Abstract
Objective:
Obesity in the United States is highly prevalent, approaching 60% for black women. We investigated whether nutrition education sessions at the work place added to internet-based wellness information and exercise resources would facilitate weight and fat mass loss in a racially diverse population of overweight female employees.
Methods:
A total of 199 (average body mass index 33.9±6.3 kg m−2) nondiabetic women (57% black) at our institution were randomized to a 6-month program of either internet-based wellness information (WI) combined with dietitian-led nutrition education group sessions (GS) weekly for 3 months and then monthly with shift in emphasis to weight loss maintenance (n=99) or to WI alone (n=100). All were given access to exercise rooms convenient to their work site. Fat mass was measured by dual-energy X-ray absorptiometry.
Results:
WI+GS subjects lost more weight than WI subjects at 3 months (−2.2±2.8 vs −1.0±3.0 kg, P>0.001). Weight (−2.7±3.9 vs −2.0±3.9 kg) and fat mass (−2.2±3.1 vs −1.7±3.7 kg) loss at 6 months was significant for WI+GS and WI groups (both P<0.001), but without significant difference between groups (both P>0.10); 27% of the WI+GS group achieved ⩾5% loss of initial weight as did 18% of the WI group (P=0.180). Blacks and whites similarly completed the study (67 vs 74%, P=0.303), lost weight (−1.8±3.4 vs −3.3±5.2 kg, P=0.255) and fat mass (−1.6±2.7 vs −2.5±4.3 kg, P=0.532), and achieved ⩾5% loss of initial weight (21 vs 32%, P=0.189), irrespective of group assignment.
Conclusion:
Overweight women provided with internet-based wellness information and exercise resources at the work site lost weight and fat mass, with similar achievement by black and white women. Additional weight loss benefit of nutrition education sessions, apparent at 3 months, was lost by 6 months and may require special emphasis on subjects who fail to achieve weight loss goals to show continued value.
Keywords: obesity, adiposity, weight loss program, racial disparity, women's health
Introduction
In the United States, nearly 70% of adults are overweight and more than 30% of women are obese.1 The prevalence of obesity is particularly high among underrepresented minority populations, ∼60% for black women.1 Previous studies have indicated that employees in the United States spend large portions of the work day sedentary, which likely contributes to energy intake in excess of energy expenditure.2, 3 Because of the adverse impact of physical inactivity and obesity on health care costs, many organizations have initiated ‘wellness' programs, which may include facilities at the work site to encourage exercise.4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18 Although these programs have often resulted in improved fitness for participants, weight loss has been more difficult to achieve.5, 6, 13, 14, 17
Successful weight loss by women has been reported with inclusion of some form of an interactive approach, such as group sessions designed in accordance with social cognitive theory,19 including programs designed and led by registered dietitians20, 21, 22 in accordance with guidelines from the Academy of Nutrition and Dietetics.23 Black women, however, have generally been found to achieve less weight loss than white women in behavioral weight loss interventions.24 Alternatively, internet-based educational tools have also been successful in achieving weight loss,12, 18, 25, 26, 27 although efficacy in underrepresented minorities is unknown. Therefore, the objectives of this study were to: (i) determine the added weight and fat mass loss efficacy of small-group sessions led by a registered dietitian to a work site wellness program that provided internet-based nutrition and lifestyle information, and access to exercise facilities close to the work site in a randomized clinical trial and (ii) examine racial (black and white) differences in response to the study intervention. We reasoned that small-group nutrition education—designed and conducted by registered dietitians—would be an effective method for weight loss in a racially diverse population of overweight female employees when combined with internet-based wellness information and exercise resources that could be accessed by participants at their convenience.
Materials and methods
Study population
Overweight (body mass index (BMI) 25–<30 kg m−2) and obese (BMI ⩾30 kg m−2) nondiabetic (fasting glucose <126 mg dl−1) female employees of the National Institutes of Health, Bethesda, MD, USA, who self-identified as healthy and not active participants in exercise or weight-reduction programs were recruited by campus announcements. Women were excluded from the study for anemia (hemoglobin <11 g dl−1) regardless of etiology; liver, kidney or thyroid disease by screening blood work; or recent (<2 months) initiation of prescription medication. Prescription medications at stable doses for at least 2 months—including hormonal preparations for thyroid dysfunction, birth control or post-menopausal symptoms— were permitted, but change in medications during the study was pre-specified as an exclusion criterion from further participation because of possible effects on study end points. The protocol was approved by the Institutional Review Board of the National Heart, Lung, and Blood Institute, and registered in ClinicalTrials.gov (NCT00666172) before study initiation. All subjects provided informed written consent. Race and ethnicity were identified by self-report. All testing was performed after an overnight fast, and for premenopausal women, within the first 10 days of their menstrual cycle. Subjects were compensated for time and inconvenience of testing but were otherwise not paid for participation.
Weight loss and fitness resources
Each participant was provided internet-based wellness information created by the NHLBI for employees (recent version can be found at http://apps.nhlbi.nih.gov/keepthebeat) that included recommendations from the Department of Health and Human Services and the US Department of Agriculture.28 The website included walking paths around the NIH Bethesda campus, sample menus, healthful lifestyle information and tools for counting calories. Each participant was given a pedometer (Walk4Life, Plainfield, IL, USA) with instructions to increase average daily step count by 5000 steps over their baseline average, and given card–key access to private fitness rooms located in three buildings on campus, each equipped with aerobic exercise equipment (for example, treadmill, elliptical machine and supine bicycle). Participants were also encouraged to continue physical activity—especially walking—on days when not at work.
Study groups
Subjects were randomized by the Clinical Center Pharmacy Development Service into either internet wellness information combined with nutrition education group sessions (WI+GS) or internet wellness information alone (WI) using a table of random numbers with block size not revealed to the investigators. Those randomized to WI+GS were instructed to attend nutrition education sessions (weekly for the first 3 months, monthly for the last 3 months) in small groups (⩽10 persons per session) conducted by a registered dietitian; attendance was recorded. Entry into classes was on a rolling basis depending on when the subject enrolled in the study; all subjects received the same information over the course of 6 months participation. Sessions were held at noon and participants were encouraged to bring lunch so that there was minimal disruption from their work responsibilities. Before the initial group session, subjects met privately with the dietitian to set weight loss goals for the 6-month program. After reviewing their 3-day food record, the dietitian provided a handout delineating their calculated energy needs to promote weight loss, along with a daily meal plan reflecting this individualized calorie level. The dietitians encouraged class participants to keep daily food journals throughout the study as a technique to improve dietary compliance. The first 3 months of the group education sessions consisted of a 12-week curriculum that was created by three registered dietitians associated with this study (NGS, JdJ and BDF) based in part on NHLBI's Aim for a Healthy Weight Program (most recent version can be found at http://www.nhlbi.nih.gov/resources/obesity/education/aim.htm). The curriculum (Table 1) provided pertinent healthful information that could easily be incorporated into the women's lifestyle. Each 45 min session included an individual (private) weigh-in, homework questions related to previous sessions to be discussed by attendees and a presentation on nutrition information relevant to weight management and cardiovascular health. After 3 months, WI+GS participants transitioned to monthly classes for the remaining 3 months, which also included weigh-ins and were conducted by a dietitian, with focus on weight loss maintenance.
Table 1. Class topics for nutrition education sessions.
| Session # for months 1–3: weekly class topic |
| Session 1: energy balance/food journaling |
| Session 2: what counts as a serving and low calorie menu plans |
| Session 3: reading labels and smart shopping |
| Session 4: keeping your portions under control |
| Session 5: making better choices when you eat out |
| Session 6: food preparation and food storage |
| Session 7: action plan development |
| Session 8: heart health |
| Session 9: eating cues and mindful eating |
| Session 10: beverages: think about what you drink |
| Session 11: eating hints for the workplace |
| Session 12: restaurant eating |
| Session # for months 4–6: monthly class topic |
| Session 1: staying motivated |
| Session 2: tips for success |
| Session 3: National Weight Control Registry |
Testing
All testing was performed at the NIH Clinical Center, Bethesda, MD, USA. Baseline, 3 month and 6-month visits included weight measurement; baseline and 6-month visits included waist (at the uppermost border of the iliac crest) and hip circumference (at the maximum protuberance of the buttocks) measurements to the nearest millimeter with a non-stretch tension tape measure (Gulick II, Gays Mills, WI, USA), fasting blood work (glucose, insulin and lipids), and total fat mass and percent truncal fat measured by dual-energy X-ray absorptiometry (DXA; iDXA Software Encore 11.10, GE Lunar Medical Systems, Madison, WI, USA). Exercise performance was measured at baseline and 5 months during graded treadmill exercise (standard Bruce protocol29) with a SensorMedics Vmax Spectra 229c metabolic cart (CareFusion, San Diego, CA, USA) for the analysis of oxygen consumption at peak exercise (peak VO2). Insulin sensitivity was assessed by the homeostasis model assessment for insulin resistance (HOMA-IR).30 Women were asked to maintain a diary of daily pedometer counts throughout the 6-month study. All testing was conducted and analyzed by investigators who were blinded to randomized assignment.
Statistical analysis
The primary end points of this study were the differences in weight reduction between the WI+GS and WI groups from baseline to 3 months and to 6 months follow-up, with analysis of differences in weight loss by race (black, white). We performed an intention-to-treat analysis in which weight loss for subjects who withdrew from the study after at least the 3-month weight measurement was imputed on the basis of 0.3 kg per month regained weight31 as well as weight loss analysis for subjects who completed the 6-month program. Participants who withdrew from the study before 3 months were excluded from analysis because no end point data were available. Secondary outcomes included: changes in total fat mass, truncal fat (as percent of total fat), abdominal and hip circumferences, lipid levels, insulin sensitivity and exercise performance from baseline to 6 months for participants who completed the entire program. T-tests or Mann–Whitney–Wilcoxon test for continuous data and χ2 proportionality test were performed using InStat biostatistics software (GraphPad Software, Version 3.06, 2003; San Diego, CA, USA). Associations between frequency of attendance at group sessions and weight or fat mass loss were performed using either Pearson's correlation or Spearman's rank correlation, as appropriate. In addition, separate repeated-measures mixed-effects models were fit to the primary outcome of weight change at 3 and 6 months, and each of the secondary outcomes at 6 months. Adjusted models were evaluated to determine the treatment (WI+GS or WI) effect, time effect and the treatment × time interaction effect. All models were adjusted for age, race and baseline BMI. Skewed data were log-transformed. Differences in treatment effect within racial groups were assessed with a race × treatment interaction term (limited to non-Hispanic black and white women, given the small number of other racial groups in the study population). All adjusted model analyses were performed using the SAS statistical analysis package (SAS User's Guide: Statistics, Version 9 Edition: SAS Institute Inc, Cary, NC, USA). A P-value ⩽0.05 was considered statistically significant. The study had 80% power at a two-sided type I error of 0.05 to detect a difference in weight change between WI+GS and WI groups of 2 kg, assuming a population s.d. of 3 kg and a withdrawal rate of 30%. Data are reported as mean±s.d.
Results
Study participants
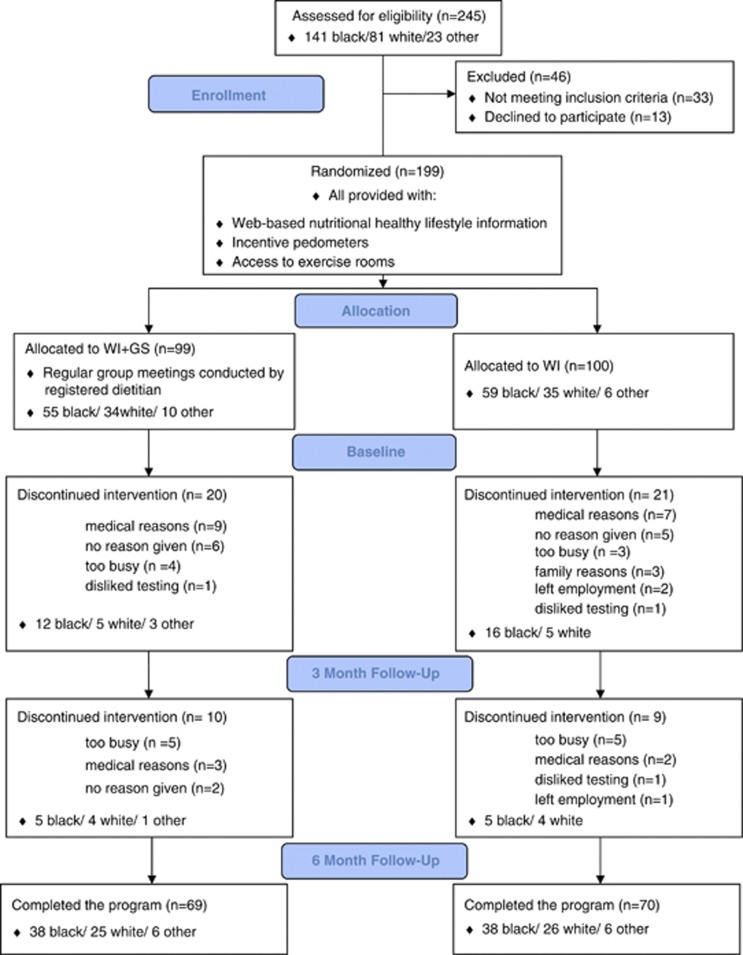
After screening 245 nondiabetic women who responded to the initial advertisement, 199 were consented to the protocol (Figure 1). BMI for the group averaged 33.9±6.3 kg m−2, ranged 25.0–57.7 kg m−2. Fifteen subjects reported taking HMG-CoA reductase inhibitor (statin) therapy for hypercholesterolemia, with stable drug preparation and dose for at least 2 months before study entry. There were no significant differences in demographics or clinical characteristics between WI+GS and WI groups at baseline (Table 2).
Figure 1.
Flow chart of participants in a protocol randomizing participants to internet-based wellness information and nutrition education group sessions (WI+GS) vs wellness information only (WI).
Table 2. Baseline clinical characteristics–internet-based wellness information and nutrition education group sessions (WI+GS) vs wellness information only (WI).
| WI+GS (n=99) | WI (n=100) | P-value | |
|---|---|---|---|
| Age | 47±9 | 45±12 | 0.191 |
| Race/ethnicity | |||
| Black (%) | 56 | 59 | 0.942 |
| White (%) | 33 | 34 | |
| Asian (%) | 4 | 1 | |
| Hispanic (black or white) (%) | 7 | 6 | |
| Adiposity | |||
| BMI (kg m−2) | 34.0±6.2 | 33.8±6.6 | 0.748 |
| Weight (kg) | 91.3±18.7 | 90.6±18.3 | 0.657 |
| Fat mass (kg) | 39.9±11.9 | 40.6±12.5 | 0.829 |
| Truncal fat (%) | 46±6 | 47±6 | 0.557 |
| Abdominal circumference (cm) | 104.4±14.9 | 105.7±14.5 | 0.518 |
| Hip circumference (cm) | 118.5±12.6 | 118.0±12.6 | 0.646 |
| Exercise performance | |||
| Duration (s) | 406±96 | 403±107 | 0.786 |
| Peak VO2 (ml kg−1 min−1) | 23.3±5.0 | 23.4±5.5 | 0.812 |
| Insulin sensitivity | |||
| HOMA | 2.3±2.1 | 2.1±1.6 | 0.852 |
| Lipids (n=89, 96) | |||
| Total cholesterol (mg dl−1) | 185±33 | 187±34 | 0.685 |
| LDL-cholesterol (mg dl−1) | 114±28 | 112±31 | 0.563 |
| HDL-cholesterol (mg dl−1) | 53±13 | 56±14 | 0.17 |
| Triglycerides (mg dl−1) | 88±46 | 93±50 | 0.592 |
Abbreviations: BMI, body mass index (weight divided by squared height); HDL, high-density lipoprotein; HOMA, homeostasis model assessment; LDL, low-density lipoprotein; VO2, oxygen consumption.
Lipid measurements reported for subjects not taking HMG-CoA reductase inhibitor (statin) medications. Data are presented as mean values±s.d. or as frequency (%).
Program participation
One hundred fifty-eight participants completed at least 3 months of participation, with 139 women completing the entire 6-month program (Figure 1). Sixty women withdrew from the study before completing 6 months participation (30 subjects in each group), with reasons for discontinuation of participation indicated in the flow chart.
Study outcomes
Repeated-measures mixed models for weight change (adjusted for age, race and baseline BMI) for the 158 women (79 in WI+GS and 79 in WI) who remained in the protocol at 3 months showed a statistically significant time effect for weight loss (P<0.001) and treatment × time interaction (P=0.009), with greater weight loss for the 79 participants in the WI+GS compared with the 79 in WI (−2.2±2.8 vs −1.0±3.0 kg) (Figure 2). By intention-to-treat analysis, at 6 months a statistically significant time effect was evident for weight loss (P<0.001), but the treatment × time interaction was not significant (P=0.436). In all, 21 of 79 (27%) women in the WI+GS group achieved ⩾5% weight loss from baseline, as did 14 of 79 (18%) women in the WI group (P=0.180). The average pedometer counts were similar between the WI+GS subjects and the WI subjects (6239±3393 vs 7110±3325 steps per day, P=0.136).
Figure 2.
Weight loss for the 158 women (79 receiving internet wellness information combined with nutrition education group sessions (WI+GS), 79 receiving internet wellness information alone (WI)) who participated in the protocol for at least 3 months. Repeated-measures mixed-effects models (adjusted for age, race and baseline BMI) were used to assess the effect of 3 and 6 months participation and WI+GS vs WI assignment on weight loss.
Changes in weight, adiposity, exercise performance, insulin sensitivity and lipids for the 139 women who completed the 6-month program are reported in Table 3. The time effect for measures of adiposity, exercise performance, insulin sensitivity and blood lipids was likewise statistically significant (all P<0.05). The treatment × time interaction, however, was not statistically significant for these secondary outcomes (all P>0.05).
Table 3. Baseline to 6-month changes in outcome measures for women who completed 6-month program—internet-based wellness information and nutrition education group sessions (WI+GS) vs wellness information only (WI).
| WI+GS (n=69) | WI (n=70) | Time effect P-value | Treatment effect P-value | Treatment × time effect P-value | |
|---|---|---|---|---|---|
| Adiposity | |||||
| Weight (kg) | −2.7±3.9 | −2.0±3.9 | <0.001 | 0.784 | 0.332 |
| Fat mass (kg) | −2.2±3.1 | −1.7±3.7 | <0.001 | 0.148 | 0.411 |
| Truncal fat (%) | −1.8±2.9 | −1.3±3.1 | <0.001 | 0.143 | 0.423 |
| Abdominal circumference (cm) | −3.4±5.2 | −2.7±5.4 | <0.001 | 0.266 | 0.461 |
| Hip circumference (cm) | −2.4±4.6 | −1.1±4.2 | <0.001 | 0.920 | 0.154 |
| Exercise performance | |||||
| Duration (s) | +47±60 | +50±69 | <0.001 | 0.408 | 0.754 |
| Peak VO2 (ml kg−1 min−1) | +1.7±3.1 | +1.5±3.1 | <0.001 | 0.522 | 0.754 |
| Insulin sensitivity | |||||
| HOMA | −0.5±1.0 | −0.1±1.3 | <0.001 | 0.906 | 0.099 |
| Lipids (n=65, 69) | |||||
| Total cholesterol (mg dl−1) | −13±25 | −8±23 | <0.001 | 0.313 | 0.252 |
| LDL-cholesterol (mg dl−1) | −8±18 | −5±23 | <0.001 | 0.978 | 0.458 |
| HDL-cholesterol (mg dl−1) | −2±10 | −2±8 | 0.016 | 0.034 | 0.587 |
| Triglycerides (mg dl−1) | −10±32 | −9±29 | <0.001 | 0.577 | 0.867 |
Abbreviations: BMI, body mass index (weight divided by squared height); HDL, high-density lipoprotein; HOMA, homeostasis model assessment; LDL, low-density lipoprotein; VO2, oxygen consumption.
Lipid measurements reported for subjects not taking HMG-CoA reductase inhibitor (statin) medications. Data are presented as mean values±s.d.
Repeated-measures mixed-effects models (adjusted for age, race and baseline BMI) were used to assess the effect of 6 months participation (time) and WI+GS vs WI assignment (treatment) on the primary outcome of weight loss and all secondary outcomes.
Attendance at group sessions and weight loss
For WI+GS subjects, frequency of attendance at the sessions ranged from 0% (two subjects) to 100% (three subjects) with a median attendance frequency of 73% of sessions. Attendance at group sessions was inversely associated with changes in weight (r=−0.368, P=0.002) and fat mass (r=−0.310, P=0.011), such that those who attended group sessions most frequently achieved the greatest weight and fat mass loss. Attendance at group meetings by WI+GS subjects was independent of age (P=0.429) and race (P=0.242).
Study outcome by race
Compared with white women, black women were significantly younger (45±9 vs 48±11 years; P=0.031), more obese (BMI 35.2±6.4 vs 31.7±5.3 kg m−2; P<0.001) and had lower peak VO2 (21.7±4.7 vs 26.0±4.8 ml O2 kg−1 min−1; P<0.001) at the start of the study. Similar proportions of blacks and whites completed the study (67% vs 74%, P=0.303). Average pedometer counts trended to be higher in white subjects compared with black subjects (7301±3195 vs 6162±3422 steps per day, P=0.061). Time effect for weight loss at 3 and 6 months was significant for black women and for white women (P<0.001). There was no evidence of a differential effect of the WI+GS vs WI on weight loss for black vs white women in the study based on intention-to-treat analysis, as the race × treatment interaction was not statistically significant for the primary outcome of weight loss at 3 months (P=0.816) or at 6 months (P=0.819). For those black and white women who completed the 6-month program, the time effect for measures of adiposity, exercise performance, insulin sensitivity and blood lipids was statistically significant for both races (all P<0.05). The race × treatment interaction, however, was not statistically significant for weight and fat mass loss and for all secondary outcomes, and there were no statistically significant differences in improvement in outcomes by race (Table 4). No statistically significant difference between blacks and whites was observed in the proportion of women achieving ⩾5% loss of initial weight (21% vs 32%, P=0.189), irrespective of group assignment.
Table 4. Baseline to 6-month changes in outcome measures for black and for white women who completed 6-month program.
| Black (n=76) | White (n=51) | P-value | |
|---|---|---|---|
| Adiposity | |||
| Weight (kg) | −1.8±3.4 | −3.3±5.2 | 0.255 |
| Fat mass (kg) | −1.6±2.7 | −2.5±4.3 | 0.532 |
| Truncal fat (%) | −1.3±2.5 | −1.7±3.7 | 0.878 |
| Abdominal circumference (cm) | −2.1±4.4 | −4.1±6.2 | 0.066 |
| Hip circumference (cm) | −1.5±3.6 | −1.9±5.6 | 0.909 |
| Exercise performance | |||
| Duration (s) | +47±67 | +50±65 | 0.688 |
| Peak VO2 (ml kg−1 min−1) | +1.4±3.2 | +1.7±3.1 | 0.585 |
| Insulin sensitivity | |||
| HOMA | −0.4±1.1 | −0.4±1.1 | 0.947 |
| Lipids (n=70, 42) | |||
| Total cholesterol (mg dl−1) | −10±19 | −11±31 | 0.760 |
| LDL-cholesterol (mg dl−1) | −6±18 | −7±25 | 0.967 |
| HDL-cholesterol (mg dl−1) | −2±8 | −3±12 | 0.946 |
| Triglycerides (mg dl−1) | −8±29 | −10±32 | 0.501 |
Abbreviations: HDL, high-density lipoprotein; HOMA-IR, homeostasis model assessment for insulin resistance; LDL, low-density lipoprotein; VO2, oxygen consumption.
Lipid measurements reported for subjects not taking HMG-CoA reductase inhibitor (statin) medications. Data are presented as mean values±s.d.
Discussion
In an effort to improve health of employees and reduce costs of disease and absence from work, workplace-based approaches to improve diet and physical activity, ranging from provision of information alone to initiation of exercise programs, and nutrition and behavioral counseling, have been endorsed by the Task Force on Community Preventive Services of the Centers for Disease Control and Prevention, and the American Heart Association.32 Consistent with these recommendations, NHLBI created a website (http://apps.nhlbi.nih.gov/keepthebeat) with nutrition and healthy lifestyle information for employees and provided access to exercise rooms on campus to be used before or after work hours, or during breaks through the day. The purpose of our study was to examine the added effect of nutrition education in group sessions—designed and conducted by registered dietitians during the work day—to the provision of internet-based wellness information and exercise resources convenient to the work site on weight loss and other health measures in a racially diverse population of overweight female employees. At 3 months of participation, during which time WI+GS subjects were instructed to attend weekly weigh-in and nutrition education group sessions, subjects in the WI+GS lost significantly more weight from baseline than those randomized to WI alone. By 6 months of participation, both groups had a significant decrease in weight and fat mass and improved cardiovascular risk markers including insulin sensitivity and lipid profile in addition to exercise performance in comparison to baseline measures, but without significant difference between WI+GS and WI groups. Black women achieved similar weight and fat mass reduction, and improvement in exercise performance, insulin sensitivity and lipid profile as did white women. There were no significant differences, however, in the magnitude of changes in outcome measures between women randomized to nutrition education group sessions compared with those who were not. Although the magnitude of weight and fat mass loss for the groups was modest, approximately one-fifth of the WI+GS and WI groups lost over 5% of their initial weight, generally considered to be associated with significant reduction in health risks,32 with similar achievement by black and by white women. Weight loss for blacks and for whites in our study was similar to previous reports from multicenter and single center clinical trials (recently reviewed by Fitzgibbon et al.24) that included women from both races33, 34 or black women only,35, 36, 37, 38, 39, 40, 41, 42 although less than Diabetes Prevention Program43 and Weight Loss Management Trial44 that included women at higher risk for cardiovascular disease. Our study extends these findings to the work site with provision of information, group sessions and exercise resources made convenient to the employee.
A potential explanation for failure of the nutrition education group sessions to achieve greater weight loss and improvement in secondary outcomes compared with controls at 6 months is that all participants were provided internet-based information created by NHLBI on nutrition, lifestyle choices and access to convenient exercise resources, which together may have masked contribution from nutrition education sessions. However, WI+GS participants did achieve significantly greater weight loss compared with the WI group at 3 months, during which the emphasis in the instructional sessions was on weight loss. Weight loss stabilized with 3 additional months of participation, during which WI+GS transitioned from weekly to monthly group sessions with instructional emphasis shifted to weight loss maintenance. By contrast, the WI group progressively lost weight during this interval and closely approximated weight loss achieved by the WI+GS subjects at 6 months. This raises the possibility that the weekly weigh-ins and nutrition education sessions focusing on weight loss for the initial 3 months were of value to the WI+GS group, and that a move to monthly sessions and shift in instructional focus for the remaining 3 months was premature for many subjects. Accordingly, some participants might have benefitted from continuation of weekly instruction to facilitate further weight loss, consistent with programs that focused special attention on those unable to achieve weight loss goals. Thus, Jakicic et al.45 tested a stepped-care model in a randomized trial of 363 overweight and obese adults (83 female, 33% nonwhite) that included increased contact frequency (group sessions, mail, telephone and individual sessions) and even meal replacements for participants missing weight loss goals at 3-month intervals. This intervention approach resulted in ∼7% weight loss after 18 months of participation. Finally, our study may have been underpowered to show a smaller difference in outcomes favoring the use of nutrition education sessions, at least as designed for our study.
Adherence to the program was a major concern for our study, as true for previously reported weight loss trials, with several reporting a lower retention rate for blacks than whites.24 Thirty percent of women who responded to the initial program announcement posted at our institution, were found to be eligible, consented to the protocol and began the program, did not complete 6 months of participation. The most common explanation for dropping out was work commitments that did not allow time for exercise in the facilities provided to them or attendance at the nutrition education group sessions for those randomized to this intervention. Solutions to this may include not only greater appreciation for the health benefits on the part of supervisors for employees, but also improved time management to allow breaks for exercise during the work day, if not before or following work. Interactive web-based provision of information and self-monitoring of weight loss as well as email reminders to promote continued engagement in weight loss programs, as used in the POWER study,25 might have achieved greater engagement with our weight loss program.
We considered whether nutritional instruction from the registered dietitians in our study, who were all white, may not have been of value to the majority of participants who were black. In this regard, Batch et al.46 found that race concordance between behavioral interventionist leader and participants in Weight Loss Maintenance trial was not associated with weight loss for black participants. There was no significant difference, however, in the number of blacks randomized to the weekly nutrition education sessions who dropped out of the study in comparison with whites. In addition, there was no significant difference in weight loss between blacks and whites randomized to this intervention. When analyzed on the basis of attendance, which was similar for black women and for white women, WI+GS subjects who were frequent attendees at the weigh-in and educational sessions achieved greater weight and fat mass loss than those randomized to the WI+GS who attended infrequently. The relevance of attendance in our study is consistent with findings of the POUNDS LOST study, in which attendance at group counseling sessions was predictive of weight loss at 2 years.31 Personal intervention in the form of group sessions may also be useful in maintenance of weight loss. In this regard, the Weight Loss Maintenance Collaborative Research Group found that monthly personal contact with the specialist who had previously led 20 weekly group sessions resulted in less weight regain than use of an interactive website.47
Strengths of our study include the large and racially diverse composition of the study population, and the association of weight and fat mass loss both in black women and in white women with improvement in health measures including insulin sensitivity and lipid profile. In addition, exercise rooms and equipment were provided at the workplace to all study participants for their convenience, which may have facilitated similar improvement in exercise performance for black and for white participants. A limitation of the study is the possibility that continuation of weekly nutrition education sessions might have facilitated continued weight loss in the WI+GS group, whose weight appeared to stabilize following transition from weekly to monthly sessions with instructional emphasis shifted to weight loss maintenance. Further, the duration of the study was 6 months: Continuation for a longer period, even with monthly sessions, might have favored the nutrition education group intervention regarding continued weight loss or maintenance of weight loss. Others have shown that continuation of group sessions may sustain weight loss over time.47 Additional limitations of this study include the possibility that greater weight loss may have been achievable by use of portable devices to self-monitor diet and physical activity as reported in the Move! Trial conducted in a Veterans Administration cohort.48 In addition, sessions including motivational interviewing, which were not included in our nutrition education sessions, have also been reported to be effective in several weight loss trials.49
Conclusions
Overweight women provided with internet-based wellness information and exercise resources at the work site lost weight and fat mass, with similar achievement by black and white women. Additional weight loss benefit of nutrition education sessions, apparent at 3 months, was lost by 6 months and may require special emphasis on subjects who fail to achieve weight loss goals to show continued value.
Acknowledgments
This research was supported by the intramural research programs of the National Heart, Lung, and Blood Institute, the National Institute of Diabetes, and Digestive and Kidney Diseases, and the Clinical Center, National Institutes of Health.
The authors declare no conflict of interest.
References
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- McCrady SK, Levine JA. Sedentariness at work: how much do we really sit. Obesity. 2009;17:2103–2105. doi: 10.1038/oby.2009.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, Johnson DB, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med. 2009;37:340–357. doi: 10.1016/j.amepre.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Atlantis E, Chow CM, Kirby A, Fiatarone Singh MA. Worksite intervention effects on physical health: a randomized controlled trial. Health Promot Int. 2006;21:191–200. doi: 10.1093/heapro/dal012. [DOI] [PubMed] [Google Scholar]
- Calderon KS, Smallwood C, Tipton DA. Kennedy Space Center Cardiovascular Disease Risk Reduction Program evaluation. Vasc Health Risk Manag. 2008;4:421–426. doi: 10.2147/vhrm.s2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen J, Faber A, Ekner D, Overgaard K, Holtermann A, Sogaard K. Diet physical exercise, and cognitive behavioral training as a combined workplace based intervention to reduce body weight and increase physical capacity in health care workers – a randomized controlled trial. BMC Public Health. 2011;11:671. doi: 10.1186/1471-2458-11-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chund M, Melnyk P, Blue D, Renaud D, Breton MC. Worksite health promotion: the value of the Tune Up Your Heart program. Popul Health Manag. 2009;12:297–304. doi: 10.1089/pop.2008.0044. [DOI] [PubMed] [Google Scholar]
- Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease—a systematic review. Scand J Work Environ Health. 2010;36:202–215. doi: 10.5271/sjweh.2891. [DOI] [PubMed] [Google Scholar]
- Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. Short and long term effects of a lifestyle intervention for construction workers at risk for cardiovascular disease: a randomized controlled trial. BMC Public Health. 2011;11:836. doi: 10.1186/1471-2458-11-836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennikus DJ, Jeffery RW. Worksite intervention for weight control: a review of the literature. Am J Health Promot. 1996;10:471–498. doi: 10.4278/0890-1171-10.6.471. [DOI] [PubMed] [Google Scholar]
- Lemon SC, Zapka J, Li W, Estabrook B, Rosal M, Magner R, et al. Step ahead a worksite obesity prevention trial among hospital employees. Am J Prev Med. 2010;38:27–38. doi: 10.1016/j.amepre.2009.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippincott MF, Desai A, Zalos G, Carlow A, De Jesus J, Blum A, et al. Predictors of endothelial function in employees with sedentary occupations in a worksite exercise program. Am J Cardiol. 2008;102:820–824. doi: 10.1016/j.amjcard.2008.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milani RV, Lavie CJ. Impact of worksite wellness intervention on cardiac risk factors and one-year health costs. Am J Cardiol. 2009;104:1389–1392. doi: 10.1016/j.amjcard.2009.07.007. [DOI] [PubMed] [Google Scholar]
- Proper KI, Koning M, van der Beek AJ, Hildebrandt VH, Bosscher RJ, van Mechelen W. The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med. 2003;13:106–117. doi: 10.1097/00042752-200303000-00008. [DOI] [PubMed] [Google Scholar]
- Proper KI, Hildebrandt VH, Van der Beek AJ, Twisk JW, Van Mechelen W. Effect of individual counseling on physical activity fitness and health: a randomized controlled trial in a workplace setting. Am J Prev Med. 2003;24:218–226. doi: 10.1016/s0749-3797(02)00645-1. [DOI] [PubMed] [Google Scholar]
- Racette SB, Deusinger SS, Inman CL, Burlis TL, Highstein GR, Buskirk TD, et al. Worksite Opportunities for Wellness (WOW): effects on cardiovascular disease risk factors after 1 year. Prev Med. 2009;49:108–114. doi: 10.1016/j.ypmed.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touger-Decker R, Denmark R, Bruno M, O'Sullivan-Maillet J, Lasser N. Workplace weight loss program: comparing live and internet methods. J Occup Environ Med. 2010;52:1112–1118. doi: 10.1097/JOM.0b013e3181f9ee8c. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Nicklas BJ, Dennis KE, Berman DM, Sorkin J, Ryan AS, Goldberg AP. Lifestyle intervention of hypocaloric dieting and walking reduces abdominal obesity and improves coronary heart disease risk factors in obese, postmenopausal, African-American and Caucasian women. J Gerontol A Biol Sci Med Sci. 2003;58:181–189. doi: 10.1093/gerona/58.2.m181. [DOI] [PubMed] [Google Scholar]
- Annesi JJ. Relations of changes in exercise self-efficacy, physical self-concept, and body satisfaction with weight changes in obese white and African American women initiating a physical activity program. Ethn Dis. 2007;17:19–22. [PubMed] [Google Scholar]
- Raatz SK, Wimmer JK, Kwong CA, Sibley SD. Intensive diet instruction by registered dietitians improves weight-loss success. J Am Diet Assoc. 2008;108:110–113. doi: 10.1016/j.jada.2007.10.010. [DOI] [PubMed] [Google Scholar]
- Seagle HM, Strain GW, Makris A, Reeves RS. American Dietetic Association. Position of the American Dietetic Association: weight management. J Am Diet Assoc. 2009;109:330–346. doi: 10.1016/j.jada.2008.11.041. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, Martin IK, Odoms-Young A, Sharp LK. Weight loss and African–American women: a systematic review of the behavioural weight loss intervention literature. Obes Rev. 2012;13:193–213. doi: 10.1111/j.1467-789X.2011.00945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365:1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coons MJ, Demott A, Buscemi J, Duncan JM, Pellegrini CA, Steglitz J, et al. Technology Interventions to Curb Obesity: Systematic Review of the Current Literature. Curr Cardiovasc Risk Rep. 2012;6:120–134. doi: 10.1007/s12170-012-0222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate DF, Wing RR, Winett RA. Using internet technology to deliver a behavioral weight loss program. JAMA. 2001;285:1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services and US Department of Agriculture. Dietary Guidelines for Americans, Washington, DC2005
- Bruce RA, Blackmon JR, Jones JW, Strait G. Exercising testing in adult normal subjects and cardiac patients. 1963. Ann Noninvasive Electrocardiol. 2004;9:291–303. doi: 10.1111/j.1542-474X.2004.93003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360:859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, et al. Population approaches to improve diet, physical activity, and smoking habits. A scientific statement from the American Heart Association. Circulation. 2012;126:1514–1563. doi: 10.1161/CIR.0b013e318260a20b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svetkey LP, Erlinger TP, Vollmer WM, Feldstein A, Cooper LS, Appel LJ, et al. Effect of lifestyle modifications on blood pressure by race, sex, hypertension status, and age. J Hum Hypertens. 2005;19:21–31. doi: 10.1038/sj.jhh.1001770. [DOI] [PubMed] [Google Scholar]
- Brandon LJ, Elliott-Lloyd MB. Walking body composition, and blood pressure dose-response in African American and white women. Ethn Dis. 2006;16:675–681. [PubMed] [Google Scholar]
- Davis Martin P, Rhode PC, Dutton GR, Redmann SM, Ryan DH, Brantley PJ. A primary care weight management intervention for low-income African-American women. Obesity. 2006;14:1412–1420. doi: 10.1038/oby.2006.160. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Sanchez-Johnsen LA, Wells AM, Dyer A. A combined breast health/weight loss intervention for Black women. Prev Med. 2005;40:373–383. doi: 10.1016/j.ypmed.2004.06.018. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Ganschow P, Schiffer L, Wells A, Simon N, et al. Results of a faith-based weight loss intervention for black women. J Natl Med Assoc. 2005;97:1393–1402. [PMC free article] [PubMed] [Google Scholar]
- Befort CA, Nollen N, Ellerbeck EF, Sullivan DK, Thomas JL, Ahluwalia JS. Motivational interviewing fails to improve outcomes of a behavioral weight loss program for obese African American women: a pilot randomized trial. J Behav Med. 2008;31:367–377. doi: 10.1007/s10865-008-9161-8. [DOI] [PubMed] [Google Scholar]
- Kennedy BM, Champagne CM, Ryan DH, Newton R, Jr, Conish BK, Harsha DW, et al. The ‘Rolling Store': an economical and environmental approach to the prevention of weight gain in African American women. Ethn Dis. 2009;19:7–12. [PubMed] [Google Scholar]
- McNabb W, Quinn M, Kerver J, Cook S, Karrison T. The PATHWAYS church-based weight loss program for urban African American women at risk for diabetes. Diabetes Care. 1997;20:1518–1523. doi: 10.2337/diacare.20.10.1518. [DOI] [PubMed] [Google Scholar]
- Stolley MR, Fitzgibbon ML, Schiffer L, Sharp LK, Singh V, Van Horn L, et al. Obesity reduction black intervention trial (ORBIT): six-month results. Obesity. 2009;17:100–106. doi: 10.1038/oby.2008.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djuric Z, Mirasolo J, Kimbrough L, Brown DR, Heilbrun LK, Canar L, et al. A pilot trial of spirituality counseling for weight loss maintenance in African American breast cancer survivors. J Natl Med Assoc. 2009;101:552–564. doi: 10.1016/s0027-9684(15)30940-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West DS, Prewitt TE, Bursac Z, Felix HC. Weight loss of black, white, and Hispanic men and women in the Diabetes Prevention Program. Obesity. 2008;16:1413–1420. doi: 10.1038/oby.2008.224. [DOI] [PubMed] [Google Scholar]
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, et al. Weight loss during the intensive intervention phase of the weight-loss maintenance trial. Am J Prev Med. 2008;35:118–126. doi: 10.1016/j.amepre.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakicic JM, Tate DF, Lang W, Davis KK, Polzien K, Rickman AD, et al. Effect of a stepped-care intervention approach on weight loss in adults: a randomized clinical trial. JAMA. 2012;307:2617–2626. doi: 10.1001/jama.2012.6866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batch BC, Ard JD, Vollmer WM, Funk K, Appel LJ, Stevens VJ, et al. Impact of Participant and Interventionist Race Concordance on Weight Loss Outcomes Obesity 2012. e-pub ahead of print 2 July 2012; doi: 10.1038/oby.2012.184 [DOI] [PMC free article] [PubMed]
- Svetkey LP, Stevens VJ, Brantley PJ, Appel LJ, Hollis JF, Loria CM, et al. Comparison of strategies for sustaining weight loss: the Weight Loss Maintenance Randomized Controlled Trial. JAMA. 2008;299:1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- Spring B, Duncan JM, Janke EA, Kozak AT, McFadden HG, DeMott A, et al. Integrating technology into standard weight loss treatment: a randomized controlled trial. Arch Intern Med. 2012;10:1–7. doi: 10.1001/jamainternmed.2013.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12:709–723. doi: 10.1111/j.1467-789X.2011.00892.x. [DOI] [PubMed] [Google Scholar]