Abstract
Background:
Dysmenorrhea is a common gynecologic disorder affecting as many as 60% of menstruating women. In the United States, work absenteeism due to dysmenorrhea is estimated to be 600 million work hours per year, and the economic consequences are estimated at $2 billion per year; therefore, it is a public problem nowadays.
Aim:
The purpose of this study was to compare the effects of combination of fennel extract/vitamin E with ibuprofen on the intensity of pain in primary dysmenorrhea among the students of Tabriz city in 2007-2009.
Materials and Methods:
This study was done by using double-blinded quasi-experimental research method. After taking the required licenses from ethics committee, 68 students from Medical and Tabriz universities, who were living in the dormitory, suffering from primary dysmenorrhea, and were eligible for the study, were randomly divided into two groups of 34 students each (the two groups used combination of fennel extract/vitamin E and ibuprofen cross-over form in the 2 months). We used Visual Analogue Scale (VAS) tool for ranking the intensity of the pain. Data analysis was done by using SPSS Ver. 14.
Results:
The mean of peak pain intensity in the first, second, third, sixth, and forty-eighth hours in the group that had used combination of fennel extract/vitamin E was lower than the group that had used ibuprofen, and statistical differences were observed between the two groups in the first and second hours; combination of fennel extract/vitamin E was more effective than ibuprofen in the first hour (P < 0.03) and second hour (P < 0.04).
Conclusion:
Combination of fennel extract/vitamin E is effective on decreasing the intensity of pain of primary dysmenorrhea, and it is advised to those who cannot use chemical drugs.
Keywords: Fennel, ibuprofen, primary dysmenorrhea, vitamin E
INTRODUCTION
Dysmenorrhea is a common gynecologic disorder affecting as many as 60% of menstruating women.[1] Based on the pathology, dysmenorrhea has been classified as primary and secondary.[2] Primary dysmenorrhea refers to menstrual pain without pelvic pathology. The pain of primary dysmenorrhea usually begins a few hours before or just after the onset of menstrual period and may last 48-72 h. The pain is similar to labor pain, with suprapubic cramping, and may be accompanied by lumbosacral backache, with pain radiating down the anterior thigh.[1,2,3] Primary dysmenorrhea is not associated with recognizable pelvic pathology.[3] It is caused due to prostaglandin compounds that cause the contraction of myometrium,[1,4,5] and occurs in 50%-75% of women.[6]
Dysmenorrhea represents a significant personal and public health problem. It is a common complaint of both adolescent and adult women. In the United States, work absenteeism due to dysmenorrhea is estimated to be 600 million work hours per year, and the economic consequences are estimated at $2 billion per year,[7] therefore, it is a public problem nowadays.[8]
A research in Sweden showed that more than 72% of 19-year-old women complained of primary dysmenorrhea. Among those affected, 34% reported mild symptoms, 23% moderate, and 15% reported severe symptoms.[7] In surveys conducted in Iran, the prevalence of primary dysmenorrhea has been reported to be 71%-85.5%.[9,10,11,12]
The different options and nutrition methods used for treating primary dysmenorrhea include: psychotherapy, transcutaneous electrical nerve stimulation (TENS), vitamins, and medicines such as prostaglandin inhibitors, non-steroid anti-inflammatory drugs (NSAIDs), and contraception pills.[13]
Prostaglandin synthase inhibitors, or NSAIDs (such as Ibuprofen), are effective for the treatment of primary dysmenorrhea, but the medication may be contraindicated in patients with gastrointestinal ulcers or bronchospastic hypersensitivity to aspirin. Side effects are usually mild, and include nausea, dyspepsia, diarrhea, and occasionally fatigue.[1]
On the other hand, the use of plants accompanied with synthetic drugs can help to treat the disease. In Iran, folk herbal remedies can be used for healing of dysmenorrhea (such as fennel, chamomile, and marigold). Fennel (Foeniculum vulgare Mill) is an umbelliferous plant.[14] Both the seed and extract of this plant are appetizing, digestive, diuretic, increased health, menstrative, anti-spasmodic, lactigenic, and laxative.[15,16,17]
The study that compared the effect of oral fennel effect and mefenamic acid on primary dysmenorrhea reported no significant difference between them.[18]
The probably effect of fennel might be related to the anti-spasmodic property of this plant. Anethole, the major fragrant in fennel seed, is similar in properties.
Nowadays, vitamins play an important role in the treatment of dysmenorrhea. Studies have shown this property with dopamine. It has been shown that anethole joins with dopamine receptors and decreases pain.[19,20,21,22] Use of these products has no adverse effect of tranquilizers.[23] Vitamin E relieves primary dysmenorrhea, and probably its antioxidant property can suppress the oxidation of arachidonic acid, decreasing the production of prostaglandin.[24,25,26] Iaghmaii et al. reported that vitamin E/mefenamic acid provided grater pain relief than mefenamic acid alone.[27] The aim of this survey was to evaluate the efficacy of fennel extract/vitamin E compared with ibuprofen in the treatment of primary dysmenorrhea, with due attention to the different mechanisms of vitamin E and fennel extract (vitamin E is an antioxidant, and anethole in the extract of fennel is anti-spasmodic).
MATERIALS AND METHODS
This study was a double-blinded, cross-over study. The samples were female students of Tabriz University and Tabriz University of Medical Science, who suffered from primary dysmenorrhea. Inclusion criteria were having a history of primary dysmenorrhea, with regular menses in the last 3 months prior to the first visit, and no previous history of gynecologic disease and of allergy to NSAIDs, or suspected contraindication to herbal remedies, no history of pelvic major surgery, seizure, stressor factor in the last 6 months, severe gastrointestinal disorders, or any diseases that might interfere with the conduct of the study or the interpretation of the results. Exclusion criteria were having pain in the Duration of the menstruation period or before the onset of menstrual bleeding, use of oral hormonal contraception during treatment, having urinary tract infection in the study period, simultaneous participation in another clinical trial or participation in another clinical trial prior to study entry that might have an impact on the study objectives at the discretion of the investigator. The data were collected by using Visual Analogue Scale (VAS; questionnaire number 1, 2). For validation of the questionnaire, we used content validity that was conducted by 10 academic members of Tabriz University of Medical Science. For questionnaire reliability, test-retest was used. This study was undertaken with approval of the Tabriz University and Tabriz University of Medical Science ethics committee. Students who had the criteria for admission, and want to participate in the trial were asked to give their informed consent. The questionnaires were distributed to the students, and they were asked to fill them up. They were asked about demographic characteristics, menstrual health, general health, and intensity of menstruation pain. The researchers requested the participants who completed the questionnaire in the next month without use of any drugs. After that, the eligible students were determined; every student was randomly (Systematic Random Sampling) assigned to fennel/vitamin E group or ibuprofen group (34 participants in each group). For both groups, questionnaires 1 and 2 and drug packages with randomization codes of A and B were dispensed. The shape, size, and color of the capsule of drugs were similar. The subjects were requested to record the intensity of menstrual pain by VAS at 1, 2, 3, 6, 12, 24, and 48 h after the onset of bleeding. The first group used package A in the first month and package B in the second month. The second group was treated by package B in the first month and package A in the second month. Packages A and B contained fennel extract/vitamin E and ibuprofen. The study was double-blinded, i.e. the researcher and students did not know which medication was administered.
Statistical analysis
Data were analyzed using SPSS version 14. Decrease in pain on using fennel extract/vitamin E and ibuprofen was expressed as mean ± SD. Wilcoxon test was used to compare the pain intensity between the two groups. P value <0.05 was considered as significant.
RESULTS
The mean age of the respondents was 21.8 ± 2.5 years. The mean of menstrual cycle duration was 28.1 ± 1.5 days, and the mean age of menarche was 16.1 ± 1.7 years [Table 1].
Table 1.
Characteristics of the study population on entry to the trial

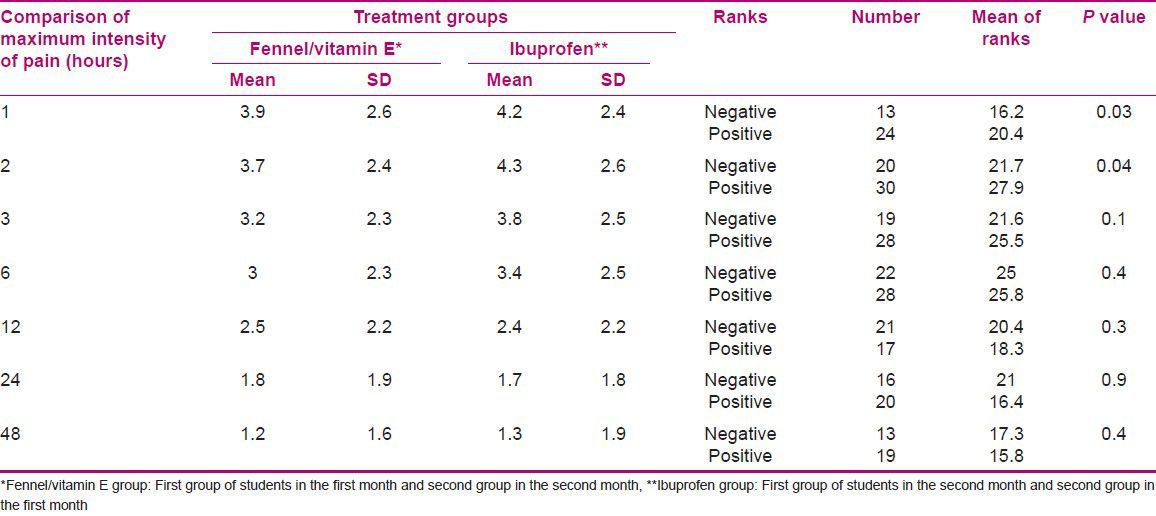
In our study, we found that 60.3% of subjects had missed school or daily activities due to dysmenorrhea, 89.7% participants reported use of tranquilizers, and 22.1% had family history of dysmenorrhea. The mean of maximum pain intensity in the fennel/vitamin E group at 1, 2, 3, 6, 48 h after administration was lower than the mean of maximum pain intensity in the ibuprofen group, although fennel extract/vitamin E composition was significantly more potent than ibuprofen in the first and second hours [Table 2].
Table 2.
Results of comparison of the severity of dysmenorrhea before and after intervention in both groups and between groups
DISCUSSION
This analysis includes 68 female students who suffered from dysmenorrhea. The mean age was 21.8 ± 2.5 years. In this study, the age of onset of menarche was 13.8 ± 1.3 years, the mean of menstrual cycle interval was 28.1 ± 1.5 days, and the mean of menstrual cycle duration was 5.9 ± 1.1 days. Our finding is in agreement with the findings of Norouzi et al. in Bushehr,[28] Modarres Nejad et al. in Rafsanjan,[18] and Ozgoli et al. in Tehran.[29]
The age of menarche in this study was at least 11 years, and in Norouzi et al.'s study conducted in Bushehr in 2003, it was reported to be 9 years (28). The age of dysmenorrhea onset was 16.1 ± 1.7 years, and in Modarres Nejad et al.'s survey in Rafsanjan in 2006, it was 13.7 ± 1.1 years.[18] Moreover, Tarke Zahrani and colleagues reported the age of onset of dysmenorrhea in Tehran to be 14.46 ± 1.43 years.[30] The discrepancy between the age of menarche and the age of onset of dysmenorrhea that we reported and in the above-mentioned surveys may be due to the individual, social, and environmental differences. The mean of pain intensity score in this study was 6.5 ± 1.6, which is in agreement with that reported by Iaghmaii et al. in Zahedan in 2005.[27]
The prevalence of use of tranquilizers before study was 89.7%. In another survey in Tehran (2007), 95.7% of the participants reported using another drug for pain relief in the case group and about 95.5% used these drugs in the control group.[30] The mentioned survey results are similar with our findings. Our study found that the mean of maximum pain intensity in fennel/vitamin E group was lower than that of ibuprofen group at 1, 2, 3, 6, and 48 h, although based on Wilcoxon test, this difference was statistically significant only in the first and second hours. Fennel extract/vitamin E was more potent than ibuprofen at 1 and 2 h (P < 0.03 and P < 0.04, respectively). No randomized control trial has examined the efficacy of fennel/vitamin E on dysmenorrhea, but Iaghmaii et al. (2005) in Zahedan compared the effect of mefenamic acid and vitamin E with that of mefenamic acid alone on pain and their results are consistent with our findings. Results showed that the mean of maximum pain difference before and after treatment in the group receiving mefenamic acid and vitamin E was 48.5 ± 17.5, but in the group taking mefenamic acid and placebo, this scale was 25.9 ± 21, and the difference was significant (P < 0.001).[27] Also, Tarke Zahrani and colleagues and Namavar Jahromi et al.'s results on the effect of F. vulgare on primary dysmenorrhea,[30,31] Modarres Nejad et al.'s results of their study in Rafsanjan about the effect of F. vulgare and mefenamic acid on the intensity pain in primary dysmenorrhea,[18] Farahmad et al.'s study results about the effect of vitamin E and brufen on primary dysmenorrhea,[32] Ziaei et al.'s study results about the effect of vitamin E in the treatment of primary dysmenorrhea[26] were similar to our findings.
CONCLUSION
Combination of fennel extract/vitamin E is effective on decreasing the intensity of pain of primary dysmenorrhea and it is advised to those who cannot use chemical drugs.
ACKNOWLEDGMENTS
This study was performed with financial support from Research Deputy of Tabriz University of Medical sciences, Tabriz, Iran. Also, the authors express their appreciation for all participants of this study for making this study possible.
Footnotes
Source of Support: None
Conflict of Interest: None declared.
REFERENCES
- 1.Jonathan S, Berek MD. 15th ed. Philadelphia: Williams and Wilkins; 2012. Novak's Gynecology; pp. 481–3. [Google Scholar]
- 2.Berek G. 13th ed. Philadelphia: Lippincott Williams and Wilkins; 2003. Novak's Gynecology; pp. 393–5. [Google Scholar]
- 3.Berek y. 14th ed. Philadelphia: Wilkins company; 2007. Novak's Gynecology; pp. 516–9. [Google Scholar]
- 4.Sperroff L, Fritz MA. 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. Clinical gynecologic endocrinology and infertility; p. 473. [Google Scholar]
- 5.Thomas E, Andreoli-charles CY, Carpenter Robert C, Criggs- Joseph Loscalzo. 6th ed. Philadelphia: Saunders; 2004. Cecil Essentials Medicine; pp. 651–2. [Google Scholar]
- 6.Mackay HT. Current Medical Diagnosis a Treatment. 41th ed. New York City, U.S: The McGraw — Hill companies; 2002. Gynecology; p. 748. [Google Scholar]
- 7.Ahmed M, Minawi EL, Fred M. Howard. Pelvic Pain Diagnosis and management. Philadelphia: LWW; 2000. Dysmenorrhea; pp. 100–9. [Google Scholar]
- 8.Hsua CS. Effect of “Dang – Qui – Shao – Yao-San” a Chinese medicinal prescription for dysmenorrhea on uterus contractility in vitro. Phytomedicine. 2006;13:94–100. doi: 10.1016/j.phymed.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 9.Pour eslami M, Amin A, Sarmast H. Knowledge, attitude and practice of girl student of 15-18 years about dysmenorrhea and menstrual health in Karaj high schools. Iran J Iazd Univ Med Sci. 1998;9:30–3. [Google Scholar]
- 10.Jalili Z, Safi ZH, Shams PN. Prevalence and facing of primary dysmenorrhea in college students in Sirjan. Iran J Paiesh. 2004;4:61–7. [Google Scholar]
- 11.Mirzaii F, Bakhshi H, Iasini M, Bashar DN. Frequency of primary dysmenorrhea according by personality type in girl students, at Rafsanjan high schools — 2001. Iran J Rafsanjan Univ Med Sci. 2003;2:151–7. [Google Scholar]
- 12.Kamjou A. Prevalence and intensity of primary dysmenorrhea and some of its related risk factors in dormitory students. Iran J Hormozgan Univ Med Sci. 2001;5:6–9. [Google Scholar]
- 13.Speroff L, Fritz MA. 7th ed. Philadelphia: Williams and Wilkin Company; 2005. Clinical gynecologic endocrinology and infertility; p. 342. [Google Scholar]
- 14.Mir HH. 2nd ed. Vol. 2. Tehran Islamic culture press; 1996. Application of plants in prevention and treatment of disease; pp. 234–8. [Google Scholar]
- 15.Zargari A. 5th ed. Vol. 2. Tehran, Iran: Tehran University press; 1991. Herbal remedies; pp. 553–6. [Google Scholar]
- 16.Valenth ZH. Tehran Rah Kamalco; 2002. Herbal remedies, Treatment by plants; p. 247. [Google Scholar]
- 17.Ahmadi L, Baher Niz Z, Barazande Kamkar M, Rezaii M, Sefid Kon F, Sharifi A, et al. 1st ed. Iran: Alavi Publisher; 2001. Iran herbal and aromatic remedies, Forest research center; p. 13. [Google Scholar]
- 18.Modares Nejad V, Motamedi B, Asadi pour M. Comparison of oral Fennel and Mefenamic acid on pain relief of primary dysmenorrhea. Iran J Rafsanjan Univ Med Sci. 2006;5:1–6. [Google Scholar]
- 19.Khorshidi N. Clinical effects of essential oil on primary dysmenorrhea. Iran J pharmacist Skill. 2003;2:89–93. [Google Scholar]
- 20.Alexandrovich I. The effect of Fennel (Foeniculum Vulgar) seed oil emulsion in infantile. Alternate Therap Health Med. 2003;9:58. [PubMed] [Google Scholar]
- 21.Ostad SN, Soodi M, Sariffzadeh M, Khoshidi N, Marzban H. The effect of fennel essenyial oil on uterine contraction as a model for dysmenorrheal, pharmacology and toxicology study. J Ethnopharmacol. 2001;76:299–304. doi: 10.1016/s0378-8741(01)00249-5. [DOI] [PubMed] [Google Scholar]
- 22.Fleming T. 2nd ed. Montrale Medical Economics Company; 2000. PDR for Herbal medicines; pp. 302–4. [Google Scholar]
- 23.Proctor ML, Murphy PA. Herbal and dietary therapies for primary and secondary dysmenorhea. Cochrane Database system Rev. 2001:CD002124. doi: 10.1002/14651858.CD002124. [DOI] [PubMed] [Google Scholar]
- 24.Wu D, Mura C, Beharka AA, Han SN, Paulson KE, Hwang D, et al. Age-associated increase in PGE 2 synthesis and COX activity in murin macrophages is reversed by vitamin E. Am Physiol SOC. 1998:661–6. doi: 10.1152/ajpcell.1998.275.3.C661. [DOI] [PubMed] [Google Scholar]
- 25.Ellattar TM, Lin HS. Effect of vitamin C and vitamin e on prostaglandin synthesis by fibroblasts and squamous carcinoma cells. Prostaglandins Leukot Essent Fatty Acids. 1992;47:253–7. doi: 10.1016/0952-3278(92)90194-n. [DOI] [PubMed] [Google Scholar]
- 26.Ziaei S, Faghihzadeh S, Sohrabvand F, Lamyian M, Emamgholy T. A randomized placebo controlled trial to determine the effect of Vitamin E in treatment of primary dysmenorrhea. Br J Obstet Gynecol. 2001;108:1181–3. doi: 10.1111/j.1471-0528.2003.00279.x. [DOI] [PubMed] [Google Scholar]
- 27.Iaghmaii M, Mir teimouri M, Mokhtari M, Mohammadi M. Comparison of Mefenamic acid / Vitamin E and Mefenamic acid effect on primary dysmenorrhea. Iran J Fertil Steril. 2005;6:187–93. [Google Scholar]
- 28.Nouruzi A, Tahmasebi R, Kamali F. Comparison of Ibuprofen, Naproxen and Mefenamic acid effect on primary dysmenorrhe pain and symptoms. Iranian J Teb jonoob J Bushehr Univ Med Sci. 2003;6:45–51. [Google Scholar]
- 29.Ozgoli Gh, Goly M, Moatar F, Velaii N. Comparison of ginger with Mefenamic acid and Ibuprofen on primary dysmenorrhea treatment. Iran J Pajhuhesh Pezeshkey J Shahid Beheshti Univ Med Sci. 2007;31:61–5. [Google Scholar]
- 30.Tark ZS, Akhavan AM, Mojab M, Alavi MH. Effect of Fennel extract on primary dysmenorrhea. Iran J Fertil Steril. 2007;8:45–51. [Google Scholar]
- 31.Namavar Jahromi B, Tartifizadeh A, Khabnadideh S. Comparison of fennel and mefenamic acid for the treatment of primary dysmenorrhea. Int J Gynaecol Obstetr. 2003;80:153–7. doi: 10.1016/s0020-7292(02)00372-7. [DOI] [PubMed] [Google Scholar]
- 32.Farahmand M, Zahedi asl S, Abbaspour Z, Rasekh A. Comparison of Ibuprofen and Vit E effect on primary dysmenorrhea pain intensity. Physiol Pharmacol. 2005;9:139–42. [Google Scholar]


