Abstract
Background:
Oculomotor nerve palsy (OMNP) is a well-recognized complication of posterior communicating artery (PCOM) aneurysms. Only a few comparative studies have assessed the effect of clipping versus coiling on recovery from OMNP in PCOM aneurysms. A retrospective review and meta-analysis was conducted to assess the relationship between PCOM aneurysm treatment and OMNP.
Materials and Methods:
Medical records of all patients presenting between January 2000 and February 2013 with intracranial aneurysm were searched. All patients with OMNP secondary to PCOM aneurysm were included for analysis. Patients undergoing surgical clipping or endovascular coiling were compared with respect to complete resolution of OMNP after aneurysm surgery (i.e., primary outcome). A meta-analysis of published studies of OMNP associated with PCOM aneurysm was performed after a MEDLINE search.
Results:
Seventeen patients with OMNP secondary to PCOM aneurysms met the inclusion criteria. Surgical clipping (seven of eight patients, or 87.5%) resulted in greater complete resolution of OMNP compared with endovascular coiling (four of nine patients, or 44.4%), P = 0.13. A meta-analysis of similar studies revealed that complete resolution of OMNP was more commonly associated with surgical clipping (36 of 43 patients, or 83.7%) than with endovascular coiling (29 of 55 patients, or 52.7%), yielding an adjusted odds ratio (OR) of 6.04 [confidence interval (CI) =1.88-19.45, P = 0.003]. Multivariate analysis found that the degree of pre-operative OMNP (OR = 0.07, CI = 0.02-0.28, P = 0.001) and surgical clipping (OR = 6.37, CI = 1.73-23.42, P = 0.005) were significant factors that affected the complete recovery of OMNP.
Conclusion:
Complete recovery of OMNP with PCOM aneurysms is more commonly associated with surgical clipping than with endovascular coiling. Also, the degree of pre-operative OMNP and the treatment modality are significant factors that affect the complete recovery of OMNP.
Keywords: Endovascular coiling, oculomotor nerve palsy, posterior communicating artery aneurysm, surgical clipping
Introduction
It has been estimated that oculomotor nerve palsy (OMNP) occurs in up to one-third of patients with posterior communicating artery (PCOM) aneurysms due to a mass effect on the oculomotor nerve.[1] This mass effect is not reduced after endovascular coiling of the aneurysm, unlike surgical clipping. However, endovascular coiling has been reported to result in high resolution rates for OMNP.[2,3,4] Treatment of OMNP with endovascular coiling may be alluring to clinicians in light of the recently published large trials.[5,6] These trials attest to better functional outcomes in patients undergoing endovascular coiling compared with surgical clipping.
Till date, there have been only a few comparative studies[7,8,9] that have assessed the efficacy of clipping or coiling on recovery from OMNP in PCOM aneurysms. All of these studies have been retrospective and inadequately powered (largest study of 17 patients), and have failed to produce consistent results. We therefore conducted a retrospective review of our database to assess the efficacy of surgical clipping or endovascular coiling on the resolution of OMNP associated with PCOM aneurysms. We also performed a meta-analysis of similar data from previously published studies in order to provide more information for clinical decision making.
Materials and Methods
After institutional review board approval, all patients presenting with intracranial aneurysm at the Duke University Hospital between January 2000 and February 2013 were identified using the appropriate International Classification of Diseases (ICD 9) code. Patients were included in the analysis if OMNP was diagnosed as secondary to a PCOM aneurysm. Patients were excluded from the analysis if they had incomplete medical records, were not followed-up for at least 6 months or till complete resolution of OMNP or if they were not treated with surgical clipping or endovascular coiling. Degree of OMNP was defined based on previous studies.[7,10] OMNP was defined as being complete if the following features were noted to be present: Ptosis, Mydriasis, Opthalmoplegia and Diplopia. If any of the above features was absent, the OMNP was defined as partial. Similarly, complete resolution of OMNP was defined as the absence of any of the above features. If any of the features persisted during the follow-up or remained the same as in the pre-operative assessment, the patients were categorized as having partial or no recovery, respectively. All preliminary data were collected by an investigator (SAK) from the electronic medical records (eBrowser, version 7.07, Pegasus Imaging Corporation, Tampa, FL, USA) and from the Duke's decision support repository (DSR) via the Duke Enterprise Data Unified Content Explorer (DEDUCE) portal. The DSR is a quality-assured custom-built data warehouse containing integrated clinical and financial data of all patients admitted to the Duke health care system.[11] Individual values that deviated noticeably from the normal, or any missing data points, were further cross-checked manually by a separate investigator (AA) after completion of the preliminary data collection. Medical conditions at the time of admission were considered to be present if they were recorded in the electronic medical records. The primary outcome (recovery from OMNP) was obtained from the follow-up notes of neurosurgeons, neurologists or neuro-ophthalmologists attending to the patients.
Literature search
Two independent reviewers (SAK and AA) performed a MEDLINE search using combinations of keywords: “Posterior Communicating artery aneurysm” and “oculomotor nerve palsy,” “third nerve palsy,” “cranial nerve palsy” or “ophthalmoplegia.” The search was limited to all English language publications in humans that were published between 1 January 1990 and 31 March 2013. Full texts of all publications considered to be relevant were obtained and the references of these studies were searched manually until no further relevant publications were found. Studies were included in the meta-analysis if they met all the following criteria: (1) were regarding OMNP associated with PCOM aneurysms, (2) included patient(s) undergoing surgical clipping or endovascular coiling, (3) had the degree and resolution of OMNP defined as per our definition or had adequate patient details available for us to best apply our definitions, (4) had all patients followed-up till complete resolution of OMNP or at least 6 months and (5) had medical details (age, sex, incidence of aneurysm rupture, degree of OMNP at admission, period from OMNP onset to treatment, type of treatment and degree of OMNP resolution) for each patient available. Any disagreement between the two independent reviewers was resolved by consensus with the senior author (MLJ).
Statistical analysis
Data are presented as median [interquartile range (IQR)] for continuous variables and as count (percentage) for categorical variables. Mann–Whitney U test or Chi-square tests were used for intergroup comparisons as appropriate. Odds ratios (ORs) were adjusted using logistic regression for unbalanced co-variates on univariate analysis. Statistical significance was defined as P < 0.05. A multivariate regression analysis to determine the independent predictors for complete resolution of OMNP was performed. Multivariable analysis included age, degree of pre-operative OMNP, aneurysm size, aneurysm rupture, time between diagnosis to treatment and treatment modality (clipping or coiling) as independent variables, based on previous studies.[1,2,4,7,9,10,12,13,14,15] A backward stepwise method was used to construct the multivariate regression model with the inclusion criterion of P < 0.05. All analyses were performed using SPSS version 20.0 (SPSS, Chicago, IL, USA).
Results
Current retrospective comparative study
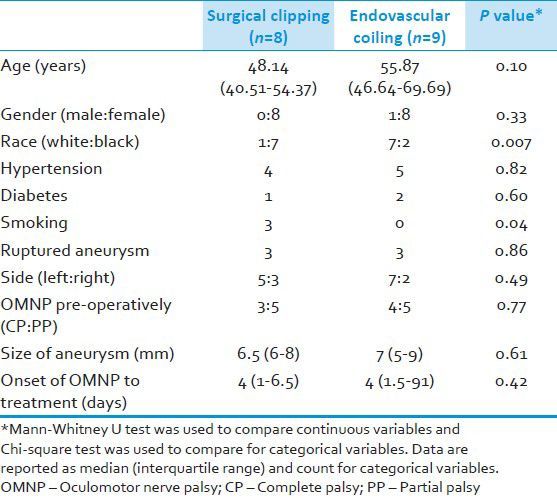
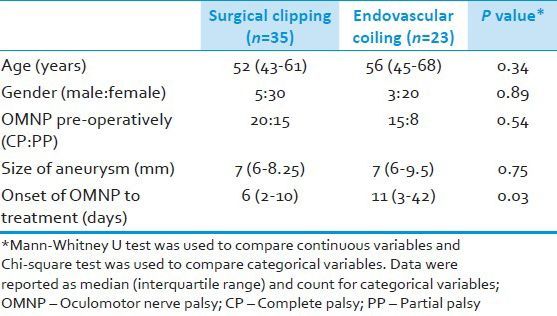
Seventeen patients with OMNP associated with PCOM aneurysm met the inclusion criteria. Eight (47%) patients underwent surgical clipping and nine (52.9%) patients underwent endovascular coiling. Detailed comparison of the demographics is presented in Table 1. Overall, the median (IQR) age was 39.24 (45.77-61.83) years, the median (IQR) size of the aneurysm was 7 (5.50-8.50) mm and the median (IQR) onset of OMNP to treatment duration in our cohort was 4 (1-12) days. Complete resolution of OMNP was seen in seven (87.5%) and four (44.4%) patients in the surgical clipping and endovascular coiling groups, respectively (P = 0.13).
Table 1.
Comparison of characteristics between patients undergoing surgical clipping and endovascular coiling in the current comparative study
Meta-analysis
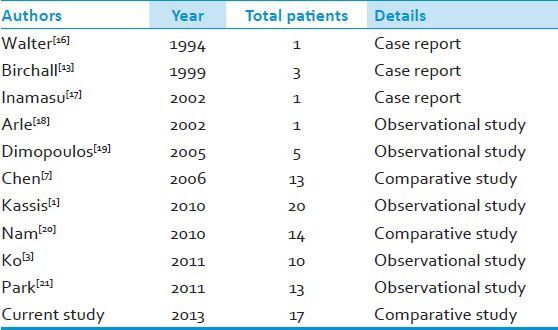
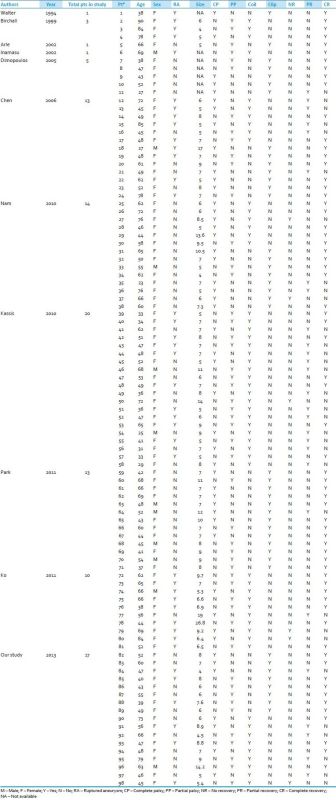
The MEDLINE search yielded 835 publications. After removal of 392 duplicate publications, 443 of the remaining publications were screened for relevance by two independent reviewers (SAK and AA). After the review, 10 publications met all inclusion criteria and were included in the final meta-analysis with the current comparative study. Table 2 and Appendix 1 contain the details of the included studies.
Table 2.
Details of all the studies included in the meta-analysis
Characteristics of all patients included in the meta-analysis
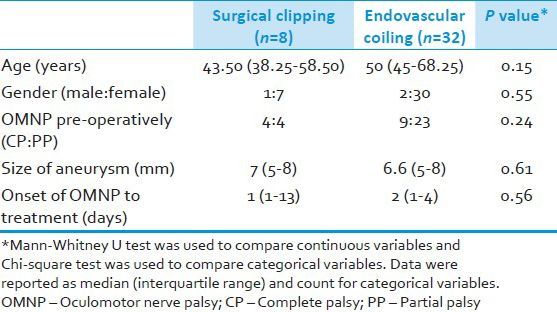
There were 98 patients from 11 studies included in the meta-analysis. Forty-three (43.9%) patients underwent surgical clipping while 55 (56.1%) patients underwent endovascular coiling. Overall, the median (IQR) age was 52 (44-65.25) years, the median (IQR) size of the aneurysm was 7 (6-8.5) mm and the median (IQR) onset of OMNP to treatment duration were 4 (1-10.25) days. A detailed comparison of the patient characteristics in the study population is presented in Table 3. Complete resolution of OMNP occurred more often in patients with surgical clipping compared with that in patients with endovascular coiling, [36 (83.7%) vs. 29 (52.7%); P = 0.001]. After adjusting for incidence of aneurysm rupture, odds of complete recovery occurred more commonly with surgical clipping (OR = 6.04; CI = 1.88-19.45; P = 0.003; Figure 1).
Table 3.
Comparison of the characteristics of all patients undergoing surgical clipping or endovascular coiling in the meta-analysis
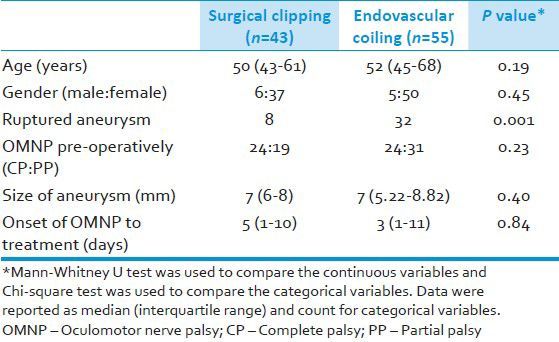
Figure 1.
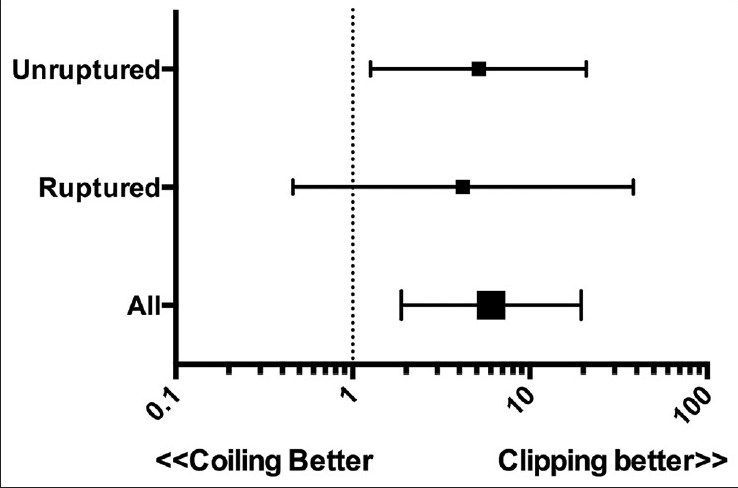
Forest plot of the adjusted odds of complete resolution of oculomotor nerve palsy
Unruptured aneurysms
Of the 58 patients with unruptured aneurysms included in the meta-analysis, 35 (60.3%) and 23 (39.6%) patients underwent surgical clipping and endovascular coiling, respectively. A detailed comparison of the patient characteristics between the two groups with unruptured aneurysms is presented in Table 4. Patients in the surgical coiling group had significantly shorter durations of OMNP before treatment compared with the endovascular coiling group. Complete resolution of OMNP occurred more often in patients with surgical clipping compared with that in patients with endovascular coiling [29 (82.8%) vs. nine (39.1%); P = 0.001]. After adjusting for the difference in durations of OMNP before treatment between the two groups, the odds of complete recovery occurred more frequently with surgical clipping (OR = 5.13; CI = 1.26-20.84; P = 0.02; Figure 1).
Table 4.
Comparison of the characteristics of all patients with unruptured aneurysms undergoing surgical clipping or endovascular coiling in the meta-analysis
Ruptured aneurysms
Of the 40 patients with ruptured aneurysms included in the meta-analysis, eight (20%) and 32 (80%) patients underwent surgical clipping and endovascular coiling, respectively. A detailed comparison of the patient characteristics between the two groups with ruptured aneurysms is presented in Table 5.
Table 5.
Comparison of the characteristics of all patients with ruptured aneurysms undergoing surgical clipping or endovascular coiling in the meta-analysis
Complete resolution of OMNP occurred more often in patients with surgical clipping compared with that in patients with endovascular coiling, seven (87.5%) vs. 20 (62.5%) patients, respectively, yielding an OR of 4.2 (CI = 0.46-38.44; P = 0.24; Figure 1).
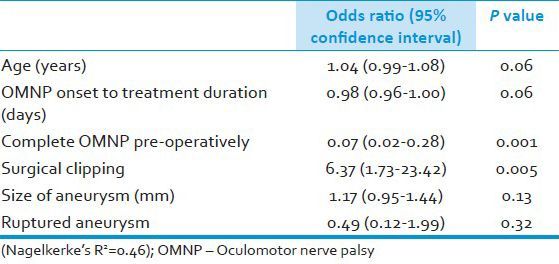
Predictors of complete resolution of OMNP
The predictive model (Nagelkerke's R2 = 0.46) produced by stepwise backward logistical regression suggested that the degree of OMNP before treatment and treatment modality (endovascular coiling or surgical clipping) were significant predictors of complete resolution of OMNP [Table 6].
Table 6.
Multivariate logistical regression analysis of predictors of complete resolution of OMNP
Discussion
This comparative study and meta-analysis found that complete resolution of OMNP was more commonly associated with surgical clipping than with endovascular coiling (although statistical significance was achieved only in the meta-analysis).
OMNP can result from PCOM aneurysms due to close anatomical proximity. Mass effect from an enlarging aneurysm or irritation from a blood clot from a ruptured aneurysm has been suggested as the causative factor.[1,7,10] Unlike surgical clipping, endovascular coiling does not relieve the mass effect on the nerve but has still been shown to produce recovery of OMNP in several studies and case series.[2,3,4] This beneficial effect of endovascular coiling may result from decreased pulsatility of the PCOM aneurysm.[13,22] The potential to produce OMNP recovery via the less-invasive endovascular coiling route is appealing. Few comparative studies have compared the efficacy of surgical clipping and endovascular coiling with respect to recovery from OMNP.[7,8,9] Unlike the study by Ahn et al., which was not able to demonstrate differences between clipping and coiling,[8] Chen et al. were able to show a significant improvement with surgical clipping.[7] In the present comparative study, complete recovery from OMNP occurred in 87.5% and 44.4% patients in the clipping and endovascular coiling groups, respectively. Unfortunately, this study did not achieve the required power to demonstrate a difference between the treatment modalities. This illustrates a major limitation with all studies in the subject, leaving the clinician unable to draw meaningful conclusions.
Most studies assessing the efficacy of surgical clipping versus endovascular coiling in resolution of OMNP associated with PCOM aneurysms have limited power to detect a clinically significant effect size. One meta-analysis on this subject has been published by Guresir et al.,[9] which reviewed all published data before 2009. However, several studies on this subject have been published since 2009.[1,2,3,20,21] Therefore, a meta-analysis of all the similar publications in this topic was conducted.
We found that, overall, patients undergoing surgical clipping were more likely to have a complete resolution of OMNP compared with those having endovascular coiling even after adjusting for ORs. This was similar in patients with unruptured PCOM aneurysms, where the odds of recovery of OMNP were more with surgical clipping. However, a difference in recovery of OMNP for patients with ruptured aneurysms was not achieved. Although this was most likely a result of a lack of power, the difference could also be due to the different pathological mechanisms of OMNP. OMNP in ruptured aneurysms may be due to the presence of blood near the nerve rather than a mass effect of the aneurysm wall itself. Therefore, recovery in such cases may be dependent on clot resolution rather than aneurysm decompression.[1] It may be further hypothesized that in such cases, endovascular coiling may prove equally efficacious to surgical clipping.
Previous studies have suggested that factors like aneurysm size,[15] age,[12] duration of OMNP onset to treatment,[2,10,14] pre-operative degree of OMNP[7,9,10] or the presence of ruptured aneurysms[1,2,4] with OMNP may effect complete recovery from OMNP. In the present multivariate analysis, degree of OMNP pre-operatively and treatment modality (endovascular coiling or surgical clipping) significantly effected complete OMNP recovery. These results are similar to the results of previous studies,[9,10] which found no relation between aneurysm size and OMNP. Thus, our results agree with the concept that OMNP associated with PCOM aneurysms may be due to a combination of mass effect and pulsatility, with little correlation to aneurysm size.[9] Also, similar to other studies,[7,9] our data suggest that age, duration of OMNP onset to treatment and the presence of ruptured aneurysms did not influence complete recovery from OMNP.
Our study has some limitations. Firstly, our current comparative study and the subsequent meta-analysis contain only retrospective data. Although we compared the study groups with respect to all variables known to affect the primary outcome, there are certainly confounders and variables unaccounted for that may affect the results. There is a conspicuous absence of prospective randomized trials in this subject area, which should be addressed in future research. The results of our study and meta-analysis provide essential data like sample size required, expected treatment effect size and potential factors that can effect recovery from OMNP, which may be required to design a future randomized controlled trial. Secondly, as with all meta-analysis, there may be subtle differences in definition and assessment of primary outcomes between studies. We tried to overcome this potential issue by defining a priori our outcomes and by including only those studies in the meta-analysis that conformed most to our definitions or included patient details that allowed us to best apply our definitions.
Conclusions
We found that complete recovery of OMNP with PCOM aneurysms is more commonly associated with surgical clipping than with endovascular coiling. Also, the degree of OMNP pre-operatively and the treatment modality are significant factors that affect complete recovery of OMNP.
Appendix 1: Details of all patients included in the meta-analysis
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kassis SZ, Jouanneau E, Tahon FB, Salkine F, Perrin G, Turjman F. Recovery of third nerve palsy after endovascular treatment of posterior communicating artery aneurysms. World Neurosurg. 2010;73:11–6. doi: 10.1016/j.surneu.2009.03.042. [DOI] [PubMed] [Google Scholar]
- 2.Zhang SH, Pei W, Cai XS, Cheng G. Endovascular management and recovery from oculomotor nerve palsy associated with aneurysms of the posterior communicating artery. World Neurosurg. 2010;74:316–9. doi: 10.1016/j.wneu.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 3.Ko JH, Kim YJ. Oculomotor nerve palsy caused by posterior communicating artery aneurysm: Evaluation of symptoms after endovascular treatment. Interv Neuroradiol. 2011;17:415–9. doi: 10.1177/159101991101700403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mansour N, Kamel MH, Kelleher M, Aquilina K, Thornton J, Brennan P, et al. Resolution of cranial nerve paresis after endovascular management of cerebral aneurysms. Surg Neurol. 2007;68:500–4. doi: 10.1016/j.surneu.2006.12.061. [DOI] [PubMed] [Google Scholar]
- 5.McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, et al. The barrow ruptured aneurysm trial. J Neurosurg. 2012;116:135–44. doi: 10.3171/2011.8.JNS101767. [DOI] [PubMed] [Google Scholar]
- 6.Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366:809–17. doi: 10.1016/S0140-6736(05)67214-5. [DOI] [PubMed] [Google Scholar]
- 7.Chen PR, Amin-Hanjani S, Albuquerque FC, McDougall C, Zabramski JM, Spetzler RF. Outcome of oculomotor nerve palsy from posterior communicating artery aneurysms: Comparison of clipping and coiling. Neurosurgery. 2006;58:1040–6. doi: 10.1227/01.NEU.0000215853.95187.5E. [DOI] [PubMed] [Google Scholar]
- 8.Ahn JY, Han IB, Yoon PH, Kim SH, Kim NK, Kim S, et al. Clipping vs coiling of posterior communicating artery aneurysms with third nerve palsy. Neurology. 2006;66:121–3. doi: 10.1212/01.wnl.0000191398.76450.c4. [DOI] [PubMed] [Google Scholar]
- 9.Guresir E, Schuss P, Setzer M, Platz J, Seifert V, Vatter H. Posterior communicating artery aneurysm-related oculomotor nerve palsy: Influence of surgical and endovascular treatment on recovery: Single-center series and systematic review. Neurosurgery. 2011;68:1527–34. doi: 10.1227/NEU.0b013e31820edd82. [DOI] [PubMed] [Google Scholar]
- 10.Hanse MC, Gerrits MC, van Rooij WJ, Houben MP, Nijssen PC, Sluzewski M. Recovery of posterior communicating artery aneurysm-induced oculomotor palsy after coiling. AJNR Am J Neuroradiol. 2008;29:988–90. doi: 10.3174/ajnr.A1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horvath MM, Winfield S, Evans S, Slopek S, Shang H, Ferranti J. The DEDUCE Guided Query tool: Providing simplified access to clinical data for research and quality improvement. J Biomed Inform. 2011;44:266–76. doi: 10.1016/j.jbi.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albuquerque FC. Coiling versus clipping for posterior communicating artery aneurysms associated with oculomotor nerve palsy: Only time will tell. World Neurosurg. 2010;74:250–1. doi: 10.1016/j.wneu.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 13.Birchall D, Khangure MS, McAuliffe W. Resolution of third nerve paresis after endovascular management of aneurysms of the posterior communicating artery. AJNR Am J Neuroradiol. 1999;20:411–3. [PMC free article] [PubMed] [Google Scholar]
- 14.Leivo S, Hernesniemi J, Luukkonen M, Vapalahti M. Early surgery improves the cure of aneurysm-induced oculomotor palsy. Surg Neurol. 1996;45:430–4. doi: 10.1016/0090-3019(95)00432-7. [DOI] [PubMed] [Google Scholar]
- 15.Teasdale E, Statham P, Straiton J, Macpherson P. Non-invasive radiological investigation for oculomotor palsy. J Neurol Neurosurg Psychiatry. 1990;53:549–53. doi: 10.1136/jnnp.53.7.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walter KA, Newman NJ, Lessell S. Oculomotor palsy from minor head trauma: Initial sign of intracranial aneurysm. Neurology. 1994;44:148–50. doi: 10.1212/wnl.44.1.148. [DOI] [PubMed] [Google Scholar]
- 17.Inamasu J, Nakamura Y, Saito R, Kuroshima Y, Ohba S, Ichikizaki K. Early resolution of third nerve palsy following endovascular treatment of a posterior communicating artery aneurysm. J Neuroophthalmol. 2002;22:12–4. doi: 10.1097/00041327-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Arle JE, Abrahams JM, Zager EL, Taylor C, Galetta SL. Pupil-sparing third nerve palsy with preoperative improvement from a posterior communicating artery aneurysm. Surg Neurol. 2002;57:423–7. doi: 10.1016/s0090-3019(02)00717-6. [DOI] [PubMed] [Google Scholar]
- 19.Dimopoulos VG, Fountas KN, Feltes CH, Robinson JS, Grigorian AA. Literature review regarding the methodology of assessing third nerve paresis associated with non-ruptured posterior communicating artery aneurysms. Neurosurg Rev. 2005;28:256–60. doi: 10.1007/s10143-005-0393-6. [DOI] [PubMed] [Google Scholar]
- 20.Nam KH, Choi CH, Lee JI, Ko JG, Lee TH, Lee SW. Unruptured Intracranial Aneurysms with Oculomotor Nerve Palsy: Clinical Outcome between Surgical Clipping and Coil Embolization. J Korean Neurosurg Soc. 2010;48:109–14. doi: 10.3340/jkns.2010.48.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park J, Kang DH, Chun BY. Superciliary keyhole surgery for unruptured posterior communicating artery aneurysms with oculomotor nerve palsy: Maximizing symptomatic resolution and minimizing surgical invasiveness. J Neurosurg. 2011;115:700–6. doi: 10.3171/2011.5.JNS102087. [DOI] [PubMed] [Google Scholar]
- 22.Halbach VV, Higashida RT, Dowd CF, Barnwell SL, Fraser KW, Smith TP, et al. The efficacy of endosaccular aneurysm occlusion in alleviating neurological deficits produced by mass effect. J Neurosurg. 1994;80:659–66. doi: 10.3171/jns.1994.80.4.0659. [DOI] [PubMed] [Google Scholar]


