Abstract
Background:
Providing high-quality care in the intensive care units (ICUs) is a major goal of every medical system. Nurses play a crucial role in achieving this goal. One of the most important responsibilities of nurses is sedation and pain control of patients. The present study tried to assess the effect of nurses’ practice of a sedation protocol on sedation and consciousness levels and the doses of sedatives and analgesics in the ICU patients.
Materials and Methods:
This clinical trial was conducted on 132 ICU patients on mechanical ventilation. The patients were randomly allocated to two groups. While the control group received the ICU's routine care, the intervention group was sedated by ICU nurses based on Jacob's modified sedation protocol. The subjects’ sedation and consciousness levels were evaluated by the Richmond Agitation Sedation Scale (RASS) and the Glasgow Coma Scale (GCS), respectively. Doses of administered midazolam and morphine were also recorded.
Results:
The mean RASS score of the intervention group was closer to the ideal range (−1 to +1), compared to the control group (−0.95 ± 0.3 vs. −1.88 ± 0.4). Consciousness level of the control group was lower than that of the intervention group (8.4 ± 0.4 vs. 8.8 ± 0.4). Finally, higher doses of midazolam and morphine were administered in the control group than in the intervention group.
Conclusion:
As nurses are in constant contact with the ICU patients, their practice of a sedation protocol can result in better sedation and pain control in the patients and reduce the administered doses of sedatives and analgesics.
Keywords: Consciousness level, nurse, pain, sedation, sedation protocol
INTRODUCTION
Providing appropriate sedation is currently one of the most important aspects of nursing care for patients receiving mechanical ventilation in the intensive care units (ICUs). Although sedation has to prevent patients from having painful experiences in the ICU, deep sedation and its side effects must be avoided.[1,2] In order to sedate patients in the ICUs, physicians prescribe tranquilizers according to patients’ needs, and nurses administer the drugs based on their conditions.[3,4,5] Nurses’ understanding of patients’ clinical conditions may influence the level of sedation and lead to deep or inadequate sedation. Previous research has shown that more experienced nurses in the ICUs tend to administer lower doses of tranquilizers and first try to use non-pharmacological measures to relieve the anxiety and restlessness of patients.[3,6]
The Society of Critical Care Medicine has proposed the use of sedation guidelines and protocols in order for the health care team to reach a consensus about patient sedation.[7] Robinson et al. showed that using sedation protocols in the ICUs can decrease patients’ need for mechanical ventilation and shorten their hospital stay.[8] Similarly, Marshall et al. reported that performing a sedation protocol by a pharmacologist in the ICU can decrease patients’ need for mechanical ventilation.[9] The first study on the use of a sedation protocol by ICU nurses was conducted by Brook et al. in 1997. After evaluating 321 patients with acute respiratory failure and requiring mechanical ventilation, they reported that the application of a sedation protocol by nurses could decrease the patients’ need for mechanical ventilation and tracheostomy.[10]
In Iran, however, sedation protocols or criteria are not followed. In fact, patients in the ICUs are sedated based on the prescriptions of the physicians and by nurses. The possible use of high doses of tranquilizers and analgesics such as midazolam and morphine can result in cardiovascular and respiratory complications.[11] As patients’ level of consciousness in the ICUs is affected by the method of sedation, complications such as delayed separation of patients from the ventilator and pressure ulcers may occur due to inappropriate sedation. Considering the important role of nurses in the sedation of patients and the inadequate data available in this regard, the present study aimed to examine the effects of the application of a sedation protocol by ICU nurses on patients’ sedation and consciousness levels, and the use of tranquilizers and analgesics.
MATERIALS AND METHODS
This clinical trial was conducted on 132 patients receiving mechanical ventilation in three ICUs of a hospital in Kerman, Iran. It was approved by the president of the hospital and the technology and research committee of Kerman University of Medical Sciences (Kerman, Iran). The inclusion criteria were ICU stay of at least 48 h, a score of higher than 7 on the Glasgow Coma Scale (GCS), being 15-48 years of age, requiring mechanical ventilation, lack of any underlying problems of the heart, lung, kidney, and liver, and not being allergic to midazolam and morphine.
Eligible subjects were randomly allocated to two groups of control and intervention. For randomization purpose, patients who were hospitalized at the beginning of the study were numbered. A nurse, unaware of the study and the groupings, was then asked to randomly select the numbers from a table and place them in the two groups. For allocation of patients who were hospitalized after the study had started, the first patient was randomly placed in one of the groups. Every other patient was also placed in the same group. The rest of the patients were allocated to the other group.
As the patients were unconscious, their immediate families were explained about the study and their consent was obtained. The control group received the routine care of the ward, i.e. the doctor prescribed sedatives and the nurses administered the drugs according to the patients’ clinical status and their own personal judgment. In the intervention group, patients were sedated after the ICU nurses had assessed them by the Richmond Agitation Sedation Scale (RASS) and Jacob's Sedation Protocol[12] [Figure 1]. The sedation protocol included 48 h of intravenous injection of midazolam and morphine to maintain the sedation level of patients between −1 and +1 according to the RASS.
Figure 1.
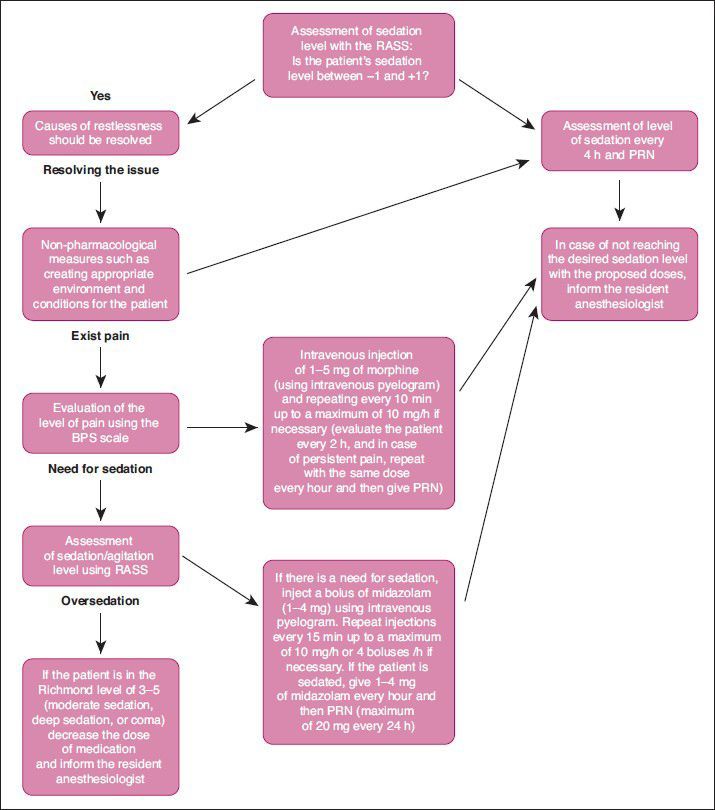
The sedation and pain control protocol of patients receiving mechanical ventilation in intensive care unit RASS: Richmond Agitation-Sedation Scale; BPS: Behavioral Pain Scale; PRN: Pro Re Nata
First, patients’ levels of irritability and restlessness were evaluated according to the RASS, and its underlying causes (airway obstruction, urinary retention, noise and environmental conditions, patient's position, and splints) were resolved. In case of persisting irritability, pain was assessed by the Behavioral Pain Scale. If pain existed, non-pharmacological methods were initially employed to resolve its causes. Continuing restlessness and pain were treated with a minimum dose of tranquilizers and analgesics.
A 1-day workshop was held by the researchers at the hospital to train the nurses with the protocol of sedation. Any problems of the nurses were then recognized and solved. The trained nurses conducted the protocol in the ICU for 2 weeks prior to the research to become more familiar with it. During each shift, patients’ level of alertness was measured three times using the GCS. Moreover, the amounts of midazolam and morphine used for each patient were recorded in milligrams in a specific form. Patients who needed a different drug, such as fentanyl for sedation and pain control, were excluded from the study. In all stages, the ICU specialist supervised the study and offered necessary instructions in case of an emergency to avoid any harm to the patients.
Descriptive statistics, Pearson correlation, and independent t-test were used to analyze the collected data. All analyses were performed with SPSS for Windows 15.0 (SPSS Inc., Chicago, IL, USA). P values less than 0.05 were considered significant.
RESULTS
Of the 132 patients who participated in this study, 85% were men and 15% were women. The mean age of the patients was 37.2 years. The most common cause of hospitalization was intracranial hemorrhage in the intervention group (19.7%) and multiple traumas in the control group (20.5%). While 97% of the subjects were connected to the ventilator via an endotracheal tube, a tracheostomy tube was employed for the remaining 3%.
Before the initiation of the study, the mean RASS score was 0.85 ± 0.7 in the control group and 0.9 ± 0.6 in the intervention group (P > 0.05). After entering the study, the scores changed to −1.88 ± 0.4 in the control group and −0.95 ± 0.3 in the intervention group (P < 0.05). The mean scores of GCS in the control and intervention groups were 8.4 ± 0.4 and 8.8 ± 0.4, respectively (P < 0.05).
The mean doses of midazolam and morphine were significantly lower in the intervention group than in the control group (2.7 ± 0.6 vs. 3.7 ± 0.7 mg and 3.3 ± 0.6 vs. 4.2 ± 0.6 mg; P < 0.05). Pearson correlation coefficient showed a significant, indirect correlation between the dose of midazolam and RASS scores in both groups (P < 0.05; r = 0.470). It also indicated a significant, direct correlation between patients’ level of alertness and RASS scores (P < 0.05; r = 0.127). Based on the results of the independent t-tests, there were no significant relations between sex and RASS scores, level of alertness, and the mean doses of midazolam and morphine (P > 0.05).
DISCUSSION
ICU patients are restless and need sedation due to many reasons such as device noises, loss of contact with the outside environment, little differentiation between day and night, intubation, mechanical ventilation, underlying issues, and pain. Ideal sedation level should be neither deep nor inadequate. Planning and intervention of the medical team are essential in this regard. In the current study, the mean RASS score of the intervention group was closer to the ideal score (between −1 and +1), compared to the control group. In other words, sedation was better controlled in the intervention group. Other studies have reported controversial findings in this respect. In a study from Australia, Bucknall et al. suggested that using a sedation protocol (different from ours) does not have much effect on the ICU patients’ sedation level.[13] In contrast, Eduardo et al. assessed 40 patients on mechanical ventilation and found that using a sedation protocol improved the quality of sedation in ICU patients.[14]
Apparently, employing a sedation protocol is beneficial in inducing an appropriate level of sedation among the ICU patients. Using a protocol makes nurses find the causes of patients’ restlessness before administering tranquilizers and analgesics. Identifying various causes of restlessness that do not require pharmacological measures, such as noise in the ICU, will prevent the unnecessary use of drugs and, hence, deep sedation. Since nurses are in constant contact with the patients, sedation and pain control protocols should preferably be practiced by ICU nurses than by other members of the medical team. Therefore, providing nurses with more and higher quality education on sedation and pain control must be a priority of the educational systems.
In the present study, the intervention group had higher consciousness compared to the control group, i.e. deep sedation was less frequent among the patients in the intervention group. Previous research has also indicated a correlation between usage of a sedation protocol and level of consciousness of ICU patients.[15,16,17,18] Reduction in the consciousness level of the patients caused by deep sedation can have many risks such as reduced respiratory activity, delayed separation from the ventilator, increased duration of hospitalization, and increased risk of infection and pressure ulcers for ICU patients.[15,19,20,21,22,23] According to the available literature, sedation breaks, which make the patients conscious, cause their earlier separation from the ventilator and decrease their duration of hospitalization.[16,17,18]
In our study, the application of a sedation protocol by nurses decreased the amount of tranquilizer and analgesic intake. Such a finding seems logical since most cases of restlessness and pain among the ICU patients can be controlled by non-pharmacological measures such as correct method of bandaging, appropriate position of the patient's body, removing tension from the areas that are unnecessarily under pressure, and creating a peaceful environment. Likewise, Eduardo et al. reported reduced midazolam consumption in patients who were sedated using a protocol.[14] Although midazolam is one of the main sedative drugs used in the ICUs, its family (including lorazepam) of drugs have interactions with many other drugs used (such as phenytoin) in the ICU.[24] It appears that using a protocol can reduce the occurrence of drug interactions in ICU patients by reducing the number of prescriptions for sedatives. However, more research is necessary in this respect.
CONCLUSION
As nurses are continually present by their patients’ side during their shifts, they can play a crucial role in appropriate sedation of the patients. Many of the causes of pain and anxiety in ICU patients can be resolved by non-pharmacological measures. Thus, it is time for nursing education systems to pay more attention to educating nurses about sedation and pain control of ICU patients.
ACKNOWLEDGMENT
The researchers would like to thank the ICU nurses who helped them conduct this study.
Footnotes
Source of Support: None
Conflict of Interest: None declared.
REFERENCES
- 1.Brush DR. Sedation and analgesia for the mechanically ventilated Patient. Clin Chest Med. 2009;30:131–41. doi: 10.1016/j.ccm.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Walker N, Gillen P. Investigating nurses’ perceptions of their role in managing sedation in intensive care: An exploratory study. Intensive Crit Care Nurs. 2006;22:338–45. doi: 10.1016/j.iccn.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 3.Egerod I. Uncertain terms of sedation in ICU: How nurse and physicians manage and describe sedation for mechanically ventilated patients. J Clin Nurs. 2002;11:831–40. doi: 10.1046/j.1365-2702.2002.00725.x. [DOI] [PubMed] [Google Scholar]
- 4.Slomka J, Hoffman-Hogg L, Mion LC, Bair N, Bobek MB, Arroliga A. Influence of clinician's values and perceptions on use of clinical practice guidelines for sedation. Am J Crit Care. 2000;9:412. [PubMed] [Google Scholar]
- 5.Murray K. The need for assessment of sedation in the critically ill. Nurs Crit Care. 1997;2:297–302. [PubMed] [Google Scholar]
- 6.Guttormson JL, Chlan L, Weinert C, Savik K. Factors influencing nurse sedation practices with mechanically ventilated patients: A U.S. national survey. Intensive Crit Care Nurs. 2010;26:44–50. doi: 10.1016/j.iccn.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Sedation and Analgesia Task Force of the American College of Critical Care Medicine (ACCM) of the Society of Critical Care Medicine. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119–41. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Robinson BR, Mueller EW, Henson K, Branson RD, Barsoum S, Tsuei BJ. An analgesia-delirium-sedation protocol for critically ill trauma patients reduces ventilator days and hospital length of stay. J Trauma. 2008;65:517–26. doi: 10.1097/TA.0b013e318181b8f6. [DOI] [PubMed] [Google Scholar]
- 9.Marshall J, Finn CA, Theodore AC. Impact of a clinical pharmacist-enforced intensive care unit sedation protocol on duration of mechanical ventilation and hospital stay. Crit Care Med. 2008;36:427–33. doi: 10.1097/01.CCM.0000300275.63811.B3. [DOI] [PubMed] [Google Scholar]
- 10.Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G, Shannon W, et al. Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Crit Care Med. 1999;27:2609–15. doi: 10.1097/00003246-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Urden LD, Stacy KM, Lough ME. 5th ed. St Louis: Mosby; 2010. Critical care Nursing Diagnosis and management; pp. 135–71. [Google Scholar]
- 12.Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119–41. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Bucknall TK, Manias E, Presneill JJ. A randomized trial of protocol- directed sedation management for mechanical ventilation in an Australian intensive care unit. Crit Care Med. 2008;36:1444–50. doi: 10.1097/CCM.0b013e318168f82d. [DOI] [PubMed] [Google Scholar]
- 14.Eduardo TA. Protocol based sedation versus conventional treatment in critically ill patients on mechanical ventilation. Rev Méd Chile. 2008;136:711–8. [PubMed] [Google Scholar]
- 15.Iranmanesh S, Rafiei H, Sabzevari S. Relationship between Braden scale score and pressure ulcer development in patients admitted in trauma intensive care unit. Int Wound J. 2012;9:248–52. doi: 10.1111/j.1742-481X.2011.00852.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dotson B. Daily interruption of sedation in patients treated with mechanical ventilation. Am J Health Syst Pharm. 2010;67:1002–6. doi: 10.2146/ajhp090134. [DOI] [PubMed] [Google Scholar]
- 17.Strom T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: A randomized trial. Lancet. 2010;375:475–80. doi: 10.1016/S0140-6736(09)62072-9. [DOI] [PubMed] [Google Scholar]
- 18.Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily interruption of sedative infusions in critically Ill patients undergoing mechanical ventilation. N Engl J Med. 2000;342:1471–7. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]
- 19.Pun BT, Dunn J. The sedation of critically ill adults: Part 2: Management. Am J Nurs. 2007;107:40–9. doi: 10.1097/01.NAJ.0000282293.72946.1f. [DOI] [PubMed] [Google Scholar]
- 20.Pun BT, Dunn J. The sedation of critically ill adults: Part 1: Assessment. The first in a two-part series focuses on assessing sedated patients in the ICU. Am J Nurs. 2007;107:40–8. doi: 10.1097/01.NAJ.0000279265.66906.2f. [DOI] [PubMed] [Google Scholar]
- 21.Cevik F, Celik M, Clark PM, Macit C. Sedation and analgesia in intensive care: A comparison of fentanyl and remifentanil. Pain Res Treat. 2011 doi: 10.1155/2011/650320. doi:10 1155/2011/650320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arabi Y, Haddad S, Hawes R, Moore T, Pillay M, Naidu B, et al. Changing sedation practices in the intensive care unit-protocol implementation, multifaceted multidisciplinary approach and teamwork. Middle East J Anesthesiol. 2007;19:429–47. [PubMed] [Google Scholar]
- 23.Iranmanesh S, Rafiei H, Foroogh AG. Critical care nurses’ knowledge about pressure ulcer in southeast of Iran. Int Wound J. 2011;8:459–64. doi: 10.1111/j.1742-481X.2011.00817.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rafiei H, Arab M, Ranjbar H, Sepehri GH, Arab N, Amiri M. The prevalence of potential drug interaction in intensive care unit. IJCCN. 2012;4:191–6. [Google Scholar]


