Abstract
Background:
Organophosphorous (OP) poisoning is one of the most common poisonings seen in India. OP compounds act through inhibition of enzyme acetylcholinesterase and estimation of pseudocholinesterase (PCE) activity strengthens the diagnosis in clinically uncertain cases of OP poisoning. The role of pralidoxime (PAM) therapy in OP poisoning has been controversial.
Study Objectives:
This study was aimed to determine the prognostic significance of estimation of PCE activity and also to assess the role of PAM therapy in OP poisoning.
Materials and Methods:
Patients of suspected OP poisoning of age >12 years admitted to emergency unit at a tertiary healthcare center of north India were enrolled. Patients were categorized into two groups; group A who were given intravenous atropine and group B who were given injectable PAM along with atropine. Serum PCE level was estimated at the time of admission in all patients and severity of OP poisoning was assessed according to PCE level. Requirement of atropine, oxygen inhalation, intubation and ventilatory support, total hospital stay, and mortality were compared between different classes of severity and also between Groups A and B.
Results:
This study included a total of 70 subjects, 35 in each group with mean age of 24.99 ± 8.7 years. Out of 70 subjects 49 (70%) were male and 21 (30%) were female. Forty nine patients (70%) of OP poisoning were with suicidal intent while 21 (30%) cases were accidentally poisoned. In all suicidal cases route of poisoning was ingestion whereas in all the accidental cases route of exposure was inhalational. PCE levels were reduced in all the cases and the mean level was 3,154.16 ± 2,562.40 IU/L. The total dose of atropine required, need for oxygen inhalation and need for intubation and ventilatory support, mean duration of hospital stay and mortality rate (P = 0.003) were higher in moderate to severe cases and did not have significant difference between Groups A and B.
Conclusion:
The study recommends estimation of PCE level at admission to classify severity of OP poisoning and to estimate prognosis. This study did not find any beneficial role of PAM therapy in reducing morbidity as well as mortality.
Keywords: Atropine, insecticides, organophosphorous, pralidoxime, pseudocholinesterase
INTRODUCTION
It is estimated by World Health Organization (WHO) that around 0.3 million people die every year due to various poisonings.[1] OP poisoning is one of the most common poisoning seen in India. India has been predominantly an agricultural country since ancient times and pesticides/insecticides are used abundantly for cultivation and these substances are easily accessible to the people. The commonest types of insecticide/pesticides substance used for poisoning are organophosphates, chlorinated hydrocarbons, aluminium phosphide, carbamates, and pyrethroids. The prevalence of poisoning in India varies in different regions. Recent study from south India reported mortality rate of 4% in poisoning cases.[2]
In organophosphorous (OP) poisoning, common route is ingestion for suicidal purpose but infrequently accidental cases are also encountered where OP compounds have been ingested or inhaled by mistake. OP compounds are anti-acetylcholinesterase which exert their toxicity by allowing acetylcholine (ACh) to overact at its receptors in the central and peripheral nervous system. The anticholinesterase effects can be evidenced biochemically by suppressed levels of serum pseudocholinesterase (PCE) and red cell cholinesterases.
The significance of estimation of serum PCE in assessment of the severity as well as prognosis in patients of OP poisoning has been elusive in previous studies.[3,4] Similarly, the issue of Pralidoxime (PAM) therapy in OP poisoning has been controversial. In the present study, we made an effort to evaluate the prognostic significance of estimating serum PCE level and to assess the role of PAM administration on outcome in patients of OP poisoning.
MATERIALS AND METHODS
Patients of suspected OP poisoning of age >12 years hospitalized in a tertiary healthcare center of north India were enrolled for this study. Prior approval for the study was obtained from the institutional ethical committee. After explaining the possible prognosis, consent from a responsible attendant of the patient was taken. Patients poisoned with double insecticide, multiple poisoning with other drugs such as opioids, diazepam, barbiturate, etc., and patients with chronic medical illness or who were on drugs (aminophylline, succinylcholine, reserpine, and phenothiazine-type tranquilizers) were excluded. Patients with pregnancy or those who received treatment prior to admission at our hospital were also excluded from the study.
All patients were evaluated clinically by history and examination. Treatment was commenced as soon as the patients were attended. The patients were given stomach wash, body wash, and an intravenous line was established. An intravenous bolus of atropine (5-10 mg) was administered promptly. The patients were assessed for respiratory failure, and if so, intubated and shifted to intensive care unit (ICU) for mechanical ventilation. Patients were divided into two groups, Group A and B. Group A patients received injection atropine 2.4 mg every 5-10 min, till signs of atropinization appeared. Group B patients were given PAM along with injection atropine. PAM was given in the form of intravenous infusion (30 mg/kg body weight in 200 ml of normal saline over 30 min followed by 2.0 g in 200 ml of normal saline over 30 min, at 6 h interval for initial 72 h). Arterial blood gas, complete blood picture, random blood sugar, serum electrolytes, blood urea, serum creatinine, and chest X-ray were done routinely in all patients. Serum PCE level was estimated at the time of admission in all the patients by spectrophotometry method. The laboratory reference range for PCE used in the present study was 7,000-19,000 IU/L. Based on the serum PCE levels, the severity of poisoning was defined as per Kumar et al.[5]
Latent: PCE level >50% of normal or >3,500 IU/L
Mild poisoning: PCE level 20-50% of normal or >1,401-3,500 IU/L
Moderate poisoning: PCE level 10-20% of normal or 701-1,400 IU/L
Severe poisoning: PCE level is <10% of normal or <700 IU/L.
Statistical analysis
Data were presented either as mean ± standard deviation (SD) or as percentage and median. A comparison between Groups A and B was made by Mann-Whitney U test/two sample t-tests for quantitative data and Fisher's exact test for categorical data. A factor influencing outcome of interest was considered significant if its P value was <0.05. Analyses was performed with the statistical software Strata, version 11.1 (Stat Corp Inc., College Station, Texas, USA).
RESULTS
A total of 70 patients of OP poisoning were studied. Mean age of patient in our study was 24.99 ± 8.7 years. Mean age of patients in Groups A and B was 24.80 ± 8.3 and 25.17 ± 9.2 years, respectively. More than half of patients were in the age group of 20-30 years. Males were 49 (70%) and females were 21 (30%). Majority of patients were from rural areas (71.43%) and were agricultural workers by occupation. Forty-nine patients (70%) of OP poisoning were with suicidal intent, while 21 (30%) cases were accidentally poisoned. In all suicidal cases, route of poisoning was ingestion; whereas in all the accidental cases, route of exposure was inhalational. The mean time interval between OP exposure and admission to emergency ward was 5.60 ± 3.3 h. Majority of patients (75%) reached to medical facility within 6 h of exposure.
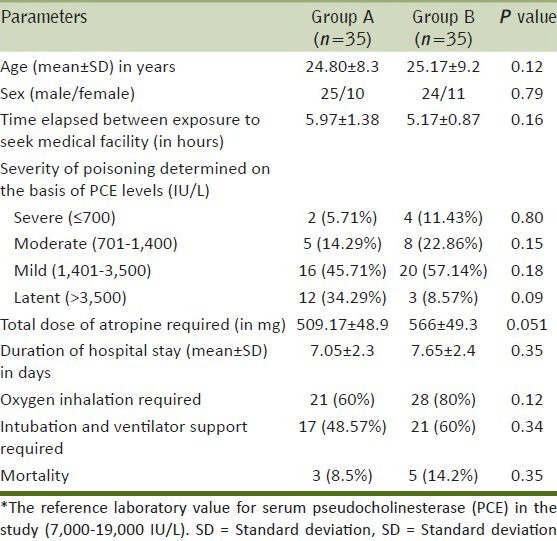
At admission, PCE levels was reduced in all cases and the mean level was 3,154.16 ± 2,562.40 IU/L. Around half of the patients had mild poisoning as classified by Kumar et al.[5] [Table 1]. The average dose of atropine used in study was 509.17 ± 48.9 mg in Group A and 566 ± 49.3 mg in Group B. The dose of atropine and need for oxygen inhalation was maximum in severe cases (PCE < 700 IU/L). An increasing trend was seen for percentages of the cases requiring oxygen inhalation and intubation as severity of OP poisoning increased. The mean duration of hospital stay was higher in moderate to severe cases. Similarly, mortality rate was higher in moderate to severe cases (P = 0.003). The total dose of atropine required, need for oxygen inhalation, intubation and vetilatory support, duration of hospital stay, and mortality rate did not have significant difference between Groups A and B [Table 2]. There was no mortality in patients with serum PCE levels above 4,000 IU/L.
Table 1.
Prognostic variables observed in accordance with the severity of OP poisoning determined through the levels of serum pseudocholinesterase
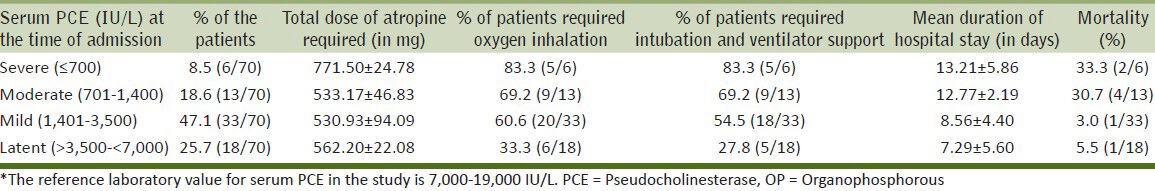
Table 2.
Depicts comparison of overall parameters in between Groups A and B
DISCUSSION
The present study found that the level of PCE on the day of presentation was reduced in all cases of OP poisoning. Similar to our finding, Areekul et al.,[6] also have found that PCE was lower than normal in all studied patients of OP poisoning; whereas, Mehta et al.,[7] observed lower activity of PCE in more than 70% of cases at presentation. Goswamy et al., in their study concluded that apart from clinical indicators, low serum cholinesterase levels were of greatest predictive value for ventilation in OP poisoning.[3] However, Aygun et al., found that serum cholinesterase level estimations are useful in diagnosis of OP poisoning in acute phase, but show no relation to severity of poisoning.[4] Nouira et al.,[8] did not find any statistically significant difference in mean serum cholinesterase levels in those mechanically ventilated and those not needing ventilatory support. Interestingly, the present study showed an increasing trend for percentages of the cases requiring oxygen inhalation and intubation as the severity of OP poisoning increased. In addition mortality was also high in moderate to severe cases. This showed a significant association of rate of mortality with the serum PCE levels. Ram et al.,[9] observed a mortality of 8% (four out of 45), with no correlation with serum PCE activity.
Second objective of the study was to evaluate the role of PAM in OP poisoning. The study did not find any beneficial role of PAM in OP poisoning to reduce mortality. The study favors the finding evaluated in meta-analysis by Peter et al.,[10] that there was no statistically significant association of oxime therapy with mortality and ventilator requirements.
In our study, cases that required ventilatory support were considered to have severe form of OP poisoning clinically and were intubated and put on ventilatory support as per availability of resources. Though it seemed clearly that ventilatory support was required in higher number of patients in Group B than Group A, but it was statistically insignificant (P = 0.059). Eddleston et al.,[11] found no evidence that PAM improves survival or reduces need for intubation in patients with OP poisoning.
The present study also did not find any significant difference in total dose of atropine required in both the groups. Thus, it supports the findings of Chugh et al.,[12] that the mean atropine requirement during the first 24 h did not have significant difference with PAM therapy. Further, the amount of atropine used daily from 24 h onward till final outcome, remained more or less same in both the groups. The total amount of atropine calculated in Group A was 248 ± 196.33 mg, and in Group B it was 235.48 ± 95.55 mg. Thus, observations of the present study are consistent with those who have claimed that PAM does not alter the dose requirement of atropine.
Although the average dose of atropine used in study was higher in patients presenting with serum PCE levels <700 IU/L, but we did not find any correlation of dose of atropine with the serum PCE levels. In contrary, Avasthi and Singh[13] observed an inverse relation between atropine requirement and the serum PCE levels.
Cases of OP poisoning were predominantly young males (below 40 years of age) and belonged to rural areas. This could be due to the facts that males have easy accessibility to OP compounds because they work in agriculture fields. The major route of poisoning in our study was by ingestion with suicidal intent. The accidental ingestion of OP compounds is very rare because of its taste and smell. Few patients initially presented with history of accidental ingestion, but later on it was revealed that OP compounds were taken because of suicidal intention. Accidental exposure through skin or by inhalation occurs in agricultural and industrial worker due to neglect of protective measures. About half of the patients were brought to emergency after 4 h of exposure to OP compounds. This could be related to the fact that majority of the patient were from rural areas (and agricultural workers by occupation) and needed to be brought to the hospital from their residence or site of poisoning for management.
This study is limited by the facts that sample size was small. Serum PCE level was estimated only at the time of admission. Daily estimation of PCE levels would have been more informative in foretelling the prognosis or severity of poisoning and to monitor the effectiveness of either therapy. The study was not randomized rather a case-control, this too limits our findings.
Still, we would like to conclude that the serum PCE is reduced in OP poisoning and serum PCE level should be estimated routinely in all cases of OP poisoning because it has prognostic significance. Moderate to severe cases of OP poisoning have higher morbidity and mortality. PAM therapy in addition to atropine was ineffective in reducing hospital stay, requirement of oxygen inhalation, intubation and mechanical ventilation, and mortality in OP poisoning.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Thundiyil JG, Stober J, Besbelli N, Pronczuk J. Acute pesticide poisoning: A proposed classification tool. Bull World Health Organ. 2008;86:205–9. doi: 10.2471/BLT.08.041814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jesslin J, Adepu R, Churi S. Assessment of prevalence and mortality incidences due to poisoning in a South Indian tertiary care teaching hospital. Indian J Pharm Sci. 2010;72:587–91. doi: 10.4103/0250-474X.78525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goswamy R, Chaudhuri A, Mahashur AA. Study of respiratory failure in organophosphate and carbamate poisoning. Heart Lung. 1994;23:466–72. [PubMed] [Google Scholar]
- 4.Aygun D, Dognnay Z, Altintop L, Guven H, Onar M, Deniz T, et al. Serum acetylcholinesterase and prognosis of acute organophosphate poisoning. J Toxicol Clin Toxicol. 2002;40:903–10. doi: 10.1081/clt-120016962. [DOI] [PubMed] [Google Scholar]
- 5.Kumar SV, Fareedullah MD, Sudhakar Y, Venkateswarlu B, Kumar EA. Current review on organophosphorus poisoning. Arch Appl Sci Res. 2010;2:199–215. [Google Scholar]
- 6.Areekul S, Srichairat S, Kirdudom P. Serum and red cell cholinesterase activity in people exposed to organophosphate insecticides. Southeast Asian J Trop Med Public Health. 1981;12:94–8. [PubMed] [Google Scholar]
- 7.Mehta AB, Shah AC, Joshi LG, Kale AK, Vora DD. Clinical features and plasma acetylcholinesterase activity in poisoning with insecticidal organophosphorus compounds. J Assoc Physicians India. 1971;19:181–4. [PubMed] [Google Scholar]
- 8.Nouira S, Abroug F, Elatrous S, Boujdaria R, Bouchoucha S. Prognostic value of serum cholinesterase in organophosphate poisoning. Chest. 1994;106:1811–4. doi: 10.1378/chest.106.6.1811. [DOI] [PubMed] [Google Scholar]
- 9.Ram JS, Kumar SS, Jayarajan A, Kuppuswamy G. Continuous infusion of high doses of atropine in the management of organophosphorus compound poisoning. J Assoc Physicians India. 1991;39:190–3. [PubMed] [Google Scholar]
- 10.Peter JV, Moran JL, Graham P. Oxime therapy and outcomes in human organophosphate poisoning: An evaluation using meta-analytic techniques. Crit Care Med. 2006;34:502–10. doi: 10.1097/01.ccm.0000198325.46538.ad. [DOI] [PubMed] [Google Scholar]
- 11.Eddleston M, Buckley NA, Eyer P, Dawson AH. Management of acute organophosphorus pesticides poisoning. Lancet. 2008;371:597–607. doi: 10.1016/S0140-6736(07)61202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chugh SN, Aggarwal N, Dabla S, Chhabra B. Comparative evaluation of atropine alone and atropine with pralidoxime in the management of organophosphorus poisoning. J Indian Aca Clin Med. 2005;6:33–7. [Google Scholar]
- 13.Avasthi G, Singh G. Serial Neuro-electrophysiological studies in acute organophosphate poisoning-correlation with clinical findings, serum cholinesterase levels and atropine dosage. J Assoc Physicians India. 2000;48:794–9. [PubMed] [Google Scholar]


