Abstract
Background:
Rheumatic fever (RF) is an important problem concerning developing countries like India. Rheumatic heart disease (RHD) is one of the most readily preventable chronic diseases.
Aim:
This study was done to find out the clinical profile, risk factors, compliance with treatment and outcome among RF/RHD cases so as to suggest better case management strategies.
Materials and Methods:
Clinical records of 51 RF and 71 RHD cases admitted in tertiary care hospitals in Mangalore between 2001 and 2010 were reviewed retrospectively.
Results:
Mean age of RF cases were 17.4 ± 12.1 years and RHD cases were 33.2 ± 18.6 years. More than half of RF and RHD cases were males. Commonest risk factors among RF cases were poor socioeconomic status (60.4%), history of upper respiratory tract infection before disease onset (58.8%) and undernutrition (35.3%). Commonest clinical manifestation among RF cases was fever 39 (76.5%) followed by polyarthritis 34 (66.7%). Commonest valvular lesions among RHD cases was mitral stenosis with mitral regurgitation found in 42.9% cases. Compliance of patients with prophylactic antibiotics was found to be 37 (30.3%). Mortality rate was significantly more among RHD cases (P = 0.0399).
Conclusions:
Improvement of socioeconomic and nutritional factors is an important task required for primary prophylaxis and of compliance for secondary prophylaxis of RF.
Keywords: Clinical features, Compliance, Rheumatic fever, Rheumatic heart disease, Risk factors, Valvular lesions
Introduction
Rheumatic fever (RF) is a multisystem disease resulting from an autoimmune reaction mainly due to infection of upper respiratory tract with group A Streptococcus. The disease usually affects children of school going age. All manifestations except for cardiac valvular damage are known to resolve completely.[1] Valvular damage which is the hallmark of rheumatic heart disease (RHD) remains the most common acquired heart disease worldwide[2,3] and is the major cause of cardiovascular death during the first 5 decades of life in developing countries.[4] Thus, RHD is associated with considerable disability and fatality in children and young adults and imposes a substantial economic burden.[2]
Although it is an eminently preventable disease and guidelines for its control have been laid down by the World Health Organization (WHO) and other bodies, because of other health priorities in many of these countries, its control has been largely neglected.[5] For the prevention of RF/RHD in developing countries its risk factors like poverty, malnutrition, overcrowding and poor housing has to be well understood and suitable corrective measures needs to be taken.[6,7] Moreover, persons already manifesting with clinical features of this disease should be promptly referred for diagnosis and long-term management with regular penicillin injections. This will control the disease by limiting heart damage.[8] But the fact is that in developing countries, the long journey to the hospital is usually undertaken when the patient develops disabling symptoms such as congestive heart failure. Arthritis and arthralgia by themselves often receive indigenous treatment.[9]
Present study was therefore designed to study the clinical profile of RF/RHD cases, to study the risk factors, to find out the treatment practices, compliance rate with treatment during the follow-up period and to find out the disease outcome in patients with RF or RHD admitted in five major tertiary care hospitals in Mangalore city of south India.
Materials and Methods
This cross-sectional study was conducted in Government Wenlock Hospital, Government Pediatrics Hospital, Kasturba Medical College (KMC) Hospital Attavar, KMC Hospital Jyothi Circle and Father Muller's Teaching Hospital situated in Mangalore city in January 2011. Ethical clearance for the conduct of this study was obtained from Institutional Ethics Committee. Later clinical records of patients with confirmed RF/RHD who were hospitalized at these hospitals between 2001 and 2010 were examined. The information was recorded in a semistructured proforma consisting of a checklist of sociodemographic variables, risk factors of RF, clinical features on admission/presentation, type of valvular lesions, diagnostic contribution of various laboratory parameters, treatment given, compliance with the treatment and disease outcome. Socioeconomic status was classified based on modified BG Prasad classification of 2004.[10] Nutritional status was assessed by the body mass index. Overcrowding was assessed by dividing the number of persons in the household by the number of rooms in the dwelling and comparing it with the accepted standards.
The clinical features of RF were classified as per the revised Jones criteria.
RF recurrence was defined as patients who fulfilled the criteria for RF at entry but who had a history of either RF or echocardiography showing evidence of previous valvular involvement.[8]
RHD included all cases with established heart disease considered to be of rheumatic origin.[11]
Compliant patient was one who did not miss more than 1 monthly prophylaxis injection per year.[8]
Statistical analysis
All the data collected was entered and analyzed using Statistical Package for Social Sciences (SPSS) version 15.0 into categories and percentages. Chi-square was used for testing statistical significance.
Results
The total number of RF/RHD patients included in this study was 122. The proportion of cases with RF was 51 (41.8%) and RHD was 71 (58.2%). Among the RHD cases, recurrence of RF was seen in 31 (43.7%) cases. Among them the previous episode of RF attack was reported within 5 years in 21 (67.7%) cases.
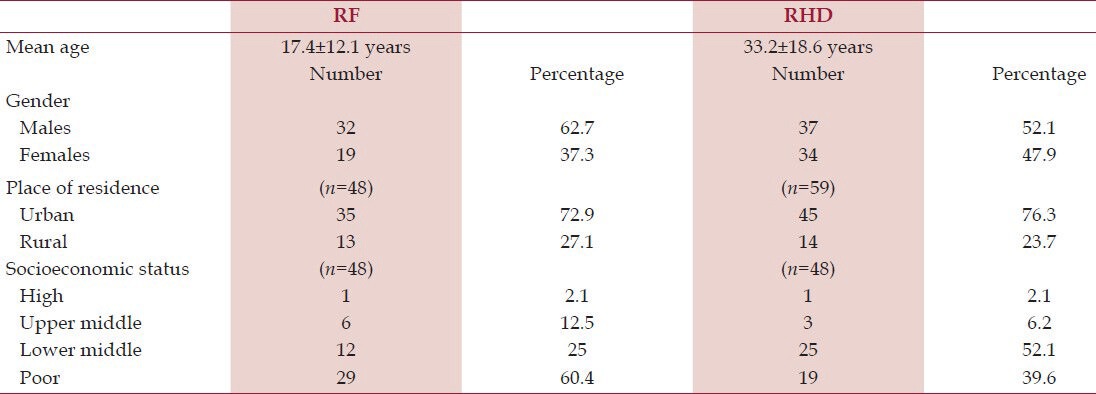
The mean age of RF cases were 17.4 ± 12.1 years and majority were males 32 (62.7%). Thirty-five (72.9%) were from urban areas and 29 (60.4%) belonged to poor socioeconomic status [Table 1]. Out of the 51 RF patients, upper respiratory tract infections before RF onset was seen in 30 (58.8%) cases, undernutrition in 18 (35.3%) cases, overcrowding in seven (13.7%) cases and family history of RF in 11 (21.6%) cases.
Table 1.
Sociodemographic distribution of rheumatic fever (RF; n = 51) and rheumatic heart disease (RHD; n = 71) cases
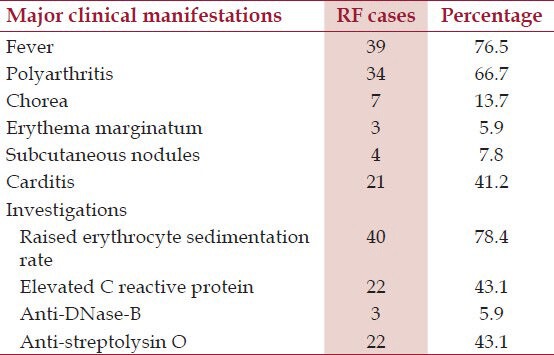
Among RF cases, fever was the commonest clinical presentation (39, 76.5%) followed by polyarthritis (34, 66.7%) [Table 2]. Of these 34 cases with joint manifestations, majority were treated with aspirin (26, 76.5%) and rest by other nonsteroidal anti-inflammatory drugs. All six (11.8%) patients with rheumatic carditis and congestive cardiac failure (CCF) were treated with steroids (along with dietary salt restriction, digoxin, and diuretics). In patients with chorea, sodium valproate was given in five cases and carbamazepine in rest two cases. The commonest laboratory finding was raised erythrocyte sedimentation rate (ESR) seen in 40 (78.4%) RF cases [Table 2]. No deaths were reported among the RF cases.
Table 2.
Major clinical manifestations and laboratory investigation findings in rheumatic fever (RF) cases (n = 51)
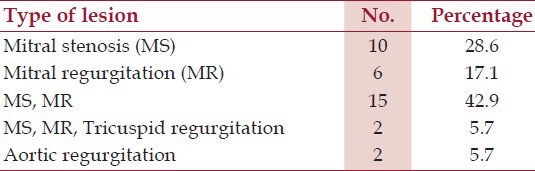
The mean age of RHD cases were 33.2 ± 18.6 years and majority were males 37 (52.1%) [Table 1]. Of the 71 cases with RHD, echocardiography findings of 35 cases were available. Among them, isolated valve lesions were found in 18 (51.4%) of which the commonest lesion was mitral stenosis (MS). MS with mitral regurgitation (MR) was found in 15 (42.9%) cases. The mean age of patients with MS and MR were 50 ± 8.37 years [Table 3]. Out of 71 RHD cases, 10 (14.1%) cases underwent surgical correction for the valve lesions. This included mitral valve repair in eight cases and mitral valve and aortic valve replacement in one case each. Among the RHD cases, three died due to CCF and three due to infective endocarditis. Mortality rate was significantly more among RHD cases (P = 0.0399).
Table 3.
Classification of valvular heart lesions in rheumatic heart disease (RHD) cases (n = 35)
Out of the total 122 cases, secondary prevention was given mostly using once monthly benzathine penicillin injections in 52 (42.6%) cases. Oral antibiotics were used in the remaining cases. Compliance of patients with prophylactic antibiotics was found to be 37 (30.3%).
Discussion
RHD is one of the most readily preventable chronic diseases. This is possible by understanding the clinical manifestations of RF leading to early diagnosis and complete treatment with antibiotics as per regimen. The mean age on admission of RF patients in a study done in Turkey was 11.2 years which was lower than our findings.[12] The observation with respect to mean age support the fact that children are at the highest risk for developing RF. This is because group A Streptococcal commonly affects younger school going children and schools are often overcrowded and badly ventilated increasing the spread of Streptococcal infection.[6] Proportion of male RF patients in this study were more than females which was in contrast to findings of several other studies where female patients were more.[7,8,13,14] In this study, almost all patients were from poor and lower middle socioeconomic group which was similar to the findings of a study done in Bangladesh.[15] However, a study done in New Delhi[13] reported more than 90% cases from poor socioeconomic group which was higher than our observation. Overcrowding in houses was seen only in few cases in this study, which was in contrast to findings of a study done in Egypt where it was present in majority of RF cases.[7] The latter study also reported majority of cases from rural areas which was again different from our observations. However, family history of RF seen in 25.5% cases in the Egyptian study was similar to our observations.[7] Recurrent history of RF which was present in 43.7% RHD cases in this study was much higher than the observations of 9.6% among RHD cases reported in an Ethiopian study.[16] Avoidance of recurrent RF attack is essential in preventing RHD in future. Also in about 68% of these RHD cases with history of recurrent episodes, previous episode was reported within 5 years of current episode. This again stresses the importance of prophylaxis for at least 5 years after the initial attack with monthly injections to minimize chances of recurrent attack.
Prior history of sore throat infection before disease onset ranged between 14 and 45.9% among cases in other studies,[7,11,13,17,18] which were lower than our observations. This wide variation in infection rates could be because of differing immunity status and living conditions among patients in different parts of the world. Cases with sore throat reported at schools and villages have to be immediately referred to health centers for confirmation. Unfortunately, timely detection is invariably absent at these places due to nonavailability of trained microbiology staff along with the lack of materials to take throat swabs added with inadequate supply of penicillins to treat positive RF cases in developing countries.[1] Another issue which threatens the treatment of sore throat infection being resistance to commonly used antibiotics.[19]
In the study done in Egypt, nutritional status among 47.9% patients was poor which was higher than our observations.[7] Fever was the commonest clinical manifestation followed by polyarthritis among RF cases in this study. Similar observations were made in studies done in Lucknow,[8] Mumbai,[20] and in literature.[1] However, few studies done in Allahabad,[9] Kathmandu[6] and New Delhi[13] have reported fever followed by polyarthralgia as the commonest clinical presentation of RF which were different from our findings.
Chorea was seen in 13.7% cases in this study and it varied from 2.7 to 18.8% cases in other studies.[6,8,9,13,15,17,20,21,22] In literature too, the prevalence of chorea in ARF has been found to vary substantially between populations ranging from <2 to 30%.[1] Chorea in most severe cases is disabling as the affected individuals are unable to perform activities of daily living and are at risk of injuring themselves.[1] The proportion of cases with erythema marginatum (5.9%) in the present study was much higher than the observations made by other studies where it ranged from 0.2 to 1.6%.[8,13,17,20] Similarly, presence of subcutaneous nodules seen in 7.8% cases in this study was higher than observations made in other studies where it was reported between 1.1 and 6% cases.[6,9,13,21,22]
Carditis seen in 41.2% of RF cases in this study was reported from 37.5 to 93% in other studies.[6,8,9,12,13,15,20,21,23,24,25] Carditis is a condition known to have a mortality of about 70% in the initial phase and this often progresses to chronic RHD.[26] As carditis is known to recur in patients with a previous history, prophylaxis with antibiotics should be continued for a longer duration in RF cases.[27]
The commonest valvular lesion among RHD cases was combined MS with MR, which was also supported by another study done in Ethiopia where this pattern was seen in 25.4% cases.[16] But other studies have reported MR to be the commonest valvular presentation in RHD cases.[11,17,20,28] Few other studies have reported MS as the commonest valvular lesion.[8,13,29] However, the reason behind predominance of mitral valve involvement by the disease as stated in all the studies mentioned above is still uncertain.[20,30]
MS (either as isolated lesion or in combination) found in 27 (77.1%) RHD cases in this study was higher than that reported between 48 and 70% of RHD cases in other studies.[13,15,16,29] MR found in 23 (65.7%) RHD cases in our study was observed between 43.8 and 96.3% in RHD cases in other studies.[15,16,17,20,29] Tricuspid regurgitation found in 5.7% RHD cases was again much lower than findings of Arora et al. study where it was present among 24% of RHD cases.[13] Aortic regurgitation found in 5.7% RHD cases was reported between 3.1 and 47% RHD cases in other studies.[8,11,13,17,29]
Raised ESR being the commonest laboratory finding in this study has also been supported by other studies.[12,13,17] Percentage of patients with raised ESR (>30 mm at the end of 1st hour) ranged between 73 and 100%[6,12,13] in other studies was also similar to our observations. Raised C-reactive proteins seen in 43.1% RF cases ranged between 2.3 and 78% cases of ARF in other studies.[6,12,13,17] Similarly, raised anti-streptolysin O (ASO) titer seen in 43.1% RF cases ranged between 13.6 and 94% ARF cases in other studies.[6,12,13,17,21]
In this study, joint manifestations were mostly treated with acetyl salicylic acid which was in accordance to the findings of other studies.[6,13] Management of patients with rheumatic carditis and CCF in this study was also similar to that reported by other studies.[6,12,21] It has also been proven that steroids controlled more promptly than salicylates the acute process of RF.[13]
Penicillin was the most common antibiotics used for treatment in this study has also been observed in other studies.[6,8,13] Compliance with treatment in this study was found to be unsatisfactory with almost 70% patients either being irregular or having discontinued antibiotics as compared to observations made by other studies where noncompliance rate ranged between 4.5 and 57.8%.[12,16,17,20] More than 57% patients in this study were on oral antibiotics. This could be a reason for high noncompliance observed in this study. Previous studies have found that patients who were compliant and who took regular penicillin prophylaxis did not have recurrence of RF.[8,11] Therefore, patients and their family members need to be educated about this disease, emphasizing the importance of adherence to secondary prophylaxis if carditis is present and also providing information of the need for antibiotic prophylaxis against endocarditis for dental and surgical procedures.[1]
Surgical treatment in this study was done in 14.1% of RHD cases. This was higher than the observations made by other studies where it ranged between 2.6 and 9.2 %.[8,13] However, a Lebanon based study reported operative procedure being done among 30.8% cases.[23] Delay in treatment seeking probably would have resulted in good number of RHD cases requiring surgical interventions for management in this study. On the other hand, there might be RHD cases whose misery is added to by delay in timely surgery due to high expenses, lack of education and sometimes patient reluctance.[31]
Mortality rate of 4.9% observed here among RF/RHD cases ranged between 2 and 22.8% in other studies.[6,8,9,11,20,23] Commonest cause of mortality in other studies was CCF with mortality rate due to this condition ranging between 37.5 and 100%. These findings were much higher than our observation.[8,9,11,23] A study done in Nigeria reported proportional mortality rate of infective endocarditis in RHD cases to be 23.8% which was lower than our observation of 50%.[11] A study done in Haryana reported three deaths among ARF patients which was different from our findings where no deaths were reported.[8] The various causes of death in RHD cases highlight conditions requiring prompt management so as to minimize casualties.
Limitation
This was a record based study and thus includes information pertaining to patients referred to a tertiary care hospital. Hence these results may not be applicable to the general population because of referral bias. However, as the study settings was major hospitals in Mangalore, the observed findings in this study can be a good approximation of the disease scenario of targeted hospitals catchment area rather than any geographical area. Also, important information such as reason for noncompliance with treatment was not mentioned in the records and hence could not be analyzed.
Conclusions
Compliance with treatment among cases was found to be poor. If physicians vigorously enforce the long-term prophylaxis among detected cases and also take up the responsibility of educating the patients and their family members regarding importance of compliance with treatment during follow-up, the compliance rate can be further improved.
This study also identified risk factors like history of sore throat infection before disease onset, poor economic and nutritional status among RF cases. Thus, early identification and treating of Streptococcal infection along with improvement of socioeconomic and nutritional factors in the family is an important task required under primary prophylaxis of RF.
Acknowledgments
We thank MBBS students Mr. Tapit Moudgil, Ms. Swati, Ms. Shantanu Singh, Ms. Shreya Sinha, Mr. Joel Samuel Thomas and Ms. Surabhi Chattree of Kasturba Medical College, Mangalore for their help in data collection. We also thank the medical superintendents of these respective hospitals for permitting us to review the medical records.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Carapetis JR. Acute rheumatic fever. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 18th ed. New York: The McGraw-Hill Companies; 2012. pp. 2752–7. [Google Scholar]
- 2.Nordet P. WHO/ISFC Global programme for the prevention and control of RF/RHD. J Int Soc Fed Cardiol. 1993;3:4–5. [Google Scholar]
- 3.Eisenberg MJ. Rheumatic heart disease in the developing world: Prevalence, prevention and control. Eur Heart J. 1993;14:122–8. doi: 10.1093/eurheartj/14.1.122. [DOI] [PubMed] [Google Scholar]
- 4.Haffejee I. Rheumatic fever and rheumatic heart disease: The current status of its immunology, diagnostic criteria and prophylaxis. Q J Med. 1992;84:641–58. [PubMed] [Google Scholar]
- 5.Padmavati S. Rheumatic fever and rheumatic heart disease in developing countries. Bull World Health Organ. 1978;56:543–50. [PMC free article] [PubMed] [Google Scholar]
- 6.Rayamajhi A, Sharma D, Shakya U. Clinical, laboratory and echocardiographic profile of acute rheumatic fever in Nepali children. Ann Trop Paediatr. 2007;27:169–77. doi: 10.1179/146532807X220271. [DOI] [PubMed] [Google Scholar]
- 7.Bajjey M, Radwan A. Spotlight on Current Clinical Profile of Rheumatic Heart Diseases (RHD) and Rheumatic Fever (RF) in Sohag University Hospital (Upper Egypt) 2011. Jan 18, [Accessed Jun 5, 2012]. at http://www.egmedicals.com/pediatric2010/013005.pdf .
- 8.Grover A, Dhawan A, Iyengar SD, Anand IS, Wahi PL, Ganguly NK. Epidemiology of rheumatic fever and rheumatic heart disease in a rural community in northern India. Bull World Health Organ. 1993;71:59–66. [PMC free article] [PubMed] [Google Scholar]
- 9.Agarwal BL, Agrawal R. Rheumatic fever: Clinical profile of the initial attack in India. Bull World Health Organ. 1986;64:573–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Agarwal AK. Social classification: The need to update in the present scenario. Indian J Community Med. 2008;33:50–1. doi: 10.4103/0970-0218.39245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fadahunsi HO, Coker AO, Usoro PD. Rheumatic heart disease in Nigerian children: Clinical and preventive aspects. Ann Trop Paediatr. 1987;7:54–8. doi: 10.1080/02724936.1987.11748474. [DOI] [PubMed] [Google Scholar]
- 12.Ozer S, Hallioglu O, Ozkutlu S, Celiker A, Alehan D, Karagoz T. Childhood acute rheumatic fever in Ankara, Turkey. Turk J Pediatr. 2005;47:120–4. [PubMed] [Google Scholar]
- 13.Arora R, Subramanyam G, Khalilullah M, Gupta MP. Clinical profile of rheumatic fever and rheumatic heart disease: A study of 2,500 cases. Indian Heart J. 1981;33:264–9. [PubMed] [Google Scholar]
- 14.Mathur KS, Banerji SC, Nigam DK, Prasad R. Rheumatic heart disease and rheumatic fever in a village community of Bichpuri block, Agra. J Assoc Physicians India. 1971;19:151–6. [PubMed] [Google Scholar]
- 15.Khatoon M. Clinical profile of rheumatic fever in some hospitalized children of Bangladesh. Bangladesh Med Res Counc Bull. 1985;11:33–8. [PubMed] [Google Scholar]
- 16.Melka A. Rheumatic heart disease in Gondar college of medical sciences teaching hospital: socio-demographic and clinical profile. Ethiop Med J. 1996;34:207–16. [PubMed] [Google Scholar]
- 17.Thakur JS, Negi PC, Ahluwalia SK, Vaidya NK. Epidemiological survey of rheumatic heart disease among school children in the Shimla Hills of northern India: Prevalence and risk factors. J Epidemiol Community Health. 1996;50:62–7. doi: 10.1136/jech.50.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saksena PN, Kapoor VK, Kumar N. Rheumatic fever. Indian J Pediatr. 1969;36:1–4. doi: 10.1007/BF02749357. [DOI] [PubMed] [Google Scholar]
- 19.Al-Charrakh AH, Al-Khafaji JK, Al-Rubaye RH. Prevalence of beta hemolytic groups C and F Streptococci in patients with acute pharyngitis. N Am J Med Sci. 2011;3:129–36. doi: 10.4297/najms.2011.3129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ravisha MS, Tullu MS, Kamat JR. Rheumatic fever and rheumatic heart disease: Clinical profile of 550 cases in India. Arch Med Res. 2003;34:382–7. doi: 10.1016/S0188-4409(03)00072-9. [DOI] [PubMed] [Google Scholar]
- 21.Vasan SR, Shrivastava S, Vijayakumar M, Narang R, Lister BC, Narula J. Echocardiographic evaluation of patients with acute rheumatic fever and rheumatic carditis. Circulation. 1996;94:73–82. doi: 10.1161/01.cir.94.1.73. [DOI] [PubMed] [Google Scholar]
- 22.Setty MR, Shadaksharappa KS, Madappa N, Setty G, Champakamalini Chronic rheumatic heart disease in Bangalore. Indian Heart J. 1972;24:253–6. [PubMed] [Google Scholar]
- 23.Bitar FF, Hayek P, Obeid M, Gharzeddine W, Mikati M, Dbaibo GS. Rheumatic fever in children: A 15-year experience in a developing country. Pediatr Cardiol. 2000;21:119–22. doi: 10.1007/s002469910017. [DOI] [PubMed] [Google Scholar]
- 24.Tani LY, Veasy LG, Minich LL, Shaddy RE. Rheumatic fever in children younger than 5 years: Is the presentation different? Pediatrics. 2003;112:1065–8. doi: 10.1542/peds.112.5.1065. [DOI] [PubMed] [Google Scholar]
- 25.Chockalingam A, Gnanavelu G, Elangovan S, Chockalingam V. Current profile of acute rheumatic fever and valvulitis in southern India. J Heart Valve Dis. 2003;12:573–6. [PubMed] [Google Scholar]
- 26.Kumar R. Controlling rheumatic heart disease in developing countries. World Health Forum. 1995;16:47–51. [PubMed] [Google Scholar]
- 27.Alto WA, Gibson R. Acute rheumatic fever: An update. Am Fam Physician. 1992;45:613–20. [PubMed] [Google Scholar]
- 28.Negi PC, Kanwar A, Chauhan R, Asotra S, Thakur JS, Bhardwaj AK. Epidemiological trends of RF/RHD in school children of Shimla in north India. Ind J Med Res. 2013;137:1121–7. [PMC free article] [PubMed] [Google Scholar]
- 29.Faheem M, Hafizullah M, Gul A, Jan H, Khan MA. Pattern of valvular lesions in rheumatic heart disease. J Postgrad Med Inst. 2007;21:99–103. [Google Scholar]
- 30.Jadoon S, Haider N, Hassan M. Retrospective analysis of 54 patients with acute rheumatic fever. Pak Paed J. 2003;27:118–20. [Google Scholar]
- 31.Bassili A, Zahers SR, Abdel-Fattah M, Tognoni G. Profile of secondary prophylaxis among children with RHD in Alexandrea, Egypt. East Mediterr Health J. 2000;6:437–46. [PubMed] [Google Scholar]


