evaluation of an educational interactive CD-ROM for teens with cancer. Pediatr Blood Cancer. 2010;55(3):512–519. doi: 10.1002/pbc.22608. Epub 2010/06/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sung L, Regier DA. Decision making in pediatric oncology: evaluation and incorporation of patient and parent preferences. Pediatric blood & cancer. 2013;60(4):558–563. doi: 10.1002/pbc.24450. Epub 2013/01/03. [DOI] [PubMed] [Google Scholar]
- 12.Gulati S, Watt L, Shaw N, Sung L, Poureslami IM, Klaassen R, et al. Communication and language challenges experienced by Chinese and South Asian immigrant parents of children with cancer in Canada: implications for health services delivery. Pediatric blood & cancer. 2012;58(4):572–578. doi: 10.1002/pbc.23054. Epub 2011/03/04. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.