Abstract
Background:
Most countries use educated nurses called “nurse practitioners” (NPs) besides the family physicians for diagnosis, treatment, and specifically health education of the family. The main goal of this study was to redefine the role of NPs for better use of their capabilities in the so-called “family physician reform” in Iran.
Materials and Methods:
This is a qualitative and comparative study carried out in three stages (triangulation method) in 2011. In the first stage, we conducted a literature review to design a conceptual framework. The second stage was a comparative study on four countries. In this study, we focused on the role of NPs, which in turn helped to redefine this role in the health sector reform of Iran. In the third stage, two expert panels were involved and the suggested roles were confirmed.
Results:
In the United States, NPs are licensed by the state in which they practice and have a national board certification. In Canada, nurses involved in clinics should participate in specific training course of diagnosis and management of health care after registration. In Austria, nurses in Nursing homes and maternity do some of the medical procedures under the supervision of the physicians. In the United Kingdom, NPs increasingly substitute for GPs in the care of minor illness and routine management of chronic diseases.
Conclusions:
There is still debate in nursing and medical circles about what the focus of the NP roles should be. In Iran, whereas a noticeable reform toward “family physician” is ongoing, redefining the nurses’ role is essential. They can perform more active roles in associating with GPs in the clinics of family physicians, both in urban and rural areas, even with higher degrees of autonomy.
Keywords: General practitioner, health care sector, Iran, nurse practitioner, reform
INTRODUCTION
In 1978, Primary Health Care was seen as the solution to the inadequate illness management systems that had developed throughout the world. It was hoped that PHC would address some of the major inequalities in health that were observed by a balanced system of treatment and disease prevention. The World Health Organization (WHO) envisaged that PHC would take place as close as possible to where people live and work and be the first element of a continuing health care process. Additionally, health service collaboration and multi-professional partnerships were expected to replace professional boundaries and competition.[1,2] To sum up, PHC used family physician as the most important ways to increase equitable access and utilization of public health services.
In any case, family physician, with the key elements of first contact, comprehensiveness, continuity, and coordination of patient care, is central to the health of any health care system.[2]
Recent government initiatives are supporting general practice to deliver health care through a variety of means and personnel. These initiatives have included expanding the roles of nurses in general practice and enabling better access to allied health services through general practitioners (GPs). Evidence clearly indicates the effectiveness of teams in improving the outcomes, especially in chronic disease.[3,4]
Now, people in most of the countries use professional and educated nurses [called nurse practitioner (NP)] besides family physician or are under their supervision for diagnosis, treatment, and specifically health education of the family.
In accordance with the International Council of Nurses definition, “A nurse practitioner is a registered nurse who has acquired the expert knowledge base, complex decision-making skills, and clinical competencies for expanded practice, the characteristics of which are shaped by the context and/or country in which s/he is credentialed to practice. A Master's degree is recommended for entry level.”[5]
The Royal College of Nursing (RCN) defines an NP as a registered nurse who has undertaken a specific course of study of at least first-degree (Honors) level and who:
Makes professionally autonomous decision, for which he or she is accountable;
Works collaboratively with other health care professionals;
Provides counseling and health education;
Screens patient for disease risk factors and early signs of illness; and
Has the authority to admit or discharge patients from their caseload, and refers patients to other health care providers as appropriate.[6]
In new reform toward family physician in Iran, there is not enough attention toward nurses, their services, and specifically their role in education and counseling. According to the health-for-all goals, the central concern of nurses in primary care should be the prevention of the disease by educating individuals and families on healthy lifestyles, and teaching community health workers and traditional birth practitioners to carry out many of the functions that nurses themselves have normally performed.[7] Whereas a big part of the family physician program has not been realized in Iran yet (especially in big cities with a population of over 20,000), most graduate nurses are now working in the School of Nursing and Midwifery, hospitals, and ambulatory clinics with limited responsibilities. In addition, most graduate nurses in our community can play an important role in preventing medicine and family physician team.[8] Consequently, in spite of their ability and capacity, They have a brief role in our family physician team & their job description.
MATERIALS AND METHODS
The main goal of this study was to review the role and situation of NPs in the new reform for better use of their capabilities in health care services. This is a qualitative, comparative (role of nurses in family physicians’ team), and cross-sectional study that was carried out with triangulation method in three stages in 2011. In the first stage, we conducted a literature review to design a conceptual framework. The second stage was a comparative study on four countries that had great experiences in these two fields (family physician reform and NPs) and included USA, UK, Austria, and Canada, based on purposive sampling.
In the third stage, six experts in two panels revised and finally confirmed the suggested roles. All experts were completely familiar with the health system and had academic and research experiences in nursing education system in Iran.
RESULTS
First stage: Literature review
The survey on health systems in different countries indicates that many of the health sectors have begun their reforms with two main goals, including quality improvement and cost limiting. Family physician and referral system are among the few options that can maintain and even upgrade the quality of services, reducing the costs simultaneously. As each health system in each country has its specific referral system, Iran is now on the verge of implementing a “best fit” referral system reform. So, it is crucial to well define the roles of each component, such as nurses, in this system.
Second stage: Comparative study
In the United States, NPs are licensed by the state in which they practice, and have a national board certification (usually through the American Nurses Credentialing Center or American Academy of Nurse Practitioner). Most NPs specialize in a particular field of medical care, and there are as many types of NPs as there are medical specialties.
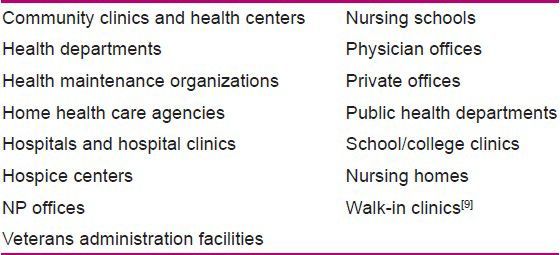
NPs provide high-quality, cost-effective individualized care that is comparable to the health care provided by the physicians, and NP services are often covered by insurance providers. NPs practice in all the states. Some institutions in which they work include the ones given in Table 1.
Table 1.
Role of nurses in some organizations
In Canada, the nurses involved in clinics should participate in specific training course of diagnosis and management of health care after registration. Then, they are allowed to prescribe drugs, and lab and other diagnostic tests. Having access to patient medical record, NPs can reduce unnecessary visits.
According to the standards of practice for NPs, the College of Nurses of Ontario states that they offer “the full scope of primary health care practice, including consultation with physicians or other health care professionals when the client requires care beyond the NPs’ scope of practice.” Further, they are accountable for establishing a consultative relationship with a physician and consultation occurs with a family physician; however, NPs may consult with a specialist physician, if appropriate to the situation and practice setting. No legislative or regulatory deterrent related to the scope of practice exists for the NPs to refer to specialist physicians.[10]
In Austria, nurses in Nursing home and maternity do some of the medical procedures under the supervision of physicians. These nurses are educated, and can treat, inject drugs, and request for some diagnostic tests for their patients.[11]
In the United Kingdom, the GPs’ monopoly on primary care has been broken by nurse-led services, including NHS Direct, which provides 24-h health advice by telephone, and NHS walk-in centers, which treat minor illness and injury. Practice nurses and NPs increasingly substitute for GPs in the care of minor illness and routine management of chronic diseases such as asthma, diabetes, and coronary heart disease. In England and Wales, the role of the NPs had evolved from that of undertaking traditional, medically prescribed nursing tasks in a treatment room to undertaking screening activities and health assessments of new patients, with over 50% of the NPs managing chronic disease clinics.[11]
Third stage: Expert panels
Six experts in two panels were asked to confirm the role of nurses in family physician reform. They suggested that special courses are needed to empower our graduated nurses for their new rules. Meanwhile, using NPs as substitution of GPs does not seem to be logically correct due to the GPs’ workload and the social and cultural background in Iran.
DISCUSSION
According to the WHO, in most countries, nurses are the most important group of health workers in terms of numbers, closeness to people and their health problems, and understanding of community needs.[12]
There is still debate in nursing and medical circles about what the focus of their role should be. For example, Lauder, Sharkey, and Reel suggest that NPs and GPs in rural and remote areas should be interchangeable and that the focus should be on the competency of the person delivering care rather than the right of one discipline (medicine) to perform a particular role.[13] In contrast, Campbell believes that public acceptance of nurses as GP substitutes would be poor, and therefore suggests that a better role for nurses in primary care would be health education and illness prevention.[14] On the other hand, in our country (Iran) until now, nurses have not got a competent role in health sector reform.
Consumers and their consumptions have a great value in this case. Given that consumers have limited understanding of PHC, it is not surprising they do not articulate confidence in NPs acting autonomously but rather as complementary to GPs, perhaps undertaking initial assessment for triage purposes and providing ongoing management, education, and support under the GPs’ delegation. They would also like them to be family oriented and holistic in their practice, supporting their emotional and social needs in the context of their family lives.[15]
It means that any effort to change nurses’ roles in health care services should accompany with some social and cultural changes toward their competencies.
In Iran, whereas a noticeable reform toward “family physician” is going on, redefining nurses’ role is essential. They can perform more active roles in associating with GPs in the clinics of family physicians, both in urban and rural areas, even with higher degrees of autonomy. Their competencies for case management, education, treatment, and follow-up may repair many of the pitfalls we are confronting in health care services. Of course, if it has to be done, special courses are needed to empower graduated nurses for their new rules. Meanwhile, substitution of GPs with NPs does not seem to be a good suggestion due to GP workload and social and cultural background in Iran.
Thus, it can be concluded that in order to achieve the goals of family physicians’ reform and also utilize the maximum capacity of trained nurses, a fixed and definite place must be considered for them in the GP team to provide their services under the supervision of family physicians. Their active role not only enriches the family physician team, but also might be crucial in patients’ training, which is currently one of our weaknesses.
Footnotes
Source of Support: Tehran University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Geneva: WHO, Manila; 2001. World Health Organization. Mid-level and nurse practitioners in the Pacific: Models and Issues. [Google Scholar]
- 2.Van Der Weyden M. Australian General Practice: Time for renewed purpose. MJA. 2003;179:6–7. doi: 10.5694/j.1326-5377.2003.tb05404.x. [DOI] [PubMed] [Google Scholar]
- 3.Wanger E, Austain B, Von Korff M. Organizing Care for Patients with Chronic illness. Milbank Q. 1996;74:511–34. [PubMed] [Google Scholar]
- 4.Sibbald B, Luarant M, Scott TA. Changing task profiles. In: Saltman RB, Rico A, Boerma W, editors. Primary care in the driver's seat? Organizational reform in European primary care. Berkshire, UK: Open University Press; 2006. pp. 149–64. [Google Scholar]
- 5.International Council of Nurses Announces Position on Advanced Nursing Roles Geneva IC. [Last accessed on 2003 March 21]. Available from: http://www.icn.ch/pr19_02.htm .
- 6.Royal college of nursing. Statement on the role and scope of nurse practitioner practice. 2005. [Last accessed on 2013 Feb 11]. p. 4. Available from: http://www.rcn.org.uk/direct .
- 7.Mozafari M, Delpisheh A. 1st ed. Ilam, Iran: Gouyesh; 2003. Community oriented nursing education. [Google Scholar]
- 8.Iran nooiro. 1st ed. Tehran: Nursing Organization of Islamic Republic of Iran; 2006. Text book of nursing care standards. [Google Scholar]
- 9.Rollet J, Lebo S. Salary Survey Results. Advance for Nurse Practitioners. 2009 [Google Scholar]
- 10.Nurse Practitioners’ Association of Ontario; [Last accessed on 2013 Feb 11]. Position Statement Nurse Practitioner Referral to Specialists; p. 4. Available from: http://www.npao.org . [Google Scholar]
- 11.Buchan J, Calman L. OECD Health Working Paper, No. 17; 2005. “ Skill Mix and Policy Change in the Health Workforce: Nurses in Advanced Roles”. [Google Scholar]
- 12.WHO Technical Report Series; 1994. World Health Organization. nursing beyond the year 2000: Report of a WHO study group. No 860. [PubMed] [Google Scholar]
- 13.Lauder W, Sharkey S, Reel S. The development of family health nurses and family nurse practitioners in remote and rural Australia. Aust Fam Physician. 2003;32:750–2. [PubMed] [Google Scholar]
- 14.Campbell S. The newest gatekeepers: Nurses take on the duties of primary care. Health Care Strateg Manage. 1997;15:14–5. [PubMed] [Google Scholar]
- 15.Wilson A, Pearson D, Hassey A. Barriers to developing the nurse practitioner role in primary care: The GP perspective. Fam Pract. 2002;19:641–6. doi: 10.1093/fampra/19.6.641. [DOI] [PubMed] [Google Scholar]


